User login
Changes in Hospital Glycemic Control
The prevalence of diabetes mellitus continues to increase, now affecting almost 26 million people in the United States alone.[1] Hospitalizations associated with diabetes also continue to rise,[2] and nearly 50% of the $174 billion annual costs related to diabetes care in the United States are for inpatient hospital stays.[3] In recent years, inpatient glucose control has received considerable attention, and consensus statements for glucose targets have been published.[4, 5, 6]
A number of developments support the rationale for tracking and reporting inpatient glucose control. For instance, there are clinical scenarios where treatment of hyperglycemia has been shown to lead to better patient outcomes.[6, 7, 8, 9] Second, several organizations have recognized the value of better inpatient glucose management and have developed educational resources to assist practitioners and their institutions toward achieving that goal.[10, 11, 12, 13, 14] Finally, pay‐for‐performance requirements are emerging that are relevant to inpatient diabetes management.[15, 16]
Reports on the status of inpatient glucose control in large samples of US hospitals are now becoming available, and their findings suggest differences on the basis of hospital size, hospital type, and geographic location.[17, 18] However, these reports represent cross‐sectional studies, and little is known about trends in hospital glucose control over time. To determine whether changes were occurring, we obtained inpatient point‐of‐care blood glucose (POC‐BG) data from 126 hospitals for January to December 2009 and compared these with glycemic control data collected from the same hospitals for January to December 2007,[19] separately analyzing measurements from the intensive care unit (ICU) and the non‐intensive care unit (non‐ICU).
METHODS
Data Collection
The methods we used for data collection have been described previously.[18, 19, 20] Hospitals in the study used standard bedside glucose meters downloaded to the Remote Automated Laboratory System‐Plus (RALS‐Plus) (Medical Automation Systems, Charlottesville, VA). We originally evaluated data for adult inpatients for the period from January to December 2007[19]; for this study, we extracted POC‐BG from the same hospitals for the period from January to December 2009. Data excluded measurements obtained in emergency departments. Patient‐specific data (age, sex, race, and diagnoses) were not provided by hospitals, but individual patients could be distinguished by a unique identifier and also by location (ICU vs non‐ICU).
Hospital Selection
The characteristics of the 126 hospitals have been published previously.[19] However, hospital characteristics for 2009 were reevaluated for this analysis using the same methods already described for 2007[19] to determine whether any changes had occurred. Briefly, hospital characteristics during 2009 were determined via a combination of accessing the hospital Web site, consulting the Hospital Blue Book (Billian's HealthDATA; Billian Publishing Inc., Atlanta, Georgia), and determining membership in the Council of Teaching Hospitals and Health Systems of the Association of American Medical Colleges. The characteristics of the hospitals were size (number of beds), type (academic, urban community, or rural), and geographic region (Northeast, Midwest, South, or West). Per the Hospital Blue Book, a rural hospital is a hospital that operates outside of a metropolitan statistical area, typically with fewer than 100 beds, whereas an urban hospital is located within a metropolitan statistical area, typically with more than 100 beds. Institutions provided written permission to remotely access their glucose data and combine it with other hospitals into a single database for analysis. Patient data were deidentified, and consent to retrospective analysis and reporting was waived. The analysis was considered exempt by the Mayo Clinic Institutional Review Board. Participating hospitals were guaranteed confidentiality regarding their data.
Statistical Analysis
ICU and non‐ICU glucose datasets were differentiated on the basis of the download location designated by the RALS‐Plus database. As previously described, patient‐day‐weighted mean POC‐BG values were calculated as means of daily POC‐BG averaged per patient across all days during the hospital stay.[18, 19] We determined the overall patient‐day‐weighted mean values, and also the proportion of patient‐day‐weighted mean values greater than 180, 200, 250, 300, 350, and 400 mg/dL.[18, 19] We also examined the data to determine if there were any changes in the proportion of patient hospital days when there was at least 1 value <70 mg/dL or <40 mg/dL.
Differences in patient‐day‐weighted mean POC‐BG values between the years 2007 and 2009 were assessed in a mixed‐effects model with the term of year as the fixed effect and hospital characteristics as the random effect. The glucose trends between years 2007 and 2009 were examined to identify any differentiation by hospital characteristics by conducting mixed‐effects models using the terms of year, hospital characteristics (hospital size by bed capacity, hospital type, or geographic region), and interaction between year as the fixed effects and hospital characteristics as the random effect. These analyses were performed separately for ICU patients and non‐ICU patients. Values were compared between data obtained in 2009 and that obtained previously in 2007 using the Pearson [2] test. The means within the same category of hospital characteristics were compared for the years 2007 and 2009.
RESULTS
Characteristics of Participating Hospitals
Fewer than half of the 126 hospitals had changes in characteristics from 2007 to 2009 (size and type [Table 1]). There were 71 hospitals whose characteristics did not change compared to when the previous analysis was performed. The rest (n = 55) had changes in their characteristics that resulted in a net redistribution in the number of beds in the <200 and 200 to 299 categories, and a change in the rural/urban categories. These changes slightly altered the distributions by hospital size and hospital type compared to those in the previous analysis (Table 1). The regional distribution of the 126 hospitals was 41 (32.5%) in the South, 37 (29.4%) in the Midwest, 28 (22.2%) in the West, and 20 (15.9%) in the Northeast.[19]
| Characteristic | 2007, No. (%) [N = 126] | 2009, No. (%) [N = 126] |
|---|---|---|
| Hospital size, no. of beds | ||
| <200 | 48 (38.1) | 45 (35.7) |
| 200299 | 25 (19.8) | 28 (22.2) |
| 300399 | 17 (13.5) | 17 (13.5) |
| 400 | 36 (28.6) | 36 (28.6) |
| Hospital type | ||
| Academic | 11 (8.7) | 11 (8.7) |
| Urban | 69 (54.8) | 79 (62.7) |
| Rural | 46 (36.5) | 36 (28.6) |
Changes in Glycemic Control
For 2007, we analyzed a total of 12,541,929 POC‐BG measurements for 1,010,705 patients, and for 2009, we analyzed a total of 10,659,418 measurements for 656,206 patients. For ICU patients, a mean of 4.6 POC‐BG measurements per day was obtained in 2009 compared to a mean of 4.7 POC‐BG measurements per day in 2007. For non‐ICU patients, the POC‐BG mean was 3.1 per day in 2009 vs 2.9 per day in 2007.
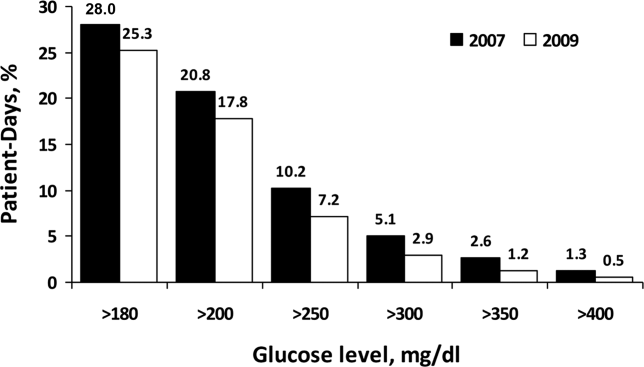
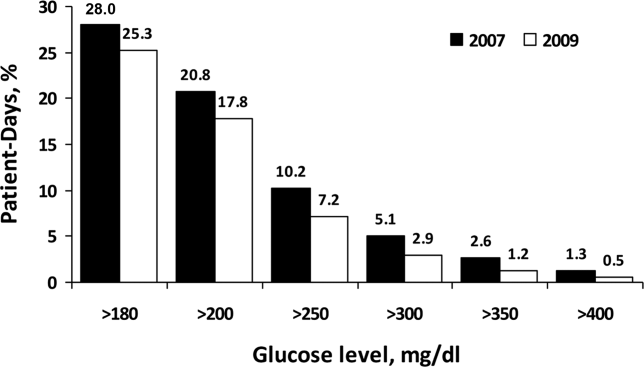
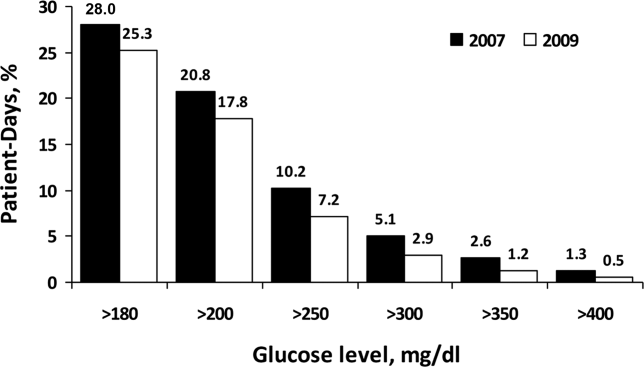
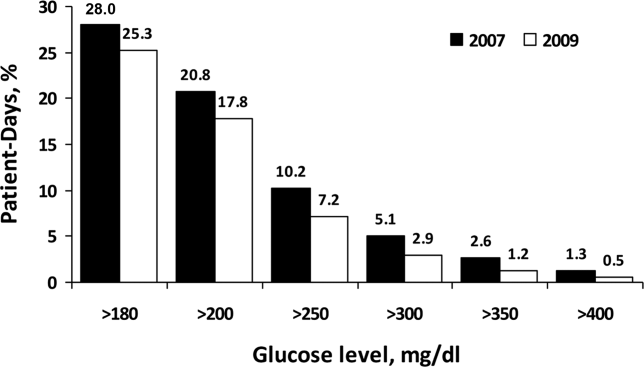
For non‐ICU data, the patient‐day‐weighted mean POC‐BG values decreased in 2009 by 5 mg/dL compared with the 2007 values (154 mg/dL vs 159 mg/dL, respectively; P < 0.001), and were clinically unchanged in the ICU data (167 mg/dL vs 166 mg/dL, respectively; P < 0.001). For non‐ICU data, the proportion of patient‐day‐weighted mean POC‐BG values in any hyperglycemia category decreased in 2009 compared with those in 2007 among all patients (all P < 0.001) (Figure 1). For the ICU data, there was no significant difference (all P > 0.20; not shown) from 2007 to 2009.
In the ICU data, 2.9% of patient days on average had at least 1 POC‐BG value <70 mg/dL in both 2007 and 2009 (P = 0.67). There were fewer patient days with values <40 mg/dL in 2009 (1.1%) compared to 2007 (1.4%) in the ICU (P < 0.001). In the non‐ICU data, the mean percentage of patient days with a value <70 mg/dL was higher in 2009 (5.1%) than in 2007 (4.7%) (P < 0.001); however, there were actually fewer patient days in 2009 on average with a value <40 mg/dL (0.84% vs 1.1% for 2009 vs 2007; P < 0.001).
Changes in Glycemic Control by Hospital Characteristics
Next, changes in glucose levels between the 2 analytic periods were evaluated according to hospital characteristics. Significant interactions were found between the year and each of the hospital characteristics both for the ICU group (Table 2) and for the non‐ICU group (Table 3) (all P < 0.001 for interaction terms). In the ICU data, changes were generally small but significant on the basis of hospital size, hospital type, and geographic region, and these changes were not necessarily in the same direction, because there were increases in patient‐day‐weighted mean glucose values in some categories, whereas there were decreases in others. For instance, hospitals with <200 inpatient beds experienced no significant change in ICU glycemic control, whereas those with 200 to 299 beds or >400 beds had an increase in patient‐day‐weighted mean values, and ones with 300 to 399 beds had a decrease. In regard to hospital type, only ICUs in academic medical institutions had a significant change over time in patient‐day‐weighted mean glucose levels, and these changes were toward higher values. ICUs in institutions in the Northeast and West had significantly higher glucose levels between the 2 periods, whereas those in the Midwest and South demonstrated lower glucose levels. In contrast to the different trends in ICU data by hospital characteristics, non‐ICU glucose control improved for hospitals of all sizes and types, and in all regions, over time.
| Characteristic | Year 2007, mg/dL | Year 2009, mg/dL | P Value |
|---|---|---|---|
| |||
| Overall | 166 (1) | 167 (1) | <0.001 |
| Hospital size, no. of beds | |||
| <200 | 175 (2) | 174 (2) | 0.19 |
| 200299 | 164 (2) | 165 (2) | 0.009 |
| 300399 | 166 (3) | 164 (3) | <0.002 |
| 400 | 157 (2) | 160 (2) | <0.001 |
| Hospital type | |||
| Academic | 150 (3) | 156 (4) | <0.001 |
| Rural | 172 (2) | 172 (2) | 0.94 |
| Urban | 166 (1) | 166 (1) | 0.61 |
| Region | |||
| Northeast | 165 (3) | 167 (3) | 0.003 |
| Midwest | 169 (2) | 168 (2) | 0.007 |
| South | 168 (2) | 167 (2) | <0.001 |
| West | 160 (2) | 165 (2) | <0.001 |
| Characteristic | Year 2007, mg/dL | Year 2009, mg/dL | P Value |
|---|---|---|---|
| |||
| Overall | 159 (1) | 154 (1) | <0.001 |
| Hospital size, no. of beds | |||
| <200 | 162 (2) | 158 (2) | <0.001 |
| 200299 | 156 (2) | 152 (2) | <0.001 |
| 300399 | 158 (3) | 151 (3) | <0.001 |
| 400 | 156 (2) | 151 (2) | < 0.001 |
| Hospital type | |||
| Academic | 162 (3) | 159 (3) | <0.001 |
| Rural | 161 (2) | 156 (2) | <0.001 |
| Urban | 157 (1) | 152 (1) | <0.001 |
| Region | |||
| Northeast | 162 (3) | 158 (3) | <0.001 |
| Midwest | 157 (2) | 149 (2) | <0.001 |
| South | 160 (2) | 157 (2) | <0.001 |
| West | 156 (2) | 151 (2) | <0.001 |
DISCUSSION
Optimal management of hospital hyperglycemia is now advocated by a number of professional societies and organizations.[10, 11, 12, 13] One of the next major tasks in the area of inpatient diabetes management will be how to identify and evaluate changes in glycemic control among US hospitals over time. Respondents to a recent survey of hospitals indicated that most institutions are now attempting to initiate quality improvement programs for the management of inpatients with diabetes.[21] These initiatives may translate into objective changes that could be monitored on a national level. However, few data exist on trends in glucose control in US hospitals. In our analysis, POC‐BG data from 126 hospitals collected in 2009 were compared to data obtained from the same hospitals in 2007. Our findings, and the methods of data collection and analysis described previously,[18, 19] demonstrate how such data can be used as a national benchmarking process for inpatient glucose control.
At all levels of hyperglycemia, significant decreases in patient‐day‐weighted mean values were found in non‐ICU data but not in ICU data. During the time these data were collected, recommendations about glucose targets in the critically ill were in a state of flux.[22, 23, 24, 25, 26, 27] Thus, the lack of hyperglycemia improvement in the ICU data between 2007 and 2009 may reflect the reluctance of providers to aggressively manage hyperglycemia because of recent reports linking increased mortality to tight glucose control.[25, 28, 29, 30] The differences in patient‐day‐weighted mean glucose values detected in the non‐ICU data between the 2 analytic periods were statistically significant, but were otherwise small and may not have clinical implications as far as an association with improved patient outcomes. Ongoing longitudinal analysis is required to establish whether these improvements in non‐ICU glucose control will persist over time.
Changes in glycemic control between the 2 periods were also noted when data were stratified according to hospital characteristics. Differences in glucose control in ICU data were not consistently better or worse, but varied by category of hospital characteristics (hospital size, hospital type, and geographic region). Other than academic hospitals and hospitals in the West, changes in the ICU data were small and likely do not have clinical importance. Analysis of non‐ICU data, however, showed consistent improvement within all 3 categories. Some hospital characteristics did change between the 2 study periods: there were fewer hospitals with <200 beds, more hospitals with 200 to 299 beds, a decrease in hospitals identified as rural, and an increase in hospitals designated as urban. Our previous analyses have indicated that hospital characteristics should be considered when examining national inpatient glucose data.[18, 19] In this analysis there was a statistically significant interaction between the year for which data were analyzed and each category of hospital characteristics. It is unclear how these evolving characteristics could have impacted inpatient glucose control. A change in hospital characteristics may in fact represent a change in resources to manage inpatient hyperglycemia. Future studies with nationally aggregated inpatient glucose data that assess longitudinal changes in glucose data may also have to account for variations in hospital characteristics over time in addition to the characteristics of the hospitals themselves.
Differences in hypoglycemia frequency, as calculated as the proportion of patient hospital days, were also detected. In the ICU data, the percentage of days with at least 1 value <70 mg/dL was similar between 2007 and 2009, but the proportion of days with at least 1 value <40 mg/dL was less in 2009, suggesting that institutions as a whole in this analysis may have been more focused on reducing the frequency of severe hypoglycemia. However, in the non‐ICU, there were more days in 2009 with a value <70 mg/dL, but fewer with a value <40 mg/dL. In noncritically ill patients, institutions likely continue to attempt to find the best balance between optimizing glycemic control while minimizing the risk of hypoglycemia. It should be pointed out, however, that overall, the frequency of hypoglycemia, particularly severe hypoglycemia, was quite low in this analysis, as it has been in our previous reports.[18, 19] An examination of hypoglycemia frequency by hospital characteristic to evaluate differences in this metric would be of interest in a future analysis.
The limitations of these data have been previously outlined,[18, 19] and they include the lack of patient‐level data such as demographics and the lack of information on diagnoses that allow adjustment of comparisons by the severity of illness. Moreover, without detailed treatment‐specific information (such as type of insulin protocol), one cannot establish the basis for longitudinal differences in glucose control. Volunteer‐dependent hospital involvement that creates selection bias may skew data toward those who are aware that they are witnessing a successful reduction in hyperglycemia. Finally, POC‐BG may not be the optimal method for assessing glycemic control. The limitations of current methods of evaluating inpatient glycemic control were recently reviewed.[31] Nonetheless, POC‐BG measurements remain the richest source of data on hospital hyperglycemia because of their widespread use and large sample size. A data warehouse of nearly 600 hospitals now exists,[18] which will permit future longitudinal analyses of glucose control in even larger samples.
Despite such limitations, our findings do represent the first analysis of trends in glucose control in a large cross‐section of US hospitals. Over 2 years, non‐ICU hyperglycemia improved among hospitals of all sizes and types and in all regions, whereas similar improvement did not occur in ICU hyperglycemia. Continued analysis will determine whether these trends continue. For those hospitals that are achieving better glucose control in non‐ICU patients, more information is needed on how they are accomplishing this so that protocols can be standardized and disseminated.
Acknowledgments
Disclosures: This project was supported entirely by The Epsilon Group Virginia, LLC, Charlottesville, Virginia, and a contractual arrangement is in place between the Mayo Clinic, Scottsdale, Arizona, and The Epsilon Group. The Mayo Clinic does not endorse the products mentioned in this article. The authors report no conflicts of interest.
- 2011 National Diabetes Fact Sheet.Diagnosed and undiagnosed diabetes in the United States, all ages, 2010.Atlanta, GA:Centers for Disease Control and Prevention;2011 [updated 2011]. Available at: http://www.cdc.gov/diabetes/pubs/estimates11.htm#2. Accessed November 23, 2012.
- Diabetes Data and Trends.Atlanta, GA:Centers for Disease Control and Prevention;2009 [updated 2009]. Available at: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed November 23, 2012.
- American Diabetes Association. Economic costs of diabetes in the U.S. In 2007 [published correction appears in Diabetes Care. 2008;31(6):1271.]. Diabetes Care. 2008;31(3):596–615.
- , , , et al.;American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10(1):77–82.
- ACE/ADA Task Force on Inpatient Diabetes. American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control. Endocr Pract. 2006;12(4):458–468.
- , , , et al.;American Association of Clinical Endocrinologists; American Diabetes Association. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32(6):1119–1131.
- ;DIGAMI (Diabetes Mellitus, Insulin Glucose Infusion in Acute Myocardial Infarction) Study Group. Prospective randomised study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus. BMJ. 1997;314(7093):1512–1515.
- , , , et al.;American Diabetes Association Diabetes in Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals [published correction appears in Diabetes Care. 2004;27(5):1255; Diabetes Care. 2004;27(3):856]. Diabetes Care. 2004;27(2):553–591.
- , , , , . Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital. J Hosp Med. 2006;1(3):145–150.
- , , , , ;Society of Hospital Medicine Glycemic Control Task Force. Society of Hospital Medicine Glycemic Control Task Force summary: practical recommendations for assessing the impact of glycemic control efforts. J Hosp Med. 2008;3(5 suppl):66–75.
- , , , , , . Adherence to surgical care improvement project measures and the association with postoperative infections. JAMA. 2010;303(24):2479–2485.
- Glycemic Control Resource Room.Philadelphia, PA:Society of Hospital Medicine;2008. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm. Accessed November 23, 2012.
- Inpatient Glycemic Control Resource Center.Jacksonville, FL:American Association of Clinical Endocrinologists;2011. Available at: http://resources.aace.com. Accessed November 23, 2012.
- , , , et al.;Endocrine Society. Management of hyperglycemia in hospitalized patients in non‐critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(1):16–38.
- Hospital Quality Initiative.Baltimore, MD:Centers for Medicare and Medicaid Services;2012 [updated 2012]. Available at: http://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp. Accessed November 23, 2012.
- Hospital‐Acquired Conditions (Present on Admission Indicator).Baltimore, MD:Centers for Medicare and Medicaid Services;2012 [updated 2012]. Available at: http://www.cms.gov/hospitalacqcond/06_hospital‐acquired_conditions.asp. Accessed November 23, 2012.
- , , , et al. Evaluation of hospital glycemic control at US academic medical centers. J Hosp Med. 2009;4(1):35–44.
- , , , . Update on inpatient glycemic control in hospitals in the United States. Endocr Pract. 2011;17(6):853–861.
- , , , , , . Inpatient glucose control: a glycemic survey of 126 U.S. hospitals. J Hosp Med. 2009;4(9):E7–E14.
- , , , , . Inpatient point‐of‐care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control. Diabetes Technol Ther. 2007;9(6):493–500.
- , , , , , . Diabetes and hyperglycemia quality improvement efforts in hospitals in the United States: current status, practice variation, and barriers to implementation. Endocr Pract. 2010;16(2):219–230.
- , , , et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–1367.
- , , , et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449–461.
- , , , et al.;German Competence Network Sepsis (SepNet). Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358(2):125–139.
- , , , et al.;NICE‐SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–1297.
- , , , et al. A prospective randomised multi‐centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med. 2009;35(10):1738–1748.
- , , . Benefits and risks of tight glucose control in critically ill adults: a meta‐analysis [published correction appears in JAMA. 2009;301(9):936]. JAMA. 2008;300(8):933–944.
- , . Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med. 2007;35(10):2262–2267.
- , , , et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA. 2009;301(15):1556–1564.
- , , , et al. Hypoglycemia and outcome in critically ill patients. Mayo Clin Proc. 2010;85(3):217–224.
- , , , . Assessing inpatient glycemic control: what are the next steps?J Diabetes Sci Technol. 2012;6(2):421–427.
The prevalence of diabetes mellitus continues to increase, now affecting almost 26 million people in the United States alone.[1] Hospitalizations associated with diabetes also continue to rise,[2] and nearly 50% of the $174 billion annual costs related to diabetes care in the United States are for inpatient hospital stays.[3] In recent years, inpatient glucose control has received considerable attention, and consensus statements for glucose targets have been published.[4, 5, 6]
A number of developments support the rationale for tracking and reporting inpatient glucose control. For instance, there are clinical scenarios where treatment of hyperglycemia has been shown to lead to better patient outcomes.[6, 7, 8, 9] Second, several organizations have recognized the value of better inpatient glucose management and have developed educational resources to assist practitioners and their institutions toward achieving that goal.[10, 11, 12, 13, 14] Finally, pay‐for‐performance requirements are emerging that are relevant to inpatient diabetes management.[15, 16]
Reports on the status of inpatient glucose control in large samples of US hospitals are now becoming available, and their findings suggest differences on the basis of hospital size, hospital type, and geographic location.[17, 18] However, these reports represent cross‐sectional studies, and little is known about trends in hospital glucose control over time. To determine whether changes were occurring, we obtained inpatient point‐of‐care blood glucose (POC‐BG) data from 126 hospitals for January to December 2009 and compared these with glycemic control data collected from the same hospitals for January to December 2007,[19] separately analyzing measurements from the intensive care unit (ICU) and the non‐intensive care unit (non‐ICU).
METHODS
Data Collection
The methods we used for data collection have been described previously.[18, 19, 20] Hospitals in the study used standard bedside glucose meters downloaded to the Remote Automated Laboratory System‐Plus (RALS‐Plus) (Medical Automation Systems, Charlottesville, VA). We originally evaluated data for adult inpatients for the period from January to December 2007[19]; for this study, we extracted POC‐BG from the same hospitals for the period from January to December 2009. Data excluded measurements obtained in emergency departments. Patient‐specific data (age, sex, race, and diagnoses) were not provided by hospitals, but individual patients could be distinguished by a unique identifier and also by location (ICU vs non‐ICU).
Hospital Selection
The characteristics of the 126 hospitals have been published previously.[19] However, hospital characteristics for 2009 were reevaluated for this analysis using the same methods already described for 2007[19] to determine whether any changes had occurred. Briefly, hospital characteristics during 2009 were determined via a combination of accessing the hospital Web site, consulting the Hospital Blue Book (Billian's HealthDATA; Billian Publishing Inc., Atlanta, Georgia), and determining membership in the Council of Teaching Hospitals and Health Systems of the Association of American Medical Colleges. The characteristics of the hospitals were size (number of beds), type (academic, urban community, or rural), and geographic region (Northeast, Midwest, South, or West). Per the Hospital Blue Book, a rural hospital is a hospital that operates outside of a metropolitan statistical area, typically with fewer than 100 beds, whereas an urban hospital is located within a metropolitan statistical area, typically with more than 100 beds. Institutions provided written permission to remotely access their glucose data and combine it with other hospitals into a single database for analysis. Patient data were deidentified, and consent to retrospective analysis and reporting was waived. The analysis was considered exempt by the Mayo Clinic Institutional Review Board. Participating hospitals were guaranteed confidentiality regarding their data.
Statistical Analysis
ICU and non‐ICU glucose datasets were differentiated on the basis of the download location designated by the RALS‐Plus database. As previously described, patient‐day‐weighted mean POC‐BG values were calculated as means of daily POC‐BG averaged per patient across all days during the hospital stay.[18, 19] We determined the overall patient‐day‐weighted mean values, and also the proportion of patient‐day‐weighted mean values greater than 180, 200, 250, 300, 350, and 400 mg/dL.[18, 19] We also examined the data to determine if there were any changes in the proportion of patient hospital days when there was at least 1 value <70 mg/dL or <40 mg/dL.
Differences in patient‐day‐weighted mean POC‐BG values between the years 2007 and 2009 were assessed in a mixed‐effects model with the term of year as the fixed effect and hospital characteristics as the random effect. The glucose trends between years 2007 and 2009 were examined to identify any differentiation by hospital characteristics by conducting mixed‐effects models using the terms of year, hospital characteristics (hospital size by bed capacity, hospital type, or geographic region), and interaction between year as the fixed effects and hospital characteristics as the random effect. These analyses were performed separately for ICU patients and non‐ICU patients. Values were compared between data obtained in 2009 and that obtained previously in 2007 using the Pearson [2] test. The means within the same category of hospital characteristics were compared for the years 2007 and 2009.
RESULTS
Characteristics of Participating Hospitals
Fewer than half of the 126 hospitals had changes in characteristics from 2007 to 2009 (size and type [Table 1]). There were 71 hospitals whose characteristics did not change compared to when the previous analysis was performed. The rest (n = 55) had changes in their characteristics that resulted in a net redistribution in the number of beds in the <200 and 200 to 299 categories, and a change in the rural/urban categories. These changes slightly altered the distributions by hospital size and hospital type compared to those in the previous analysis (Table 1). The regional distribution of the 126 hospitals was 41 (32.5%) in the South, 37 (29.4%) in the Midwest, 28 (22.2%) in the West, and 20 (15.9%) in the Northeast.[19]
| Characteristic | 2007, No. (%) [N = 126] | 2009, No. (%) [N = 126] |
|---|---|---|
| Hospital size, no. of beds | ||
| <200 | 48 (38.1) | 45 (35.7) |
| 200299 | 25 (19.8) | 28 (22.2) |
| 300399 | 17 (13.5) | 17 (13.5) |
| 400 | 36 (28.6) | 36 (28.6) |
| Hospital type | ||
| Academic | 11 (8.7) | 11 (8.7) |
| Urban | 69 (54.8) | 79 (62.7) |
| Rural | 46 (36.5) | 36 (28.6) |
Changes in Glycemic Control
For 2007, we analyzed a total of 12,541,929 POC‐BG measurements for 1,010,705 patients, and for 2009, we analyzed a total of 10,659,418 measurements for 656,206 patients. For ICU patients, a mean of 4.6 POC‐BG measurements per day was obtained in 2009 compared to a mean of 4.7 POC‐BG measurements per day in 2007. For non‐ICU patients, the POC‐BG mean was 3.1 per day in 2009 vs 2.9 per day in 2007.
For non‐ICU data, the patient‐day‐weighted mean POC‐BG values decreased in 2009 by 5 mg/dL compared with the 2007 values (154 mg/dL vs 159 mg/dL, respectively; P < 0.001), and were clinically unchanged in the ICU data (167 mg/dL vs 166 mg/dL, respectively; P < 0.001). For non‐ICU data, the proportion of patient‐day‐weighted mean POC‐BG values in any hyperglycemia category decreased in 2009 compared with those in 2007 among all patients (all P < 0.001) (Figure 1). For the ICU data, there was no significant difference (all P > 0.20; not shown) from 2007 to 2009.
In the ICU data, 2.9% of patient days on average had at least 1 POC‐BG value <70 mg/dL in both 2007 and 2009 (P = 0.67). There were fewer patient days with values <40 mg/dL in 2009 (1.1%) compared to 2007 (1.4%) in the ICU (P < 0.001). In the non‐ICU data, the mean percentage of patient days with a value <70 mg/dL was higher in 2009 (5.1%) than in 2007 (4.7%) (P < 0.001); however, there were actually fewer patient days in 2009 on average with a value <40 mg/dL (0.84% vs 1.1% for 2009 vs 2007; P < 0.001).
Changes in Glycemic Control by Hospital Characteristics
Next, changes in glucose levels between the 2 analytic periods were evaluated according to hospital characteristics. Significant interactions were found between the year and each of the hospital characteristics both for the ICU group (Table 2) and for the non‐ICU group (Table 3) (all P < 0.001 for interaction terms). In the ICU data, changes were generally small but significant on the basis of hospital size, hospital type, and geographic region, and these changes were not necessarily in the same direction, because there were increases in patient‐day‐weighted mean glucose values in some categories, whereas there were decreases in others. For instance, hospitals with <200 inpatient beds experienced no significant change in ICU glycemic control, whereas those with 200 to 299 beds or >400 beds had an increase in patient‐day‐weighted mean values, and ones with 300 to 399 beds had a decrease. In regard to hospital type, only ICUs in academic medical institutions had a significant change over time in patient‐day‐weighted mean glucose levels, and these changes were toward higher values. ICUs in institutions in the Northeast and West had significantly higher glucose levels between the 2 periods, whereas those in the Midwest and South demonstrated lower glucose levels. In contrast to the different trends in ICU data by hospital characteristics, non‐ICU glucose control improved for hospitals of all sizes and types, and in all regions, over time.
| Characteristic | Year 2007, mg/dL | Year 2009, mg/dL | P Value |
|---|---|---|---|
| |||
| Overall | 166 (1) | 167 (1) | <0.001 |
| Hospital size, no. of beds | |||
| <200 | 175 (2) | 174 (2) | 0.19 |
| 200299 | 164 (2) | 165 (2) | 0.009 |
| 300399 | 166 (3) | 164 (3) | <0.002 |
| 400 | 157 (2) | 160 (2) | <0.001 |
| Hospital type | |||
| Academic | 150 (3) | 156 (4) | <0.001 |
| Rural | 172 (2) | 172 (2) | 0.94 |
| Urban | 166 (1) | 166 (1) | 0.61 |
| Region | |||
| Northeast | 165 (3) | 167 (3) | 0.003 |
| Midwest | 169 (2) | 168 (2) | 0.007 |
| South | 168 (2) | 167 (2) | <0.001 |
| West | 160 (2) | 165 (2) | <0.001 |
| Characteristic | Year 2007, mg/dL | Year 2009, mg/dL | P Value |
|---|---|---|---|
| |||
| Overall | 159 (1) | 154 (1) | <0.001 |
| Hospital size, no. of beds | |||
| <200 | 162 (2) | 158 (2) | <0.001 |
| 200299 | 156 (2) | 152 (2) | <0.001 |
| 300399 | 158 (3) | 151 (3) | <0.001 |
| 400 | 156 (2) | 151 (2) | < 0.001 |
| Hospital type | |||
| Academic | 162 (3) | 159 (3) | <0.001 |
| Rural | 161 (2) | 156 (2) | <0.001 |
| Urban | 157 (1) | 152 (1) | <0.001 |
| Region | |||
| Northeast | 162 (3) | 158 (3) | <0.001 |
| Midwest | 157 (2) | 149 (2) | <0.001 |
| South | 160 (2) | 157 (2) | <0.001 |
| West | 156 (2) | 151 (2) | <0.001 |
DISCUSSION
Optimal management of hospital hyperglycemia is now advocated by a number of professional societies and organizations.[10, 11, 12, 13] One of the next major tasks in the area of inpatient diabetes management will be how to identify and evaluate changes in glycemic control among US hospitals over time. Respondents to a recent survey of hospitals indicated that most institutions are now attempting to initiate quality improvement programs for the management of inpatients with diabetes.[21] These initiatives may translate into objective changes that could be monitored on a national level. However, few data exist on trends in glucose control in US hospitals. In our analysis, POC‐BG data from 126 hospitals collected in 2009 were compared to data obtained from the same hospitals in 2007. Our findings, and the methods of data collection and analysis described previously,[18, 19] demonstrate how such data can be used as a national benchmarking process for inpatient glucose control.
At all levels of hyperglycemia, significant decreases in patient‐day‐weighted mean values were found in non‐ICU data but not in ICU data. During the time these data were collected, recommendations about glucose targets in the critically ill were in a state of flux.[22, 23, 24, 25, 26, 27] Thus, the lack of hyperglycemia improvement in the ICU data between 2007 and 2009 may reflect the reluctance of providers to aggressively manage hyperglycemia because of recent reports linking increased mortality to tight glucose control.[25, 28, 29, 30] The differences in patient‐day‐weighted mean glucose values detected in the non‐ICU data between the 2 analytic periods were statistically significant, but were otherwise small and may not have clinical implications as far as an association with improved patient outcomes. Ongoing longitudinal analysis is required to establish whether these improvements in non‐ICU glucose control will persist over time.
Changes in glycemic control between the 2 periods were also noted when data were stratified according to hospital characteristics. Differences in glucose control in ICU data were not consistently better or worse, but varied by category of hospital characteristics (hospital size, hospital type, and geographic region). Other than academic hospitals and hospitals in the West, changes in the ICU data were small and likely do not have clinical importance. Analysis of non‐ICU data, however, showed consistent improvement within all 3 categories. Some hospital characteristics did change between the 2 study periods: there were fewer hospitals with <200 beds, more hospitals with 200 to 299 beds, a decrease in hospitals identified as rural, and an increase in hospitals designated as urban. Our previous analyses have indicated that hospital characteristics should be considered when examining national inpatient glucose data.[18, 19] In this analysis there was a statistically significant interaction between the year for which data were analyzed and each category of hospital characteristics. It is unclear how these evolving characteristics could have impacted inpatient glucose control. A change in hospital characteristics may in fact represent a change in resources to manage inpatient hyperglycemia. Future studies with nationally aggregated inpatient glucose data that assess longitudinal changes in glucose data may also have to account for variations in hospital characteristics over time in addition to the characteristics of the hospitals themselves.
Differences in hypoglycemia frequency, as calculated as the proportion of patient hospital days, were also detected. In the ICU data, the percentage of days with at least 1 value <70 mg/dL was similar between 2007 and 2009, but the proportion of days with at least 1 value <40 mg/dL was less in 2009, suggesting that institutions as a whole in this analysis may have been more focused on reducing the frequency of severe hypoglycemia. However, in the non‐ICU, there were more days in 2009 with a value <70 mg/dL, but fewer with a value <40 mg/dL. In noncritically ill patients, institutions likely continue to attempt to find the best balance between optimizing glycemic control while minimizing the risk of hypoglycemia. It should be pointed out, however, that overall, the frequency of hypoglycemia, particularly severe hypoglycemia, was quite low in this analysis, as it has been in our previous reports.[18, 19] An examination of hypoglycemia frequency by hospital characteristic to evaluate differences in this metric would be of interest in a future analysis.
The limitations of these data have been previously outlined,[18, 19] and they include the lack of patient‐level data such as demographics and the lack of information on diagnoses that allow adjustment of comparisons by the severity of illness. Moreover, without detailed treatment‐specific information (such as type of insulin protocol), one cannot establish the basis for longitudinal differences in glucose control. Volunteer‐dependent hospital involvement that creates selection bias may skew data toward those who are aware that they are witnessing a successful reduction in hyperglycemia. Finally, POC‐BG may not be the optimal method for assessing glycemic control. The limitations of current methods of evaluating inpatient glycemic control were recently reviewed.[31] Nonetheless, POC‐BG measurements remain the richest source of data on hospital hyperglycemia because of their widespread use and large sample size. A data warehouse of nearly 600 hospitals now exists,[18] which will permit future longitudinal analyses of glucose control in even larger samples.
Despite such limitations, our findings do represent the first analysis of trends in glucose control in a large cross‐section of US hospitals. Over 2 years, non‐ICU hyperglycemia improved among hospitals of all sizes and types and in all regions, whereas similar improvement did not occur in ICU hyperglycemia. Continued analysis will determine whether these trends continue. For those hospitals that are achieving better glucose control in non‐ICU patients, more information is needed on how they are accomplishing this so that protocols can be standardized and disseminated.
Acknowledgments
Disclosures: This project was supported entirely by The Epsilon Group Virginia, LLC, Charlottesville, Virginia, and a contractual arrangement is in place between the Mayo Clinic, Scottsdale, Arizona, and The Epsilon Group. The Mayo Clinic does not endorse the products mentioned in this article. The authors report no conflicts of interest.
The prevalence of diabetes mellitus continues to increase, now affecting almost 26 million people in the United States alone.[1] Hospitalizations associated with diabetes also continue to rise,[2] and nearly 50% of the $174 billion annual costs related to diabetes care in the United States are for inpatient hospital stays.[3] In recent years, inpatient glucose control has received considerable attention, and consensus statements for glucose targets have been published.[4, 5, 6]
A number of developments support the rationale for tracking and reporting inpatient glucose control. For instance, there are clinical scenarios where treatment of hyperglycemia has been shown to lead to better patient outcomes.[6, 7, 8, 9] Second, several organizations have recognized the value of better inpatient glucose management and have developed educational resources to assist practitioners and their institutions toward achieving that goal.[10, 11, 12, 13, 14] Finally, pay‐for‐performance requirements are emerging that are relevant to inpatient diabetes management.[15, 16]
Reports on the status of inpatient glucose control in large samples of US hospitals are now becoming available, and their findings suggest differences on the basis of hospital size, hospital type, and geographic location.[17, 18] However, these reports represent cross‐sectional studies, and little is known about trends in hospital glucose control over time. To determine whether changes were occurring, we obtained inpatient point‐of‐care blood glucose (POC‐BG) data from 126 hospitals for January to December 2009 and compared these with glycemic control data collected from the same hospitals for January to December 2007,[19] separately analyzing measurements from the intensive care unit (ICU) and the non‐intensive care unit (non‐ICU).
METHODS
Data Collection
The methods we used for data collection have been described previously.[18, 19, 20] Hospitals in the study used standard bedside glucose meters downloaded to the Remote Automated Laboratory System‐Plus (RALS‐Plus) (Medical Automation Systems, Charlottesville, VA). We originally evaluated data for adult inpatients for the period from January to December 2007[19]; for this study, we extracted POC‐BG from the same hospitals for the period from January to December 2009. Data excluded measurements obtained in emergency departments. Patient‐specific data (age, sex, race, and diagnoses) were not provided by hospitals, but individual patients could be distinguished by a unique identifier and also by location (ICU vs non‐ICU).
Hospital Selection
The characteristics of the 126 hospitals have been published previously.[19] However, hospital characteristics for 2009 were reevaluated for this analysis using the same methods already described for 2007[19] to determine whether any changes had occurred. Briefly, hospital characteristics during 2009 were determined via a combination of accessing the hospital Web site, consulting the Hospital Blue Book (Billian's HealthDATA; Billian Publishing Inc., Atlanta, Georgia), and determining membership in the Council of Teaching Hospitals and Health Systems of the Association of American Medical Colleges. The characteristics of the hospitals were size (number of beds), type (academic, urban community, or rural), and geographic region (Northeast, Midwest, South, or West). Per the Hospital Blue Book, a rural hospital is a hospital that operates outside of a metropolitan statistical area, typically with fewer than 100 beds, whereas an urban hospital is located within a metropolitan statistical area, typically with more than 100 beds. Institutions provided written permission to remotely access their glucose data and combine it with other hospitals into a single database for analysis. Patient data were deidentified, and consent to retrospective analysis and reporting was waived. The analysis was considered exempt by the Mayo Clinic Institutional Review Board. Participating hospitals were guaranteed confidentiality regarding their data.
Statistical Analysis
ICU and non‐ICU glucose datasets were differentiated on the basis of the download location designated by the RALS‐Plus database. As previously described, patient‐day‐weighted mean POC‐BG values were calculated as means of daily POC‐BG averaged per patient across all days during the hospital stay.[18, 19] We determined the overall patient‐day‐weighted mean values, and also the proportion of patient‐day‐weighted mean values greater than 180, 200, 250, 300, 350, and 400 mg/dL.[18, 19] We also examined the data to determine if there were any changes in the proportion of patient hospital days when there was at least 1 value <70 mg/dL or <40 mg/dL.
Differences in patient‐day‐weighted mean POC‐BG values between the years 2007 and 2009 were assessed in a mixed‐effects model with the term of year as the fixed effect and hospital characteristics as the random effect. The glucose trends between years 2007 and 2009 were examined to identify any differentiation by hospital characteristics by conducting mixed‐effects models using the terms of year, hospital characteristics (hospital size by bed capacity, hospital type, or geographic region), and interaction between year as the fixed effects and hospital characteristics as the random effect. These analyses were performed separately for ICU patients and non‐ICU patients. Values were compared between data obtained in 2009 and that obtained previously in 2007 using the Pearson [2] test. The means within the same category of hospital characteristics were compared for the years 2007 and 2009.
RESULTS
Characteristics of Participating Hospitals
Fewer than half of the 126 hospitals had changes in characteristics from 2007 to 2009 (size and type [Table 1]). There were 71 hospitals whose characteristics did not change compared to when the previous analysis was performed. The rest (n = 55) had changes in their characteristics that resulted in a net redistribution in the number of beds in the <200 and 200 to 299 categories, and a change in the rural/urban categories. These changes slightly altered the distributions by hospital size and hospital type compared to those in the previous analysis (Table 1). The regional distribution of the 126 hospitals was 41 (32.5%) in the South, 37 (29.4%) in the Midwest, 28 (22.2%) in the West, and 20 (15.9%) in the Northeast.[19]
| Characteristic | 2007, No. (%) [N = 126] | 2009, No. (%) [N = 126] |
|---|---|---|
| Hospital size, no. of beds | ||
| <200 | 48 (38.1) | 45 (35.7) |
| 200299 | 25 (19.8) | 28 (22.2) |
| 300399 | 17 (13.5) | 17 (13.5) |
| 400 | 36 (28.6) | 36 (28.6) |
| Hospital type | ||
| Academic | 11 (8.7) | 11 (8.7) |
| Urban | 69 (54.8) | 79 (62.7) |
| Rural | 46 (36.5) | 36 (28.6) |
Changes in Glycemic Control
For 2007, we analyzed a total of 12,541,929 POC‐BG measurements for 1,010,705 patients, and for 2009, we analyzed a total of 10,659,418 measurements for 656,206 patients. For ICU patients, a mean of 4.6 POC‐BG measurements per day was obtained in 2009 compared to a mean of 4.7 POC‐BG measurements per day in 2007. For non‐ICU patients, the POC‐BG mean was 3.1 per day in 2009 vs 2.9 per day in 2007.
For non‐ICU data, the patient‐day‐weighted mean POC‐BG values decreased in 2009 by 5 mg/dL compared with the 2007 values (154 mg/dL vs 159 mg/dL, respectively; P < 0.001), and were clinically unchanged in the ICU data (167 mg/dL vs 166 mg/dL, respectively; P < 0.001). For non‐ICU data, the proportion of patient‐day‐weighted mean POC‐BG values in any hyperglycemia category decreased in 2009 compared with those in 2007 among all patients (all P < 0.001) (Figure 1). For the ICU data, there was no significant difference (all P > 0.20; not shown) from 2007 to 2009.
In the ICU data, 2.9% of patient days on average had at least 1 POC‐BG value <70 mg/dL in both 2007 and 2009 (P = 0.67). There were fewer patient days with values <40 mg/dL in 2009 (1.1%) compared to 2007 (1.4%) in the ICU (P < 0.001). In the non‐ICU data, the mean percentage of patient days with a value <70 mg/dL was higher in 2009 (5.1%) than in 2007 (4.7%) (P < 0.001); however, there were actually fewer patient days in 2009 on average with a value <40 mg/dL (0.84% vs 1.1% for 2009 vs 2007; P < 0.001).
Changes in Glycemic Control by Hospital Characteristics
Next, changes in glucose levels between the 2 analytic periods were evaluated according to hospital characteristics. Significant interactions were found between the year and each of the hospital characteristics both for the ICU group (Table 2) and for the non‐ICU group (Table 3) (all P < 0.001 for interaction terms). In the ICU data, changes were generally small but significant on the basis of hospital size, hospital type, and geographic region, and these changes were not necessarily in the same direction, because there were increases in patient‐day‐weighted mean glucose values in some categories, whereas there were decreases in others. For instance, hospitals with <200 inpatient beds experienced no significant change in ICU glycemic control, whereas those with 200 to 299 beds or >400 beds had an increase in patient‐day‐weighted mean values, and ones with 300 to 399 beds had a decrease. In regard to hospital type, only ICUs in academic medical institutions had a significant change over time in patient‐day‐weighted mean glucose levels, and these changes were toward higher values. ICUs in institutions in the Northeast and West had significantly higher glucose levels between the 2 periods, whereas those in the Midwest and South demonstrated lower glucose levels. In contrast to the different trends in ICU data by hospital characteristics, non‐ICU glucose control improved for hospitals of all sizes and types, and in all regions, over time.
| Characteristic | Year 2007, mg/dL | Year 2009, mg/dL | P Value |
|---|---|---|---|
| |||
| Overall | 166 (1) | 167 (1) | <0.001 |
| Hospital size, no. of beds | |||
| <200 | 175 (2) | 174 (2) | 0.19 |
| 200299 | 164 (2) | 165 (2) | 0.009 |
| 300399 | 166 (3) | 164 (3) | <0.002 |
| 400 | 157 (2) | 160 (2) | <0.001 |
| Hospital type | |||
| Academic | 150 (3) | 156 (4) | <0.001 |
| Rural | 172 (2) | 172 (2) | 0.94 |
| Urban | 166 (1) | 166 (1) | 0.61 |
| Region | |||
| Northeast | 165 (3) | 167 (3) | 0.003 |
| Midwest | 169 (2) | 168 (2) | 0.007 |
| South | 168 (2) | 167 (2) | <0.001 |
| West | 160 (2) | 165 (2) | <0.001 |
| Characteristic | Year 2007, mg/dL | Year 2009, mg/dL | P Value |
|---|---|---|---|
| |||
| Overall | 159 (1) | 154 (1) | <0.001 |
| Hospital size, no. of beds | |||
| <200 | 162 (2) | 158 (2) | <0.001 |
| 200299 | 156 (2) | 152 (2) | <0.001 |
| 300399 | 158 (3) | 151 (3) | <0.001 |
| 400 | 156 (2) | 151 (2) | < 0.001 |
| Hospital type | |||
| Academic | 162 (3) | 159 (3) | <0.001 |
| Rural | 161 (2) | 156 (2) | <0.001 |
| Urban | 157 (1) | 152 (1) | <0.001 |
| Region | |||
| Northeast | 162 (3) | 158 (3) | <0.001 |
| Midwest | 157 (2) | 149 (2) | <0.001 |
| South | 160 (2) | 157 (2) | <0.001 |
| West | 156 (2) | 151 (2) | <0.001 |
DISCUSSION
Optimal management of hospital hyperglycemia is now advocated by a number of professional societies and organizations.[10, 11, 12, 13] One of the next major tasks in the area of inpatient diabetes management will be how to identify and evaluate changes in glycemic control among US hospitals over time. Respondents to a recent survey of hospitals indicated that most institutions are now attempting to initiate quality improvement programs for the management of inpatients with diabetes.[21] These initiatives may translate into objective changes that could be monitored on a national level. However, few data exist on trends in glucose control in US hospitals. In our analysis, POC‐BG data from 126 hospitals collected in 2009 were compared to data obtained from the same hospitals in 2007. Our findings, and the methods of data collection and analysis described previously,[18, 19] demonstrate how such data can be used as a national benchmarking process for inpatient glucose control.
At all levels of hyperglycemia, significant decreases in patient‐day‐weighted mean values were found in non‐ICU data but not in ICU data. During the time these data were collected, recommendations about glucose targets in the critically ill were in a state of flux.[22, 23, 24, 25, 26, 27] Thus, the lack of hyperglycemia improvement in the ICU data between 2007 and 2009 may reflect the reluctance of providers to aggressively manage hyperglycemia because of recent reports linking increased mortality to tight glucose control.[25, 28, 29, 30] The differences in patient‐day‐weighted mean glucose values detected in the non‐ICU data between the 2 analytic periods were statistically significant, but were otherwise small and may not have clinical implications as far as an association with improved patient outcomes. Ongoing longitudinal analysis is required to establish whether these improvements in non‐ICU glucose control will persist over time.
Changes in glycemic control between the 2 periods were also noted when data were stratified according to hospital characteristics. Differences in glucose control in ICU data were not consistently better or worse, but varied by category of hospital characteristics (hospital size, hospital type, and geographic region). Other than academic hospitals and hospitals in the West, changes in the ICU data were small and likely do not have clinical importance. Analysis of non‐ICU data, however, showed consistent improvement within all 3 categories. Some hospital characteristics did change between the 2 study periods: there were fewer hospitals with <200 beds, more hospitals with 200 to 299 beds, a decrease in hospitals identified as rural, and an increase in hospitals designated as urban. Our previous analyses have indicated that hospital characteristics should be considered when examining national inpatient glucose data.[18, 19] In this analysis there was a statistically significant interaction between the year for which data were analyzed and each category of hospital characteristics. It is unclear how these evolving characteristics could have impacted inpatient glucose control. A change in hospital characteristics may in fact represent a change in resources to manage inpatient hyperglycemia. Future studies with nationally aggregated inpatient glucose data that assess longitudinal changes in glucose data may also have to account for variations in hospital characteristics over time in addition to the characteristics of the hospitals themselves.
Differences in hypoglycemia frequency, as calculated as the proportion of patient hospital days, were also detected. In the ICU data, the percentage of days with at least 1 value <70 mg/dL was similar between 2007 and 2009, but the proportion of days with at least 1 value <40 mg/dL was less in 2009, suggesting that institutions as a whole in this analysis may have been more focused on reducing the frequency of severe hypoglycemia. However, in the non‐ICU, there were more days in 2009 with a value <70 mg/dL, but fewer with a value <40 mg/dL. In noncritically ill patients, institutions likely continue to attempt to find the best balance between optimizing glycemic control while minimizing the risk of hypoglycemia. It should be pointed out, however, that overall, the frequency of hypoglycemia, particularly severe hypoglycemia, was quite low in this analysis, as it has been in our previous reports.[18, 19] An examination of hypoglycemia frequency by hospital characteristic to evaluate differences in this metric would be of interest in a future analysis.
The limitations of these data have been previously outlined,[18, 19] and they include the lack of patient‐level data such as demographics and the lack of information on diagnoses that allow adjustment of comparisons by the severity of illness. Moreover, without detailed treatment‐specific information (such as type of insulin protocol), one cannot establish the basis for longitudinal differences in glucose control. Volunteer‐dependent hospital involvement that creates selection bias may skew data toward those who are aware that they are witnessing a successful reduction in hyperglycemia. Finally, POC‐BG may not be the optimal method for assessing glycemic control. The limitations of current methods of evaluating inpatient glycemic control were recently reviewed.[31] Nonetheless, POC‐BG measurements remain the richest source of data on hospital hyperglycemia because of their widespread use and large sample size. A data warehouse of nearly 600 hospitals now exists,[18] which will permit future longitudinal analyses of glucose control in even larger samples.
Despite such limitations, our findings do represent the first analysis of trends in glucose control in a large cross‐section of US hospitals. Over 2 years, non‐ICU hyperglycemia improved among hospitals of all sizes and types and in all regions, whereas similar improvement did not occur in ICU hyperglycemia. Continued analysis will determine whether these trends continue. For those hospitals that are achieving better glucose control in non‐ICU patients, more information is needed on how they are accomplishing this so that protocols can be standardized and disseminated.
Acknowledgments
Disclosures: This project was supported entirely by The Epsilon Group Virginia, LLC, Charlottesville, Virginia, and a contractual arrangement is in place between the Mayo Clinic, Scottsdale, Arizona, and The Epsilon Group. The Mayo Clinic does not endorse the products mentioned in this article. The authors report no conflicts of interest.
- 2011 National Diabetes Fact Sheet.Diagnosed and undiagnosed diabetes in the United States, all ages, 2010.Atlanta, GA:Centers for Disease Control and Prevention;2011 [updated 2011]. Available at: http://www.cdc.gov/diabetes/pubs/estimates11.htm#2. Accessed November 23, 2012.
- Diabetes Data and Trends.Atlanta, GA:Centers for Disease Control and Prevention;2009 [updated 2009]. Available at: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed November 23, 2012.
- American Diabetes Association. Economic costs of diabetes in the U.S. In 2007 [published correction appears in Diabetes Care. 2008;31(6):1271.]. Diabetes Care. 2008;31(3):596–615.
- , , , et al.;American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10(1):77–82.
- ACE/ADA Task Force on Inpatient Diabetes. American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control. Endocr Pract. 2006;12(4):458–468.
- , , , et al.;American Association of Clinical Endocrinologists; American Diabetes Association. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32(6):1119–1131.
- ;DIGAMI (Diabetes Mellitus, Insulin Glucose Infusion in Acute Myocardial Infarction) Study Group. Prospective randomised study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus. BMJ. 1997;314(7093):1512–1515.
- , , , et al.;American Diabetes Association Diabetes in Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals [published correction appears in Diabetes Care. 2004;27(5):1255; Diabetes Care. 2004;27(3):856]. Diabetes Care. 2004;27(2):553–591.
- , , , , . Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital. J Hosp Med. 2006;1(3):145–150.
- , , , , ;Society of Hospital Medicine Glycemic Control Task Force. Society of Hospital Medicine Glycemic Control Task Force summary: practical recommendations for assessing the impact of glycemic control efforts. J Hosp Med. 2008;3(5 suppl):66–75.
- , , , , , . Adherence to surgical care improvement project measures and the association with postoperative infections. JAMA. 2010;303(24):2479–2485.
- Glycemic Control Resource Room.Philadelphia, PA:Society of Hospital Medicine;2008. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm. Accessed November 23, 2012.
- Inpatient Glycemic Control Resource Center.Jacksonville, FL:American Association of Clinical Endocrinologists;2011. Available at: http://resources.aace.com. Accessed November 23, 2012.
- , , , et al.;Endocrine Society. Management of hyperglycemia in hospitalized patients in non‐critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(1):16–38.
- Hospital Quality Initiative.Baltimore, MD:Centers for Medicare and Medicaid Services;2012 [updated 2012]. Available at: http://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp. Accessed November 23, 2012.
- Hospital‐Acquired Conditions (Present on Admission Indicator).Baltimore, MD:Centers for Medicare and Medicaid Services;2012 [updated 2012]. Available at: http://www.cms.gov/hospitalacqcond/06_hospital‐acquired_conditions.asp. Accessed November 23, 2012.
- , , , et al. Evaluation of hospital glycemic control at US academic medical centers. J Hosp Med. 2009;4(1):35–44.
- , , , . Update on inpatient glycemic control in hospitals in the United States. Endocr Pract. 2011;17(6):853–861.
- , , , , , . Inpatient glucose control: a glycemic survey of 126 U.S. hospitals. J Hosp Med. 2009;4(9):E7–E14.
- , , , , . Inpatient point‐of‐care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control. Diabetes Technol Ther. 2007;9(6):493–500.
- , , , , , . Diabetes and hyperglycemia quality improvement efforts in hospitals in the United States: current status, practice variation, and barriers to implementation. Endocr Pract. 2010;16(2):219–230.
- , , , et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–1367.
- , , , et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449–461.
- , , , et al.;German Competence Network Sepsis (SepNet). Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358(2):125–139.
- , , , et al.;NICE‐SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–1297.
- , , , et al. A prospective randomised multi‐centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med. 2009;35(10):1738–1748.
- , , . Benefits and risks of tight glucose control in critically ill adults: a meta‐analysis [published correction appears in JAMA. 2009;301(9):936]. JAMA. 2008;300(8):933–944.
- , . Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med. 2007;35(10):2262–2267.
- , , , et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA. 2009;301(15):1556–1564.
- , , , et al. Hypoglycemia and outcome in critically ill patients. Mayo Clin Proc. 2010;85(3):217–224.
- , , , . Assessing inpatient glycemic control: what are the next steps?J Diabetes Sci Technol. 2012;6(2):421–427.
- 2011 National Diabetes Fact Sheet.Diagnosed and undiagnosed diabetes in the United States, all ages, 2010.Atlanta, GA:Centers for Disease Control and Prevention;2011 [updated 2011]. Available at: http://www.cdc.gov/diabetes/pubs/estimates11.htm#2. Accessed November 23, 2012.
- Diabetes Data and Trends.Atlanta, GA:Centers for Disease Control and Prevention;2009 [updated 2009]. Available at: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed November 23, 2012.
- American Diabetes Association. Economic costs of diabetes in the U.S. In 2007 [published correction appears in Diabetes Care. 2008;31(6):1271.]. Diabetes Care. 2008;31(3):596–615.
- , , , et al.;American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10(1):77–82.
- ACE/ADA Task Force on Inpatient Diabetes. American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control. Endocr Pract. 2006;12(4):458–468.
- , , , et al.;American Association of Clinical Endocrinologists; American Diabetes Association. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32(6):1119–1131.
- ;DIGAMI (Diabetes Mellitus, Insulin Glucose Infusion in Acute Myocardial Infarction) Study Group. Prospective randomised study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus. BMJ. 1997;314(7093):1512–1515.
- , , , et al.;American Diabetes Association Diabetes in Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals [published correction appears in Diabetes Care. 2004;27(5):1255; Diabetes Care. 2004;27(3):856]. Diabetes Care. 2004;27(2):553–591.
- , , , , . Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital. J Hosp Med. 2006;1(3):145–150.
- , , , , ;Society of Hospital Medicine Glycemic Control Task Force. Society of Hospital Medicine Glycemic Control Task Force summary: practical recommendations for assessing the impact of glycemic control efforts. J Hosp Med. 2008;3(5 suppl):66–75.
- , , , , , . Adherence to surgical care improvement project measures and the association with postoperative infections. JAMA. 2010;303(24):2479–2485.
- Glycemic Control Resource Room.Philadelphia, PA:Society of Hospital Medicine;2008. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm. Accessed November 23, 2012.
- Inpatient Glycemic Control Resource Center.Jacksonville, FL:American Association of Clinical Endocrinologists;2011. Available at: http://resources.aace.com. Accessed November 23, 2012.
- , , , et al.;Endocrine Society. Management of hyperglycemia in hospitalized patients in non‐critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(1):16–38.
- Hospital Quality Initiative.Baltimore, MD:Centers for Medicare and Medicaid Services;2012 [updated 2012]. Available at: http://www.cms.gov/HospitalQualityInits/08_HospitalRHQDAPU.asp. Accessed November 23, 2012.
- Hospital‐Acquired Conditions (Present on Admission Indicator).Baltimore, MD:Centers for Medicare and Medicaid Services;2012 [updated 2012]. Available at: http://www.cms.gov/hospitalacqcond/06_hospital‐acquired_conditions.asp. Accessed November 23, 2012.
- , , , et al. Evaluation of hospital glycemic control at US academic medical centers. J Hosp Med. 2009;4(1):35–44.
- , , , . Update on inpatient glycemic control in hospitals in the United States. Endocr Pract. 2011;17(6):853–861.
- , , , , , . Inpatient glucose control: a glycemic survey of 126 U.S. hospitals. J Hosp Med. 2009;4(9):E7–E14.
- , , , , . Inpatient point‐of‐care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control. Diabetes Technol Ther. 2007;9(6):493–500.
- , , , , , . Diabetes and hyperglycemia quality improvement efforts in hospitals in the United States: current status, practice variation, and barriers to implementation. Endocr Pract. 2010;16(2):219–230.
- , , , et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–1367.
- , , , et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449–461.
- , , , et al.;German Competence Network Sepsis (SepNet). Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358(2):125–139.
- , , , et al.;NICE‐SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–1297.
- , , , et al. A prospective randomised multi‐centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med. 2009;35(10):1738–1748.
- , , . Benefits and risks of tight glucose control in critically ill adults: a meta‐analysis [published correction appears in JAMA. 2009;301(9):936]. JAMA. 2008;300(8):933–944.
- , . Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med. 2007;35(10):2262–2267.
- , , , et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA. 2009;301(15):1556–1564.
- , , , et al. Hypoglycemia and outcome in critically ill patients. Mayo Clin Proc. 2010;85(3):217–224.
- , , , . Assessing inpatient glycemic control: what are the next steps?J Diabetes Sci Technol. 2012;6(2):421–427.
Copyright © 2012 Society of Hospital Medicine
Resident Perceptions of Hyperglycemia
Ongoing surveillance indicates that the number of hospitalizations involving patients with a diagnosis of diabetes mellitus is increasing in the United States.1, 2 Hospitalized patients with hyperglycemia have worse outcomes (eg, greater mortality, longer length of stay, and more infections) than those without high glucose levels.3, 4 The rate of adverse outcomes associated with hyperglycemia can be decreased with improved management.3, 4 Consequently, the American Diabetes Association and the American College of Endocrinology advocate lower glucose targets for all hospitalized patients regardless of whether they have a known diagnosis of diabetes.3, 4
Practitioners continue to debate the exact glucose targets that should be attained for inpatients;5, 6 however, there is more to inpatient hyperglycemia management than just trying to achieve a specific glucose range. Caring for patients with diabetes in the hospital is complex and must also encompass patient safety, but many practitioners perceive a state of glycemic chaos in the hospital.7 Because many physicians frequently overlook diabetes and glucose control in the hospital, appropriate therapeutic responses to hyperglycemia do not occur.810 National,11, 12 state,13 and specialty societies3, 4, 14 are working toimprove care for hospitalized patients with hyperglycemia. A recent consensus conference emphasized the need to develop broad‐based educational programs to increase awareness about the importance of inpatient glycemic control and to develop a standardized set of tools for hospitals to use to improve care.4 However, there is ongoing concern about the slow pace at which hospitals are implementing recommendations about glycemic control.4
Intensive and prolonged educational efforts about the importance of glycemic control will be essential ingredients of any quality improvement effort designed to create glycemic order out of glycemic chaos in the hospital.15 Before educational interventions and policies directed at improving the management of hyperglycemia in hospitalized patients can be developed, institutions need to gain a better understanding of how clinicians view the importance of inpatient glucose control and which barriers they perceive as constraints to their ability to care for inpatients with hyperglycemia.
At Atlanta Medical Center (AMC), the large urban teaching hospital where this study was conducted, the glucose control team detected resistance to changes that were implemented to improve the hospital's quality of glycemic control;16 this observation led to a desire to gain more information about practitioner attitudes regarding inpatient glucose control management. Data on practitioner attitudes and beliefs about inpatient hyperglycemia are only now emerging and are limited to studies from a single institution.17, 18 Thus, additional studies are needed to determine whether findings from these first studies are applicable to other types of hospital settings that have different inpatient populations. To gain additional insight into clinician beliefs about inpatient glucose control, we adapted a previously published questionnaire17, 18 and used it to survey resident physicians training at AMC.
METHODS
Setting
AMC is a community teaching hospital located in downtown Atlanta, Georgia, and it is a 460‐bed tertiary care facility. All adult general medical and surgical specialties are represented, in addition to obstetrics and gynecology, a neonatal unit, a level 2 trauma unit, a stroke unit, and an inpatient rehabilitation unit. The inpatient population is mostly minority in mix, with 45% African American, 37% Caucasian, 12% Hispanic, and 6% other races.16, 19 Various types of practitioners provide patient care at AMC, including postgraduate trainees (resident physicians), graduate medical education faculty, physician assistants, and nurse practitioners.
Description of Survey
A previously published survey instrument (the Mayo Clinic Inpatient Diabetes Attitude Survey) was adapted for this project.17, 18 The survey was developed by a team of endocrinologists and primary care physicians with the assistance of our institutional experts in survey design; it was then piloted and submitted to iterative cycles of review and revision.17 The survey was used to assess beliefs first among resident physicians17 and then among midlevel practitioners at the same facility.18 The survey tool was specifically developed to evaluate perceptions of practitioners about inpatient glucose management, including beliefs about the importance of glucose control in the hospital, optimal glucose targets, and barriers to the successful treatment of hyperglycemia. Additionally, the questionnaire was previously used to solicit residents' perceptions about the proportion of their inpatient practices represented by diabetes patients, their beliefs regarding whether patients were achieving their glucose targets, their degree of comfort with managing hyperglycemia and using insulin therapy, and their familiarity with existing institutional policies and preprinted insulin order sets.17, 18 The questionnaire was expanded from its original version to include questions about the use of intravenous insulin.
Survey Participants
As in most academic teaching facilities, at AMC resident physicians treat many of the inpatients who have a diagnosis of diabetes, making the residents an important group to target for educational programs focused on inpatient glucose management. Thus, the audience for this survey included only resident physicians who had ongoing inpatient responsibilities so that the data could be used to assist in educational planning strategies for increasing awareness and improving treatment of inpatients with hyperglycemia. We identified 85 residents who met the inclusion criteria, and we conducted the survey from March to April 2007.
Data Analysis
Written surveys were collected and entered into SurveyTracker version 4.0 (Training Technologies, Inc., Lebanon, Ohio) for analysis. We then examined the distribution of responses to individual questions. Finally, we listed the frequency of expressed barriers to inpatient glucose management from most common to least common.
RESULTS
Respondent Demographics
Sixty‐six of 85 residents (78%) responded to the survey. The mean age of the respondents was 31 years, 47% were men, 33% were in their first year of residency training, and 73% had graduated from medical school during the year 2002 or later. The residents represented the following departments: 41% from internal medicine (n = 27), 18% from family medicine (n = 12), 15% from general surgery (n = 10), 12% from orthopedics (n = 8), and 14% from obstetrics and gynecology (n = 9).
Perceptions About Inpatient Burden of Diabetes
When asked to estimate the percentage of their hospitalized patients who were considered to have a diagnosis of diabetes or hyperglycemia, 14% of the residents indicated that 0% to 20% of their hospitalized patients were in this category, 30% of the residents estimated that 21% to 40% of their inpatients were in this group, and 25% of the residents believed that such a diagnosis applied to 41% to 60% of their inpatients. Additionally, 23% of the residents said that 61% to 80% of their inpatients were considered to have a diagnosis of diabetes or hyperglycemia, 3% of the residents estimated that 81% to 100% of their hospitalized patients had such a diagnosis, and 5% of the residents were unsure. Thus, respondents perceived that diabetes constituted a substantial portion of their inpatient practices, with 50% of the residents estimating that more than 40% of their hospitalized patients had a diagnosis of diabetes or hyperglycemia and nearly 25% of responding residents believing that more than 60% of their inpatients had the same diagnosis.
Views on the Importance of Glycemic Control
Most resident physicians believed that good glycemic control was important in hospitalized patients (Table 1); 97% believed that it was very important to have tight glycemic control in critically‐ill patients, 72% emphasized that it was very important in non‐critically‐ill patients, and 85% indicated that it was very important during the perioperative period. Nearly all residents believed that it was important to achieve good glycemic control in pregnant patients (Table 1).
| ||||
| Category | Response | |||
| Importance of Treating Hyperglycemia | Very Important | Somewhat Important | Not at All Important | Don't Know |
| Critically ill patients | 97 | 3 | 0 | 0 |
| Non‐critically‐ill patients | 72 | 26 | 2 | 0 |
| Perioperative patients | 85 | 15 | 0 | 0 |
| Pregnant patients | 97 | 3 | 0 | 0 |
| Comfort Level | Very Comfortable | Somewhat Comfortable | Not at All Comfortable | Don't Know |
| Treating hyperglycemia | 42 | 47 | 11 | 0 |
| Treating hypoglycemia | 49 | 44 | 6 | 1 |
| Using subcutaneous insulin | 44 | 44 | 11 | 1 |
| Using insulin drips | 38 | 42 | 18 | 2 |
| Using insulin pumps* | 14 | 17 | 58 | 12 |
| Familiarity | Very Familiar | Somewhat Familiar | Not at All Familiar | Unaware of Policy |
| Insulin pump policy | 9 | 15 | 52 | 24 |
| Insulin pump orders | 6 | 17 | 54 | 23 |
| Hypoglycemia policy | 23 | 45 | 17 | 15 |
| Subcutaneous insulin orders | 34 | 35 | 14 | 17 |
| Intravenous insulin orders | 38 | 33 | 21 | 8 |
| Glucose Goal, mg/dL | 80‐110 | 111‐180 | 181‐250 | Don't Know |
| Critically ill patients | 91 | 6 | 2 | 1 |
| Non‐critically‐ill patients | 53 | 46 | 0 | 1 |
| Perioperative patients | 76 | 23 | 0 | 1 |
| Glucose Level for Initiation of IV Insulin, mg/dL | >110 | >140 | >180 | Don't Know |
| Critically ill patients | 8 | 30 | 51 | 11 |
| Non‐critically‐ill patients | 1 | 6 | 65 | 28 |
| Pregnant patients | 8 | 27 | 30 | 35 |
Comfort With Treatment and Management
Survey participants were asked how comfortable they felt about different scenarios pertaining to inpatient glucose management (Table 1). Although more than 40% of respondents indicated that they felt very comfortable treating hyperglycemia and hypoglycemia in the hospital, a large proportion (50% or more) also indicated that they were only somewhat comfortable or not at all comfortable treating these conditions. Similarly, in response to questions about their degree of comfort working with subcutaneous or intravenous insulin, more than 50% of trainees were only somewhat comfortable or not at all comfortable. Finally, most were not at all comfortable with the use of insulin pumps in the hospital (Table 1).
Familiarity With Existing Policies and Procedures
Most of the trainees indicated that they were not at all familiar with existing hospital policies and orders pertaining to insulin pumps (Table 1). Most respondents were only somewhat familiar with the institutional hypoglycemia policy, but a substantial percentage (32%) were either not at all familiar or even unaware that an institutional hypoglycemia policy existed. Similarly, most were only somewhat familiar, not at all familiar, or even unaware of orders or policies pertaining to use of subcutaneous or intravenous insulin (Table 1).
Beliefs About Glucose Targets and Hypoglycemia
When asked to indicate the target glucose levels that they would like to achieve, most resident physicians indicated that good glycemic control meant a target range of 80 to 110 mg/dL for critically‐ill patients and for perioperative patients. For non‐critically‐ill patients, targets were split between a target range of 80 to 110 mg/dL and 111 to 180 mg/dL. Trainees rarely suggested targets greater than 180 mg/dL (Table 1).
Most respondents believed that they were achieving their glycemic goals in 41% to 60% of their patients (Fig. 1A). More than half (56%) perceived that they were achieving their glucose targets in more than 40% of their diabetes patients. When asked at what glucose level they first considered the patient to be hypoglycemic, half of the respondents chose <60 mg/dL (Fig. 1B), although some had even lower cutoffs before they considered someone to have a diagnosis of hypoglycemia.

Thresholds for Starting Intravenous Insulin
For both critically‐ill and non‐critically‐ill patients, most resident physicians indicated that they would wait until the glucose level was greater than 180 mg/dL before starting an insulin infusion (Table 1). Likewise, obstetrics residents identified a glucose level greater than 180 mg/dL as a threshold to start intravenous insulin in pregnant patients.
Perceived Barriers to Care
The survey concluded with a question that asked resident physicians to choose from a list of factors they perceived as obstacles to inpatient glucose management. The 5 most frequently chosen obstacles, from most common to least common, were as follows: knowing what insulin type or regimen works best, fluctuating insulin demands related to stress and risk of causing patient hypoglycemia (cited with equal frequency), unpredictable changes in patient diet and meal times, and unpredictable timing of patient procedures (Table 2).
| Barrier | Response, Number (%) (n = 66) |
|---|---|
| |
| Knowing what insulin type or regimen works best | 26 (39) |
| Fluctuating insulin demands related to stress/concomitantly used medications | 26 (39) |
| Risk of causing hypoglycemia | 25 (38) |
| Unpredictable changes in patient diet and mealtimes | 25 (38) |
| Unpredictable timing of patient procedures | 19 (29) |
| Patient not in hospital long enough to control glucose adequately | 18 (27) |
| Shift changes and cross‐coverage lead to inconsistent management | 18 (27) |
| Knowing best options to treat hyperglycemia | 16 (24) |
| Knowing when to start insulin | 14 (21) |
| Knowing how to adjust insulin | 14 (21) |
| Conversion between different forms of insulin | 13 (20) |
| Lack of guidelines on how to treat hyperglycemia | 11 (17) |
| Preferring to defer management to outpatient care or to another specialty | 10 (15) |
| Knowing how to start insulin | 10 (15) |
| Knowing how to best prevent hypoglycemia | 7 (11) |
| None, I have no trouble treating hyperglycemia in the hospital | 7 (11) |
| Glucose management not adequately addressed on rounds | 6 (9) |
| Treating hyperglycemia is not a priority in the hospital | 6 (9) |
| Other* | 4 (6) |
| Disagreement with other team members on how to control glucose | 3 (5) |
DISCUSSION
In recent years national and regional organizations have focused greater attention on the management of hyperglycemia among inpatient populations by introducing and promoting guidelines for better care.3, 4, 1114 A consensus conference in 2006 urged hospitals to move rapidly to make euglycemia a goal for all inpatients and to make patient safety in glycemic control a reality. 20 AMC has already taken some steps toward understanding and improving its hospital‐based care of hyperglycemia, including understanding the mortality associated with hyperglycemia within the institution and implementing a novel insulin infusion algorithm.16, 19
Before hospitals can develop high‐quality improvement and educational programs focused on inpatient hyperglycemia, they will need more insight into their clinicians' views on inpatient glycemic control and the perceived barriers to successful treatment of hyperglycemia. However, the only data that have been published about practitioner attitudes on inpatient diabetes and glycemic control are from a single institution.17, 18 Thus, analyses should be broadened to include different types of hospital settings to determine common beliefs on the topic.
AMC is very different from the hospital facility where earlier studies on physician attitudes about inpatient glucose management were conducted. Whereas the site of the earlier studies is located in the Southwest and has a diabetes inpatient population that is primarily white, AMC is an urban hospital in the Southeast whose diabetes inpatient population is primarily minority.21 Despite the institutional, geographic, and patient population differences, however, results of the current survey suggest that there may be similar beliefs among practitioners about inpatient glucose management as well as common knowledge deficits that can be targeted for educational interventions.
Similar to the resident physicians surveyed in previous studies,17, 18 AMC resident physicians considered diabetes to be a substantial part of their inpatient practices: 56% of respondents believed that more than 40% of their inpatients had a diagnosis of diabetes. Historically, the prevalence at AMC of hyperglycemia has been about 38% and the prevalence of diabetes about 26%.19 The increasing number of hospital dismissals attributable to diabetes likely has increased the inpatient prevalence of the disease at AMC as well, but very high rates perceived by some residents (eg, 81%‐100%) are likely not accurate. Nonetheless, this perception of such a large burden of diabetes clearly substantiates the need to provide pertinent information and essential tools to clinicians for successful management of hyperglycemia in hospital patients. We also established that most AMC resident physicians who were surveyed believed that good glucose control was very important in situations relating to critical illness or noncritical illness. For most respondents, good glucose control was also very important in the perioperative period. This finding suggests that the trainees understand the importance of good glucose control in such situations.
In keeping with findings from previous studies,17, 18 respondents to this survey indicated glucose targets that would be well within currently existing guidelines.3, 4 Glucose management training might be improved by conveying whether actual glucose outcomes match residents' perceived achievement of glycemic control.
Insulin is the recommended treatment for inpatient hyperglycemia,3, 4 yet residents' responses reflected concern about insulin use. The most commonly noted issues, cited with equal frequency, were related to insulin use: knowing what insulin type or regimen works best and fluctuating insulin demands related to stress/concomitantly used medications. Our survey did not evaluate whether residents had different degrees of comfort with different subcutaneous insulin programs (eg, sliding scale versus basal‐bolus). Future surveys could be modified to better hone in on evaluating self‐perceived competencies in these areas.
Given the increasing complexity of insulin therapy, resident physicians' perception of insulin administration as the top barrier to inpatient glucose management may not be surprising.17, 18 The number of insulin analogs has increased in recent years. Moreover, numerous intravenous insulin algorithms are available.22, 23 Errors in insulin administration are among the most frequently occurring medication errors in hospitals.24 To address patient safety and medical system errors in the fields of diabetes and endocrinology, the American College of Endocrinology published a position statement on the topic in 2005.25 Guidelines about when to initiate insulin therapy, how to choose from numerous insulin treatment options, and how to adjust therapy in response to rapidly changing clinical situations will have to be integrated into any effort to improve inpatient glucose management. One study indicated that an educational process focused on teaching residents about insulin therapy can be successful.26
Clinician fear of hypoglycemia is often perceived as the primary obstacle to successful control of inpatient glucose levels;3, 27 however, this was not the chief concern expressed by either AMC resident physicians or by practitioners surveyed in prior studies.17, 18 Emerging data suggest that hypoglycemia in the hospital is actually uncommon.21, 28 As hospitals intensify hyperglycemia management efforts, hypoglycemia and concerns about its frequency of occurrence will most likely increase. No consensus exists regarding the number of hypoglycemic events that are acceptable in a hospitalized patient. The American Diabetes Association Workgroup on Hypoglycemia has defined hypoglycemia as an (arterialized venous) plasma glucose concentration of less than or equal to 70 mg/dL.29 As a group, residents surveyed for the current study were not consistent in their definition of hypoglycemia.
The residents at AMC also reported potential obstacles to care besides insulin management that suggest system‐based problems. Unpredictable timing of patient procedures and unpredictable changes in patient diet and mealtimes were among the 5 most frequently cited concerns. Other concerns included patient not in hospital long enough to adequately control glucose and shift changes and cross‐coverage lead to inconsistent management. These findings are identical to those of prior studies17, 18 and suggest system‐based problems as common barriers to inpatient glucose management. Some of these obstacles, such as length of hospital stay and timing of procedures, would be difficult to reengineer. However, other aspects, such as adjusting therapy to mealtimes and ensuring standardization of treatment across shifts, could be addressed through institution‐wide education and changes in policies.
As in previous studies, another major finding that emerged from this survey was the lack of resident physician familiarity with existing policies and procedures related to inpatient glucose management. AMC has a longstanding policy on hypoglycemia management and has preprinted order sets for subcutaneous insulin. AMC has implemented a revised insulin infusion algorithm16 in addition to a policy and an order set for the use of insulin pumps.30 There are no specific data on how many patients receiving insulin pump therapy are hospitalized, but these patients are likely to be encountered only rarely in the hospital setting. Hence, it may not be surprising that residents are unfamiliar with policies pertaining to inpatient insulin pump use, but they should at least be aware that guidance is available. One of the first steps to enhancing and standardizing hospital glucose management may simply be to make certain that clinicians are familiar with policies that are already in place within the institution.
A limitation of this study is the small sample size. The results of the present study should not be extrapolated to nonresident medical staff such as attending physicians, but the questionnaire could be adapted, with minor modifications, to investigate how other health care professionals view inpatient glucose management. In addition, the questionnaire could be used to assess changes in beliefs over time. Future studies should be designed to correlate resident perceptions about their inpatient diabetes care and actual practice patterns.
More surveys such as the one reported on here need to be conducted in additional institutions in order to expand our understanding of practitioner attitudes regarding inpatient diabetes care. Data from the current study and previous ones suggest that practitioners share beliefs, knowledge deficits, and perceived barriers about inpatient glucose management. Most AMC resident physicians recognized the importance of good glucose control and set target glucose ranges consistent with existing guidelines. Knowledge deficits may be addressed by developing training programs that specifically spotlight insulin use in the hospital. As a first step to quality improvement, training programs should focus on familiarizing staff with existing institutional policies and procedures pertaining to hospital hyperglycemia. In addition, hospitals need to design strategies to overcome perceived and actual barriers to care so that they can realize the desired improvement in the management of hyperglycemia in their patients. We have already begun the development and implementation of educational modules directed at addressing many of these important issues.
- Centers for Disease Control and Prevention. Hospitalization for diabetes as first‐listed diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmfirst/index.htm. Accessed October2008.
- Centers for Disease Control and Prevention. Hospitalizations for diabetes as any‐listed diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmany/index.htm. Accessed October2008.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ACE/ADA Task Force on Inpatient Diabetes.American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control.Endocr Pract.2006;12:458–468.
- ,.Counterpoint: inpatient glucose management: a premature call to arms?Diabetes Care.2005;28:976–979.
- ,.Point: inpatient glucose management: the emperor finally has clothes.Diabetes Care.2005;28:973–975.
- ,.Glycemic chaos (not glycemic control) still the rule for inpatient care: how do we stop the insanity? [Editorial]J Hosp Med.2006;1:141–144.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,, et al.Diabetes care in the hospital: is there clinical inertia?J Hosp Med.2006;1:151–160.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1:145–150.
- The Joint Commission. Inpatient diabetes. Available at: http://www.jointcommission.org/CertificationPrograms/Inpatient+Diabetes. Accessed October2008.
- Institute for Healthcare Improvement. Implement effective glucose control. Available at: http://www.ihi.org/IHI/Topics/CriticalCare/IntensiveCare/Changes/ImplementEffectiveGlucoseControl.htm. Accessed October2008.
- ,,, et al.;the Georgia Hospital Association Diabetes Special Interest Group. Working to improve care of hospital hyperglycemia through statewide collaboration.Endocr Pract.2007;13:45–50.
- Society of Hospital Medicine. Glycemic control resource room. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Search_Advanced_Search1:383–385.
- ,,, et al.Improving hyperglycemia management in the intensive care unit: preliminary report of a nurse‐driven quality improvement project using a redesigned insulin infusion algorithm.Diabetes Educ.2006;32:394–403.
- ,,, et al.Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians.Endocr Pract.2007;13:117–124.
- ,,, et al.Beliefs about hospital diabetes and perceived barriers to glucose management among inpatient midlevel practitioners.Diabetes Educ.2008;34:75–83.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- .Patient safety and inpatient glycemic control: translating concepts into action.Endocr Pract.2006;12 (Suppl 3):49–55.
- ,,, et al.Diabetes care in hospitalized noncritically ill patients: more evidence for clinical inertia and negative therapeutic momentum.J Hosp Med.2007;2:203–211.
- ,,.Insulin infusion protocols for critically ill patients: a highlight of differences and similarities.Endocr Pract.2007;13:137–146.
- ,,.Intensive insulin therapy in critical care: a review of 12 protocols.Diabetes Care.2007;30:1005–1011.
- Institute for Safe Medication Practices. ISMP's list of high‐alert medications. Available at: http://www.ismp.org/Tools/highalertmedications.pdf. Accessed October2008.
- American Association of Clinical Endocrinologists. Patient safety and medical system errors in diabetes and endocrinology consensus conference: position statement. Available at: http://www.aace.com/pub/pdf/guidelines/PatientSafetyPositionStatement.pdf. Accessed October2008.
- ,,,.Eliminating inpatient sliding‐scale insulin: a reeducation project with medical house staff.Diabetes Care.2005;28:1008–1011.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10 (Suppl 2):89–99.
- ,,,,.Inpatient point‐of‐care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control.Diabetes Technol Ther.2007;9:493–500.
- Workgroup on Hypoglycemia, American Diabetes Association.Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia.Diabetes Care.2005;28:1245–1249.
- ,,, et al.Use of continuous subcutaneous insulin infusion (insulin pump) therapy in the hospital setting: proposed guidelines and outcome measures.Diabetes Educ.2005;31:849–857.
Ongoing surveillance indicates that the number of hospitalizations involving patients with a diagnosis of diabetes mellitus is increasing in the United States.1, 2 Hospitalized patients with hyperglycemia have worse outcomes (eg, greater mortality, longer length of stay, and more infections) than those without high glucose levels.3, 4 The rate of adverse outcomes associated with hyperglycemia can be decreased with improved management.3, 4 Consequently, the American Diabetes Association and the American College of Endocrinology advocate lower glucose targets for all hospitalized patients regardless of whether they have a known diagnosis of diabetes.3, 4
Practitioners continue to debate the exact glucose targets that should be attained for inpatients;5, 6 however, there is more to inpatient hyperglycemia management than just trying to achieve a specific glucose range. Caring for patients with diabetes in the hospital is complex and must also encompass patient safety, but many practitioners perceive a state of glycemic chaos in the hospital.7 Because many physicians frequently overlook diabetes and glucose control in the hospital, appropriate therapeutic responses to hyperglycemia do not occur.810 National,11, 12 state,13 and specialty societies3, 4, 14 are working toimprove care for hospitalized patients with hyperglycemia. A recent consensus conference emphasized the need to develop broad‐based educational programs to increase awareness about the importance of inpatient glycemic control and to develop a standardized set of tools for hospitals to use to improve care.4 However, there is ongoing concern about the slow pace at which hospitals are implementing recommendations about glycemic control.4
Intensive and prolonged educational efforts about the importance of glycemic control will be essential ingredients of any quality improvement effort designed to create glycemic order out of glycemic chaos in the hospital.15 Before educational interventions and policies directed at improving the management of hyperglycemia in hospitalized patients can be developed, institutions need to gain a better understanding of how clinicians view the importance of inpatient glucose control and which barriers they perceive as constraints to their ability to care for inpatients with hyperglycemia.
At Atlanta Medical Center (AMC), the large urban teaching hospital where this study was conducted, the glucose control team detected resistance to changes that were implemented to improve the hospital's quality of glycemic control;16 this observation led to a desire to gain more information about practitioner attitudes regarding inpatient glucose control management. Data on practitioner attitudes and beliefs about inpatient hyperglycemia are only now emerging and are limited to studies from a single institution.17, 18 Thus, additional studies are needed to determine whether findings from these first studies are applicable to other types of hospital settings that have different inpatient populations. To gain additional insight into clinician beliefs about inpatient glucose control, we adapted a previously published questionnaire17, 18 and used it to survey resident physicians training at AMC.
METHODS
Setting
AMC is a community teaching hospital located in downtown Atlanta, Georgia, and it is a 460‐bed tertiary care facility. All adult general medical and surgical specialties are represented, in addition to obstetrics and gynecology, a neonatal unit, a level 2 trauma unit, a stroke unit, and an inpatient rehabilitation unit. The inpatient population is mostly minority in mix, with 45% African American, 37% Caucasian, 12% Hispanic, and 6% other races.16, 19 Various types of practitioners provide patient care at AMC, including postgraduate trainees (resident physicians), graduate medical education faculty, physician assistants, and nurse practitioners.
Description of Survey
A previously published survey instrument (the Mayo Clinic Inpatient Diabetes Attitude Survey) was adapted for this project.17, 18 The survey was developed by a team of endocrinologists and primary care physicians with the assistance of our institutional experts in survey design; it was then piloted and submitted to iterative cycles of review and revision.17 The survey was used to assess beliefs first among resident physicians17 and then among midlevel practitioners at the same facility.18 The survey tool was specifically developed to evaluate perceptions of practitioners about inpatient glucose management, including beliefs about the importance of glucose control in the hospital, optimal glucose targets, and barriers to the successful treatment of hyperglycemia. Additionally, the questionnaire was previously used to solicit residents' perceptions about the proportion of their inpatient practices represented by diabetes patients, their beliefs regarding whether patients were achieving their glucose targets, their degree of comfort with managing hyperglycemia and using insulin therapy, and their familiarity with existing institutional policies and preprinted insulin order sets.17, 18 The questionnaire was expanded from its original version to include questions about the use of intravenous insulin.
Survey Participants
As in most academic teaching facilities, at AMC resident physicians treat many of the inpatients who have a diagnosis of diabetes, making the residents an important group to target for educational programs focused on inpatient glucose management. Thus, the audience for this survey included only resident physicians who had ongoing inpatient responsibilities so that the data could be used to assist in educational planning strategies for increasing awareness and improving treatment of inpatients with hyperglycemia. We identified 85 residents who met the inclusion criteria, and we conducted the survey from March to April 2007.
Data Analysis
Written surveys were collected and entered into SurveyTracker version 4.0 (Training Technologies, Inc., Lebanon, Ohio) for analysis. We then examined the distribution of responses to individual questions. Finally, we listed the frequency of expressed barriers to inpatient glucose management from most common to least common.
RESULTS
Respondent Demographics
Sixty‐six of 85 residents (78%) responded to the survey. The mean age of the respondents was 31 years, 47% were men, 33% were in their first year of residency training, and 73% had graduated from medical school during the year 2002 or later. The residents represented the following departments: 41% from internal medicine (n = 27), 18% from family medicine (n = 12), 15% from general surgery (n = 10), 12% from orthopedics (n = 8), and 14% from obstetrics and gynecology (n = 9).
Perceptions About Inpatient Burden of Diabetes
When asked to estimate the percentage of their hospitalized patients who were considered to have a diagnosis of diabetes or hyperglycemia, 14% of the residents indicated that 0% to 20% of their hospitalized patients were in this category, 30% of the residents estimated that 21% to 40% of their inpatients were in this group, and 25% of the residents believed that such a diagnosis applied to 41% to 60% of their inpatients. Additionally, 23% of the residents said that 61% to 80% of their inpatients were considered to have a diagnosis of diabetes or hyperglycemia, 3% of the residents estimated that 81% to 100% of their hospitalized patients had such a diagnosis, and 5% of the residents were unsure. Thus, respondents perceived that diabetes constituted a substantial portion of their inpatient practices, with 50% of the residents estimating that more than 40% of their hospitalized patients had a diagnosis of diabetes or hyperglycemia and nearly 25% of responding residents believing that more than 60% of their inpatients had the same diagnosis.
Views on the Importance of Glycemic Control
Most resident physicians believed that good glycemic control was important in hospitalized patients (Table 1); 97% believed that it was very important to have tight glycemic control in critically‐ill patients, 72% emphasized that it was very important in non‐critically‐ill patients, and 85% indicated that it was very important during the perioperative period. Nearly all residents believed that it was important to achieve good glycemic control in pregnant patients (Table 1).
| ||||
| Category | Response | |||
| Importance of Treating Hyperglycemia | Very Important | Somewhat Important | Not at All Important | Don't Know |
| Critically ill patients | 97 | 3 | 0 | 0 |
| Non‐critically‐ill patients | 72 | 26 | 2 | 0 |
| Perioperative patients | 85 | 15 | 0 | 0 |
| Pregnant patients | 97 | 3 | 0 | 0 |
| Comfort Level | Very Comfortable | Somewhat Comfortable | Not at All Comfortable | Don't Know |
| Treating hyperglycemia | 42 | 47 | 11 | 0 |
| Treating hypoglycemia | 49 | 44 | 6 | 1 |
| Using subcutaneous insulin | 44 | 44 | 11 | 1 |
| Using insulin drips | 38 | 42 | 18 | 2 |
| Using insulin pumps* | 14 | 17 | 58 | 12 |
| Familiarity | Very Familiar | Somewhat Familiar | Not at All Familiar | Unaware of Policy |
| Insulin pump policy | 9 | 15 | 52 | 24 |
| Insulin pump orders | 6 | 17 | 54 | 23 |
| Hypoglycemia policy | 23 | 45 | 17 | 15 |
| Subcutaneous insulin orders | 34 | 35 | 14 | 17 |
| Intravenous insulin orders | 38 | 33 | 21 | 8 |
| Glucose Goal, mg/dL | 80‐110 | 111‐180 | 181‐250 | Don't Know |
| Critically ill patients | 91 | 6 | 2 | 1 |
| Non‐critically‐ill patients | 53 | 46 | 0 | 1 |
| Perioperative patients | 76 | 23 | 0 | 1 |
| Glucose Level for Initiation of IV Insulin, mg/dL | >110 | >140 | >180 | Don't Know |
| Critically ill patients | 8 | 30 | 51 | 11 |
| Non‐critically‐ill patients | 1 | 6 | 65 | 28 |
| Pregnant patients | 8 | 27 | 30 | 35 |
Comfort With Treatment and Management
Survey participants were asked how comfortable they felt about different scenarios pertaining to inpatient glucose management (Table 1). Although more than 40% of respondents indicated that they felt very comfortable treating hyperglycemia and hypoglycemia in the hospital, a large proportion (50% or more) also indicated that they were only somewhat comfortable or not at all comfortable treating these conditions. Similarly, in response to questions about their degree of comfort working with subcutaneous or intravenous insulin, more than 50% of trainees were only somewhat comfortable or not at all comfortable. Finally, most were not at all comfortable with the use of insulin pumps in the hospital (Table 1).
Familiarity With Existing Policies and Procedures
Most of the trainees indicated that they were not at all familiar with existing hospital policies and orders pertaining to insulin pumps (Table 1). Most respondents were only somewhat familiar with the institutional hypoglycemia policy, but a substantial percentage (32%) were either not at all familiar or even unaware that an institutional hypoglycemia policy existed. Similarly, most were only somewhat familiar, not at all familiar, or even unaware of orders or policies pertaining to use of subcutaneous or intravenous insulin (Table 1).
Beliefs About Glucose Targets and Hypoglycemia
When asked to indicate the target glucose levels that they would like to achieve, most resident physicians indicated that good glycemic control meant a target range of 80 to 110 mg/dL for critically‐ill patients and for perioperative patients. For non‐critically‐ill patients, targets were split between a target range of 80 to 110 mg/dL and 111 to 180 mg/dL. Trainees rarely suggested targets greater than 180 mg/dL (Table 1).
Most respondents believed that they were achieving their glycemic goals in 41% to 60% of their patients (Fig. 1A). More than half (56%) perceived that they were achieving their glucose targets in more than 40% of their diabetes patients. When asked at what glucose level they first considered the patient to be hypoglycemic, half of the respondents chose <60 mg/dL (Fig. 1B), although some had even lower cutoffs before they considered someone to have a diagnosis of hypoglycemia.

Thresholds for Starting Intravenous Insulin
For both critically‐ill and non‐critically‐ill patients, most resident physicians indicated that they would wait until the glucose level was greater than 180 mg/dL before starting an insulin infusion (Table 1). Likewise, obstetrics residents identified a glucose level greater than 180 mg/dL as a threshold to start intravenous insulin in pregnant patients.
Perceived Barriers to Care
The survey concluded with a question that asked resident physicians to choose from a list of factors they perceived as obstacles to inpatient glucose management. The 5 most frequently chosen obstacles, from most common to least common, were as follows: knowing what insulin type or regimen works best, fluctuating insulin demands related to stress and risk of causing patient hypoglycemia (cited with equal frequency), unpredictable changes in patient diet and meal times, and unpredictable timing of patient procedures (Table 2).
| Barrier | Response, Number (%) (n = 66) |
|---|---|
| |
| Knowing what insulin type or regimen works best | 26 (39) |
| Fluctuating insulin demands related to stress/concomitantly used medications | 26 (39) |
| Risk of causing hypoglycemia | 25 (38) |
| Unpredictable changes in patient diet and mealtimes | 25 (38) |
| Unpredictable timing of patient procedures | 19 (29) |
| Patient not in hospital long enough to control glucose adequately | 18 (27) |
| Shift changes and cross‐coverage lead to inconsistent management | 18 (27) |
| Knowing best options to treat hyperglycemia | 16 (24) |
| Knowing when to start insulin | 14 (21) |
| Knowing how to adjust insulin | 14 (21) |
| Conversion between different forms of insulin | 13 (20) |
| Lack of guidelines on how to treat hyperglycemia | 11 (17) |
| Preferring to defer management to outpatient care or to another specialty | 10 (15) |
| Knowing how to start insulin | 10 (15) |
| Knowing how to best prevent hypoglycemia | 7 (11) |
| None, I have no trouble treating hyperglycemia in the hospital | 7 (11) |
| Glucose management not adequately addressed on rounds | 6 (9) |
| Treating hyperglycemia is not a priority in the hospital | 6 (9) |
| Other* | 4 (6) |
| Disagreement with other team members on how to control glucose | 3 (5) |
DISCUSSION
In recent years national and regional organizations have focused greater attention on the management of hyperglycemia among inpatient populations by introducing and promoting guidelines for better care.3, 4, 1114 A consensus conference in 2006 urged hospitals to move rapidly to make euglycemia a goal for all inpatients and to make patient safety in glycemic control a reality. 20 AMC has already taken some steps toward understanding and improving its hospital‐based care of hyperglycemia, including understanding the mortality associated with hyperglycemia within the institution and implementing a novel insulin infusion algorithm.16, 19
Before hospitals can develop high‐quality improvement and educational programs focused on inpatient hyperglycemia, they will need more insight into their clinicians' views on inpatient glycemic control and the perceived barriers to successful treatment of hyperglycemia. However, the only data that have been published about practitioner attitudes on inpatient diabetes and glycemic control are from a single institution.17, 18 Thus, analyses should be broadened to include different types of hospital settings to determine common beliefs on the topic.
AMC is very different from the hospital facility where earlier studies on physician attitudes about inpatient glucose management were conducted. Whereas the site of the earlier studies is located in the Southwest and has a diabetes inpatient population that is primarily white, AMC is an urban hospital in the Southeast whose diabetes inpatient population is primarily minority.21 Despite the institutional, geographic, and patient population differences, however, results of the current survey suggest that there may be similar beliefs among practitioners about inpatient glucose management as well as common knowledge deficits that can be targeted for educational interventions.
Similar to the resident physicians surveyed in previous studies,17, 18 AMC resident physicians considered diabetes to be a substantial part of their inpatient practices: 56% of respondents believed that more than 40% of their inpatients had a diagnosis of diabetes. Historically, the prevalence at AMC of hyperglycemia has been about 38% and the prevalence of diabetes about 26%.19 The increasing number of hospital dismissals attributable to diabetes likely has increased the inpatient prevalence of the disease at AMC as well, but very high rates perceived by some residents (eg, 81%‐100%) are likely not accurate. Nonetheless, this perception of such a large burden of diabetes clearly substantiates the need to provide pertinent information and essential tools to clinicians for successful management of hyperglycemia in hospital patients. We also established that most AMC resident physicians who were surveyed believed that good glucose control was very important in situations relating to critical illness or noncritical illness. For most respondents, good glucose control was also very important in the perioperative period. This finding suggests that the trainees understand the importance of good glucose control in such situations.
In keeping with findings from previous studies,17, 18 respondents to this survey indicated glucose targets that would be well within currently existing guidelines.3, 4 Glucose management training might be improved by conveying whether actual glucose outcomes match residents' perceived achievement of glycemic control.
Insulin is the recommended treatment for inpatient hyperglycemia,3, 4 yet residents' responses reflected concern about insulin use. The most commonly noted issues, cited with equal frequency, were related to insulin use: knowing what insulin type or regimen works best and fluctuating insulin demands related to stress/concomitantly used medications. Our survey did not evaluate whether residents had different degrees of comfort with different subcutaneous insulin programs (eg, sliding scale versus basal‐bolus). Future surveys could be modified to better hone in on evaluating self‐perceived competencies in these areas.
Given the increasing complexity of insulin therapy, resident physicians' perception of insulin administration as the top barrier to inpatient glucose management may not be surprising.17, 18 The number of insulin analogs has increased in recent years. Moreover, numerous intravenous insulin algorithms are available.22, 23 Errors in insulin administration are among the most frequently occurring medication errors in hospitals.24 To address patient safety and medical system errors in the fields of diabetes and endocrinology, the American College of Endocrinology published a position statement on the topic in 2005.25 Guidelines about when to initiate insulin therapy, how to choose from numerous insulin treatment options, and how to adjust therapy in response to rapidly changing clinical situations will have to be integrated into any effort to improve inpatient glucose management. One study indicated that an educational process focused on teaching residents about insulin therapy can be successful.26
Clinician fear of hypoglycemia is often perceived as the primary obstacle to successful control of inpatient glucose levels;3, 27 however, this was not the chief concern expressed by either AMC resident physicians or by practitioners surveyed in prior studies.17, 18 Emerging data suggest that hypoglycemia in the hospital is actually uncommon.21, 28 As hospitals intensify hyperglycemia management efforts, hypoglycemia and concerns about its frequency of occurrence will most likely increase. No consensus exists regarding the number of hypoglycemic events that are acceptable in a hospitalized patient. The American Diabetes Association Workgroup on Hypoglycemia has defined hypoglycemia as an (arterialized venous) plasma glucose concentration of less than or equal to 70 mg/dL.29 As a group, residents surveyed for the current study were not consistent in their definition of hypoglycemia.
The residents at AMC also reported potential obstacles to care besides insulin management that suggest system‐based problems. Unpredictable timing of patient procedures and unpredictable changes in patient diet and mealtimes were among the 5 most frequently cited concerns. Other concerns included patient not in hospital long enough to adequately control glucose and shift changes and cross‐coverage lead to inconsistent management. These findings are identical to those of prior studies17, 18 and suggest system‐based problems as common barriers to inpatient glucose management. Some of these obstacles, such as length of hospital stay and timing of procedures, would be difficult to reengineer. However, other aspects, such as adjusting therapy to mealtimes and ensuring standardization of treatment across shifts, could be addressed through institution‐wide education and changes in policies.
As in previous studies, another major finding that emerged from this survey was the lack of resident physician familiarity with existing policies and procedures related to inpatient glucose management. AMC has a longstanding policy on hypoglycemia management and has preprinted order sets for subcutaneous insulin. AMC has implemented a revised insulin infusion algorithm16 in addition to a policy and an order set for the use of insulin pumps.30 There are no specific data on how many patients receiving insulin pump therapy are hospitalized, but these patients are likely to be encountered only rarely in the hospital setting. Hence, it may not be surprising that residents are unfamiliar with policies pertaining to inpatient insulin pump use, but they should at least be aware that guidance is available. One of the first steps to enhancing and standardizing hospital glucose management may simply be to make certain that clinicians are familiar with policies that are already in place within the institution.
A limitation of this study is the small sample size. The results of the present study should not be extrapolated to nonresident medical staff such as attending physicians, but the questionnaire could be adapted, with minor modifications, to investigate how other health care professionals view inpatient glucose management. In addition, the questionnaire could be used to assess changes in beliefs over time. Future studies should be designed to correlate resident perceptions about their inpatient diabetes care and actual practice patterns.
More surveys such as the one reported on here need to be conducted in additional institutions in order to expand our understanding of practitioner attitudes regarding inpatient diabetes care. Data from the current study and previous ones suggest that practitioners share beliefs, knowledge deficits, and perceived barriers about inpatient glucose management. Most AMC resident physicians recognized the importance of good glucose control and set target glucose ranges consistent with existing guidelines. Knowledge deficits may be addressed by developing training programs that specifically spotlight insulin use in the hospital. As a first step to quality improvement, training programs should focus on familiarizing staff with existing institutional policies and procedures pertaining to hospital hyperglycemia. In addition, hospitals need to design strategies to overcome perceived and actual barriers to care so that they can realize the desired improvement in the management of hyperglycemia in their patients. We have already begun the development and implementation of educational modules directed at addressing many of these important issues.
Ongoing surveillance indicates that the number of hospitalizations involving patients with a diagnosis of diabetes mellitus is increasing in the United States.1, 2 Hospitalized patients with hyperglycemia have worse outcomes (eg, greater mortality, longer length of stay, and more infections) than those without high glucose levels.3, 4 The rate of adverse outcomes associated with hyperglycemia can be decreased with improved management.3, 4 Consequently, the American Diabetes Association and the American College of Endocrinology advocate lower glucose targets for all hospitalized patients regardless of whether they have a known diagnosis of diabetes.3, 4
Practitioners continue to debate the exact glucose targets that should be attained for inpatients;5, 6 however, there is more to inpatient hyperglycemia management than just trying to achieve a specific glucose range. Caring for patients with diabetes in the hospital is complex and must also encompass patient safety, but many practitioners perceive a state of glycemic chaos in the hospital.7 Because many physicians frequently overlook diabetes and glucose control in the hospital, appropriate therapeutic responses to hyperglycemia do not occur.810 National,11, 12 state,13 and specialty societies3, 4, 14 are working toimprove care for hospitalized patients with hyperglycemia. A recent consensus conference emphasized the need to develop broad‐based educational programs to increase awareness about the importance of inpatient glycemic control and to develop a standardized set of tools for hospitals to use to improve care.4 However, there is ongoing concern about the slow pace at which hospitals are implementing recommendations about glycemic control.4
Intensive and prolonged educational efforts about the importance of glycemic control will be essential ingredients of any quality improvement effort designed to create glycemic order out of glycemic chaos in the hospital.15 Before educational interventions and policies directed at improving the management of hyperglycemia in hospitalized patients can be developed, institutions need to gain a better understanding of how clinicians view the importance of inpatient glucose control and which barriers they perceive as constraints to their ability to care for inpatients with hyperglycemia.
At Atlanta Medical Center (AMC), the large urban teaching hospital where this study was conducted, the glucose control team detected resistance to changes that were implemented to improve the hospital's quality of glycemic control;16 this observation led to a desire to gain more information about practitioner attitudes regarding inpatient glucose control management. Data on practitioner attitudes and beliefs about inpatient hyperglycemia are only now emerging and are limited to studies from a single institution.17, 18 Thus, additional studies are needed to determine whether findings from these first studies are applicable to other types of hospital settings that have different inpatient populations. To gain additional insight into clinician beliefs about inpatient glucose control, we adapted a previously published questionnaire17, 18 and used it to survey resident physicians training at AMC.
METHODS
Setting
AMC is a community teaching hospital located in downtown Atlanta, Georgia, and it is a 460‐bed tertiary care facility. All adult general medical and surgical specialties are represented, in addition to obstetrics and gynecology, a neonatal unit, a level 2 trauma unit, a stroke unit, and an inpatient rehabilitation unit. The inpatient population is mostly minority in mix, with 45% African American, 37% Caucasian, 12% Hispanic, and 6% other races.16, 19 Various types of practitioners provide patient care at AMC, including postgraduate trainees (resident physicians), graduate medical education faculty, physician assistants, and nurse practitioners.
Description of Survey
A previously published survey instrument (the Mayo Clinic Inpatient Diabetes Attitude Survey) was adapted for this project.17, 18 The survey was developed by a team of endocrinologists and primary care physicians with the assistance of our institutional experts in survey design; it was then piloted and submitted to iterative cycles of review and revision.17 The survey was used to assess beliefs first among resident physicians17 and then among midlevel practitioners at the same facility.18 The survey tool was specifically developed to evaluate perceptions of practitioners about inpatient glucose management, including beliefs about the importance of glucose control in the hospital, optimal glucose targets, and barriers to the successful treatment of hyperglycemia. Additionally, the questionnaire was previously used to solicit residents' perceptions about the proportion of their inpatient practices represented by diabetes patients, their beliefs regarding whether patients were achieving their glucose targets, their degree of comfort with managing hyperglycemia and using insulin therapy, and their familiarity with existing institutional policies and preprinted insulin order sets.17, 18 The questionnaire was expanded from its original version to include questions about the use of intravenous insulin.
Survey Participants
As in most academic teaching facilities, at AMC resident physicians treat many of the inpatients who have a diagnosis of diabetes, making the residents an important group to target for educational programs focused on inpatient glucose management. Thus, the audience for this survey included only resident physicians who had ongoing inpatient responsibilities so that the data could be used to assist in educational planning strategies for increasing awareness and improving treatment of inpatients with hyperglycemia. We identified 85 residents who met the inclusion criteria, and we conducted the survey from March to April 2007.
Data Analysis
Written surveys were collected and entered into SurveyTracker version 4.0 (Training Technologies, Inc., Lebanon, Ohio) for analysis. We then examined the distribution of responses to individual questions. Finally, we listed the frequency of expressed barriers to inpatient glucose management from most common to least common.
RESULTS
Respondent Demographics
Sixty‐six of 85 residents (78%) responded to the survey. The mean age of the respondents was 31 years, 47% were men, 33% were in their first year of residency training, and 73% had graduated from medical school during the year 2002 or later. The residents represented the following departments: 41% from internal medicine (n = 27), 18% from family medicine (n = 12), 15% from general surgery (n = 10), 12% from orthopedics (n = 8), and 14% from obstetrics and gynecology (n = 9).
Perceptions About Inpatient Burden of Diabetes
When asked to estimate the percentage of their hospitalized patients who were considered to have a diagnosis of diabetes or hyperglycemia, 14% of the residents indicated that 0% to 20% of their hospitalized patients were in this category, 30% of the residents estimated that 21% to 40% of their inpatients were in this group, and 25% of the residents believed that such a diagnosis applied to 41% to 60% of their inpatients. Additionally, 23% of the residents said that 61% to 80% of their inpatients were considered to have a diagnosis of diabetes or hyperglycemia, 3% of the residents estimated that 81% to 100% of their hospitalized patients had such a diagnosis, and 5% of the residents were unsure. Thus, respondents perceived that diabetes constituted a substantial portion of their inpatient practices, with 50% of the residents estimating that more than 40% of their hospitalized patients had a diagnosis of diabetes or hyperglycemia and nearly 25% of responding residents believing that more than 60% of their inpatients had the same diagnosis.
Views on the Importance of Glycemic Control
Most resident physicians believed that good glycemic control was important in hospitalized patients (Table 1); 97% believed that it was very important to have tight glycemic control in critically‐ill patients, 72% emphasized that it was very important in non‐critically‐ill patients, and 85% indicated that it was very important during the perioperative period. Nearly all residents believed that it was important to achieve good glycemic control in pregnant patients (Table 1).
| ||||
| Category | Response | |||
| Importance of Treating Hyperglycemia | Very Important | Somewhat Important | Not at All Important | Don't Know |
| Critically ill patients | 97 | 3 | 0 | 0 |
| Non‐critically‐ill patients | 72 | 26 | 2 | 0 |
| Perioperative patients | 85 | 15 | 0 | 0 |
| Pregnant patients | 97 | 3 | 0 | 0 |
| Comfort Level | Very Comfortable | Somewhat Comfortable | Not at All Comfortable | Don't Know |
| Treating hyperglycemia | 42 | 47 | 11 | 0 |
| Treating hypoglycemia | 49 | 44 | 6 | 1 |
| Using subcutaneous insulin | 44 | 44 | 11 | 1 |
| Using insulin drips | 38 | 42 | 18 | 2 |
| Using insulin pumps* | 14 | 17 | 58 | 12 |
| Familiarity | Very Familiar | Somewhat Familiar | Not at All Familiar | Unaware of Policy |
| Insulin pump policy | 9 | 15 | 52 | 24 |
| Insulin pump orders | 6 | 17 | 54 | 23 |
| Hypoglycemia policy | 23 | 45 | 17 | 15 |
| Subcutaneous insulin orders | 34 | 35 | 14 | 17 |
| Intravenous insulin orders | 38 | 33 | 21 | 8 |
| Glucose Goal, mg/dL | 80‐110 | 111‐180 | 181‐250 | Don't Know |
| Critically ill patients | 91 | 6 | 2 | 1 |
| Non‐critically‐ill patients | 53 | 46 | 0 | 1 |
| Perioperative patients | 76 | 23 | 0 | 1 |
| Glucose Level for Initiation of IV Insulin, mg/dL | >110 | >140 | >180 | Don't Know |
| Critically ill patients | 8 | 30 | 51 | 11 |
| Non‐critically‐ill patients | 1 | 6 | 65 | 28 |
| Pregnant patients | 8 | 27 | 30 | 35 |
Comfort With Treatment and Management
Survey participants were asked how comfortable they felt about different scenarios pertaining to inpatient glucose management (Table 1). Although more than 40% of respondents indicated that they felt very comfortable treating hyperglycemia and hypoglycemia in the hospital, a large proportion (50% or more) also indicated that they were only somewhat comfortable or not at all comfortable treating these conditions. Similarly, in response to questions about their degree of comfort working with subcutaneous or intravenous insulin, more than 50% of trainees were only somewhat comfortable or not at all comfortable. Finally, most were not at all comfortable with the use of insulin pumps in the hospital (Table 1).
Familiarity With Existing Policies and Procedures
Most of the trainees indicated that they were not at all familiar with existing hospital policies and orders pertaining to insulin pumps (Table 1). Most respondents were only somewhat familiar with the institutional hypoglycemia policy, but a substantial percentage (32%) were either not at all familiar or even unaware that an institutional hypoglycemia policy existed. Similarly, most were only somewhat familiar, not at all familiar, or even unaware of orders or policies pertaining to use of subcutaneous or intravenous insulin (Table 1).
Beliefs About Glucose Targets and Hypoglycemia
When asked to indicate the target glucose levels that they would like to achieve, most resident physicians indicated that good glycemic control meant a target range of 80 to 110 mg/dL for critically‐ill patients and for perioperative patients. For non‐critically‐ill patients, targets were split between a target range of 80 to 110 mg/dL and 111 to 180 mg/dL. Trainees rarely suggested targets greater than 180 mg/dL (Table 1).
Most respondents believed that they were achieving their glycemic goals in 41% to 60% of their patients (Fig. 1A). More than half (56%) perceived that they were achieving their glucose targets in more than 40% of their diabetes patients. When asked at what glucose level they first considered the patient to be hypoglycemic, half of the respondents chose <60 mg/dL (Fig. 1B), although some had even lower cutoffs before they considered someone to have a diagnosis of hypoglycemia.

Thresholds for Starting Intravenous Insulin
For both critically‐ill and non‐critically‐ill patients, most resident physicians indicated that they would wait until the glucose level was greater than 180 mg/dL before starting an insulin infusion (Table 1). Likewise, obstetrics residents identified a glucose level greater than 180 mg/dL as a threshold to start intravenous insulin in pregnant patients.
Perceived Barriers to Care
The survey concluded with a question that asked resident physicians to choose from a list of factors they perceived as obstacles to inpatient glucose management. The 5 most frequently chosen obstacles, from most common to least common, were as follows: knowing what insulin type or regimen works best, fluctuating insulin demands related to stress and risk of causing patient hypoglycemia (cited with equal frequency), unpredictable changes in patient diet and meal times, and unpredictable timing of patient procedures (Table 2).
| Barrier | Response, Number (%) (n = 66) |
|---|---|
| |
| Knowing what insulin type or regimen works best | 26 (39) |
| Fluctuating insulin demands related to stress/concomitantly used medications | 26 (39) |
| Risk of causing hypoglycemia | 25 (38) |
| Unpredictable changes in patient diet and mealtimes | 25 (38) |
| Unpredictable timing of patient procedures | 19 (29) |
| Patient not in hospital long enough to control glucose adequately | 18 (27) |
| Shift changes and cross‐coverage lead to inconsistent management | 18 (27) |
| Knowing best options to treat hyperglycemia | 16 (24) |
| Knowing when to start insulin | 14 (21) |
| Knowing how to adjust insulin | 14 (21) |
| Conversion between different forms of insulin | 13 (20) |
| Lack of guidelines on how to treat hyperglycemia | 11 (17) |
| Preferring to defer management to outpatient care or to another specialty | 10 (15) |
| Knowing how to start insulin | 10 (15) |
| Knowing how to best prevent hypoglycemia | 7 (11) |
| None, I have no trouble treating hyperglycemia in the hospital | 7 (11) |
| Glucose management not adequately addressed on rounds | 6 (9) |
| Treating hyperglycemia is not a priority in the hospital | 6 (9) |
| Other* | 4 (6) |
| Disagreement with other team members on how to control glucose | 3 (5) |
DISCUSSION
In recent years national and regional organizations have focused greater attention on the management of hyperglycemia among inpatient populations by introducing and promoting guidelines for better care.3, 4, 1114 A consensus conference in 2006 urged hospitals to move rapidly to make euglycemia a goal for all inpatients and to make patient safety in glycemic control a reality. 20 AMC has already taken some steps toward understanding and improving its hospital‐based care of hyperglycemia, including understanding the mortality associated with hyperglycemia within the institution and implementing a novel insulin infusion algorithm.16, 19
Before hospitals can develop high‐quality improvement and educational programs focused on inpatient hyperglycemia, they will need more insight into their clinicians' views on inpatient glycemic control and the perceived barriers to successful treatment of hyperglycemia. However, the only data that have been published about practitioner attitudes on inpatient diabetes and glycemic control are from a single institution.17, 18 Thus, analyses should be broadened to include different types of hospital settings to determine common beliefs on the topic.
AMC is very different from the hospital facility where earlier studies on physician attitudes about inpatient glucose management were conducted. Whereas the site of the earlier studies is located in the Southwest and has a diabetes inpatient population that is primarily white, AMC is an urban hospital in the Southeast whose diabetes inpatient population is primarily minority.21 Despite the institutional, geographic, and patient population differences, however, results of the current survey suggest that there may be similar beliefs among practitioners about inpatient glucose management as well as common knowledge deficits that can be targeted for educational interventions.
Similar to the resident physicians surveyed in previous studies,17, 18 AMC resident physicians considered diabetes to be a substantial part of their inpatient practices: 56% of respondents believed that more than 40% of their inpatients had a diagnosis of diabetes. Historically, the prevalence at AMC of hyperglycemia has been about 38% and the prevalence of diabetes about 26%.19 The increasing number of hospital dismissals attributable to diabetes likely has increased the inpatient prevalence of the disease at AMC as well, but very high rates perceived by some residents (eg, 81%‐100%) are likely not accurate. Nonetheless, this perception of such a large burden of diabetes clearly substantiates the need to provide pertinent information and essential tools to clinicians for successful management of hyperglycemia in hospital patients. We also established that most AMC resident physicians who were surveyed believed that good glucose control was very important in situations relating to critical illness or noncritical illness. For most respondents, good glucose control was also very important in the perioperative period. This finding suggests that the trainees understand the importance of good glucose control in such situations.
In keeping with findings from previous studies,17, 18 respondents to this survey indicated glucose targets that would be well within currently existing guidelines.3, 4 Glucose management training might be improved by conveying whether actual glucose outcomes match residents' perceived achievement of glycemic control.
Insulin is the recommended treatment for inpatient hyperglycemia,3, 4 yet residents' responses reflected concern about insulin use. The most commonly noted issues, cited with equal frequency, were related to insulin use: knowing what insulin type or regimen works best and fluctuating insulin demands related to stress/concomitantly used medications. Our survey did not evaluate whether residents had different degrees of comfort with different subcutaneous insulin programs (eg, sliding scale versus basal‐bolus). Future surveys could be modified to better hone in on evaluating self‐perceived competencies in these areas.
Given the increasing complexity of insulin therapy, resident physicians' perception of insulin administration as the top barrier to inpatient glucose management may not be surprising.17, 18 The number of insulin analogs has increased in recent years. Moreover, numerous intravenous insulin algorithms are available.22, 23 Errors in insulin administration are among the most frequently occurring medication errors in hospitals.24 To address patient safety and medical system errors in the fields of diabetes and endocrinology, the American College of Endocrinology published a position statement on the topic in 2005.25 Guidelines about when to initiate insulin therapy, how to choose from numerous insulin treatment options, and how to adjust therapy in response to rapidly changing clinical situations will have to be integrated into any effort to improve inpatient glucose management. One study indicated that an educational process focused on teaching residents about insulin therapy can be successful.26
Clinician fear of hypoglycemia is often perceived as the primary obstacle to successful control of inpatient glucose levels;3, 27 however, this was not the chief concern expressed by either AMC resident physicians or by practitioners surveyed in prior studies.17, 18 Emerging data suggest that hypoglycemia in the hospital is actually uncommon.21, 28 As hospitals intensify hyperglycemia management efforts, hypoglycemia and concerns about its frequency of occurrence will most likely increase. No consensus exists regarding the number of hypoglycemic events that are acceptable in a hospitalized patient. The American Diabetes Association Workgroup on Hypoglycemia has defined hypoglycemia as an (arterialized venous) plasma glucose concentration of less than or equal to 70 mg/dL.29 As a group, residents surveyed for the current study were not consistent in their definition of hypoglycemia.
The residents at AMC also reported potential obstacles to care besides insulin management that suggest system‐based problems. Unpredictable timing of patient procedures and unpredictable changes in patient diet and mealtimes were among the 5 most frequently cited concerns. Other concerns included patient not in hospital long enough to adequately control glucose and shift changes and cross‐coverage lead to inconsistent management. These findings are identical to those of prior studies17, 18 and suggest system‐based problems as common barriers to inpatient glucose management. Some of these obstacles, such as length of hospital stay and timing of procedures, would be difficult to reengineer. However, other aspects, such as adjusting therapy to mealtimes and ensuring standardization of treatment across shifts, could be addressed through institution‐wide education and changes in policies.
As in previous studies, another major finding that emerged from this survey was the lack of resident physician familiarity with existing policies and procedures related to inpatient glucose management. AMC has a longstanding policy on hypoglycemia management and has preprinted order sets for subcutaneous insulin. AMC has implemented a revised insulin infusion algorithm16 in addition to a policy and an order set for the use of insulin pumps.30 There are no specific data on how many patients receiving insulin pump therapy are hospitalized, but these patients are likely to be encountered only rarely in the hospital setting. Hence, it may not be surprising that residents are unfamiliar with policies pertaining to inpatient insulin pump use, but they should at least be aware that guidance is available. One of the first steps to enhancing and standardizing hospital glucose management may simply be to make certain that clinicians are familiar with policies that are already in place within the institution.
A limitation of this study is the small sample size. The results of the present study should not be extrapolated to nonresident medical staff such as attending physicians, but the questionnaire could be adapted, with minor modifications, to investigate how other health care professionals view inpatient glucose management. In addition, the questionnaire could be used to assess changes in beliefs over time. Future studies should be designed to correlate resident perceptions about their inpatient diabetes care and actual practice patterns.
More surveys such as the one reported on here need to be conducted in additional institutions in order to expand our understanding of practitioner attitudes regarding inpatient diabetes care. Data from the current study and previous ones suggest that practitioners share beliefs, knowledge deficits, and perceived barriers about inpatient glucose management. Most AMC resident physicians recognized the importance of good glucose control and set target glucose ranges consistent with existing guidelines. Knowledge deficits may be addressed by developing training programs that specifically spotlight insulin use in the hospital. As a first step to quality improvement, training programs should focus on familiarizing staff with existing institutional policies and procedures pertaining to hospital hyperglycemia. In addition, hospitals need to design strategies to overcome perceived and actual barriers to care so that they can realize the desired improvement in the management of hyperglycemia in their patients. We have already begun the development and implementation of educational modules directed at addressing many of these important issues.
- Centers for Disease Control and Prevention. Hospitalization for diabetes as first‐listed diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmfirst/index.htm. Accessed October2008.
- Centers for Disease Control and Prevention. Hospitalizations for diabetes as any‐listed diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmany/index.htm. Accessed October2008.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ACE/ADA Task Force on Inpatient Diabetes.American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control.Endocr Pract.2006;12:458–468.
- ,.Counterpoint: inpatient glucose management: a premature call to arms?Diabetes Care.2005;28:976–979.
- ,.Point: inpatient glucose management: the emperor finally has clothes.Diabetes Care.2005;28:973–975.
- ,.Glycemic chaos (not glycemic control) still the rule for inpatient care: how do we stop the insanity? [Editorial]J Hosp Med.2006;1:141–144.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,, et al.Diabetes care in the hospital: is there clinical inertia?J Hosp Med.2006;1:151–160.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1:145–150.
- The Joint Commission. Inpatient diabetes. Available at: http://www.jointcommission.org/CertificationPrograms/Inpatient+Diabetes. Accessed October2008.
- Institute for Healthcare Improvement. Implement effective glucose control. Available at: http://www.ihi.org/IHI/Topics/CriticalCare/IntensiveCare/Changes/ImplementEffectiveGlucoseControl.htm. Accessed October2008.
- ,,, et al.;the Georgia Hospital Association Diabetes Special Interest Group. Working to improve care of hospital hyperglycemia through statewide collaboration.Endocr Pract.2007;13:45–50.
- Society of Hospital Medicine. Glycemic control resource room. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Search_Advanced_Search1:383–385.
- ,,, et al.Improving hyperglycemia management in the intensive care unit: preliminary report of a nurse‐driven quality improvement project using a redesigned insulin infusion algorithm.Diabetes Educ.2006;32:394–403.
- ,,, et al.Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians.Endocr Pract.2007;13:117–124.
- ,,, et al.Beliefs about hospital diabetes and perceived barriers to glucose management among inpatient midlevel practitioners.Diabetes Educ.2008;34:75–83.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- .Patient safety and inpatient glycemic control: translating concepts into action.Endocr Pract.2006;12 (Suppl 3):49–55.
- ,,, et al.Diabetes care in hospitalized noncritically ill patients: more evidence for clinical inertia and negative therapeutic momentum.J Hosp Med.2007;2:203–211.
- ,,.Insulin infusion protocols for critically ill patients: a highlight of differences and similarities.Endocr Pract.2007;13:137–146.
- ,,.Intensive insulin therapy in critical care: a review of 12 protocols.Diabetes Care.2007;30:1005–1011.
- Institute for Safe Medication Practices. ISMP's list of high‐alert medications. Available at: http://www.ismp.org/Tools/highalertmedications.pdf. Accessed October2008.
- American Association of Clinical Endocrinologists. Patient safety and medical system errors in diabetes and endocrinology consensus conference: position statement. Available at: http://www.aace.com/pub/pdf/guidelines/PatientSafetyPositionStatement.pdf. Accessed October2008.
- ,,,.Eliminating inpatient sliding‐scale insulin: a reeducation project with medical house staff.Diabetes Care.2005;28:1008–1011.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10 (Suppl 2):89–99.
- ,,,,.Inpatient point‐of‐care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control.Diabetes Technol Ther.2007;9:493–500.
- Workgroup on Hypoglycemia, American Diabetes Association.Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia.Diabetes Care.2005;28:1245–1249.
- ,,, et al.Use of continuous subcutaneous insulin infusion (insulin pump) therapy in the hospital setting: proposed guidelines and outcome measures.Diabetes Educ.2005;31:849–857.
- Centers for Disease Control and Prevention. Hospitalization for diabetes as first‐listed diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmfirst/index.htm. Accessed October2008.
- Centers for Disease Control and Prevention. Hospitalizations for diabetes as any‐listed diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmany/index.htm. Accessed October2008.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ACE/ADA Task Force on Inpatient Diabetes.American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control.Endocr Pract.2006;12:458–468.
- ,.Counterpoint: inpatient glucose management: a premature call to arms?Diabetes Care.2005;28:976–979.
- ,.Point: inpatient glucose management: the emperor finally has clothes.Diabetes Care.2005;28:973–975.
- ,.Glycemic chaos (not glycemic control) still the rule for inpatient care: how do we stop the insanity? [Editorial]J Hosp Med.2006;1:141–144.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,, et al.Diabetes care in the hospital: is there clinical inertia?J Hosp Med.2006;1:151–160.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1:145–150.
- The Joint Commission. Inpatient diabetes. Available at: http://www.jointcommission.org/CertificationPrograms/Inpatient+Diabetes. Accessed October2008.
- Institute for Healthcare Improvement. Implement effective glucose control. Available at: http://www.ihi.org/IHI/Topics/CriticalCare/IntensiveCare/Changes/ImplementEffectiveGlucoseControl.htm. Accessed October2008.
- ,,, et al.;the Georgia Hospital Association Diabetes Special Interest Group. Working to improve care of hospital hyperglycemia through statewide collaboration.Endocr Pract.2007;13:45–50.
- Society of Hospital Medicine. Glycemic control resource room. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Search_Advanced_Search1:383–385.
- ,,, et al.Improving hyperglycemia management in the intensive care unit: preliminary report of a nurse‐driven quality improvement project using a redesigned insulin infusion algorithm.Diabetes Educ.2006;32:394–403.
- ,,, et al.Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians.Endocr Pract.2007;13:117–124.
- ,,, et al.Beliefs about hospital diabetes and perceived barriers to glucose management among inpatient midlevel practitioners.Diabetes Educ.2008;34:75–83.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- .Patient safety and inpatient glycemic control: translating concepts into action.Endocr Pract.2006;12 (Suppl 3):49–55.
- ,,, et al.Diabetes care in hospitalized noncritically ill patients: more evidence for clinical inertia and negative therapeutic momentum.J Hosp Med.2007;2:203–211.
- ,,.Insulin infusion protocols for critically ill patients: a highlight of differences and similarities.Endocr Pract.2007;13:137–146.
- ,,.Intensive insulin therapy in critical care: a review of 12 protocols.Diabetes Care.2007;30:1005–1011.
- Institute for Safe Medication Practices. ISMP's list of high‐alert medications. Available at: http://www.ismp.org/Tools/highalertmedications.pdf. Accessed October2008.
- American Association of Clinical Endocrinologists. Patient safety and medical system errors in diabetes and endocrinology consensus conference: position statement. Available at: http://www.aace.com/pub/pdf/guidelines/PatientSafetyPositionStatement.pdf. Accessed October2008.
- ,,,.Eliminating inpatient sliding‐scale insulin: a reeducation project with medical house staff.Diabetes Care.2005;28:1008–1011.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10 (Suppl 2):89–99.
- ,,,,.Inpatient point‐of‐care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control.Diabetes Technol Ther.2007;9:493–500.
- Workgroup on Hypoglycemia, American Diabetes Association.Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia.Diabetes Care.2005;28:1245–1249.
- ,,, et al.Use of continuous subcutaneous insulin infusion (insulin pump) therapy in the hospital setting: proposed guidelines and outcome measures.Diabetes Educ.2005;31:849–857.
Copyright © 2009 Society of Hospital Medicine
Inpatient Diabetes Care
Diabetes confers a substantial burden on the hospital system. Diabetes is the fourth‐leading comorbid condition associated with any hospital discharge in the United States1. During 2001, for more than 500,000 patients discharged from U.S. hospitals diabetes was listed as the principal diagnosis and for more than 4 million it was listed as a codiagnosis.2, 3 Nearly one‐third of diabetes patients require at least 2 hospitalizations annually,4 and inpatient stays account for the largest proportion of direct medical expenses incurred by persons with the disease.5
Numerous studies have demonstrated that hyperglycemia is associated with adverse outcomes of hospitalized patients.68 However, studies have also confirmed that attention to lowering glucose levels in the hospital improves patient outcomes.7, 8 Although inpatients with known diabetes will likely constitute the largest and most visible percentage of those who will require treatment for high glucose, the recommendation to control glucose applies to all inpatients regardless of whether they have been diagnosed with diabetes prior to hospitalization or have manifested hyperglycemia only during the hospital stay.79
Now that the relationship between hyperglycemia and hospital outcomes is well established, the task of organizations that deliver care and set policy is to translate current recommendations of good glucose control into real‐world hospital settings. Quality improvement organizations are currently working toward developing and disseminating performance measures for control of inpatient hyperglycemia.10, 11 Although management of hospital hyperglycemia is often perceived as suboptimal,12 actual data are limited and are based on review of small numbers of charts,1315 and information is even sparser on the pharmacologic strategies being used to treat inpatient hyperglycemia. Before educational programs and policies can be developed, individual hospital systems need to gain more insight into how hyperglycemia is being managed in the hospital.
We reported previously the results of a review of a small number of charts (n = 90) of patients hospitalized with diabetes. The findings from this review suggested there was clinical inertia in glycemia management in the hospital.15 Clinical inertia was originally described in relationship to diabetes care in the outpatient setting and was defined as a failure to perform a needed service or make a change in treatment when indicated.16, 17 Since the original description, additional reports have documented the problem of clinical inertia, but these have all been based on experiences in the outpatient setting.1822 To our knowledge, our previous report was the first to question whether clinical inertia occurred in the hospital environment. In addition, we described the negative therapeutic momentuma deintensification of treatment despite ongoing hyperglycemia15. However, our prior study examined only a small number of cases and did not include detailed data on pharmacologic treatment for hyperglycemia. Therefore, we expanded our analysis using an information systems rather than a chart reviewbased methodology to assess the status of hyperglycemia management in our hospital.
METHODS
Setting
Our tertiary‐care academic teaching hospital is a 200‐bed facility in metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented, including transplantation services; the hospital also has a level 2 trauma center and an inpatient rehabilitation unit. Care is provided by various types of practitioners, including postgraduate trainees, faculty, physician assistants, and nurse‐practitioners. An electronic medical record links outpatient and inpatient records with laboratory results and pharmacy orders. The core electronic health record system is the Centricity/LastWord platform, provided by GE/IDX. The ancillary core systems, including laboratory and pharmacy, are interfaced with the Centricity system and maintained by on‐site Mayo Clinic information technology professionals.
Case Selection
Patients discharged with an International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9‐CM) diagnosis code for diabetes (ICD‐9‐CM code 250.xx) or hyperglycemia (ICD‐9‐CM code 790.6) were identified in a search of the hospital's electronic billing records.24 Our facility does not provide obstetric or pediatric services; therefore, corresponding ICD‐9‐CM codes for those populations were not included. Both primary and nonprimary diagnostic fields were searched. Discharges were extracted for the period between January 1, 2001, and December 31, 2004. Data retrieved included patient age, ethnicity/race, length of stay (LOS), and type of hospital service with primary responsibility for the patient's care. For confidentiality reasons, individual patients were not identified, and the unit of analysis was the discharge.
Our analyses focused principally on the noncritically ill, defined as those patients who did not require a stay in our intensive or intermediate care units; critically ill patients were identified based on room location in the data set and excluded. The reasons this study assessed hyperglycemia management in the noncritically ill were 2‐fold. First, the critically ill may migrate in and out of intensive care depending on their health status and thus experience different intensities of glucose management. Second, in our facility the therapeutic approach to hyperglycemia management is different for the critically ill than for the noncritically ill; the critically ill may receive intravenous and/or subcutaneous insulin, whereas subcutaneous insulin therapy only is given to the noncritically ill. Thus, the noncritically ill represent a more clearly defined patient population whose therapies would be easier to evaluate. We also restricted the final analysis to patients who had a LOS of 3 days or less, so that differences in glucose control and insulin therapy between the first and last 24 hours of hospital stay could be assessed.
Data on 30 randomly chosen patients from different years was extracted from electronic records. A spreadsheet of the data was compared against data in our online electronic medical records. The online data were printed, and packets were made of the data for each patient selected for review. The patient demographic information was validated against our registration screen. Inpatient stay was validated to verify a patient was in intensive or intermediate care. The result of each glucose test performed while the patient was in the hospital was printed and the calculations validated. The insulin given while the patient was hospitalized was also printed and reviewed to verify the type of insulin and calculations for the amounts of insulin given.
Assessment of Glycemic Control
After extraction of hospital cases, data were linked via patient identifiers to our electronic laboratory database to retrieve information on glucose values. Glucose data included both blood and bedside measurements. In our institution, bedside glucose monitoring is performed with an instrument that scans and records patient identification, followed by direct downloading to our laboratory database. Commercial software (Medical Automation Systems, Charlottesville, VA) facilitates the interfacing of glucometer data with the electronic laboratory file.
Nearly all hospitalized patients had either bedside glucose (84%) or blood glucose (86%) data available for analysis. However, the mean number of bedside glucose measurements was 3.4 per day, whereas the average number of blood glucose measurements was only 1.0 per day. Because of the greater number of bedside measurements and because practitioners typically make therapeutic decisions about hyperglycemia management on the basis of daily bedside glucose results, these values were used to assess glycemic control of patients in the hospital discharge data.15
To assess glycemic control, we used methods similar to those previously published by ourselves and others.15, 23 We averaged each patient's available bedside glucose measurements to determine the composite average (BedGlucavg). We also computed the average of bedside glucose measurements obtained during the first 24 hours after admission (F24BedGlucavg) and during the last 24 hours before discharge (L24BedGlucavg), then examined the distributions of BedGlucavg, F24BedGlucavg, and L24BedGlucavg. The first 24‐hour period was calculated forward from the recorded time of admission, and the last 24‐hour period was calculated backward from the time of discharge. We calculated the frequency that each patient's bedside measurements showed hypoglycemia (bedside glucose < 70, < 60, < 50, or < 40 mg/dL) and showed hyperglycemia (bedside glucose >2 00, > 250, > 300, > 350, or > 400 mg/dL). Results were recorded as the number of values per 100 measurements per person; this method allowed adjustment for variation in the individual number of measurements and captured information on multiple episodes of hypo‐ or hyperglycemia of individual patients.15, 23
Hyperglycemia Therapy
Links to our inpatient pharmacy database enabled determination of types of pharmacotherapy actually administered to patients to treat hyperglycemia. Our electronic pharmacy records are designed so that intravenous medications (eg, intravenous insulin), scheduled oral and subcutaneous medications (eg, subcutaneous insulin), and medications administered on a one‐time or as‐needed basis (eg, sliding‐scale insulin) are documented electronically as separate categories. In our facility, intravenous insulin is administered only in the intensive care setting or as a component of total parenteral nutrition, and we excluded intravenous insulin use from this data. Thus, our analysis of insulin therapy focused only on elucidating patterns of subcutaneous treatment.
We classified hyperglycemia treatment as no therapy, oral agents only, oral agents plus insulin, and insulin only. Patients were regarded as having received an oral agent or insulin if they were administered the medication at any time during their inpatient stay. For management of hyperglycemia in noncritically ill patients, the use of a programmed basal‐bolus insulin program is advocated rather than the use of only a short‐acting bolus or sliding‐scale regimen.7, 8 Therefore, we further examined the insulin treatment strategies by classifying the type of regimen as basal only (if only an extended‐release preparation was used), as basal bolus (if the therapy consisted of a long‐acting plus a short‐acting formulation), or as bolus only (if the only insulin administered was a short‐acting preparation).
In addition to characterizing the general therapeutic approaches to hyperglycemia, we determined changes in the amount of insulin administered according to the severity of the hyperglycemia. Among patients who received insulin, we compared the average total units of insulin used during the last 24 hours before discharge with the amount administered during the first 24 hours of hospitalization. If more units were used during the last 24 hours than in the first 24 hours, the amount of insulin administered was categorized as having increased; if fewer units were provided during the last 24 hours, then the insulin amount was classified as having decreased; otherwise, no change was considered to have occurred. The BedGlucavg values were divided into 3 intervals using tertile cut points, and the differences in the proportion of patients by each type of insulin treatment regimen and the categories of insulin change were compared across tertiles; differences in proportions were determined using the 2 statistic.
RESULTS
Patient Characteristics
Between January 1, 2001, and December 31, 2004, a total of 7361 patients were discharged from our facility with either a diabetes or a hyperglycemia diagnosis (16% of all discharges); the percentage of discharges associated with these diagnoses increased from 14.9% in 2001 to 16.4% in 2004. Most patients with diabetes or hyperglycemia (5198 or 71%) received care outside the intensive‐ or intermediate‐care setting.
Among the noncritically ill patients whose LOS was at least 3 days (N = 2916), average age was 69 years, and average LOS was 5.7 days. Most of the discharged patients were men (57%), and 90% were white. Most patients were discharged from primary care (45%; general internal medicine or family medicine) or surgical services (34%), with the rest discharged from other specialties (eg, cardiology, transplant medicine). Compared to the noncritically ill, who had an LOS of at least 3 days, those noncritically patients whose LOS was less than 3 days (n = 2282) were slightly younger (mean age 68 versus 69 years, P < .001 by Mann‐Whitney testing) but were comparable in sex and race distribution (P > .07 for both by chi‐square testing).
Glycemic Control
The median duration between admission and time of first bedside glucose measurement was 3.0 hours. Patients had an average of 19 bedside glucose measurements; the overall mean number of bedside measurements was 3.4 per day, 3.7 during the first 24‐hour period, and 3.4 during the last 24 hours of hospitalization. Nearly 25% of patients were hyperglycemic (bedside glucose > 200 mg/dL) during the first 24 hours of hospitalization (Fig. 1A), 20% had persistent hyperglycemia throughout the entire hospitalization (Fig. 1B), and 21% were hyperglycemic during the 24 hours before discharge (Fig. 1C), with some patients discharged with an average bedside glucose of at least 300 mg/dL during the 24 hours before discharge.
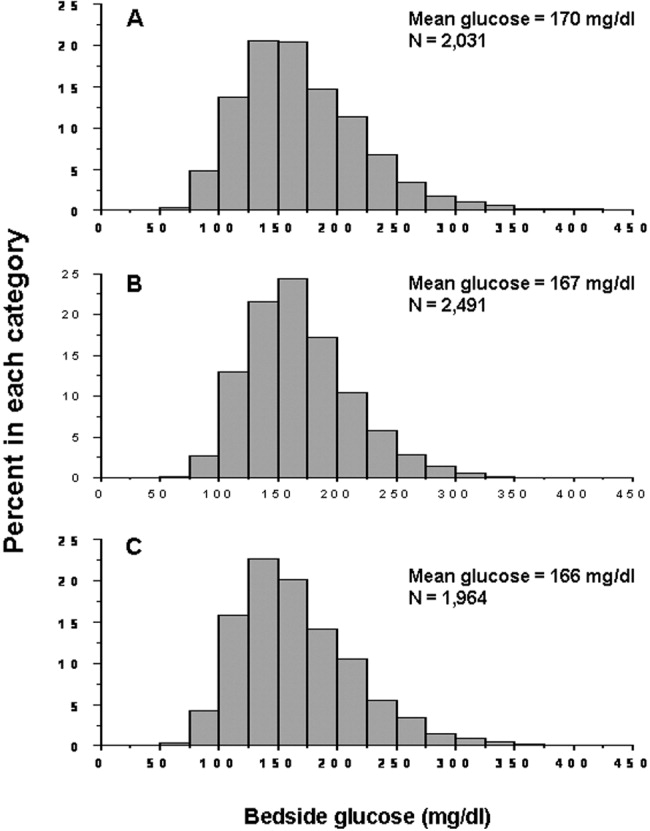
The incidence of hypoglycemic episodes was lower than that of hyperglycemic episodes: 21% of patients had at least 1 bedside glucose value less than 70 mg/dL, but 68% had at least 1 value greater than 200 mg/dL. The frequency of hypoglycemic measurements was low (Fig. 2A) compared with the frequency of hyperglycemic episodes (Fig. 2B).
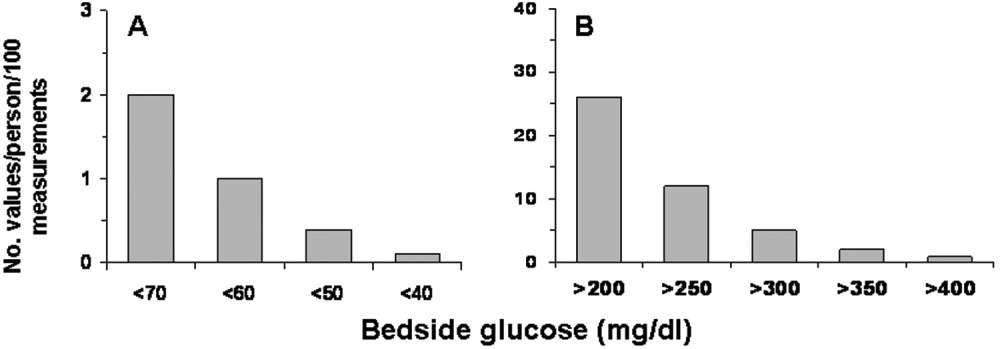
Hyperglycemia Therapy
Most patients (72%) received subcutaneous insulin at some point during their hospital stay; 19% had no therapy, 9% had oral agents only, 26% had oral agents plus insulin, and 46% had insulin only. The proportion receiving no therapy decreased from 32% among patients whose BedGlucavg was in the first tertile to 2% in the third tertile; the percentage of patients taking oral agents only decreased from 18% to 1%; the proportion taking oral agents plus insulin was 17% in the first tertile and 30% in the third; and the proportion of those taking insulin only was 32% in the first tertile and 66% in the third (Fig. 3). Thus, nearly all patients whose BedGlucavg value was in the third tertile received insulin, either as monotherapy or in combination with oral agents.
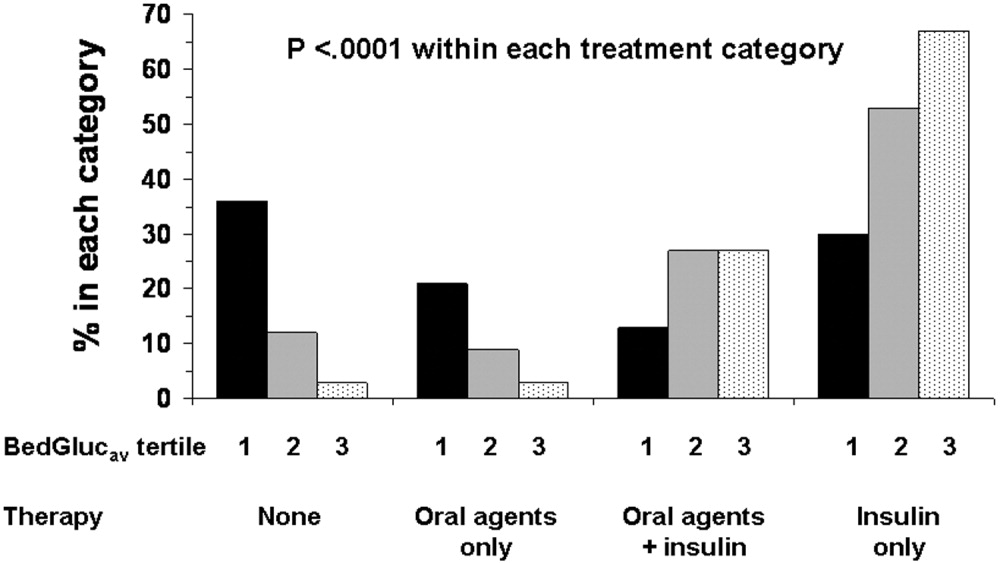
Among insulin users, 58% received bolus‐only, 42% received basal‐bolus, and 1% received basal‐only injections. Because of the small proportion of basal‐only patients, we conducted analyses only of patients whose insulin treatment fell into 1 of the first 2 categories. The use of a basal‐bolus insulin program increased from 34% in patients whose BedGlucavg was in the first tertile to 54% for those who had BedGlucavg in the third tertile (P < .001; Fig. 4, left). Thus, although there was a greater transition to a more intensive insulin regimen with worsening hyperglycemia, a substantial number of patients (46%) whose BedGlucavg was in the third tertile still did not have their insulin regimen intensified to a basal‐bolus program.
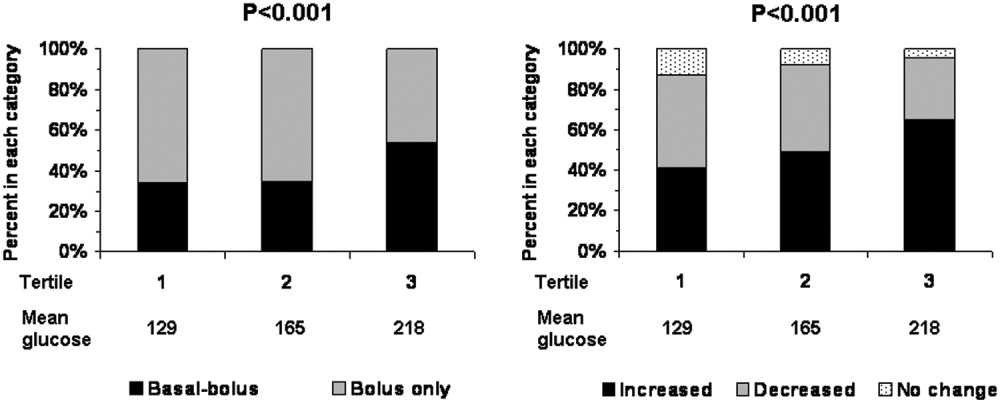
Fifty‐four percent of subcutaneous insulin users (N = 1680) had an increase in the amount of insulin administered between the first and last 24 hours of hospitalization (average increase, 17 U), 39% had a decrease (average decrease, 12 U), and 7% had no change. With rising hyperglycemia, more patients had their insulin increased by the time of discharge; 41% of persons who had BedGlucavg values in the first tertile were on more insulin by the time of discharge, whereas 65% of those who had average glucose values in the third tertile had insulin increased (Fig. 4, right). However, the pattern of changes in the amount of administered insulin was heterogeneous, with increases, decreases, and no change occurring in all tertiles of BedGlucavg (Fig. 3, right). Nearly 31% of patients whose BedGlucavg values were in the third tertile actually had a decrease in insulin. This decrease occurred despite evidence of a low frequency of hypoglycemia (only 1.2 values < 70 mg/dL per 100 measurements per person) and a high frequency of hyperglycemia (55.4 values > 200 mg/dL per person per 100 measurements).
DISCUSSION
The number of diabetes‐associated hospital discharges has been climbing2, 3; our own data indicate an increase in the number of patients with diabetes as a proportion of the total number of discharged patients. A recent consensus advocates good glucose control in the hospital to optimize outcomes,79 and institutions need to begin the process of assessing their quality of inpatient hyperglycemia management as a first step to enhancing care.
There are no guidelines about which method of glucose measurement (ie, blood glucose or bedside glucose) should be used as the quality measure to evaluate glycemic control in hospital patients. Both blood and bedside glucose measurements have been used in outcomes studies.23, 24 We analyzed capillary bedside values measured by a method subjected to ongoing quality control oversight and stored in the electronic laboratory database. Bedside glucose measurements are typically obtained with far greater frequency than blood glucose measurements and therefore provide better insight into daily changes in glycemic control; in practice, clinicians rely on bedside values when assessing hyperglycemia and making therapeutic decisions.
There is also no consensus about what glucose metric should be used to assess the status of glycemic control in the hospital. Some studies have used single glucose values to examine the relationship between hyperglycemia and outcomes,25, 26 whereas others have used values averaged over various lengths of time.24, 27 To evaluate glucose control, we averaged capillary measurements in the first 24 hours of hospitalization (F24BedGlucavg), the last 24 hours of hospitalization (L24BedGlucavg), and for the entire LOS (BedGlucavg), and we calculated the number of documented hyper‐ and hypoglycemic events. The measures we used to examine hyperglycemia would serve as useful benchmarks for following the progress of future institutional interventions directed at glucose control in hospitalized patients at our hospital.
A substantial number of our patients selected for analysis (ie, noncritically ill with LOS 3 days) were found to have sustained hyperglycemia at the beginning, during, and at the end of their hospital stay. We found very few instances of severe hypoglycemia (values < 50 or < 40 mg/dL), and the low frequency of hypoglycemia compared to that of hyperglycemia could encourage practitioners to be more aggressive in treating hyperglycemia. The high frequency of recorded bedside glucose compared with blood glucose measurements ( 3 per day), the ongoing patient surveillance by medical, nursing, and other staff members, and our institution's written hypoglycemia policy most likely minimize the number of unobserved, undocumented, or untreated hypoglycemic episodes. There are no data or recommendations about what would be an acceptable number of hypoglycemic episodes in the hospital.
Very little is known about the therapeutic strategies being applied to hyperglycemia in the hospital. Our data show that subcutaneous insulin (either alone or in combination with oral agents) was used at some point during hospitalization for nearly three‐fourths of noncritically patients who were in the hospital for 3 days or longer. Moreover, as hyperglycemia worsened, use of oral hypoglycemic agents declined, there was a shift toward greater use of a scheduled basal‐bolus insulin program, and a greater proportion of patients had more insulin administered.
Although these latter findings are encouraging and suggest that practitioners are responding to the severity of hyperglycemia, further examination of the data suggests that a substantial number of patients in the highest glucose tertile did not have insulin therapy intensified. Nearly half our patients whose glucose values were in the highest tertile were treated with short‐acting insulin aloneprobably an ineffective regimen23, 28or did not have more insulin administered. The higher doses administered were not likely solely a result of using more sliding‐scale insulin, as previous investigators actually found no correlation between intensity of the sliding scale and total daily insulin dose.14 Although evidence here is circumstantial (we did not examine changes in provider orders in response to glucose levels), these findings, together with those in our previous study15 and in another study,14 provide indirect evidence of clinical inertia in the hospital.
Beyond clinical inertia, however, there was evidence of negative therapeutic momentum: nearly one‐third of patients whose glucose was in the highest tertile had insulin decreased rather than increased, despite the low frequency of hypoglycemia and the high frequency of hyperglycemia. It is likely that even a single episode of hypoglycemia concerned practitioners, but the clinical response in these situations should be to investigate and correct the circumstances leading to the hypoglycemia, rather than to necessarily deintensify therapy in the face of continued hyperglycemia. The analysis of this larger data set corroborated our observations of clinical inertia and negative therapeutic momentum from an earlier study of chart reviews of a smaller patient sample.15
The variable application of insulin therapy to the treatment of hyperglycemia may be an indication of the level of comfort practitioners have about using this pharmacologic agent. A recently completed survey of resident physicians at our institution indicated that understanding how to use insulin was the most common barrier to successful management of inpatient hyperglycemia.29 These observations reinforce the need for institutions to develop standardized insulin order sets and develop programs to educate the staff on the use of insulin.
This study differs from our original analysis based on chart review in 4 ways. First, the sample size in our first study (n = 90) was small and derived from discharges from a single year (2003), whereas the sample in the present study spanned several years and included several thousand cases. Second, in our prior study we did not have detailed pharmacologic data on glucose management and how treatment approaches varied relative to severity of hyperglycemia. In general, there is very limited data on what therapeutic strategies are being applied to inpatient hyperglycemia, and this analysis of a large sample of cases provides more insight into how practitioners are managing glucose.
Third, we wanted to corroborate observations made in our previous report using a different methodologyin this instance, adapting existing information systems to assessment of inpatient diabetes care. For example, our last study was based on a limited number of glucose observations but suggested that the prevalence of hypoglycemia in our hospital was low compared with that of hyperglycemia; the present analysis of a very large number of glucose values confirmed these initial findings. In addition, use of information systems versus a chart review approach to assessing inpatient diabetes care corroborates our earlier suspicions about the presence of clinical inertia and negative therapeutic momentum in glucose management.
Fourth and finally, this study gave us experience with use of electronic records as a means to assess the status of inpatient diabetes care. Electronic data sources will likely be common tools to monitor quality of inpatient diabetes care and will likely figure prominently in future accreditation processes.10, 11 Unlike chart abstraction, which would require extensive man‐hours to extract data on few patients, use of electronic records allows examination of large numbers of hospital cases. Queries of information systems could be automated, and report cards potentially generated and feedback given to providers on the status of inpatient glycemic control. The industry is actively pursuing software development to assist hospitals in assessing the quality of inpatient glycemic control (eg, RALS‐TGCM, available at
However, there are also limitations to using electronic records as the sole method of assessing inpatient diabetes care. For instance, retrospective review of electronic records does not allow assessment of reasons underlying decision‐making behavior of clinicians (eg, why they did or did not change therapy). Diabetes and hyperglycemia associated hospitalizations must be identified by discharge diagnosis codes, so some cases of diabetes and hyperglycemia were likely missed.30, 31 Recent guidelines propose preprandial targets for glucose in the hospital.8 It is not easy to determine from an electronic data source which is a preprandial bedside glucose and which is a postprandial bedside glucose. Pre‐ and postpyramidal glucose categories would be difficult to define even during prospective studies, given the varying nature of nutritional support (ie, enteral, parenteral) used in the hospital and the administration of continuous dextrose infusions. Some type of quality control, such as conducting reviews of small samples of randomly selected charts to see how they compare with the electronic data, will need to be conducted.
From electronic discharge data, we cannot establish who had preexisting diabetes, who was admitted with new‐onset diabetes, and who developed hyperglycemia as a result of the hospital stay. Our previous random chart review15 indicated it is likely that most (more than 90%) had an established diagnosis of diabetes before admission. However, the recommendation to treat hyperglycemia should apply to all patients regardless of whether they had diagnosed diabetes prior to hospitalization or manifested hyperglycemia only during the hospital stay.79
As hospitals move toward making efforts to improve performance related to treating inpatient hyperglycemia, they must be cognizant of the heterogeneity of the inpatient population and the challenges to managing hospital hyperglycemia before drawing conclusions about their management. Inpatients with hyperglycemia are a diverse group, comprising patients with preexisting diabetes, with previously undiagnosed diabetes, and stress‐caused hyperglycemia. The unpredictable timing of procedures, various and changing forms of nutritional support, and different levels of staff expertise all contribute to the challenges of managing inpatient hyperglycemia. Inpatient practitioners may be forced to attempt glycemic control catch‐up for hospitalized persons who had poor outpatient glucose control. Patients who have required a stay in the intensive care unit may have very different glycemic outcomes than those who have not. Patients whose LOS was short (< 3days) may have different glycemic outcomes than persons whose LOS was longer ( 3 days as defined here) because of the length of time practitioners have to work to control their hyperglycemia. These and other variables may have to be taken into account when developing and assessing the impact of interventions.
Despite these limitations, our analysis was helpful in providing direction for enhancing the care of hospitalized patients with hyperglycemia in our facility. For instance, our generalists and surgeons are the principal caretakers of noncritically ill patients with diabetes, and these practitioners could be targeted for the first continuing educational programs about inpatient care of hyperglycemia. In addition, institutional guidelines on when and how to initiate and change therapyparticularly insulincan be designed so that hyperglycemia in noncritically ill hospital patients can be managed more effectively. These and other ongoing educational initiatives are necessary to ensure delivery of the highest quality of inpatient glucose care.
- ,,,.Hospitalization in the United States,1997.Rockville, MD:Agency for Healthcare Research and Quality;2000. Report No.: HCUP Fact Book No. 1; AHRQ Publication No. 00‐0031.
- Hospitalization for Diabetes as First‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmfirst/index.htm. Accessed November 29,2006.
- Hospitalizations for Diabetes as Any‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmany/index.htm. Accessed November 29,2006,
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26:1421–1426.
- ,,.Economic costs of diabetes in the US in 2002.Diabetes Care.2003;26:917–932.
- ,,.Inpatient diabetology. The new frontier.J Gen Intern Med.2004;19:466–471.
- ,,, et al.American Diabetes Association Diabetes in Hospitals Writing Committee: Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ACE Task Force on Inpatient Diabetes and Metabolic Control.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract,2004;10:77–82.
- ACE/ADA Task Force on Inpatient Diabetes.American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control.Endocr Pract.2006;12:459–468.
- Getting started kit: prevent surgical site infections.2006 Available at: www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed November 29,year="2006"2006.
- Joint Commission on Accreditation of Healthcare Organizations. American Diabetes Association and Joint Commission Collaborate on Joint Commission Inpatient Diabetes Care Certification.2006. Available at: http://www.jointcommission.org/NewsRoom/NewsReleases/jc_nr_072006.htm. Accessed November 29,year="2006"2006,
- ,.Glycemic chaos (not glycemic control) still the rule for inpatient care: How do we stop the insanity?J Hosp Med.2006;1:141–144.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21(2):246–249.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1(3):145–150.
- ,,, et al.Diabetes care in the non‐ICU setting: is there clinical inertia in the hospital?J Hosp Med,2006;1(3):151–160.
- ,,, et al.Diabetes in urban African‐Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes.Diabetes Care.1999;22:1494–500.
- ,,, et al.Clinical Inertia.Ann Intern Med.2001;135:825–834.
- ,,,Team UHCUDBP.Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change.Diabetes Care.2005;28:337–442.
- ,,, et al.Clinical inertia in the management of type 2 diabetes metabolic risk factors.Diabet Med,2004;21:150–155.
- ,.Clinical inertia: errors of omission in drug therapy.Am J Health Syst Pharm.2004;61:401–404.
- .Overcome clinical inertia to control systolic blood pressure.Arch Intern Med,2003;163:2677–2678.
- ,,,,.Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians?Diabetes Care.2005;28:600–606.
- ,,.Glycemic Control and Sliding Scale Insulin Use in Medical Inpatients With Diabetes Mellitus.Arch Intern Med.1997;157:545–552.
- ,,.Effect of hyperglycemia and continuous intraveneous insulin infusions on outcomes of cardiac surgical procedures: the Portland Diabetic Project.Endocr Pract.2004;10(2):21–33.
- ,,, et al.Plasma glucose at hospital admission and previous metabolic control determine myocardial infarct size and survival in patients with and without type 2 diabetes: the Langendreer Myocardial Infarction and Blood Glucose in Diabetic Patients Assessment (LAMBDA).Diabetes Care.2005;28:2551–2553.
- ,,.Admission hyperglycemia as a prognostic indicator in trauma.J Trauma Inj Infect Crit Care.2003;55(1):33–38.
- ,,, et al.Intraoperative hyperglycemia and perioperative outcomes in cardiac surgery patients.Mayo Clin Proc.2005;80:862–866.
- ,,,,.Efficacy of sliding‐scale insulin therapy: a comparison with prospective regimens.Fam Pract Res J.1994;14:313–22.
- ,,, et al.Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians.Endocr Pract., to appear.
- ,,,,.Diabetes‐related hospitalization and hospital utilization. In:Diabetes in America.Bethesda, MD:National Institutes of Diabetes and Digestive Diseases;1995:553–563.
- ,,, et al.Hospital discharge records under‐report the prevalence of diabetes in inpatients.Diabetes Res Clin Pract.2003;59(2):145–151.
Diabetes confers a substantial burden on the hospital system. Diabetes is the fourth‐leading comorbid condition associated with any hospital discharge in the United States1. During 2001, for more than 500,000 patients discharged from U.S. hospitals diabetes was listed as the principal diagnosis and for more than 4 million it was listed as a codiagnosis.2, 3 Nearly one‐third of diabetes patients require at least 2 hospitalizations annually,4 and inpatient stays account for the largest proportion of direct medical expenses incurred by persons with the disease.5
Numerous studies have demonstrated that hyperglycemia is associated with adverse outcomes of hospitalized patients.68 However, studies have also confirmed that attention to lowering glucose levels in the hospital improves patient outcomes.7, 8 Although inpatients with known diabetes will likely constitute the largest and most visible percentage of those who will require treatment for high glucose, the recommendation to control glucose applies to all inpatients regardless of whether they have been diagnosed with diabetes prior to hospitalization or have manifested hyperglycemia only during the hospital stay.79
Now that the relationship between hyperglycemia and hospital outcomes is well established, the task of organizations that deliver care and set policy is to translate current recommendations of good glucose control into real‐world hospital settings. Quality improvement organizations are currently working toward developing and disseminating performance measures for control of inpatient hyperglycemia.10, 11 Although management of hospital hyperglycemia is often perceived as suboptimal,12 actual data are limited and are based on review of small numbers of charts,1315 and information is even sparser on the pharmacologic strategies being used to treat inpatient hyperglycemia. Before educational programs and policies can be developed, individual hospital systems need to gain more insight into how hyperglycemia is being managed in the hospital.
We reported previously the results of a review of a small number of charts (n = 90) of patients hospitalized with diabetes. The findings from this review suggested there was clinical inertia in glycemia management in the hospital.15 Clinical inertia was originally described in relationship to diabetes care in the outpatient setting and was defined as a failure to perform a needed service or make a change in treatment when indicated.16, 17 Since the original description, additional reports have documented the problem of clinical inertia, but these have all been based on experiences in the outpatient setting.1822 To our knowledge, our previous report was the first to question whether clinical inertia occurred in the hospital environment. In addition, we described the negative therapeutic momentuma deintensification of treatment despite ongoing hyperglycemia15. However, our prior study examined only a small number of cases and did not include detailed data on pharmacologic treatment for hyperglycemia. Therefore, we expanded our analysis using an information systems rather than a chart reviewbased methodology to assess the status of hyperglycemia management in our hospital.
METHODS
Setting
Our tertiary‐care academic teaching hospital is a 200‐bed facility in metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented, including transplantation services; the hospital also has a level 2 trauma center and an inpatient rehabilitation unit. Care is provided by various types of practitioners, including postgraduate trainees, faculty, physician assistants, and nurse‐practitioners. An electronic medical record links outpatient and inpatient records with laboratory results and pharmacy orders. The core electronic health record system is the Centricity/LastWord platform, provided by GE/IDX. The ancillary core systems, including laboratory and pharmacy, are interfaced with the Centricity system and maintained by on‐site Mayo Clinic information technology professionals.
Case Selection
Patients discharged with an International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9‐CM) diagnosis code for diabetes (ICD‐9‐CM code 250.xx) or hyperglycemia (ICD‐9‐CM code 790.6) were identified in a search of the hospital's electronic billing records.24 Our facility does not provide obstetric or pediatric services; therefore, corresponding ICD‐9‐CM codes for those populations were not included. Both primary and nonprimary diagnostic fields were searched. Discharges were extracted for the period between January 1, 2001, and December 31, 2004. Data retrieved included patient age, ethnicity/race, length of stay (LOS), and type of hospital service with primary responsibility for the patient's care. For confidentiality reasons, individual patients were not identified, and the unit of analysis was the discharge.
Our analyses focused principally on the noncritically ill, defined as those patients who did not require a stay in our intensive or intermediate care units; critically ill patients were identified based on room location in the data set and excluded. The reasons this study assessed hyperglycemia management in the noncritically ill were 2‐fold. First, the critically ill may migrate in and out of intensive care depending on their health status and thus experience different intensities of glucose management. Second, in our facility the therapeutic approach to hyperglycemia management is different for the critically ill than for the noncritically ill; the critically ill may receive intravenous and/or subcutaneous insulin, whereas subcutaneous insulin therapy only is given to the noncritically ill. Thus, the noncritically ill represent a more clearly defined patient population whose therapies would be easier to evaluate. We also restricted the final analysis to patients who had a LOS of 3 days or less, so that differences in glucose control and insulin therapy between the first and last 24 hours of hospital stay could be assessed.
Data on 30 randomly chosen patients from different years was extracted from electronic records. A spreadsheet of the data was compared against data in our online electronic medical records. The online data were printed, and packets were made of the data for each patient selected for review. The patient demographic information was validated against our registration screen. Inpatient stay was validated to verify a patient was in intensive or intermediate care. The result of each glucose test performed while the patient was in the hospital was printed and the calculations validated. The insulin given while the patient was hospitalized was also printed and reviewed to verify the type of insulin and calculations for the amounts of insulin given.
Assessment of Glycemic Control
After extraction of hospital cases, data were linked via patient identifiers to our electronic laboratory database to retrieve information on glucose values. Glucose data included both blood and bedside measurements. In our institution, bedside glucose monitoring is performed with an instrument that scans and records patient identification, followed by direct downloading to our laboratory database. Commercial software (Medical Automation Systems, Charlottesville, VA) facilitates the interfacing of glucometer data with the electronic laboratory file.
Nearly all hospitalized patients had either bedside glucose (84%) or blood glucose (86%) data available for analysis. However, the mean number of bedside glucose measurements was 3.4 per day, whereas the average number of blood glucose measurements was only 1.0 per day. Because of the greater number of bedside measurements and because practitioners typically make therapeutic decisions about hyperglycemia management on the basis of daily bedside glucose results, these values were used to assess glycemic control of patients in the hospital discharge data.15
To assess glycemic control, we used methods similar to those previously published by ourselves and others.15, 23 We averaged each patient's available bedside glucose measurements to determine the composite average (BedGlucavg). We also computed the average of bedside glucose measurements obtained during the first 24 hours after admission (F24BedGlucavg) and during the last 24 hours before discharge (L24BedGlucavg), then examined the distributions of BedGlucavg, F24BedGlucavg, and L24BedGlucavg. The first 24‐hour period was calculated forward from the recorded time of admission, and the last 24‐hour period was calculated backward from the time of discharge. We calculated the frequency that each patient's bedside measurements showed hypoglycemia (bedside glucose < 70, < 60, < 50, or < 40 mg/dL) and showed hyperglycemia (bedside glucose >2 00, > 250, > 300, > 350, or > 400 mg/dL). Results were recorded as the number of values per 100 measurements per person; this method allowed adjustment for variation in the individual number of measurements and captured information on multiple episodes of hypo‐ or hyperglycemia of individual patients.15, 23
Hyperglycemia Therapy
Links to our inpatient pharmacy database enabled determination of types of pharmacotherapy actually administered to patients to treat hyperglycemia. Our electronic pharmacy records are designed so that intravenous medications (eg, intravenous insulin), scheduled oral and subcutaneous medications (eg, subcutaneous insulin), and medications administered on a one‐time or as‐needed basis (eg, sliding‐scale insulin) are documented electronically as separate categories. In our facility, intravenous insulin is administered only in the intensive care setting or as a component of total parenteral nutrition, and we excluded intravenous insulin use from this data. Thus, our analysis of insulin therapy focused only on elucidating patterns of subcutaneous treatment.
We classified hyperglycemia treatment as no therapy, oral agents only, oral agents plus insulin, and insulin only. Patients were regarded as having received an oral agent or insulin if they were administered the medication at any time during their inpatient stay. For management of hyperglycemia in noncritically ill patients, the use of a programmed basal‐bolus insulin program is advocated rather than the use of only a short‐acting bolus or sliding‐scale regimen.7, 8 Therefore, we further examined the insulin treatment strategies by classifying the type of regimen as basal only (if only an extended‐release preparation was used), as basal bolus (if the therapy consisted of a long‐acting plus a short‐acting formulation), or as bolus only (if the only insulin administered was a short‐acting preparation).
In addition to characterizing the general therapeutic approaches to hyperglycemia, we determined changes in the amount of insulin administered according to the severity of the hyperglycemia. Among patients who received insulin, we compared the average total units of insulin used during the last 24 hours before discharge with the amount administered during the first 24 hours of hospitalization. If more units were used during the last 24 hours than in the first 24 hours, the amount of insulin administered was categorized as having increased; if fewer units were provided during the last 24 hours, then the insulin amount was classified as having decreased; otherwise, no change was considered to have occurred. The BedGlucavg values were divided into 3 intervals using tertile cut points, and the differences in the proportion of patients by each type of insulin treatment regimen and the categories of insulin change were compared across tertiles; differences in proportions were determined using the 2 statistic.
RESULTS
Patient Characteristics
Between January 1, 2001, and December 31, 2004, a total of 7361 patients were discharged from our facility with either a diabetes or a hyperglycemia diagnosis (16% of all discharges); the percentage of discharges associated with these diagnoses increased from 14.9% in 2001 to 16.4% in 2004. Most patients with diabetes or hyperglycemia (5198 or 71%) received care outside the intensive‐ or intermediate‐care setting.
Among the noncritically ill patients whose LOS was at least 3 days (N = 2916), average age was 69 years, and average LOS was 5.7 days. Most of the discharged patients were men (57%), and 90% were white. Most patients were discharged from primary care (45%; general internal medicine or family medicine) or surgical services (34%), with the rest discharged from other specialties (eg, cardiology, transplant medicine). Compared to the noncritically ill, who had an LOS of at least 3 days, those noncritically patients whose LOS was less than 3 days (n = 2282) were slightly younger (mean age 68 versus 69 years, P < .001 by Mann‐Whitney testing) but were comparable in sex and race distribution (P > .07 for both by chi‐square testing).
Glycemic Control
The median duration between admission and time of first bedside glucose measurement was 3.0 hours. Patients had an average of 19 bedside glucose measurements; the overall mean number of bedside measurements was 3.4 per day, 3.7 during the first 24‐hour period, and 3.4 during the last 24 hours of hospitalization. Nearly 25% of patients were hyperglycemic (bedside glucose > 200 mg/dL) during the first 24 hours of hospitalization (Fig. 1A), 20% had persistent hyperglycemia throughout the entire hospitalization (Fig. 1B), and 21% were hyperglycemic during the 24 hours before discharge (Fig. 1C), with some patients discharged with an average bedside glucose of at least 300 mg/dL during the 24 hours before discharge.
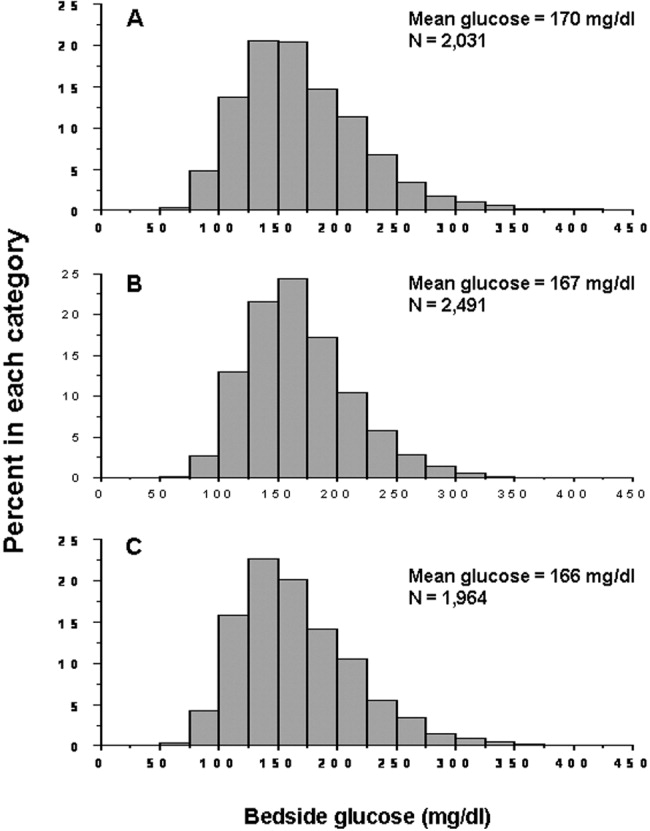
The incidence of hypoglycemic episodes was lower than that of hyperglycemic episodes: 21% of patients had at least 1 bedside glucose value less than 70 mg/dL, but 68% had at least 1 value greater than 200 mg/dL. The frequency of hypoglycemic measurements was low (Fig. 2A) compared with the frequency of hyperglycemic episodes (Fig. 2B).
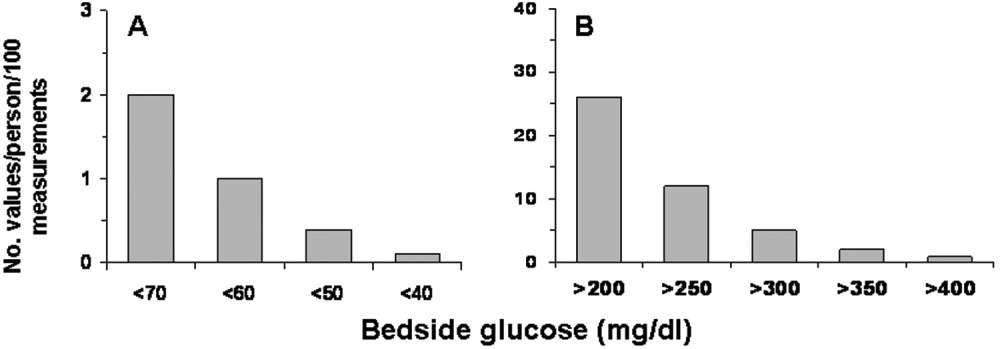
Hyperglycemia Therapy
Most patients (72%) received subcutaneous insulin at some point during their hospital stay; 19% had no therapy, 9% had oral agents only, 26% had oral agents plus insulin, and 46% had insulin only. The proportion receiving no therapy decreased from 32% among patients whose BedGlucavg was in the first tertile to 2% in the third tertile; the percentage of patients taking oral agents only decreased from 18% to 1%; the proportion taking oral agents plus insulin was 17% in the first tertile and 30% in the third; and the proportion of those taking insulin only was 32% in the first tertile and 66% in the third (Fig. 3). Thus, nearly all patients whose BedGlucavg value was in the third tertile received insulin, either as monotherapy or in combination with oral agents.
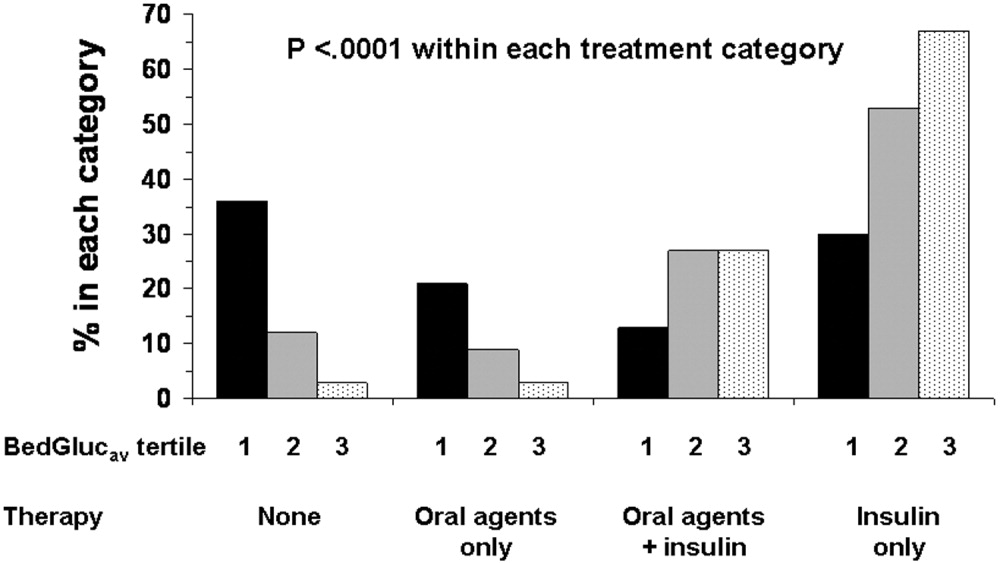
Among insulin users, 58% received bolus‐only, 42% received basal‐bolus, and 1% received basal‐only injections. Because of the small proportion of basal‐only patients, we conducted analyses only of patients whose insulin treatment fell into 1 of the first 2 categories. The use of a basal‐bolus insulin program increased from 34% in patients whose BedGlucavg was in the first tertile to 54% for those who had BedGlucavg in the third tertile (P < .001; Fig. 4, left). Thus, although there was a greater transition to a more intensive insulin regimen with worsening hyperglycemia, a substantial number of patients (46%) whose BedGlucavg was in the third tertile still did not have their insulin regimen intensified to a basal‐bolus program.
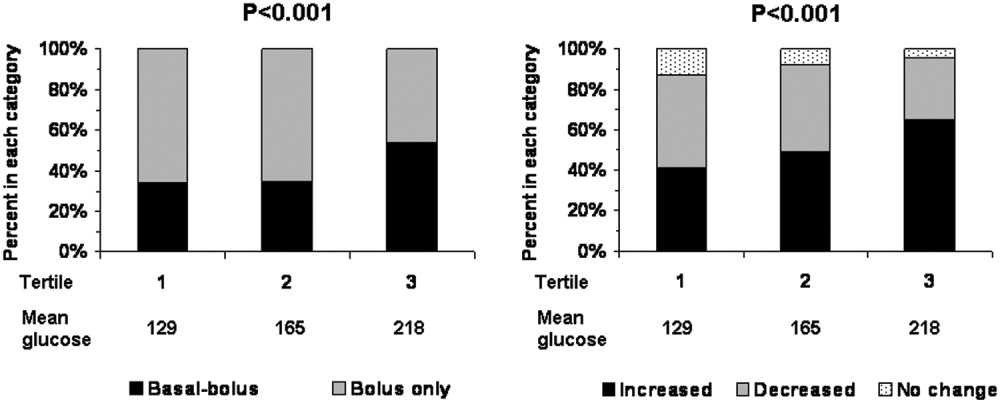
Fifty‐four percent of subcutaneous insulin users (N = 1680) had an increase in the amount of insulin administered between the first and last 24 hours of hospitalization (average increase, 17 U), 39% had a decrease (average decrease, 12 U), and 7% had no change. With rising hyperglycemia, more patients had their insulin increased by the time of discharge; 41% of persons who had BedGlucavg values in the first tertile were on more insulin by the time of discharge, whereas 65% of those who had average glucose values in the third tertile had insulin increased (Fig. 4, right). However, the pattern of changes in the amount of administered insulin was heterogeneous, with increases, decreases, and no change occurring in all tertiles of BedGlucavg (Fig. 3, right). Nearly 31% of patients whose BedGlucavg values were in the third tertile actually had a decrease in insulin. This decrease occurred despite evidence of a low frequency of hypoglycemia (only 1.2 values < 70 mg/dL per 100 measurements per person) and a high frequency of hyperglycemia (55.4 values > 200 mg/dL per person per 100 measurements).
DISCUSSION
The number of diabetes‐associated hospital discharges has been climbing2, 3; our own data indicate an increase in the number of patients with diabetes as a proportion of the total number of discharged patients. A recent consensus advocates good glucose control in the hospital to optimize outcomes,79 and institutions need to begin the process of assessing their quality of inpatient hyperglycemia management as a first step to enhancing care.
There are no guidelines about which method of glucose measurement (ie, blood glucose or bedside glucose) should be used as the quality measure to evaluate glycemic control in hospital patients. Both blood and bedside glucose measurements have been used in outcomes studies.23, 24 We analyzed capillary bedside values measured by a method subjected to ongoing quality control oversight and stored in the electronic laboratory database. Bedside glucose measurements are typically obtained with far greater frequency than blood glucose measurements and therefore provide better insight into daily changes in glycemic control; in practice, clinicians rely on bedside values when assessing hyperglycemia and making therapeutic decisions.
There is also no consensus about what glucose metric should be used to assess the status of glycemic control in the hospital. Some studies have used single glucose values to examine the relationship between hyperglycemia and outcomes,25, 26 whereas others have used values averaged over various lengths of time.24, 27 To evaluate glucose control, we averaged capillary measurements in the first 24 hours of hospitalization (F24BedGlucavg), the last 24 hours of hospitalization (L24BedGlucavg), and for the entire LOS (BedGlucavg), and we calculated the number of documented hyper‐ and hypoglycemic events. The measures we used to examine hyperglycemia would serve as useful benchmarks for following the progress of future institutional interventions directed at glucose control in hospitalized patients at our hospital.
A substantial number of our patients selected for analysis (ie, noncritically ill with LOS 3 days) were found to have sustained hyperglycemia at the beginning, during, and at the end of their hospital stay. We found very few instances of severe hypoglycemia (values < 50 or < 40 mg/dL), and the low frequency of hypoglycemia compared to that of hyperglycemia could encourage practitioners to be more aggressive in treating hyperglycemia. The high frequency of recorded bedside glucose compared with blood glucose measurements ( 3 per day), the ongoing patient surveillance by medical, nursing, and other staff members, and our institution's written hypoglycemia policy most likely minimize the number of unobserved, undocumented, or untreated hypoglycemic episodes. There are no data or recommendations about what would be an acceptable number of hypoglycemic episodes in the hospital.
Very little is known about the therapeutic strategies being applied to hyperglycemia in the hospital. Our data show that subcutaneous insulin (either alone or in combination with oral agents) was used at some point during hospitalization for nearly three‐fourths of noncritically patients who were in the hospital for 3 days or longer. Moreover, as hyperglycemia worsened, use of oral hypoglycemic agents declined, there was a shift toward greater use of a scheduled basal‐bolus insulin program, and a greater proportion of patients had more insulin administered.
Although these latter findings are encouraging and suggest that practitioners are responding to the severity of hyperglycemia, further examination of the data suggests that a substantial number of patients in the highest glucose tertile did not have insulin therapy intensified. Nearly half our patients whose glucose values were in the highest tertile were treated with short‐acting insulin aloneprobably an ineffective regimen23, 28or did not have more insulin administered. The higher doses administered were not likely solely a result of using more sliding‐scale insulin, as previous investigators actually found no correlation between intensity of the sliding scale and total daily insulin dose.14 Although evidence here is circumstantial (we did not examine changes in provider orders in response to glucose levels), these findings, together with those in our previous study15 and in another study,14 provide indirect evidence of clinical inertia in the hospital.
Beyond clinical inertia, however, there was evidence of negative therapeutic momentum: nearly one‐third of patients whose glucose was in the highest tertile had insulin decreased rather than increased, despite the low frequency of hypoglycemia and the high frequency of hyperglycemia. It is likely that even a single episode of hypoglycemia concerned practitioners, but the clinical response in these situations should be to investigate and correct the circumstances leading to the hypoglycemia, rather than to necessarily deintensify therapy in the face of continued hyperglycemia. The analysis of this larger data set corroborated our observations of clinical inertia and negative therapeutic momentum from an earlier study of chart reviews of a smaller patient sample.15
The variable application of insulin therapy to the treatment of hyperglycemia may be an indication of the level of comfort practitioners have about using this pharmacologic agent. A recently completed survey of resident physicians at our institution indicated that understanding how to use insulin was the most common barrier to successful management of inpatient hyperglycemia.29 These observations reinforce the need for institutions to develop standardized insulin order sets and develop programs to educate the staff on the use of insulin.
This study differs from our original analysis based on chart review in 4 ways. First, the sample size in our first study (n = 90) was small and derived from discharges from a single year (2003), whereas the sample in the present study spanned several years and included several thousand cases. Second, in our prior study we did not have detailed pharmacologic data on glucose management and how treatment approaches varied relative to severity of hyperglycemia. In general, there is very limited data on what therapeutic strategies are being applied to inpatient hyperglycemia, and this analysis of a large sample of cases provides more insight into how practitioners are managing glucose.
Third, we wanted to corroborate observations made in our previous report using a different methodologyin this instance, adapting existing information systems to assessment of inpatient diabetes care. For example, our last study was based on a limited number of glucose observations but suggested that the prevalence of hypoglycemia in our hospital was low compared with that of hyperglycemia; the present analysis of a very large number of glucose values confirmed these initial findings. In addition, use of information systems versus a chart review approach to assessing inpatient diabetes care corroborates our earlier suspicions about the presence of clinical inertia and negative therapeutic momentum in glucose management.
Fourth and finally, this study gave us experience with use of electronic records as a means to assess the status of inpatient diabetes care. Electronic data sources will likely be common tools to monitor quality of inpatient diabetes care and will likely figure prominently in future accreditation processes.10, 11 Unlike chart abstraction, which would require extensive man‐hours to extract data on few patients, use of electronic records allows examination of large numbers of hospital cases. Queries of information systems could be automated, and report cards potentially generated and feedback given to providers on the status of inpatient glycemic control. The industry is actively pursuing software development to assist hospitals in assessing the quality of inpatient glycemic control (eg, RALS‐TGCM, available at
However, there are also limitations to using electronic records as the sole method of assessing inpatient diabetes care. For instance, retrospective review of electronic records does not allow assessment of reasons underlying decision‐making behavior of clinicians (eg, why they did or did not change therapy). Diabetes and hyperglycemia associated hospitalizations must be identified by discharge diagnosis codes, so some cases of diabetes and hyperglycemia were likely missed.30, 31 Recent guidelines propose preprandial targets for glucose in the hospital.8 It is not easy to determine from an electronic data source which is a preprandial bedside glucose and which is a postprandial bedside glucose. Pre‐ and postpyramidal glucose categories would be difficult to define even during prospective studies, given the varying nature of nutritional support (ie, enteral, parenteral) used in the hospital and the administration of continuous dextrose infusions. Some type of quality control, such as conducting reviews of small samples of randomly selected charts to see how they compare with the electronic data, will need to be conducted.
From electronic discharge data, we cannot establish who had preexisting diabetes, who was admitted with new‐onset diabetes, and who developed hyperglycemia as a result of the hospital stay. Our previous random chart review15 indicated it is likely that most (more than 90%) had an established diagnosis of diabetes before admission. However, the recommendation to treat hyperglycemia should apply to all patients regardless of whether they had diagnosed diabetes prior to hospitalization or manifested hyperglycemia only during the hospital stay.79
As hospitals move toward making efforts to improve performance related to treating inpatient hyperglycemia, they must be cognizant of the heterogeneity of the inpatient population and the challenges to managing hospital hyperglycemia before drawing conclusions about their management. Inpatients with hyperglycemia are a diverse group, comprising patients with preexisting diabetes, with previously undiagnosed diabetes, and stress‐caused hyperglycemia. The unpredictable timing of procedures, various and changing forms of nutritional support, and different levels of staff expertise all contribute to the challenges of managing inpatient hyperglycemia. Inpatient practitioners may be forced to attempt glycemic control catch‐up for hospitalized persons who had poor outpatient glucose control. Patients who have required a stay in the intensive care unit may have very different glycemic outcomes than those who have not. Patients whose LOS was short (< 3days) may have different glycemic outcomes than persons whose LOS was longer ( 3 days as defined here) because of the length of time practitioners have to work to control their hyperglycemia. These and other variables may have to be taken into account when developing and assessing the impact of interventions.
Despite these limitations, our analysis was helpful in providing direction for enhancing the care of hospitalized patients with hyperglycemia in our facility. For instance, our generalists and surgeons are the principal caretakers of noncritically ill patients with diabetes, and these practitioners could be targeted for the first continuing educational programs about inpatient care of hyperglycemia. In addition, institutional guidelines on when and how to initiate and change therapyparticularly insulincan be designed so that hyperglycemia in noncritically ill hospital patients can be managed more effectively. These and other ongoing educational initiatives are necessary to ensure delivery of the highest quality of inpatient glucose care.
Diabetes confers a substantial burden on the hospital system. Diabetes is the fourth‐leading comorbid condition associated with any hospital discharge in the United States1. During 2001, for more than 500,000 patients discharged from U.S. hospitals diabetes was listed as the principal diagnosis and for more than 4 million it was listed as a codiagnosis.2, 3 Nearly one‐third of diabetes patients require at least 2 hospitalizations annually,4 and inpatient stays account for the largest proportion of direct medical expenses incurred by persons with the disease.5
Numerous studies have demonstrated that hyperglycemia is associated with adverse outcomes of hospitalized patients.68 However, studies have also confirmed that attention to lowering glucose levels in the hospital improves patient outcomes.7, 8 Although inpatients with known diabetes will likely constitute the largest and most visible percentage of those who will require treatment for high glucose, the recommendation to control glucose applies to all inpatients regardless of whether they have been diagnosed with diabetes prior to hospitalization or have manifested hyperglycemia only during the hospital stay.79
Now that the relationship between hyperglycemia and hospital outcomes is well established, the task of organizations that deliver care and set policy is to translate current recommendations of good glucose control into real‐world hospital settings. Quality improvement organizations are currently working toward developing and disseminating performance measures for control of inpatient hyperglycemia.10, 11 Although management of hospital hyperglycemia is often perceived as suboptimal,12 actual data are limited and are based on review of small numbers of charts,1315 and information is even sparser on the pharmacologic strategies being used to treat inpatient hyperglycemia. Before educational programs and policies can be developed, individual hospital systems need to gain more insight into how hyperglycemia is being managed in the hospital.
We reported previously the results of a review of a small number of charts (n = 90) of patients hospitalized with diabetes. The findings from this review suggested there was clinical inertia in glycemia management in the hospital.15 Clinical inertia was originally described in relationship to diabetes care in the outpatient setting and was defined as a failure to perform a needed service or make a change in treatment when indicated.16, 17 Since the original description, additional reports have documented the problem of clinical inertia, but these have all been based on experiences in the outpatient setting.1822 To our knowledge, our previous report was the first to question whether clinical inertia occurred in the hospital environment. In addition, we described the negative therapeutic momentuma deintensification of treatment despite ongoing hyperglycemia15. However, our prior study examined only a small number of cases and did not include detailed data on pharmacologic treatment for hyperglycemia. Therefore, we expanded our analysis using an information systems rather than a chart reviewbased methodology to assess the status of hyperglycemia management in our hospital.
METHODS
Setting
Our tertiary‐care academic teaching hospital is a 200‐bed facility in metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented, including transplantation services; the hospital also has a level 2 trauma center and an inpatient rehabilitation unit. Care is provided by various types of practitioners, including postgraduate trainees, faculty, physician assistants, and nurse‐practitioners. An electronic medical record links outpatient and inpatient records with laboratory results and pharmacy orders. The core electronic health record system is the Centricity/LastWord platform, provided by GE/IDX. The ancillary core systems, including laboratory and pharmacy, are interfaced with the Centricity system and maintained by on‐site Mayo Clinic information technology professionals.
Case Selection
Patients discharged with an International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9‐CM) diagnosis code for diabetes (ICD‐9‐CM code 250.xx) or hyperglycemia (ICD‐9‐CM code 790.6) were identified in a search of the hospital's electronic billing records.24 Our facility does not provide obstetric or pediatric services; therefore, corresponding ICD‐9‐CM codes for those populations were not included. Both primary and nonprimary diagnostic fields were searched. Discharges were extracted for the period between January 1, 2001, and December 31, 2004. Data retrieved included patient age, ethnicity/race, length of stay (LOS), and type of hospital service with primary responsibility for the patient's care. For confidentiality reasons, individual patients were not identified, and the unit of analysis was the discharge.
Our analyses focused principally on the noncritically ill, defined as those patients who did not require a stay in our intensive or intermediate care units; critically ill patients were identified based on room location in the data set and excluded. The reasons this study assessed hyperglycemia management in the noncritically ill were 2‐fold. First, the critically ill may migrate in and out of intensive care depending on their health status and thus experience different intensities of glucose management. Second, in our facility the therapeutic approach to hyperglycemia management is different for the critically ill than for the noncritically ill; the critically ill may receive intravenous and/or subcutaneous insulin, whereas subcutaneous insulin therapy only is given to the noncritically ill. Thus, the noncritically ill represent a more clearly defined patient population whose therapies would be easier to evaluate. We also restricted the final analysis to patients who had a LOS of 3 days or less, so that differences in glucose control and insulin therapy between the first and last 24 hours of hospital stay could be assessed.
Data on 30 randomly chosen patients from different years was extracted from electronic records. A spreadsheet of the data was compared against data in our online electronic medical records. The online data were printed, and packets were made of the data for each patient selected for review. The patient demographic information was validated against our registration screen. Inpatient stay was validated to verify a patient was in intensive or intermediate care. The result of each glucose test performed while the patient was in the hospital was printed and the calculations validated. The insulin given while the patient was hospitalized was also printed and reviewed to verify the type of insulin and calculations for the amounts of insulin given.
Assessment of Glycemic Control
After extraction of hospital cases, data were linked via patient identifiers to our electronic laboratory database to retrieve information on glucose values. Glucose data included both blood and bedside measurements. In our institution, bedside glucose monitoring is performed with an instrument that scans and records patient identification, followed by direct downloading to our laboratory database. Commercial software (Medical Automation Systems, Charlottesville, VA) facilitates the interfacing of glucometer data with the electronic laboratory file.
Nearly all hospitalized patients had either bedside glucose (84%) or blood glucose (86%) data available for analysis. However, the mean number of bedside glucose measurements was 3.4 per day, whereas the average number of blood glucose measurements was only 1.0 per day. Because of the greater number of bedside measurements and because practitioners typically make therapeutic decisions about hyperglycemia management on the basis of daily bedside glucose results, these values were used to assess glycemic control of patients in the hospital discharge data.15
To assess glycemic control, we used methods similar to those previously published by ourselves and others.15, 23 We averaged each patient's available bedside glucose measurements to determine the composite average (BedGlucavg). We also computed the average of bedside glucose measurements obtained during the first 24 hours after admission (F24BedGlucavg) and during the last 24 hours before discharge (L24BedGlucavg), then examined the distributions of BedGlucavg, F24BedGlucavg, and L24BedGlucavg. The first 24‐hour period was calculated forward from the recorded time of admission, and the last 24‐hour period was calculated backward from the time of discharge. We calculated the frequency that each patient's bedside measurements showed hypoglycemia (bedside glucose < 70, < 60, < 50, or < 40 mg/dL) and showed hyperglycemia (bedside glucose >2 00, > 250, > 300, > 350, or > 400 mg/dL). Results were recorded as the number of values per 100 measurements per person; this method allowed adjustment for variation in the individual number of measurements and captured information on multiple episodes of hypo‐ or hyperglycemia of individual patients.15, 23
Hyperglycemia Therapy
Links to our inpatient pharmacy database enabled determination of types of pharmacotherapy actually administered to patients to treat hyperglycemia. Our electronic pharmacy records are designed so that intravenous medications (eg, intravenous insulin), scheduled oral and subcutaneous medications (eg, subcutaneous insulin), and medications administered on a one‐time or as‐needed basis (eg, sliding‐scale insulin) are documented electronically as separate categories. In our facility, intravenous insulin is administered only in the intensive care setting or as a component of total parenteral nutrition, and we excluded intravenous insulin use from this data. Thus, our analysis of insulin therapy focused only on elucidating patterns of subcutaneous treatment.
We classified hyperglycemia treatment as no therapy, oral agents only, oral agents plus insulin, and insulin only. Patients were regarded as having received an oral agent or insulin if they were administered the medication at any time during their inpatient stay. For management of hyperglycemia in noncritically ill patients, the use of a programmed basal‐bolus insulin program is advocated rather than the use of only a short‐acting bolus or sliding‐scale regimen.7, 8 Therefore, we further examined the insulin treatment strategies by classifying the type of regimen as basal only (if only an extended‐release preparation was used), as basal bolus (if the therapy consisted of a long‐acting plus a short‐acting formulation), or as bolus only (if the only insulin administered was a short‐acting preparation).
In addition to characterizing the general therapeutic approaches to hyperglycemia, we determined changes in the amount of insulin administered according to the severity of the hyperglycemia. Among patients who received insulin, we compared the average total units of insulin used during the last 24 hours before discharge with the amount administered during the first 24 hours of hospitalization. If more units were used during the last 24 hours than in the first 24 hours, the amount of insulin administered was categorized as having increased; if fewer units were provided during the last 24 hours, then the insulin amount was classified as having decreased; otherwise, no change was considered to have occurred. The BedGlucavg values were divided into 3 intervals using tertile cut points, and the differences in the proportion of patients by each type of insulin treatment regimen and the categories of insulin change were compared across tertiles; differences in proportions were determined using the 2 statistic.
RESULTS
Patient Characteristics
Between January 1, 2001, and December 31, 2004, a total of 7361 patients were discharged from our facility with either a diabetes or a hyperglycemia diagnosis (16% of all discharges); the percentage of discharges associated with these diagnoses increased from 14.9% in 2001 to 16.4% in 2004. Most patients with diabetes or hyperglycemia (5198 or 71%) received care outside the intensive‐ or intermediate‐care setting.
Among the noncritically ill patients whose LOS was at least 3 days (N = 2916), average age was 69 years, and average LOS was 5.7 days. Most of the discharged patients were men (57%), and 90% were white. Most patients were discharged from primary care (45%; general internal medicine or family medicine) or surgical services (34%), with the rest discharged from other specialties (eg, cardiology, transplant medicine). Compared to the noncritically ill, who had an LOS of at least 3 days, those noncritically patients whose LOS was less than 3 days (n = 2282) were slightly younger (mean age 68 versus 69 years, P < .001 by Mann‐Whitney testing) but were comparable in sex and race distribution (P > .07 for both by chi‐square testing).
Glycemic Control
The median duration between admission and time of first bedside glucose measurement was 3.0 hours. Patients had an average of 19 bedside glucose measurements; the overall mean number of bedside measurements was 3.4 per day, 3.7 during the first 24‐hour period, and 3.4 during the last 24 hours of hospitalization. Nearly 25% of patients were hyperglycemic (bedside glucose > 200 mg/dL) during the first 24 hours of hospitalization (Fig. 1A), 20% had persistent hyperglycemia throughout the entire hospitalization (Fig. 1B), and 21% were hyperglycemic during the 24 hours before discharge (Fig. 1C), with some patients discharged with an average bedside glucose of at least 300 mg/dL during the 24 hours before discharge.
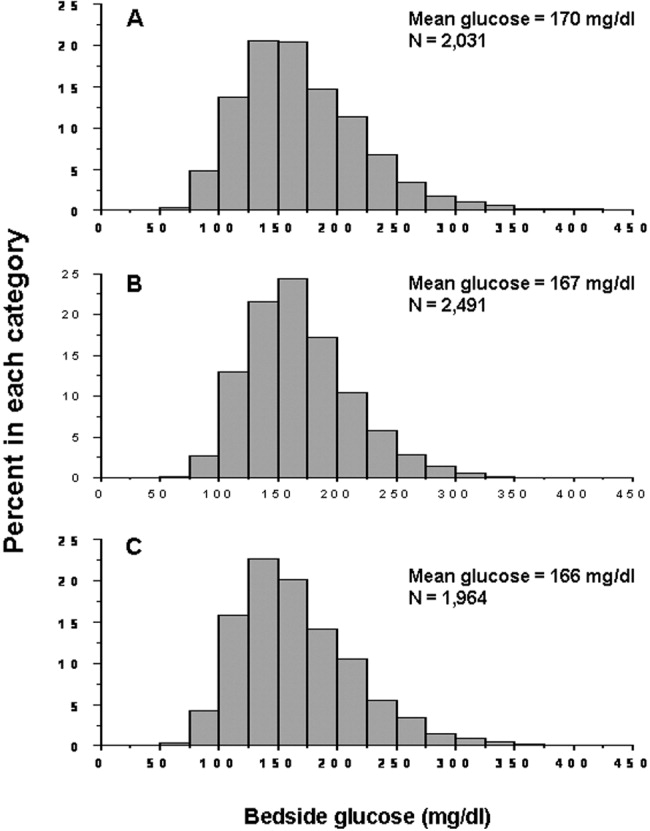
The incidence of hypoglycemic episodes was lower than that of hyperglycemic episodes: 21% of patients had at least 1 bedside glucose value less than 70 mg/dL, but 68% had at least 1 value greater than 200 mg/dL. The frequency of hypoglycemic measurements was low (Fig. 2A) compared with the frequency of hyperglycemic episodes (Fig. 2B).
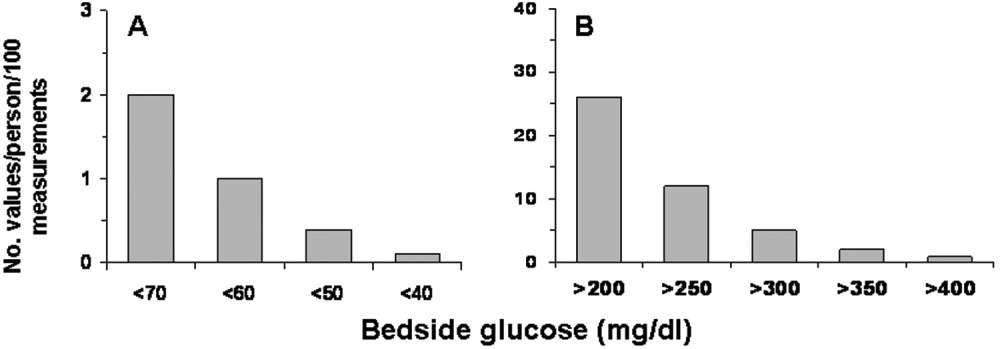
Hyperglycemia Therapy
Most patients (72%) received subcutaneous insulin at some point during their hospital stay; 19% had no therapy, 9% had oral agents only, 26% had oral agents plus insulin, and 46% had insulin only. The proportion receiving no therapy decreased from 32% among patients whose BedGlucavg was in the first tertile to 2% in the third tertile; the percentage of patients taking oral agents only decreased from 18% to 1%; the proportion taking oral agents plus insulin was 17% in the first tertile and 30% in the third; and the proportion of those taking insulin only was 32% in the first tertile and 66% in the third (Fig. 3). Thus, nearly all patients whose BedGlucavg value was in the third tertile received insulin, either as monotherapy or in combination with oral agents.
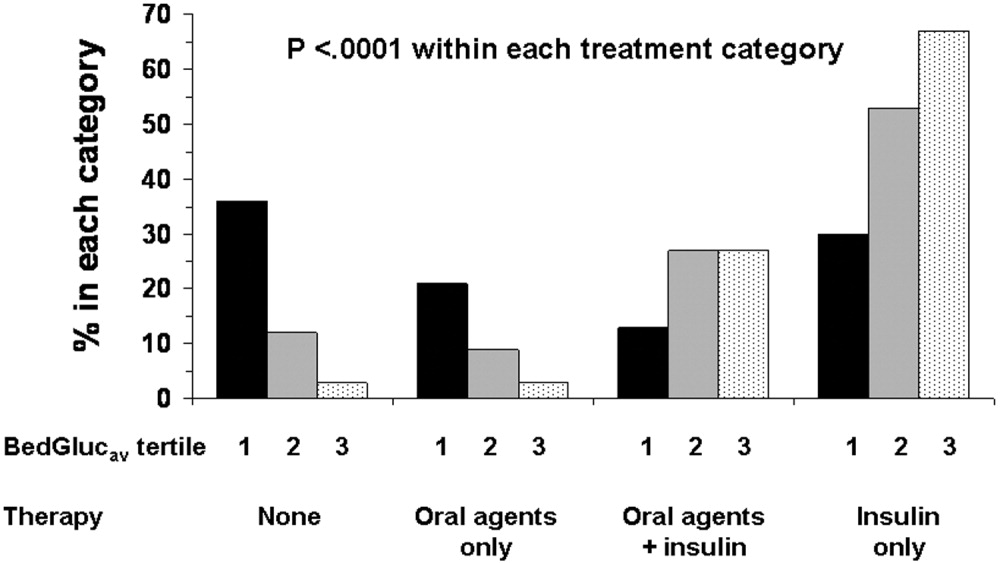
Among insulin users, 58% received bolus‐only, 42% received basal‐bolus, and 1% received basal‐only injections. Because of the small proportion of basal‐only patients, we conducted analyses only of patients whose insulin treatment fell into 1 of the first 2 categories. The use of a basal‐bolus insulin program increased from 34% in patients whose BedGlucavg was in the first tertile to 54% for those who had BedGlucavg in the third tertile (P < .001; Fig. 4, left). Thus, although there was a greater transition to a more intensive insulin regimen with worsening hyperglycemia, a substantial number of patients (46%) whose BedGlucavg was in the third tertile still did not have their insulin regimen intensified to a basal‐bolus program.
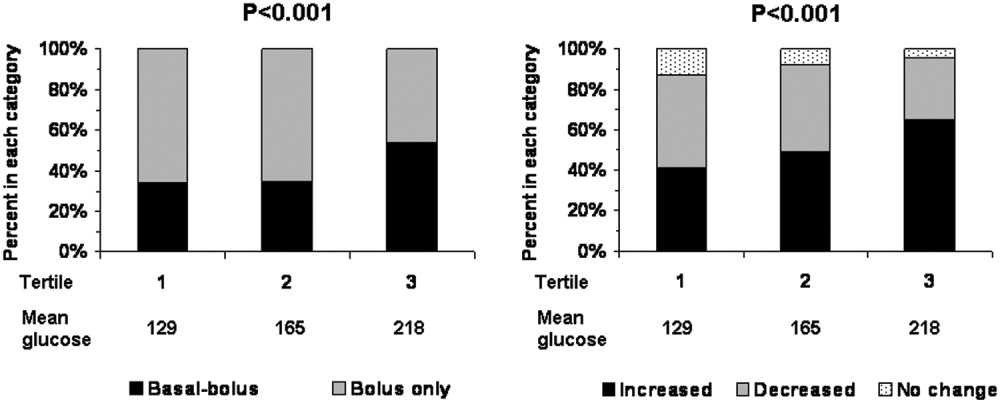
Fifty‐four percent of subcutaneous insulin users (N = 1680) had an increase in the amount of insulin administered between the first and last 24 hours of hospitalization (average increase, 17 U), 39% had a decrease (average decrease, 12 U), and 7% had no change. With rising hyperglycemia, more patients had their insulin increased by the time of discharge; 41% of persons who had BedGlucavg values in the first tertile were on more insulin by the time of discharge, whereas 65% of those who had average glucose values in the third tertile had insulin increased (Fig. 4, right). However, the pattern of changes in the amount of administered insulin was heterogeneous, with increases, decreases, and no change occurring in all tertiles of BedGlucavg (Fig. 3, right). Nearly 31% of patients whose BedGlucavg values were in the third tertile actually had a decrease in insulin. This decrease occurred despite evidence of a low frequency of hypoglycemia (only 1.2 values < 70 mg/dL per 100 measurements per person) and a high frequency of hyperglycemia (55.4 values > 200 mg/dL per person per 100 measurements).
DISCUSSION
The number of diabetes‐associated hospital discharges has been climbing2, 3; our own data indicate an increase in the number of patients with diabetes as a proportion of the total number of discharged patients. A recent consensus advocates good glucose control in the hospital to optimize outcomes,79 and institutions need to begin the process of assessing their quality of inpatient hyperglycemia management as a first step to enhancing care.
There are no guidelines about which method of glucose measurement (ie, blood glucose or bedside glucose) should be used as the quality measure to evaluate glycemic control in hospital patients. Both blood and bedside glucose measurements have been used in outcomes studies.23, 24 We analyzed capillary bedside values measured by a method subjected to ongoing quality control oversight and stored in the electronic laboratory database. Bedside glucose measurements are typically obtained with far greater frequency than blood glucose measurements and therefore provide better insight into daily changes in glycemic control; in practice, clinicians rely on bedside values when assessing hyperglycemia and making therapeutic decisions.
There is also no consensus about what glucose metric should be used to assess the status of glycemic control in the hospital. Some studies have used single glucose values to examine the relationship between hyperglycemia and outcomes,25, 26 whereas others have used values averaged over various lengths of time.24, 27 To evaluate glucose control, we averaged capillary measurements in the first 24 hours of hospitalization (F24BedGlucavg), the last 24 hours of hospitalization (L24BedGlucavg), and for the entire LOS (BedGlucavg), and we calculated the number of documented hyper‐ and hypoglycemic events. The measures we used to examine hyperglycemia would serve as useful benchmarks for following the progress of future institutional interventions directed at glucose control in hospitalized patients at our hospital.
A substantial number of our patients selected for analysis (ie, noncritically ill with LOS 3 days) were found to have sustained hyperglycemia at the beginning, during, and at the end of their hospital stay. We found very few instances of severe hypoglycemia (values < 50 or < 40 mg/dL), and the low frequency of hypoglycemia compared to that of hyperglycemia could encourage practitioners to be more aggressive in treating hyperglycemia. The high frequency of recorded bedside glucose compared with blood glucose measurements ( 3 per day), the ongoing patient surveillance by medical, nursing, and other staff members, and our institution's written hypoglycemia policy most likely minimize the number of unobserved, undocumented, or untreated hypoglycemic episodes. There are no data or recommendations about what would be an acceptable number of hypoglycemic episodes in the hospital.
Very little is known about the therapeutic strategies being applied to hyperglycemia in the hospital. Our data show that subcutaneous insulin (either alone or in combination with oral agents) was used at some point during hospitalization for nearly three‐fourths of noncritically patients who were in the hospital for 3 days or longer. Moreover, as hyperglycemia worsened, use of oral hypoglycemic agents declined, there was a shift toward greater use of a scheduled basal‐bolus insulin program, and a greater proportion of patients had more insulin administered.
Although these latter findings are encouraging and suggest that practitioners are responding to the severity of hyperglycemia, further examination of the data suggests that a substantial number of patients in the highest glucose tertile did not have insulin therapy intensified. Nearly half our patients whose glucose values were in the highest tertile were treated with short‐acting insulin aloneprobably an ineffective regimen23, 28or did not have more insulin administered. The higher doses administered were not likely solely a result of using more sliding‐scale insulin, as previous investigators actually found no correlation between intensity of the sliding scale and total daily insulin dose.14 Although evidence here is circumstantial (we did not examine changes in provider orders in response to glucose levels), these findings, together with those in our previous study15 and in another study,14 provide indirect evidence of clinical inertia in the hospital.
Beyond clinical inertia, however, there was evidence of negative therapeutic momentum: nearly one‐third of patients whose glucose was in the highest tertile had insulin decreased rather than increased, despite the low frequency of hypoglycemia and the high frequency of hyperglycemia. It is likely that even a single episode of hypoglycemia concerned practitioners, but the clinical response in these situations should be to investigate and correct the circumstances leading to the hypoglycemia, rather than to necessarily deintensify therapy in the face of continued hyperglycemia. The analysis of this larger data set corroborated our observations of clinical inertia and negative therapeutic momentum from an earlier study of chart reviews of a smaller patient sample.15
The variable application of insulin therapy to the treatment of hyperglycemia may be an indication of the level of comfort practitioners have about using this pharmacologic agent. A recently completed survey of resident physicians at our institution indicated that understanding how to use insulin was the most common barrier to successful management of inpatient hyperglycemia.29 These observations reinforce the need for institutions to develop standardized insulin order sets and develop programs to educate the staff on the use of insulin.
This study differs from our original analysis based on chart review in 4 ways. First, the sample size in our first study (n = 90) was small and derived from discharges from a single year (2003), whereas the sample in the present study spanned several years and included several thousand cases. Second, in our prior study we did not have detailed pharmacologic data on glucose management and how treatment approaches varied relative to severity of hyperglycemia. In general, there is very limited data on what therapeutic strategies are being applied to inpatient hyperglycemia, and this analysis of a large sample of cases provides more insight into how practitioners are managing glucose.
Third, we wanted to corroborate observations made in our previous report using a different methodologyin this instance, adapting existing information systems to assessment of inpatient diabetes care. For example, our last study was based on a limited number of glucose observations but suggested that the prevalence of hypoglycemia in our hospital was low compared with that of hyperglycemia; the present analysis of a very large number of glucose values confirmed these initial findings. In addition, use of information systems versus a chart review approach to assessing inpatient diabetes care corroborates our earlier suspicions about the presence of clinical inertia and negative therapeutic momentum in glucose management.
Fourth and finally, this study gave us experience with use of electronic records as a means to assess the status of inpatient diabetes care. Electronic data sources will likely be common tools to monitor quality of inpatient diabetes care and will likely figure prominently in future accreditation processes.10, 11 Unlike chart abstraction, which would require extensive man‐hours to extract data on few patients, use of electronic records allows examination of large numbers of hospital cases. Queries of information systems could be automated, and report cards potentially generated and feedback given to providers on the status of inpatient glycemic control. The industry is actively pursuing software development to assist hospitals in assessing the quality of inpatient glycemic control (eg, RALS‐TGCM, available at
However, there are also limitations to using electronic records as the sole method of assessing inpatient diabetes care. For instance, retrospective review of electronic records does not allow assessment of reasons underlying decision‐making behavior of clinicians (eg, why they did or did not change therapy). Diabetes and hyperglycemia associated hospitalizations must be identified by discharge diagnosis codes, so some cases of diabetes and hyperglycemia were likely missed.30, 31 Recent guidelines propose preprandial targets for glucose in the hospital.8 It is not easy to determine from an electronic data source which is a preprandial bedside glucose and which is a postprandial bedside glucose. Pre‐ and postpyramidal glucose categories would be difficult to define even during prospective studies, given the varying nature of nutritional support (ie, enteral, parenteral) used in the hospital and the administration of continuous dextrose infusions. Some type of quality control, such as conducting reviews of small samples of randomly selected charts to see how they compare with the electronic data, will need to be conducted.
From electronic discharge data, we cannot establish who had preexisting diabetes, who was admitted with new‐onset diabetes, and who developed hyperglycemia as a result of the hospital stay. Our previous random chart review15 indicated it is likely that most (more than 90%) had an established diagnosis of diabetes before admission. However, the recommendation to treat hyperglycemia should apply to all patients regardless of whether they had diagnosed diabetes prior to hospitalization or manifested hyperglycemia only during the hospital stay.79
As hospitals move toward making efforts to improve performance related to treating inpatient hyperglycemia, they must be cognizant of the heterogeneity of the inpatient population and the challenges to managing hospital hyperglycemia before drawing conclusions about their management. Inpatients with hyperglycemia are a diverse group, comprising patients with preexisting diabetes, with previously undiagnosed diabetes, and stress‐caused hyperglycemia. The unpredictable timing of procedures, various and changing forms of nutritional support, and different levels of staff expertise all contribute to the challenges of managing inpatient hyperglycemia. Inpatient practitioners may be forced to attempt glycemic control catch‐up for hospitalized persons who had poor outpatient glucose control. Patients who have required a stay in the intensive care unit may have very different glycemic outcomes than those who have not. Patients whose LOS was short (< 3days) may have different glycemic outcomes than persons whose LOS was longer ( 3 days as defined here) because of the length of time practitioners have to work to control their hyperglycemia. These and other variables may have to be taken into account when developing and assessing the impact of interventions.
Despite these limitations, our analysis was helpful in providing direction for enhancing the care of hospitalized patients with hyperglycemia in our facility. For instance, our generalists and surgeons are the principal caretakers of noncritically ill patients with diabetes, and these practitioners could be targeted for the first continuing educational programs about inpatient care of hyperglycemia. In addition, institutional guidelines on when and how to initiate and change therapyparticularly insulincan be designed so that hyperglycemia in noncritically ill hospital patients can be managed more effectively. These and other ongoing educational initiatives are necessary to ensure delivery of the highest quality of inpatient glucose care.
- ,,,.Hospitalization in the United States,1997.Rockville, MD:Agency for Healthcare Research and Quality;2000. Report No.: HCUP Fact Book No. 1; AHRQ Publication No. 00‐0031.
- Hospitalization for Diabetes as First‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmfirst/index.htm. Accessed November 29,2006.
- Hospitalizations for Diabetes as Any‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmany/index.htm. Accessed November 29,2006,
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26:1421–1426.
- ,,.Economic costs of diabetes in the US in 2002.Diabetes Care.2003;26:917–932.
- ,,.Inpatient diabetology. The new frontier.J Gen Intern Med.2004;19:466–471.
- ,,, et al.American Diabetes Association Diabetes in Hospitals Writing Committee: Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ACE Task Force on Inpatient Diabetes and Metabolic Control.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract,2004;10:77–82.
- ACE/ADA Task Force on Inpatient Diabetes.American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control.Endocr Pract.2006;12:459–468.
- Getting started kit: prevent surgical site infections.2006 Available at: www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed November 29,year="2006"2006.
- Joint Commission on Accreditation of Healthcare Organizations. American Diabetes Association and Joint Commission Collaborate on Joint Commission Inpatient Diabetes Care Certification.2006. Available at: http://www.jointcommission.org/NewsRoom/NewsReleases/jc_nr_072006.htm. Accessed November 29,year="2006"2006,
- ,.Glycemic chaos (not glycemic control) still the rule for inpatient care: How do we stop the insanity?J Hosp Med.2006;1:141–144.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21(2):246–249.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1(3):145–150.
- ,,, et al.Diabetes care in the non‐ICU setting: is there clinical inertia in the hospital?J Hosp Med,2006;1(3):151–160.
- ,,, et al.Diabetes in urban African‐Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes.Diabetes Care.1999;22:1494–500.
- ,,, et al.Clinical Inertia.Ann Intern Med.2001;135:825–834.
- ,,,Team UHCUDBP.Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change.Diabetes Care.2005;28:337–442.
- ,,, et al.Clinical inertia in the management of type 2 diabetes metabolic risk factors.Diabet Med,2004;21:150–155.
- ,.Clinical inertia: errors of omission in drug therapy.Am J Health Syst Pharm.2004;61:401–404.
- .Overcome clinical inertia to control systolic blood pressure.Arch Intern Med,2003;163:2677–2678.
- ,,,,.Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians?Diabetes Care.2005;28:600–606.
- ,,.Glycemic Control and Sliding Scale Insulin Use in Medical Inpatients With Diabetes Mellitus.Arch Intern Med.1997;157:545–552.
- ,,.Effect of hyperglycemia and continuous intraveneous insulin infusions on outcomes of cardiac surgical procedures: the Portland Diabetic Project.Endocr Pract.2004;10(2):21–33.
- ,,, et al.Plasma glucose at hospital admission and previous metabolic control determine myocardial infarct size and survival in patients with and without type 2 diabetes: the Langendreer Myocardial Infarction and Blood Glucose in Diabetic Patients Assessment (LAMBDA).Diabetes Care.2005;28:2551–2553.
- ,,.Admission hyperglycemia as a prognostic indicator in trauma.J Trauma Inj Infect Crit Care.2003;55(1):33–38.
- ,,, et al.Intraoperative hyperglycemia and perioperative outcomes in cardiac surgery patients.Mayo Clin Proc.2005;80:862–866.
- ,,,,.Efficacy of sliding‐scale insulin therapy: a comparison with prospective regimens.Fam Pract Res J.1994;14:313–22.
- ,,, et al.Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians.Endocr Pract., to appear.
- ,,,,.Diabetes‐related hospitalization and hospital utilization. In:Diabetes in America.Bethesda, MD:National Institutes of Diabetes and Digestive Diseases;1995:553–563.
- ,,, et al.Hospital discharge records under‐report the prevalence of diabetes in inpatients.Diabetes Res Clin Pract.2003;59(2):145–151.
- ,,,.Hospitalization in the United States,1997.Rockville, MD:Agency for Healthcare Research and Quality;2000. Report No.: HCUP Fact Book No. 1; AHRQ Publication No. 00‐0031.
- Hospitalization for Diabetes as First‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmfirst/index.htm. Accessed November 29,2006.
- Hospitalizations for Diabetes as Any‐Listed Diagnosis. Available at: http://www.cdc.gov/diabetes/statistics/dmany/index.htm. Accessed November 29,2006,
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26:1421–1426.
- ,,.Economic costs of diabetes in the US in 2002.Diabetes Care.2003;26:917–932.
- ,,.Inpatient diabetology. The new frontier.J Gen Intern Med.2004;19:466–471.
- ,,, et al.American Diabetes Association Diabetes in Hospitals Writing Committee: Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591.
- ACE Task Force on Inpatient Diabetes and Metabolic Control.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract,2004;10:77–82.
- ACE/ADA Task Force on Inpatient Diabetes.American College of Endocrinology and American Diabetes Association consensus statement on inpatient diabetes and glycemic control.Endocr Pract.2006;12:459–468.
- Getting started kit: prevent surgical site infections.2006 Available at: www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed November 29,year="2006"2006.
- Joint Commission on Accreditation of Healthcare Organizations. American Diabetes Association and Joint Commission Collaborate on Joint Commission Inpatient Diabetes Care Certification.2006. Available at: http://www.jointcommission.org/NewsRoom/NewsReleases/jc_nr_072006.htm. Accessed November 29,year="2006"2006,
- ,.Glycemic chaos (not glycemic control) still the rule for inpatient care: How do we stop the insanity?J Hosp Med.2006;1:141–144.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21(2):246–249.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1(3):145–150.
- ,,, et al.Diabetes care in the non‐ICU setting: is there clinical inertia in the hospital?J Hosp Med,2006;1(3):151–160.
- ,,, et al.Diabetes in urban African‐Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes.Diabetes Care.1999;22:1494–500.
- ,,, et al.Clinical Inertia.Ann Intern Med.2001;135:825–834.
- ,,,Team UHCUDBP.Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change.Diabetes Care.2005;28:337–442.
- ,,, et al.Clinical inertia in the management of type 2 diabetes metabolic risk factors.Diabet Med,2004;21:150–155.
- ,.Clinical inertia: errors of omission in drug therapy.Am J Health Syst Pharm.2004;61:401–404.
- .Overcome clinical inertia to control systolic blood pressure.Arch Intern Med,2003;163:2677–2678.
- ,,,,.Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians?Diabetes Care.2005;28:600–606.
- ,,.Glycemic Control and Sliding Scale Insulin Use in Medical Inpatients With Diabetes Mellitus.Arch Intern Med.1997;157:545–552.
- ,,.Effect of hyperglycemia and continuous intraveneous insulin infusions on outcomes of cardiac surgical procedures: the Portland Diabetic Project.Endocr Pract.2004;10(2):21–33.
- ,,, et al.Plasma glucose at hospital admission and previous metabolic control determine myocardial infarct size and survival in patients with and without type 2 diabetes: the Langendreer Myocardial Infarction and Blood Glucose in Diabetic Patients Assessment (LAMBDA).Diabetes Care.2005;28:2551–2553.
- ,,.Admission hyperglycemia as a prognostic indicator in trauma.J Trauma Inj Infect Crit Care.2003;55(1):33–38.
- ,,, et al.Intraoperative hyperglycemia and perioperative outcomes in cardiac surgery patients.Mayo Clin Proc.2005;80:862–866.
- ,,,,.Efficacy of sliding‐scale insulin therapy: a comparison with prospective regimens.Fam Pract Res J.1994;14:313–22.
- ,,, et al.Management of inpatient hyperglycemia: assessing perceptions and barriers to care among resident physicians.Endocr Pract., to appear.
- ,,,,.Diabetes‐related hospitalization and hospital utilization. In:Diabetes in America.Bethesda, MD:National Institutes of Diabetes and Digestive Diseases;1995:553–563.
- ,,, et al.Hospital discharge records under‐report the prevalence of diabetes in inpatients.Diabetes Res Clin Pract.2003;59(2):145–151.
Copyright © 2007 Society of Hospital Medicine
Hospital Diabetes Care
Persons with diabetes have a greater risk of being hospitalized than do nondiabetic persons,1 and hospitalization was a major contributor to health care utilization and costs of patients with diabetes. In 1997, diabetes was the fourth most common comorbid condition in hospitalized patients nationwide. In 2001 in the United States, 562,000 hospital discharges listed diabetes as a principal diagnosis, and more than 4 million discharges listed diabetes in any diagnostic field.24 Nearly one third of diabetes patients may require 2 or more hospitalizations a year,5 and inpatient stays are the largest expense incurred by persons with this disease.6, 7 A substantial number of hospitalized persons are found to have unrecognized diabetes or to develop hyperglycemia during an inpatient stay.8, 9
The severity of hyperglycemia in the hospital has been linked to numerous adverse outcomes in various clinical situations, and recent studies have demonstrated the potential benefits of achieving good glucose control in the inpatient setting.10, 11 Moreover, specific inpatient‐directed interventions can improve the delivery of diabetes care.1216
Unlike the quality of outpatient diabetes care, which has been extensively profiled,1723 little is actually known about inpatient management. However, earlier reports suggested that hyperglycemia is frequently overlooked by health care personnel.8, 24 To develop intervention and educational programs will require insight into how diabetes is being addressed in the hospital. Thus, we undertook a retrospective chart review of inpatients with a discharge diagnosis of diabetes or hyperglycemia in order to assess whether these conditions were being documented and whether glucose management was being addressed.
METHODS
Setting
Our regional referral, academic teaching hospital is a 200‐bed facility in metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented at this hospital, including renal, liver, and pancreas transplantation, a level‐2 trauma center, and an inpatient rehabilitation unit. Inpatient care is provided either by postgraduate trainees (residents) or through a separate faculty service; physician assistants and nurse‐practitioners also deliver care. Residents may be supervised by either hospitalist or nonhospitalist attendings. An electronic medical record links outpatient and inpatient records, radiology studies, and laboratory results.
Patient Selection
The study was approved by the Mayo Clinic Institutional Review Board. Patients discharged from our facility during 2003 with a diagnosis code from the International Classification of Diseases, 9th revision, Clinical Modification (ICD‐9‐CM) either for diabetes (ICD‐9‐CM code 250.0) or for hyperglycemia (ICD‐9‐CM code 790.6) were identified in a search of the hospital's electronic records. Data fields retrieved included patient age at admission, ethnicity/race, length of stay, total charges, and type of hospital service with primary responsibility for the patient's care. Because of the large number of available records, we randomly selected 5% of the total for chart review.20, 25, 26
Data Collection
Using an approach similar to that used by others,8 we reviewed admission notes, daily progress notes, and discharge summaries in order to establish whether the practitioner had recorded diabetes or hyperglycemia in the patient's chart. Subjective, objective, assessment, and plan components of notes were reviewed, and credit was given for having addressed diabetes or hyperglycemia if there was any documentation. For patients admitted for elective inpatient procedures, a preoperative outpatient evaluation conducted within 30 days of the hospitalization was counted as the admission note.
Practitioners typically make therapeutic decisions about hyperglycemia management of inpatients on the basis of daily bedside glucose measurements. In our institution, bedside glucose monitoring is performed with an instrument that scans and records patient identification, followed by direct downloading to our laboratory database. We determined whether bedside glucose levels were ordered and if so, whether they were then recorded in the daily progress notes. We determined the frequency of blood glucose measurements. Notes were examined to determine whether an assessment of hyperglycemia was made (defined as any comment in the progress note that addressed the severity of hyperglycemia or the adequacy of glucose control), and written orders were reviewed to establish any therapeutic changes. On completion of the chart reviews and entry of abstracted data into an electronic file, a link was made to the laboratory database to obtain information on bedside glucose values. We report data on notes written by the inpatient team with the principal caretaking responsibility for the patient (the primary service).
Data Analysis
Four primary outcome measures were of particular interest. First, we analyzed the percentage of patients who had diabetes or hyperglycemia documented in admission, daily progress, or discharge notes. Second, we determined the proportion of patients for whom bedside glucose measurements were ordered. Third, we calculated the percentage of patients with a written assessment of glycemic control. Finally, we examined the proportion of patients who had a change in therapy for treatment of hyperglycemia. Change in therapy was defined as any increase or decrease in the doses of an oral agent or insulin that occurred between admission day orders and the active orders on the day of discharge.
We determined the proportion of patients who had at least one hypoglycemic (glucose <70, <60, <50, <40 mg/dL) or hyperglycemic (>200, >250, >300, >350, >400 mg/dL) measurement documented by bedside monitoring. We also calculated the frequency of hypoglycemic and hyperglycemic values as the number of events per person per 100 measurements; as suggested by others,27 this approach to assessing glycemic control allows adjustment for different numbers of measurements across individuals and captures information on multiple episodes of hypo‐ or hyperglycemia in a single patient. All available bedside glucose values were averaged to determine the overall level of glucose control for the hospitalization and were divided into 3 intervals using cut points based on tertiles; the differences in the proportion of patients who had changes made in diabetes therapy was determined across tertiles using the 2 test. We determined the odds of changing therapy in the second and third tertiles of average bedside glucose relative to the first tertile. Differences in any continuous variables were evaluated using nonparametric methods (Mann‐Whitney test). Cases from all primary services were analyzed in aggregate.
RESULTS
General Patient Characteristics
Of all the patient hospitalization records for 2003, 1812 had a discharge diagnosis of diabetes or hyperglycemia. A random sample of 5% of these 1812 records yielded 90 records for chart review. The mean patient age was 68 years; 53% were male, and 90% were white.. Average length of stay was 4.8 days (Table 1). No significant differences in age, length of stay, sex, race, or source of admission (all P > .1) were detected between the 90 cases undergoing chart review and those cases that were not selected. On admission day, 63% of the patients were placed on insulin therapy, 17% on combination treatment of oral agents and insulin, and 7% on oral agents; the remaining 13% did not receive pharmacotherapy to treat their hyperglycemia. Thus, 80% were placed on insulin on the day they were admitted. By the day of discharge, 61% of the patients were on insulin therapy, either alone or in combination with oral agents. Of those on insulin therapy during their hospital stay, 35% were on a scheduled program of long‐ plus short‐acting insulin, and 65% were only on a sliding scale program.
| Characteristic | Value* |
|---|---|
| |
| Mean age (years) | 68 |
| Mean length of stay (days) | 4.8 |
| Men | 53 |
| White | 90 |
| Diabetes therapy at admission | |
| Insulin only | 63 |
| Oral agents only | 7 |
| Combination oral agents and insulin | 17 |
| Diet | 13 |
| Source of admission | |
| Physician office or clinic | 46 |
| Emergency room | 46 |
| Transfer | 8 |
| Primary service | |
| General medical | 41 |
| Surgical | 31 |
| Other | 28 |
| Teaching service | 48 |
Most patients were admitted through either an outpatient clinic (46%) or the emergency department (46%), with the remainder coming as transfers from other facilities (Table 1). Most inpatients were cared for by a general medical team (general internal or family medicine, 41%), whereas 31% were managed by one of the surgical specialties, and 28% were under the care of other specialties (eg, cardiology, transplantation, rehabilitation). Once hospitalized, most patients (94%) stayed on the original admitting service throughout their stay; 48% of patients were on a service staffed by a postgraduate trainee (Table 1). Two patients required a brief stay in the intensive care unit, but otherwise the sample was made up of noncritically ill patients.
Fifteen patients had their hemoglobin A1c measured in the hospital, with mean A1c of 7.0% 1.4%, whereas 57 patients had a documented preadmission hemoglobin A1c (average time before admission 29 weeks); their average A1c was 6.9% 1.2% (not shown).
Documentation of Diabetes
Of the 90 patients whose records were reviewed, 81 had preexisting diabetes, 3 had a diagnosis of metabolic syndrome or abnormal glucose tolerance, and 6 had hyperglycemia that developed during the admission hospitalization. When admission notes of persons with known diabetes or abnormal glucose tolerance were examined (Fig. 1), diabetes was documented in 96%. In the daily progress notes of the primary service, 62% of patients had diabetes documented at least once during their hospitalization, whereas the records of 38% had no mention of diabetes. When only those patients with known diabetes or evidence of inpatient hyperglycemia were considered, documentation of the diabetic condition was made in 60% of discharge summaries, and the need for follow‐up was noted in just 20% (Fig. 1).
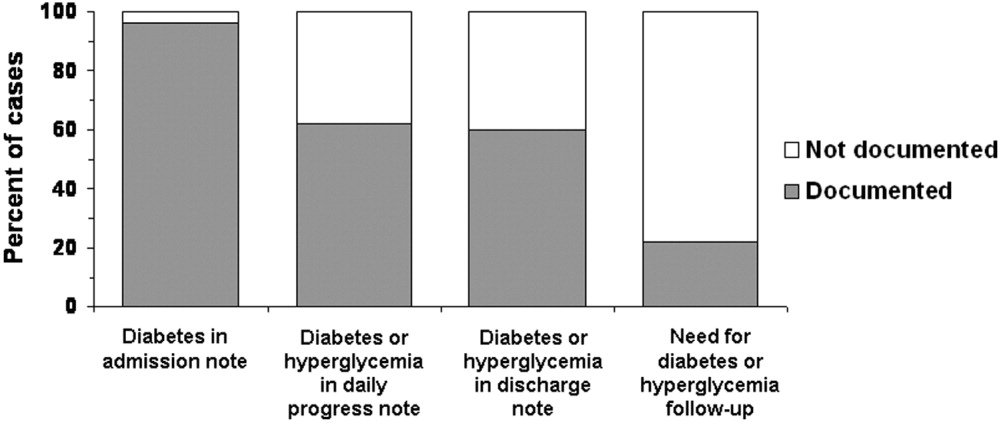
Fifty‐seven percent (n = 51) of the 90 patients whose records were sampled had had some type of consultant involved with their care, but only 13% had had an endocrinology consultation. For 27 patients (30% of all 90 cases), diabetes or hyperglycemia was documented in a consultant's note; thus, there was evidence that the issue of glucose management was being addressed by someone other than a member of the primary team and that someone was not necessarily an endocrinologist. When excluding those patients whose consultant addressed diabetes or hyperglycemia, only 53% had documentation of the problems recorded in the daily progress notes (data not shown).
Recording and Assessment of Glucose Values
Most of the 90 patients whose records were reviewed (86%; n = 79) had documentation in physician orders for bedside glucose monitoring during their hospital stay (Fig. 2), and 53% had bedside glucose levels recorded in at least one daily progress note, whereas documentation was absent in 47%. A written assessment of glucose control was found in the records of 52% of the hospitalized patients; 48% lacked any evaluation of the severity of their hyperglycemia (Fig. 2). Excluding data listed from consultants, bedside glucose data was recorded for 53% of patients, and an assessment of glycemic control was made for 41%.
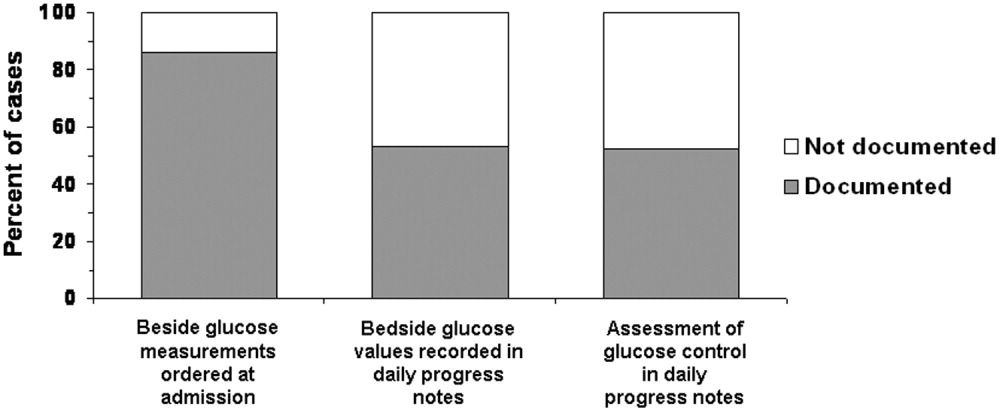
Glycemic Control
The average daily number of bedside glucose measurements was 4, while the daily frequency of blood glucose tests was only 1; an average of 10 bedside readings were obtained per patient. The mean bedside glucose value (averaged over the length of stay) was 170 mg/dL. At the time of admission, 33% of patients had a bedside glucose value >200 mg/dL (Fig 3, top panel), and 27% had a value >200 mg/dL before discharge (Fig 3, middle panel). Based on the bedside glucose averaged over the length of stay, 29% of patients had persistent hyperglycemia (Fig. 3, bottom panel).
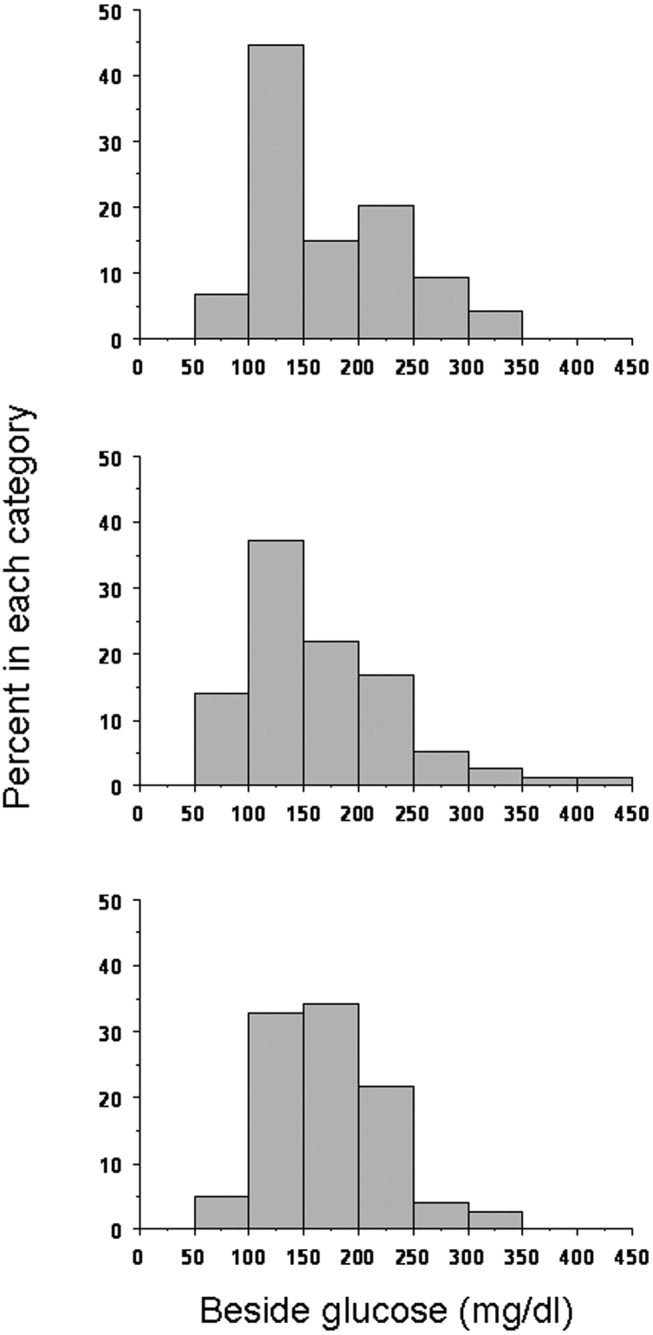
Hypoglycemia was rare. Only 11% of patients had at least one bedside measurement that was <70 mg/dL; 5% a measurement of <60 mg/dL, 4% a measurement of <50 mg/dL, and 1% a measurement of <40 mg/dL (Fig. 4). The frequency of values <70 mg/dL was 1.1 per person per 100 measurements; of values <60 mg/dL, 0.66; of values <50 mg/dL, 0.18; and of values <40 mg/dL, 0.08. In contrast, hyperglycemia was common: 71% of patients had at least one value >200 mg/dL; 43% at least one value >250 mg/dLl 24% at least one value >300 mg/dL; 20% at least one value >350 mg/dL; and 9% at least one value >400 mg/dL (Fig. 4). The frequency of hyperglycemic events was 28.2 per person per 100 measurements for values >200 mg/dL, 11.2 for values >250 mg/dL, 5.3 for values >300 mg/dL, 2.4 for values >350 mg/dL, and 1.1 for values >400 mg/dL.
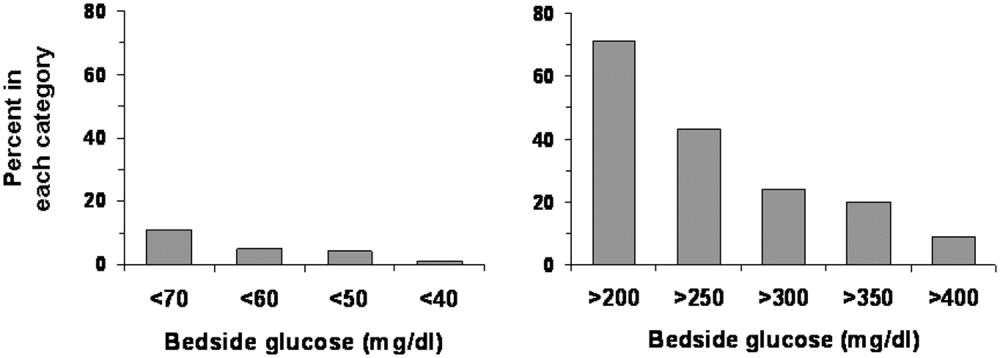
Changes in Therapy
Overall, changes were made in the hyperglycemia therapy of only 34% of patients. Treatment was changed for 50% of patients who had at least one glucose reading >200 mg/dL, and 89% of patients who had at least one glucose reading <70 mg/dL. Figure 5 shows whether changes in treatment occurred by tertiles of average bedside glucose. The percentage of patients with a change in therapy increased with worse hyperglycemia, although 32% in the third tertile still had not had a change in treatment. The odds of those in the second tertile having a change in therapy (compared with those in the first tertile) were 1.9 (95% confidence interval 0.556.25, P = .32), but were 5.6 (95% confidence interval 1.6818.7, P = .005) for patients in the third tertile. The frequency of glucose values <70 mg/dL was 1.8 per person per 100 measurements for patients in the first tertile, 1.1 for patients in the second tertile, but only 0.29 per person per 100 measurements for patients in the third tertile. The average number of glucose measurements >200 mg/dL per person was 2.9 per 100 measurements for patients in the first tertile, 22.7 for patients in the second tertile, and 60.0 for patients in the third tertile (not shown).
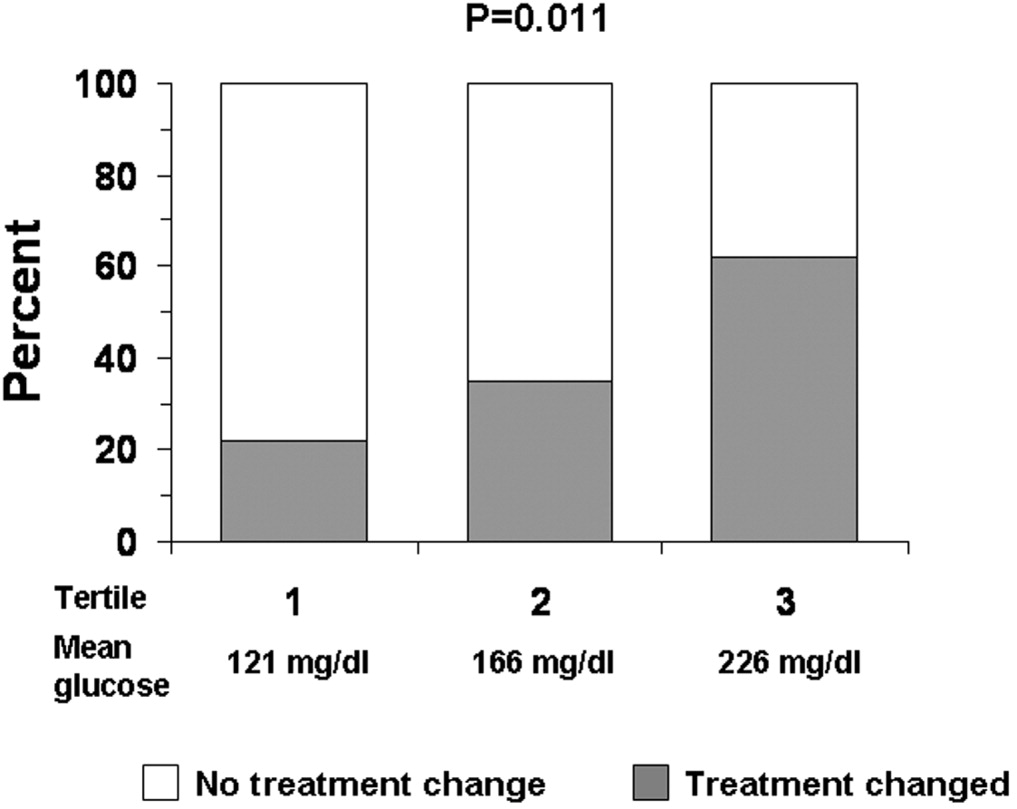
DISCUSSION
Just as clinical trials in the outpatient setting have demonstrated the benefits of good glycemic control,2830 recent studies have also suggested that treatment of hyperglycemia during hospitalization can improve outcomes.10, 11 Consequently, there has been increased attention to the management of glucose in the hospital, with recognition of the need for inpatient‐specific standards for diabetes care.10, 11, 31 Optimization of management and of education about diabetes and hyperglycemia in the hospital requires better understanding of current care practices in order to determine where to direct interventions.
Nearly all the 90 patients whose records we reviewed had preexisting diabetes or a known potential glucose abnormality that was documented either at the time of, or just prior to, hospital admission. The observation that most patients had orders for bedside glucose monitoring also indicated that practitioners were aware of the diagnosis when the patient was admitted. Although clinicians seemed to be aware of the potential problem of glucoseand the majority of clinicians did some trackinga substantial number of hospitalizations (nearly 40%) had no documentation of diabetes or hyperglycemia after admission. If diabetes was not the principal reason for hospitalization, it is possible that the primary team did not focus on managing hyperglycemia. Nonetheless, the hospital encounter does represent an opportunity to address glucose management and perhaps improve care and outcomes, even if the patient was admitted for an unrelated condition.32 Because the average length of stay was almost 5 days, there should have been sufficient time to address diabetes in most patients.
Although most patients had the condition of their diabetes documented in their discharge notes, a substantial proportion of the discharge notes did not mention an outpatient plan to follow up on the diabetes or hyperglycemia. A recent study suggested that direct referral for outpatient diabetes services increased the chances of patient follow‐up.33 Educating practitioners about the need to emphasize to patients the importance of diabetes postdischarge care is a program that could be developed and implemented in the hospital setting.
Although bedside glucose monitoring was appropriately ordered in most instances, the actual recording of values and the assessment of glucose control were documented in the records of only about half the patients during their hospitalizations. Moreover, even among patients who had high bedside glucose levels, changes in therapy often did not occur. Clinician concern about inducing hypoglycemia in hospitalized patients has been cited as a factor limiting the intensification of treatment for diabetes.34 The frequency in our facility of documented low blood glucose values was small, although there may have been unrecognized episodes. However, missed events were probably unusual, given the daily average of 4 bedside glucose measurements per patient, ongoing nursing staff contact with patients, and a formal policy to document and treat hypoglycemia. We found that hyperglycemia was far more common than hypoglycemia and that there were likely many opportunities to control blood glucose more rigorously.
Practitioners appeared to be responding to hypoglycemia, as a large proportion of the patients with a glucose reading of <70 mg/dL had a change in therapy. However, the response to hyperglycemia was delayedthe odds of therapy being changed were significant only for patients whose glucose levels were in the third tertile. Despite evidence of hyperglycemia and the low frequency of hypoglycemia of those whose glucose levels were in the second and third tertiles, a substantial proportion of patients did not have their therapy changed. Combined with the observation that glucose data and diabetes were often not documented, our data suggest that there may be a problem of clinical inertia in the inpatient setting. Clinical inertia has been defined as not initiating or intensifying therapy when doing so is indicated.35, 36 Other reports have also documented clinical inertia in the outpatient environment.23, 3741 Overcoming clinical inertia, at least in regard to diabetes management, can improve glycemic control in patients.35 To improve the management of hyperglycemia in the hospital, educational interventions must be developed to teach health care practitioners effective strategies for glucose reduction. We did not quantify the changes in therapy (eg, how much insulin was changed or in what direction), only whether a change had been made. The observation that the proportion of cases on insulin at discharge was less than on admission day suggests that there may actually have been deintensification of therapy taking placesome of the cases in which therapy was changed, therefore, likely included instances of negative therapeutic momentum despite evidence of hyperglycemia. The control of inpatient hyperglycemia will likely require frequent changes in therapy, as it does in the outpatient setting, and detailed information about treatment strategies actually employed will be necessary to design educational programs.
One limitation of our analysis was that the study was retrospective, which did not allow assessment of the reasons underlying the behavior of the clinicians, such as why they did not document diabetes or change therapy. We selected a 5% sample for our study as per common methods.20, 25, 26 Thus, although the 90 patients making up the sample were randomly selected and were not different demographically from the larger population of patients admitted with diabetes, the number of cases we reviewed was small compared with the actual number of discharged patients with diabetes. Cases were diagnosed by diagnosis codes; therefore, it is likely that some diabetes cases were missed, and other patients with hyperglycemia may not have had the diagnosis even documented.8, 24 Our study design and sample size precluded a comparison of outcomes between cases with in which a consultant was involved with those in which a consultant was not involved or a comparison of cases according to type of consultant involved.1216 Finally, our study focused on noncritically ill patients; thus, our findings cannot be generalized to care provided in the intensive care unit.
There are no definitive guidelines on what method (ie, blood or bedside glucose) should be used to evaluate glycemic control in the hospital. The methods we used here can serve as means to benchmark and track improvement in glycemic control. The observations that most patients had bedside glucose monitoring ordered and that the frequency of these measurements was high compared with the frequency of actual blood glucose assessments support the idea that practitioners favored this method to evaluate the level of glycemic control in the hospital. In practice, it is bedside glucose evaluation that clinicians use to make decisions about day‐to‐day treatment of hyperglycemia. In our facility, the method for bedside glucose monitoring is standardized and is part of a quality assurance program. Moreover, the high average frequency of bedside blood glucose determination increased the chance of detecting hyper‐ and hypoglycemic events.
Current guidelines provide suggestions about target pre‐ and postprandial glucose levels for noncritically ill patients.11 However, these targets are not universally recognized.42 For instance, the Institutes for Healthcare Improvement's Prevent Surgical Site Infections initiative defines a glucose level of <200 mg/dL as its target perioperative glucose control level.43 In practice, it can be difficult to assess glucose control in terms of pre‐ and postprandial categories. Although bedside glucose monitoring in our facility is typically ordered before meals and at bedtime, in many cases prolonged periods of patient fasting, disrupted meal schedules, mismatching insulin with meals, and use of continuous parental and enteral nutritional support all make it difficult to assess pre‐ and postprandial glycemic control retrospectively. Hence, we used as our measures the value of the bedside glucose averaged over the length of the hospital stay and the number of hyper‐ and hypoglycemic events.
In general, our study was hampered by a lack of hospital‐specific process measures to evaluate the quality of inpatient diabetes care. Process measures such as the frequency of hemoglobin A1c monitoring or performance of ophthalmologic examinations,1723 which are commonly used to assess quality of diabetes care in the outpatient arena, may not be optimal variables for evaluating care in the hospital. New methods to guide efforts to improve the quality of inpatient management of diabetes and hyperglycemia are needed.
Despite these limitations, our analysis was helpful in providing direction about how to enhance the care of hospitalized patients with hyperglycemia or known diabetes. Constructing institution‐specific management guidelines for the care of inpatient diabetes and hyperglycemia would provide a yardstick against which to measure the care provided by both the hospital and the individual clinician. Educational programs can be developed to increase awareness among practitioners of the importance of inpatient glucose control and of the need to improve ongoing documentation of the problem. Exploring practitioner barriers to treatment of inpatient hyperglycemia should be an essential component of this educational process. Finally, consensus strategies on when to initiate and change therapy should be designed so that hyperglycemia in the hospital can be managed more effectively. All these areas must be addressed to assure delivery of the highest‐quality inpatient care to patients with diabetes.
- ,,,,.Diabetes‐related hospitalization and hospital utilization. In:Diabetes in America: National Diabetes Data Group.2nd ed.Bethesda (MD):National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases;1995:553–563.
- .Hospitalization in the United States, 1997: HCUP fact book no. 1: diagnosis, charges, length of stay, insurance coverage, discharge status, inhospital deaths.Rockville (MD):Agency for Healthcare Research and Quality;2000.
- Centers for Disease Control and Prevention. Hospitalization for diabetes as first‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmfirst/table1.htm. Accessed: June 2,2005.
- Centers for Disease Control and Prevention. Hospitalizations for diabetes as any‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed: June 2,2005.
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26:1421–1426.
- ,,,.Excess costs of medical care for patients with diabetes in a managed care population.Diabetes Care.1997;20:1396–1402.
- ,,,American Diabetes Association.Economic costs of diabetes in the US in 2002.Diabetes Care.2003;26:917–932.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,,,,American Diabetes Association Diabetes in Hospitals Writing Committee, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591. Erratum in: Diabetes Care. 2004;27:856 and Diabetes Care. 2004;27:1255.
- ,,,,,,American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control, et al.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10:77–82.
- ,,,.Effect of physician specialty on outcomes in diabetic ketoacidosis.Diabetes Care.1999;22:1790–1795.
- ,,,.Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes.Am J Med.1995;99:22–28.
- ,,.Effects of an intervention by a diabetes team in hospitalized patients with diabetes.Diabetes Care.1997;20:1553–1555.
- ,.Nursing case management: an innovative model of care for hospitalized patients with diabetes.Diabetes Educ.1993;19:517–521.
- ,,,,.Evaluation of a hospital diabetes specialist nursing service: a randomized controlled trial.Diabet Med.2001;18:301–307.
- ,,,,,.Variation in office‐based quality. A claims‐based profile of care provided to Medicare patients with diabetes.JAMA.1995;273:1503–1508.
- ,,,,,, et al.Outpatient management of diabetes mellitus in five Arizona Medicare managed care plans.Am J Med Qual.1996;11:87–93.
- ,,,.Quality of outpatient care provided to diabetic patients: a health maintenance organization experience.Diabetes Care.1996;19:601–6.
- United States General Accounting Office: report to the Chairman, Subcommittee on Health and Environment, Committee on Commerce, House of Representatives.Medicare: most beneficiaries with diabetes do not receive recommended monitoring services. GAO/HEHS‐97–48.1997.
- ,,,,.Care of patients with type II diabetes: a study of family physicians' compliance with clinical practice guidelines.J Fam Pract.1997;44:374–381.
- ,,,,,.A diabetes report card for the United States: quality of care in the 1990s.Ann Intern Med.2002;136:565–574.
- ,,,University HealthSystem Consortium (UHC) Diabetes Benchmarking Project Team.Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change.Diabetes Care.2005;28:337–442.
- ,,,.An audit of the management and outcome of hospital inpatients with diabetes: resource planning implications for the diabetes care team.Diabet Med.1992;9:753–755.
- .Improving outcomes in public health practice: strategy and methods.Gaithersburg (MD):Aspen Publishers;1997:175–213.
- ,,,,,.Outpatient diabetes management of Medicare beneficiaries in four Mississippi fee‐for‐service primary care clinics.J Miss State Med Assoc.1999;40:8–13.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- The Diabetes Control and Complications Trial Research Group.The effect of intensive treatment of diabetes on the development and progression of long‐term complications in insulin‐dependent diabetes mellitus.N Engl J Med.1993;329:977–986.
- UK Prospective Diabetes Study (UKPDS) Group.Intensive blood‐glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33).Lancet.1998;352:837–53. Erratum in: Lancet. 1999;354:602.
- UK Prospective Diabetes Study (UKPDS) Group.Effect of intensive blood‐glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34).Lancet.1998;352:854–65. Erratum in: Lancet. 1998;352:1557.
- ,,.Current standards of care for inpatient glycemic management and metabolic control: is it time for definite standards and targets?Endocr Pract.2004;10(Suppl 2):10–12.
- ,.Windows of opportunity to improve diabetes care when patients with diabetes are hospitalized for other conditions.Diabetes Care.2001;24:1371–1376.
- ,,, et al.Inpatient to outpatient transfer of care in urban patients with diabetes: patterns and determinants of immediate postdischarge follow‐up.Arch Intern Med.2004;164:447–453.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10(Suppl 2):89–99.
- ,,, et al.Diabetes in urban African‐Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes.Diabetes Care.1999;22:1494–1500.
- ,,, et al.Clinical inertia.Ann Intern Med.2001;135:825–834.
- .Management of older hypertensive patients: is there a difference in approach?J Clin Hypertens (Greenwich).2003;5(Suppl 4):11–16.
- ,,, et al.Narrowing the gap in hypertension: effectiveness of a complex antihypertensive program in the elderly.Dis Manag.2004;7:235–243.
- ,,, et al.Clinical inertia in the management of Type 2 diabetes metabolic risk factors.Diabet Med.2004;21:150–155.
- ,.Clinical inertia: errors of omission in drug therapy.Am J Health Syst Pharm.2004;61:401–404.
- .Overcome clinical inertia to control systolic blood pressure.Arch Intern Med.2003;163:2677–2678.
- ,.Counterpoint: inpatient glucose management: a premature call to arms?Diabetes Care.2005;28:976–979.
- Institute for Healthcare Improvement. Getting started kit: prevent surgical site infections. Available from: www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed June 2,2005.
Persons with diabetes have a greater risk of being hospitalized than do nondiabetic persons,1 and hospitalization was a major contributor to health care utilization and costs of patients with diabetes. In 1997, diabetes was the fourth most common comorbid condition in hospitalized patients nationwide. In 2001 in the United States, 562,000 hospital discharges listed diabetes as a principal diagnosis, and more than 4 million discharges listed diabetes in any diagnostic field.24 Nearly one third of diabetes patients may require 2 or more hospitalizations a year,5 and inpatient stays are the largest expense incurred by persons with this disease.6, 7 A substantial number of hospitalized persons are found to have unrecognized diabetes or to develop hyperglycemia during an inpatient stay.8, 9
The severity of hyperglycemia in the hospital has been linked to numerous adverse outcomes in various clinical situations, and recent studies have demonstrated the potential benefits of achieving good glucose control in the inpatient setting.10, 11 Moreover, specific inpatient‐directed interventions can improve the delivery of diabetes care.1216
Unlike the quality of outpatient diabetes care, which has been extensively profiled,1723 little is actually known about inpatient management. However, earlier reports suggested that hyperglycemia is frequently overlooked by health care personnel.8, 24 To develop intervention and educational programs will require insight into how diabetes is being addressed in the hospital. Thus, we undertook a retrospective chart review of inpatients with a discharge diagnosis of diabetes or hyperglycemia in order to assess whether these conditions were being documented and whether glucose management was being addressed.
METHODS
Setting
Our regional referral, academic teaching hospital is a 200‐bed facility in metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented at this hospital, including renal, liver, and pancreas transplantation, a level‐2 trauma center, and an inpatient rehabilitation unit. Inpatient care is provided either by postgraduate trainees (residents) or through a separate faculty service; physician assistants and nurse‐practitioners also deliver care. Residents may be supervised by either hospitalist or nonhospitalist attendings. An electronic medical record links outpatient and inpatient records, radiology studies, and laboratory results.
Patient Selection
The study was approved by the Mayo Clinic Institutional Review Board. Patients discharged from our facility during 2003 with a diagnosis code from the International Classification of Diseases, 9th revision, Clinical Modification (ICD‐9‐CM) either for diabetes (ICD‐9‐CM code 250.0) or for hyperglycemia (ICD‐9‐CM code 790.6) were identified in a search of the hospital's electronic records. Data fields retrieved included patient age at admission, ethnicity/race, length of stay, total charges, and type of hospital service with primary responsibility for the patient's care. Because of the large number of available records, we randomly selected 5% of the total for chart review.20, 25, 26
Data Collection
Using an approach similar to that used by others,8 we reviewed admission notes, daily progress notes, and discharge summaries in order to establish whether the practitioner had recorded diabetes or hyperglycemia in the patient's chart. Subjective, objective, assessment, and plan components of notes were reviewed, and credit was given for having addressed diabetes or hyperglycemia if there was any documentation. For patients admitted for elective inpatient procedures, a preoperative outpatient evaluation conducted within 30 days of the hospitalization was counted as the admission note.
Practitioners typically make therapeutic decisions about hyperglycemia management of inpatients on the basis of daily bedside glucose measurements. In our institution, bedside glucose monitoring is performed with an instrument that scans and records patient identification, followed by direct downloading to our laboratory database. We determined whether bedside glucose levels were ordered and if so, whether they were then recorded in the daily progress notes. We determined the frequency of blood glucose measurements. Notes were examined to determine whether an assessment of hyperglycemia was made (defined as any comment in the progress note that addressed the severity of hyperglycemia or the adequacy of glucose control), and written orders were reviewed to establish any therapeutic changes. On completion of the chart reviews and entry of abstracted data into an electronic file, a link was made to the laboratory database to obtain information on bedside glucose values. We report data on notes written by the inpatient team with the principal caretaking responsibility for the patient (the primary service).
Data Analysis
Four primary outcome measures were of particular interest. First, we analyzed the percentage of patients who had diabetes or hyperglycemia documented in admission, daily progress, or discharge notes. Second, we determined the proportion of patients for whom bedside glucose measurements were ordered. Third, we calculated the percentage of patients with a written assessment of glycemic control. Finally, we examined the proportion of patients who had a change in therapy for treatment of hyperglycemia. Change in therapy was defined as any increase or decrease in the doses of an oral agent or insulin that occurred between admission day orders and the active orders on the day of discharge.
We determined the proportion of patients who had at least one hypoglycemic (glucose <70, <60, <50, <40 mg/dL) or hyperglycemic (>200, >250, >300, >350, >400 mg/dL) measurement documented by bedside monitoring. We also calculated the frequency of hypoglycemic and hyperglycemic values as the number of events per person per 100 measurements; as suggested by others,27 this approach to assessing glycemic control allows adjustment for different numbers of measurements across individuals and captures information on multiple episodes of hypo‐ or hyperglycemia in a single patient. All available bedside glucose values were averaged to determine the overall level of glucose control for the hospitalization and were divided into 3 intervals using cut points based on tertiles; the differences in the proportion of patients who had changes made in diabetes therapy was determined across tertiles using the 2 test. We determined the odds of changing therapy in the second and third tertiles of average bedside glucose relative to the first tertile. Differences in any continuous variables were evaluated using nonparametric methods (Mann‐Whitney test). Cases from all primary services were analyzed in aggregate.
RESULTS
General Patient Characteristics
Of all the patient hospitalization records for 2003, 1812 had a discharge diagnosis of diabetes or hyperglycemia. A random sample of 5% of these 1812 records yielded 90 records for chart review. The mean patient age was 68 years; 53% were male, and 90% were white.. Average length of stay was 4.8 days (Table 1). No significant differences in age, length of stay, sex, race, or source of admission (all P > .1) were detected between the 90 cases undergoing chart review and those cases that were not selected. On admission day, 63% of the patients were placed on insulin therapy, 17% on combination treatment of oral agents and insulin, and 7% on oral agents; the remaining 13% did not receive pharmacotherapy to treat their hyperglycemia. Thus, 80% were placed on insulin on the day they were admitted. By the day of discharge, 61% of the patients were on insulin therapy, either alone or in combination with oral agents. Of those on insulin therapy during their hospital stay, 35% were on a scheduled program of long‐ plus short‐acting insulin, and 65% were only on a sliding scale program.
| Characteristic | Value* |
|---|---|
| |
| Mean age (years) | 68 |
| Mean length of stay (days) | 4.8 |
| Men | 53 |
| White | 90 |
| Diabetes therapy at admission | |
| Insulin only | 63 |
| Oral agents only | 7 |
| Combination oral agents and insulin | 17 |
| Diet | 13 |
| Source of admission | |
| Physician office or clinic | 46 |
| Emergency room | 46 |
| Transfer | 8 |
| Primary service | |
| General medical | 41 |
| Surgical | 31 |
| Other | 28 |
| Teaching service | 48 |
Most patients were admitted through either an outpatient clinic (46%) or the emergency department (46%), with the remainder coming as transfers from other facilities (Table 1). Most inpatients were cared for by a general medical team (general internal or family medicine, 41%), whereas 31% were managed by one of the surgical specialties, and 28% were under the care of other specialties (eg, cardiology, transplantation, rehabilitation). Once hospitalized, most patients (94%) stayed on the original admitting service throughout their stay; 48% of patients were on a service staffed by a postgraduate trainee (Table 1). Two patients required a brief stay in the intensive care unit, but otherwise the sample was made up of noncritically ill patients.
Fifteen patients had their hemoglobin A1c measured in the hospital, with mean A1c of 7.0% 1.4%, whereas 57 patients had a documented preadmission hemoglobin A1c (average time before admission 29 weeks); their average A1c was 6.9% 1.2% (not shown).
Documentation of Diabetes
Of the 90 patients whose records were reviewed, 81 had preexisting diabetes, 3 had a diagnosis of metabolic syndrome or abnormal glucose tolerance, and 6 had hyperglycemia that developed during the admission hospitalization. When admission notes of persons with known diabetes or abnormal glucose tolerance were examined (Fig. 1), diabetes was documented in 96%. In the daily progress notes of the primary service, 62% of patients had diabetes documented at least once during their hospitalization, whereas the records of 38% had no mention of diabetes. When only those patients with known diabetes or evidence of inpatient hyperglycemia were considered, documentation of the diabetic condition was made in 60% of discharge summaries, and the need for follow‐up was noted in just 20% (Fig. 1).
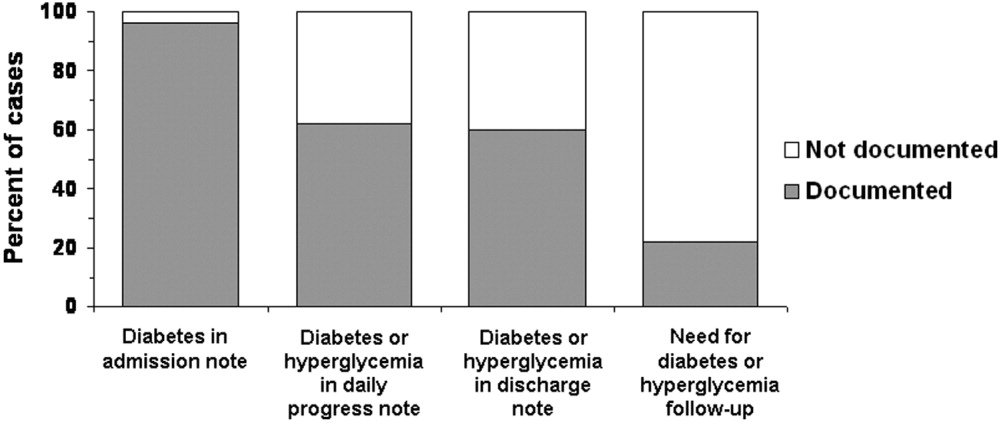
Fifty‐seven percent (n = 51) of the 90 patients whose records were sampled had had some type of consultant involved with their care, but only 13% had had an endocrinology consultation. For 27 patients (30% of all 90 cases), diabetes or hyperglycemia was documented in a consultant's note; thus, there was evidence that the issue of glucose management was being addressed by someone other than a member of the primary team and that someone was not necessarily an endocrinologist. When excluding those patients whose consultant addressed diabetes or hyperglycemia, only 53% had documentation of the problems recorded in the daily progress notes (data not shown).
Recording and Assessment of Glucose Values
Most of the 90 patients whose records were reviewed (86%; n = 79) had documentation in physician orders for bedside glucose monitoring during their hospital stay (Fig. 2), and 53% had bedside glucose levels recorded in at least one daily progress note, whereas documentation was absent in 47%. A written assessment of glucose control was found in the records of 52% of the hospitalized patients; 48% lacked any evaluation of the severity of their hyperglycemia (Fig. 2). Excluding data listed from consultants, bedside glucose data was recorded for 53% of patients, and an assessment of glycemic control was made for 41%.
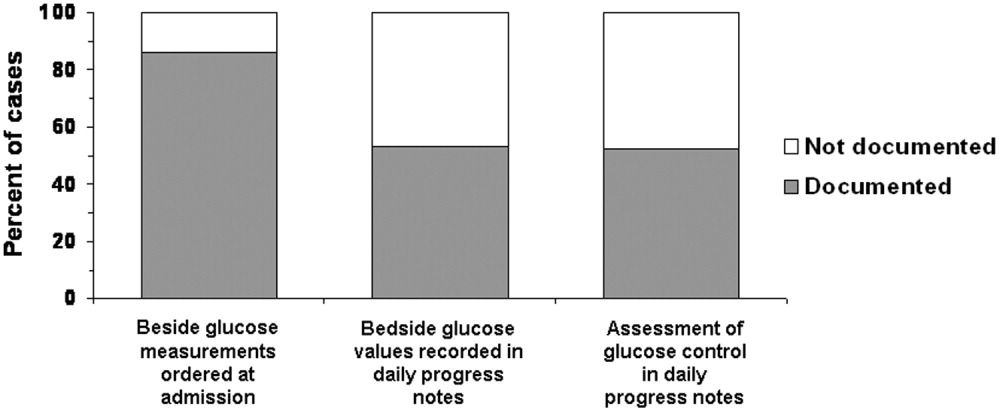
Glycemic Control
The average daily number of bedside glucose measurements was 4, while the daily frequency of blood glucose tests was only 1; an average of 10 bedside readings were obtained per patient. The mean bedside glucose value (averaged over the length of stay) was 170 mg/dL. At the time of admission, 33% of patients had a bedside glucose value >200 mg/dL (Fig 3, top panel), and 27% had a value >200 mg/dL before discharge (Fig 3, middle panel). Based on the bedside glucose averaged over the length of stay, 29% of patients had persistent hyperglycemia (Fig. 3, bottom panel).
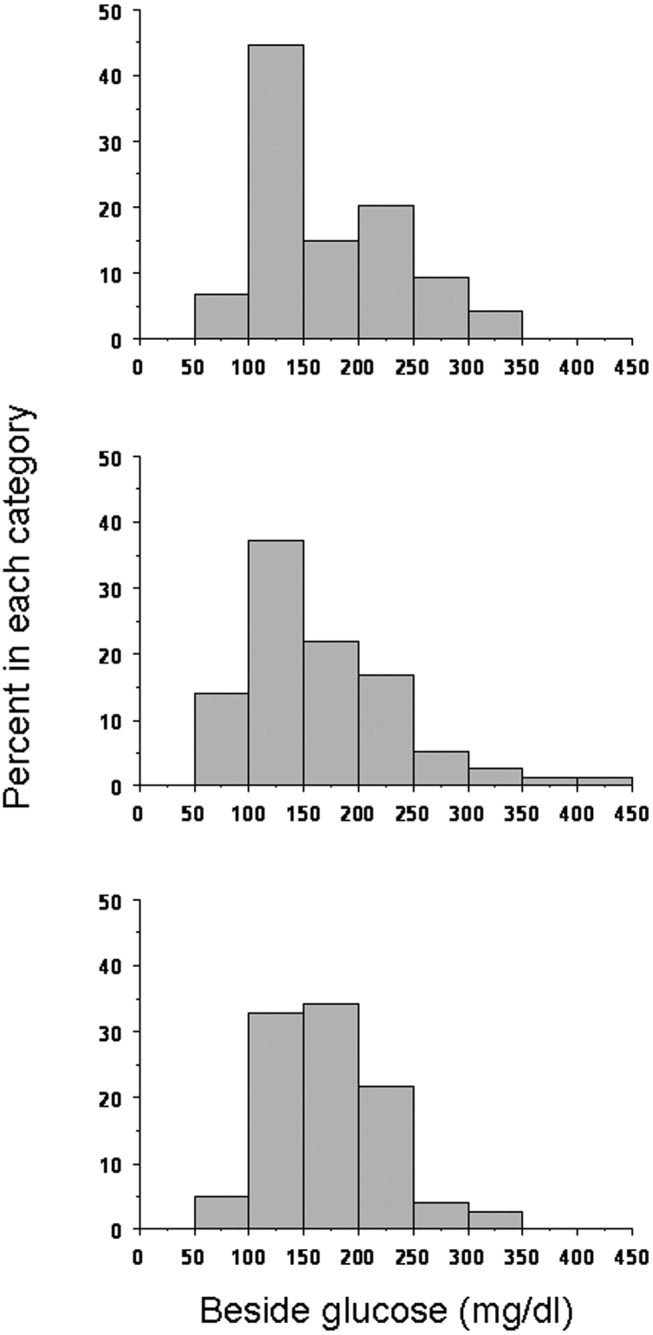
Hypoglycemia was rare. Only 11% of patients had at least one bedside measurement that was <70 mg/dL; 5% a measurement of <60 mg/dL, 4% a measurement of <50 mg/dL, and 1% a measurement of <40 mg/dL (Fig. 4). The frequency of values <70 mg/dL was 1.1 per person per 100 measurements; of values <60 mg/dL, 0.66; of values <50 mg/dL, 0.18; and of values <40 mg/dL, 0.08. In contrast, hyperglycemia was common: 71% of patients had at least one value >200 mg/dL; 43% at least one value >250 mg/dLl 24% at least one value >300 mg/dL; 20% at least one value >350 mg/dL; and 9% at least one value >400 mg/dL (Fig. 4). The frequency of hyperglycemic events was 28.2 per person per 100 measurements for values >200 mg/dL, 11.2 for values >250 mg/dL, 5.3 for values >300 mg/dL, 2.4 for values >350 mg/dL, and 1.1 for values >400 mg/dL.
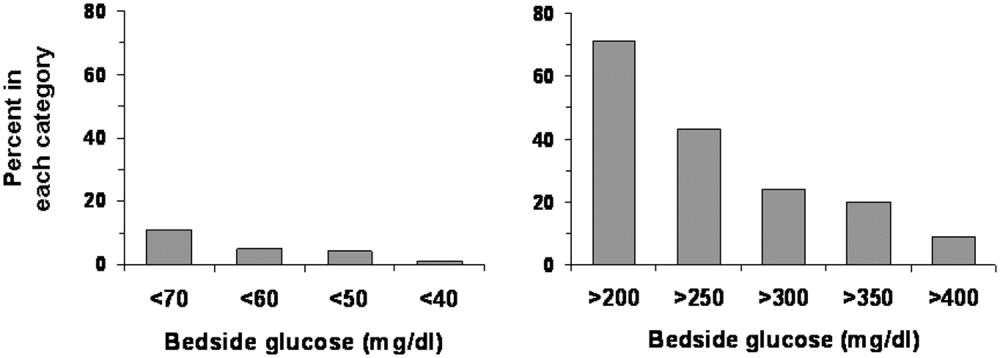
Changes in Therapy
Overall, changes were made in the hyperglycemia therapy of only 34% of patients. Treatment was changed for 50% of patients who had at least one glucose reading >200 mg/dL, and 89% of patients who had at least one glucose reading <70 mg/dL. Figure 5 shows whether changes in treatment occurred by tertiles of average bedside glucose. The percentage of patients with a change in therapy increased with worse hyperglycemia, although 32% in the third tertile still had not had a change in treatment. The odds of those in the second tertile having a change in therapy (compared with those in the first tertile) were 1.9 (95% confidence interval 0.556.25, P = .32), but were 5.6 (95% confidence interval 1.6818.7, P = .005) for patients in the third tertile. The frequency of glucose values <70 mg/dL was 1.8 per person per 100 measurements for patients in the first tertile, 1.1 for patients in the second tertile, but only 0.29 per person per 100 measurements for patients in the third tertile. The average number of glucose measurements >200 mg/dL per person was 2.9 per 100 measurements for patients in the first tertile, 22.7 for patients in the second tertile, and 60.0 for patients in the third tertile (not shown).
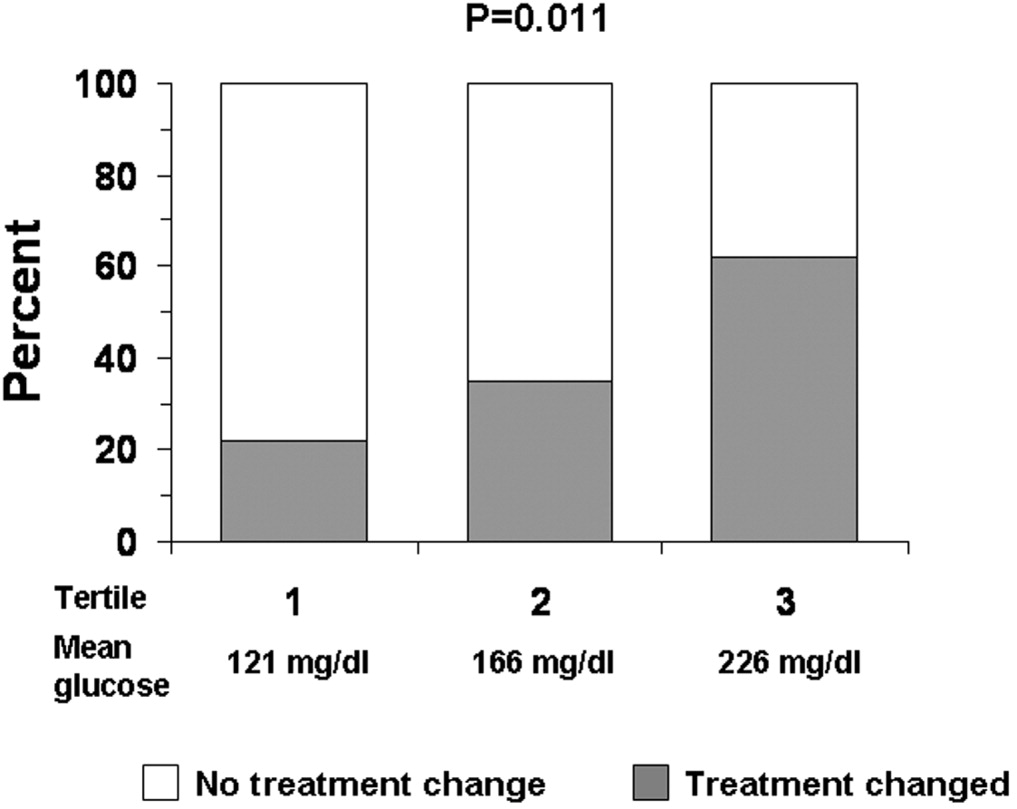
DISCUSSION
Just as clinical trials in the outpatient setting have demonstrated the benefits of good glycemic control,2830 recent studies have also suggested that treatment of hyperglycemia during hospitalization can improve outcomes.10, 11 Consequently, there has been increased attention to the management of glucose in the hospital, with recognition of the need for inpatient‐specific standards for diabetes care.10, 11, 31 Optimization of management and of education about diabetes and hyperglycemia in the hospital requires better understanding of current care practices in order to determine where to direct interventions.
Nearly all the 90 patients whose records we reviewed had preexisting diabetes or a known potential glucose abnormality that was documented either at the time of, or just prior to, hospital admission. The observation that most patients had orders for bedside glucose monitoring also indicated that practitioners were aware of the diagnosis when the patient was admitted. Although clinicians seemed to be aware of the potential problem of glucoseand the majority of clinicians did some trackinga substantial number of hospitalizations (nearly 40%) had no documentation of diabetes or hyperglycemia after admission. If diabetes was not the principal reason for hospitalization, it is possible that the primary team did not focus on managing hyperglycemia. Nonetheless, the hospital encounter does represent an opportunity to address glucose management and perhaps improve care and outcomes, even if the patient was admitted for an unrelated condition.32 Because the average length of stay was almost 5 days, there should have been sufficient time to address diabetes in most patients.
Although most patients had the condition of their diabetes documented in their discharge notes, a substantial proportion of the discharge notes did not mention an outpatient plan to follow up on the diabetes or hyperglycemia. A recent study suggested that direct referral for outpatient diabetes services increased the chances of patient follow‐up.33 Educating practitioners about the need to emphasize to patients the importance of diabetes postdischarge care is a program that could be developed and implemented in the hospital setting.
Although bedside glucose monitoring was appropriately ordered in most instances, the actual recording of values and the assessment of glucose control were documented in the records of only about half the patients during their hospitalizations. Moreover, even among patients who had high bedside glucose levels, changes in therapy often did not occur. Clinician concern about inducing hypoglycemia in hospitalized patients has been cited as a factor limiting the intensification of treatment for diabetes.34 The frequency in our facility of documented low blood glucose values was small, although there may have been unrecognized episodes. However, missed events were probably unusual, given the daily average of 4 bedside glucose measurements per patient, ongoing nursing staff contact with patients, and a formal policy to document and treat hypoglycemia. We found that hyperglycemia was far more common than hypoglycemia and that there were likely many opportunities to control blood glucose more rigorously.
Practitioners appeared to be responding to hypoglycemia, as a large proportion of the patients with a glucose reading of <70 mg/dL had a change in therapy. However, the response to hyperglycemia was delayedthe odds of therapy being changed were significant only for patients whose glucose levels were in the third tertile. Despite evidence of hyperglycemia and the low frequency of hypoglycemia of those whose glucose levels were in the second and third tertiles, a substantial proportion of patients did not have their therapy changed. Combined with the observation that glucose data and diabetes were often not documented, our data suggest that there may be a problem of clinical inertia in the inpatient setting. Clinical inertia has been defined as not initiating or intensifying therapy when doing so is indicated.35, 36 Other reports have also documented clinical inertia in the outpatient environment.23, 3741 Overcoming clinical inertia, at least in regard to diabetes management, can improve glycemic control in patients.35 To improve the management of hyperglycemia in the hospital, educational interventions must be developed to teach health care practitioners effective strategies for glucose reduction. We did not quantify the changes in therapy (eg, how much insulin was changed or in what direction), only whether a change had been made. The observation that the proportion of cases on insulin at discharge was less than on admission day suggests that there may actually have been deintensification of therapy taking placesome of the cases in which therapy was changed, therefore, likely included instances of negative therapeutic momentum despite evidence of hyperglycemia. The control of inpatient hyperglycemia will likely require frequent changes in therapy, as it does in the outpatient setting, and detailed information about treatment strategies actually employed will be necessary to design educational programs.
One limitation of our analysis was that the study was retrospective, which did not allow assessment of the reasons underlying the behavior of the clinicians, such as why they did not document diabetes or change therapy. We selected a 5% sample for our study as per common methods.20, 25, 26 Thus, although the 90 patients making up the sample were randomly selected and were not different demographically from the larger population of patients admitted with diabetes, the number of cases we reviewed was small compared with the actual number of discharged patients with diabetes. Cases were diagnosed by diagnosis codes; therefore, it is likely that some diabetes cases were missed, and other patients with hyperglycemia may not have had the diagnosis even documented.8, 24 Our study design and sample size precluded a comparison of outcomes between cases with in which a consultant was involved with those in which a consultant was not involved or a comparison of cases according to type of consultant involved.1216 Finally, our study focused on noncritically ill patients; thus, our findings cannot be generalized to care provided in the intensive care unit.
There are no definitive guidelines on what method (ie, blood or bedside glucose) should be used to evaluate glycemic control in the hospital. The methods we used here can serve as means to benchmark and track improvement in glycemic control. The observations that most patients had bedside glucose monitoring ordered and that the frequency of these measurements was high compared with the frequency of actual blood glucose assessments support the idea that practitioners favored this method to evaluate the level of glycemic control in the hospital. In practice, it is bedside glucose evaluation that clinicians use to make decisions about day‐to‐day treatment of hyperglycemia. In our facility, the method for bedside glucose monitoring is standardized and is part of a quality assurance program. Moreover, the high average frequency of bedside blood glucose determination increased the chance of detecting hyper‐ and hypoglycemic events.
Current guidelines provide suggestions about target pre‐ and postprandial glucose levels for noncritically ill patients.11 However, these targets are not universally recognized.42 For instance, the Institutes for Healthcare Improvement's Prevent Surgical Site Infections initiative defines a glucose level of <200 mg/dL as its target perioperative glucose control level.43 In practice, it can be difficult to assess glucose control in terms of pre‐ and postprandial categories. Although bedside glucose monitoring in our facility is typically ordered before meals and at bedtime, in many cases prolonged periods of patient fasting, disrupted meal schedules, mismatching insulin with meals, and use of continuous parental and enteral nutritional support all make it difficult to assess pre‐ and postprandial glycemic control retrospectively. Hence, we used as our measures the value of the bedside glucose averaged over the length of the hospital stay and the number of hyper‐ and hypoglycemic events.
In general, our study was hampered by a lack of hospital‐specific process measures to evaluate the quality of inpatient diabetes care. Process measures such as the frequency of hemoglobin A1c monitoring or performance of ophthalmologic examinations,1723 which are commonly used to assess quality of diabetes care in the outpatient arena, may not be optimal variables for evaluating care in the hospital. New methods to guide efforts to improve the quality of inpatient management of diabetes and hyperglycemia are needed.
Despite these limitations, our analysis was helpful in providing direction about how to enhance the care of hospitalized patients with hyperglycemia or known diabetes. Constructing institution‐specific management guidelines for the care of inpatient diabetes and hyperglycemia would provide a yardstick against which to measure the care provided by both the hospital and the individual clinician. Educational programs can be developed to increase awareness among practitioners of the importance of inpatient glucose control and of the need to improve ongoing documentation of the problem. Exploring practitioner barriers to treatment of inpatient hyperglycemia should be an essential component of this educational process. Finally, consensus strategies on when to initiate and change therapy should be designed so that hyperglycemia in the hospital can be managed more effectively. All these areas must be addressed to assure delivery of the highest‐quality inpatient care to patients with diabetes.
Persons with diabetes have a greater risk of being hospitalized than do nondiabetic persons,1 and hospitalization was a major contributor to health care utilization and costs of patients with diabetes. In 1997, diabetes was the fourth most common comorbid condition in hospitalized patients nationwide. In 2001 in the United States, 562,000 hospital discharges listed diabetes as a principal diagnosis, and more than 4 million discharges listed diabetes in any diagnostic field.24 Nearly one third of diabetes patients may require 2 or more hospitalizations a year,5 and inpatient stays are the largest expense incurred by persons with this disease.6, 7 A substantial number of hospitalized persons are found to have unrecognized diabetes or to develop hyperglycemia during an inpatient stay.8, 9
The severity of hyperglycemia in the hospital has been linked to numerous adverse outcomes in various clinical situations, and recent studies have demonstrated the potential benefits of achieving good glucose control in the inpatient setting.10, 11 Moreover, specific inpatient‐directed interventions can improve the delivery of diabetes care.1216
Unlike the quality of outpatient diabetes care, which has been extensively profiled,1723 little is actually known about inpatient management. However, earlier reports suggested that hyperglycemia is frequently overlooked by health care personnel.8, 24 To develop intervention and educational programs will require insight into how diabetes is being addressed in the hospital. Thus, we undertook a retrospective chart review of inpatients with a discharge diagnosis of diabetes or hyperglycemia in order to assess whether these conditions were being documented and whether glucose management was being addressed.
METHODS
Setting
Our regional referral, academic teaching hospital is a 200‐bed facility in metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented at this hospital, including renal, liver, and pancreas transplantation, a level‐2 trauma center, and an inpatient rehabilitation unit. Inpatient care is provided either by postgraduate trainees (residents) or through a separate faculty service; physician assistants and nurse‐practitioners also deliver care. Residents may be supervised by either hospitalist or nonhospitalist attendings. An electronic medical record links outpatient and inpatient records, radiology studies, and laboratory results.
Patient Selection
The study was approved by the Mayo Clinic Institutional Review Board. Patients discharged from our facility during 2003 with a diagnosis code from the International Classification of Diseases, 9th revision, Clinical Modification (ICD‐9‐CM) either for diabetes (ICD‐9‐CM code 250.0) or for hyperglycemia (ICD‐9‐CM code 790.6) were identified in a search of the hospital's electronic records. Data fields retrieved included patient age at admission, ethnicity/race, length of stay, total charges, and type of hospital service with primary responsibility for the patient's care. Because of the large number of available records, we randomly selected 5% of the total for chart review.20, 25, 26
Data Collection
Using an approach similar to that used by others,8 we reviewed admission notes, daily progress notes, and discharge summaries in order to establish whether the practitioner had recorded diabetes or hyperglycemia in the patient's chart. Subjective, objective, assessment, and plan components of notes were reviewed, and credit was given for having addressed diabetes or hyperglycemia if there was any documentation. For patients admitted for elective inpatient procedures, a preoperative outpatient evaluation conducted within 30 days of the hospitalization was counted as the admission note.
Practitioners typically make therapeutic decisions about hyperglycemia management of inpatients on the basis of daily bedside glucose measurements. In our institution, bedside glucose monitoring is performed with an instrument that scans and records patient identification, followed by direct downloading to our laboratory database. We determined whether bedside glucose levels were ordered and if so, whether they were then recorded in the daily progress notes. We determined the frequency of blood glucose measurements. Notes were examined to determine whether an assessment of hyperglycemia was made (defined as any comment in the progress note that addressed the severity of hyperglycemia or the adequacy of glucose control), and written orders were reviewed to establish any therapeutic changes. On completion of the chart reviews and entry of abstracted data into an electronic file, a link was made to the laboratory database to obtain information on bedside glucose values. We report data on notes written by the inpatient team with the principal caretaking responsibility for the patient (the primary service).
Data Analysis
Four primary outcome measures were of particular interest. First, we analyzed the percentage of patients who had diabetes or hyperglycemia documented in admission, daily progress, or discharge notes. Second, we determined the proportion of patients for whom bedside glucose measurements were ordered. Third, we calculated the percentage of patients with a written assessment of glycemic control. Finally, we examined the proportion of patients who had a change in therapy for treatment of hyperglycemia. Change in therapy was defined as any increase or decrease in the doses of an oral agent or insulin that occurred between admission day orders and the active orders on the day of discharge.
We determined the proportion of patients who had at least one hypoglycemic (glucose <70, <60, <50, <40 mg/dL) or hyperglycemic (>200, >250, >300, >350, >400 mg/dL) measurement documented by bedside monitoring. We also calculated the frequency of hypoglycemic and hyperglycemic values as the number of events per person per 100 measurements; as suggested by others,27 this approach to assessing glycemic control allows adjustment for different numbers of measurements across individuals and captures information on multiple episodes of hypo‐ or hyperglycemia in a single patient. All available bedside glucose values were averaged to determine the overall level of glucose control for the hospitalization and were divided into 3 intervals using cut points based on tertiles; the differences in the proportion of patients who had changes made in diabetes therapy was determined across tertiles using the 2 test. We determined the odds of changing therapy in the second and third tertiles of average bedside glucose relative to the first tertile. Differences in any continuous variables were evaluated using nonparametric methods (Mann‐Whitney test). Cases from all primary services were analyzed in aggregate.
RESULTS
General Patient Characteristics
Of all the patient hospitalization records for 2003, 1812 had a discharge diagnosis of diabetes or hyperglycemia. A random sample of 5% of these 1812 records yielded 90 records for chart review. The mean patient age was 68 years; 53% were male, and 90% were white.. Average length of stay was 4.8 days (Table 1). No significant differences in age, length of stay, sex, race, or source of admission (all P > .1) were detected between the 90 cases undergoing chart review and those cases that were not selected. On admission day, 63% of the patients were placed on insulin therapy, 17% on combination treatment of oral agents and insulin, and 7% on oral agents; the remaining 13% did not receive pharmacotherapy to treat their hyperglycemia. Thus, 80% were placed on insulin on the day they were admitted. By the day of discharge, 61% of the patients were on insulin therapy, either alone or in combination with oral agents. Of those on insulin therapy during their hospital stay, 35% were on a scheduled program of long‐ plus short‐acting insulin, and 65% were only on a sliding scale program.
| Characteristic | Value* |
|---|---|
| |
| Mean age (years) | 68 |
| Mean length of stay (days) | 4.8 |
| Men | 53 |
| White | 90 |
| Diabetes therapy at admission | |
| Insulin only | 63 |
| Oral agents only | 7 |
| Combination oral agents and insulin | 17 |
| Diet | 13 |
| Source of admission | |
| Physician office or clinic | 46 |
| Emergency room | 46 |
| Transfer | 8 |
| Primary service | |
| General medical | 41 |
| Surgical | 31 |
| Other | 28 |
| Teaching service | 48 |
Most patients were admitted through either an outpatient clinic (46%) or the emergency department (46%), with the remainder coming as transfers from other facilities (Table 1). Most inpatients were cared for by a general medical team (general internal or family medicine, 41%), whereas 31% were managed by one of the surgical specialties, and 28% were under the care of other specialties (eg, cardiology, transplantation, rehabilitation). Once hospitalized, most patients (94%) stayed on the original admitting service throughout their stay; 48% of patients were on a service staffed by a postgraduate trainee (Table 1). Two patients required a brief stay in the intensive care unit, but otherwise the sample was made up of noncritically ill patients.
Fifteen patients had their hemoglobin A1c measured in the hospital, with mean A1c of 7.0% 1.4%, whereas 57 patients had a documented preadmission hemoglobin A1c (average time before admission 29 weeks); their average A1c was 6.9% 1.2% (not shown).
Documentation of Diabetes
Of the 90 patients whose records were reviewed, 81 had preexisting diabetes, 3 had a diagnosis of metabolic syndrome or abnormal glucose tolerance, and 6 had hyperglycemia that developed during the admission hospitalization. When admission notes of persons with known diabetes or abnormal glucose tolerance were examined (Fig. 1), diabetes was documented in 96%. In the daily progress notes of the primary service, 62% of patients had diabetes documented at least once during their hospitalization, whereas the records of 38% had no mention of diabetes. When only those patients with known diabetes or evidence of inpatient hyperglycemia were considered, documentation of the diabetic condition was made in 60% of discharge summaries, and the need for follow‐up was noted in just 20% (Fig. 1).
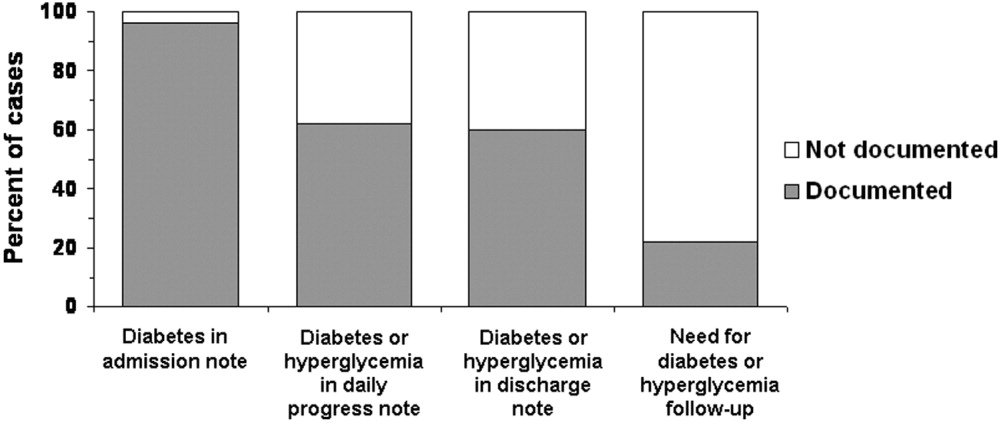
Fifty‐seven percent (n = 51) of the 90 patients whose records were sampled had had some type of consultant involved with their care, but only 13% had had an endocrinology consultation. For 27 patients (30% of all 90 cases), diabetes or hyperglycemia was documented in a consultant's note; thus, there was evidence that the issue of glucose management was being addressed by someone other than a member of the primary team and that someone was not necessarily an endocrinologist. When excluding those patients whose consultant addressed diabetes or hyperglycemia, only 53% had documentation of the problems recorded in the daily progress notes (data not shown).
Recording and Assessment of Glucose Values
Most of the 90 patients whose records were reviewed (86%; n = 79) had documentation in physician orders for bedside glucose monitoring during their hospital stay (Fig. 2), and 53% had bedside glucose levels recorded in at least one daily progress note, whereas documentation was absent in 47%. A written assessment of glucose control was found in the records of 52% of the hospitalized patients; 48% lacked any evaluation of the severity of their hyperglycemia (Fig. 2). Excluding data listed from consultants, bedside glucose data was recorded for 53% of patients, and an assessment of glycemic control was made for 41%.
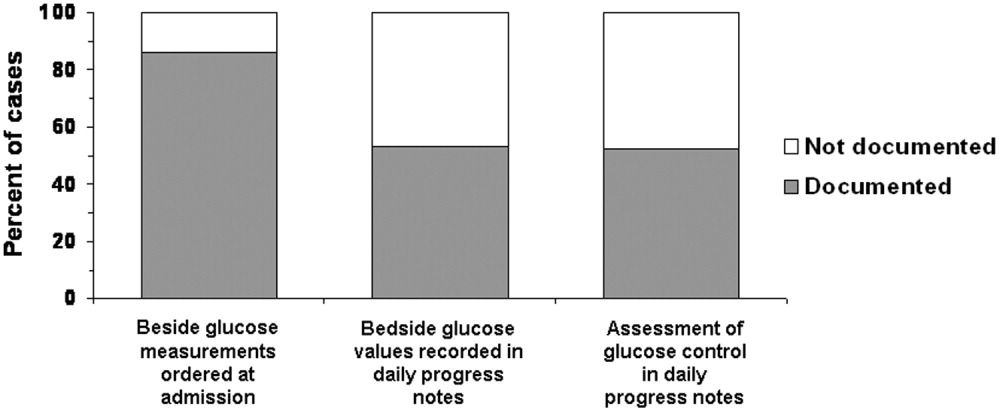
Glycemic Control
The average daily number of bedside glucose measurements was 4, while the daily frequency of blood glucose tests was only 1; an average of 10 bedside readings were obtained per patient. The mean bedside glucose value (averaged over the length of stay) was 170 mg/dL. At the time of admission, 33% of patients had a bedside glucose value >200 mg/dL (Fig 3, top panel), and 27% had a value >200 mg/dL before discharge (Fig 3, middle panel). Based on the bedside glucose averaged over the length of stay, 29% of patients had persistent hyperglycemia (Fig. 3, bottom panel).
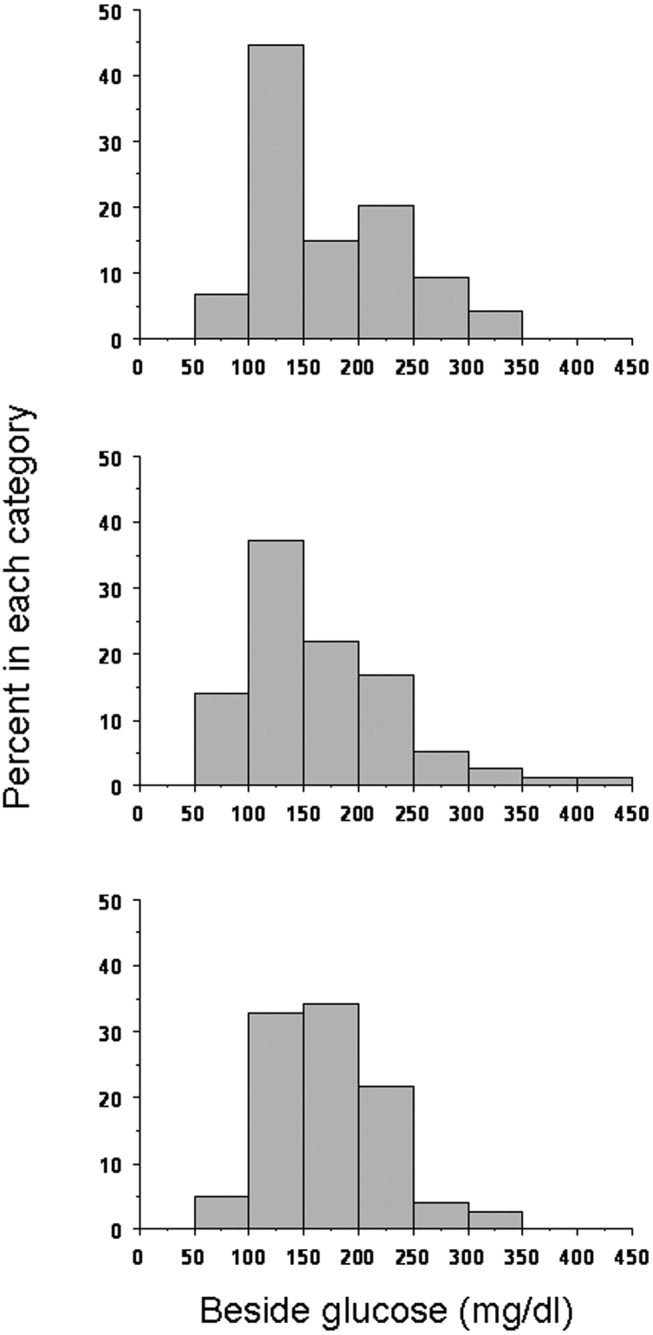
Hypoglycemia was rare. Only 11% of patients had at least one bedside measurement that was <70 mg/dL; 5% a measurement of <60 mg/dL, 4% a measurement of <50 mg/dL, and 1% a measurement of <40 mg/dL (Fig. 4). The frequency of values <70 mg/dL was 1.1 per person per 100 measurements; of values <60 mg/dL, 0.66; of values <50 mg/dL, 0.18; and of values <40 mg/dL, 0.08. In contrast, hyperglycemia was common: 71% of patients had at least one value >200 mg/dL; 43% at least one value >250 mg/dLl 24% at least one value >300 mg/dL; 20% at least one value >350 mg/dL; and 9% at least one value >400 mg/dL (Fig. 4). The frequency of hyperglycemic events was 28.2 per person per 100 measurements for values >200 mg/dL, 11.2 for values >250 mg/dL, 5.3 for values >300 mg/dL, 2.4 for values >350 mg/dL, and 1.1 for values >400 mg/dL.
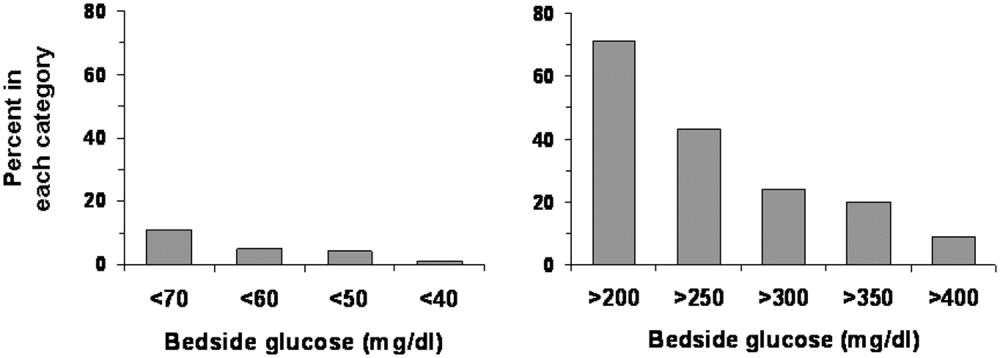
Changes in Therapy
Overall, changes were made in the hyperglycemia therapy of only 34% of patients. Treatment was changed for 50% of patients who had at least one glucose reading >200 mg/dL, and 89% of patients who had at least one glucose reading <70 mg/dL. Figure 5 shows whether changes in treatment occurred by tertiles of average bedside glucose. The percentage of patients with a change in therapy increased with worse hyperglycemia, although 32% in the third tertile still had not had a change in treatment. The odds of those in the second tertile having a change in therapy (compared with those in the first tertile) were 1.9 (95% confidence interval 0.556.25, P = .32), but were 5.6 (95% confidence interval 1.6818.7, P = .005) for patients in the third tertile. The frequency of glucose values <70 mg/dL was 1.8 per person per 100 measurements for patients in the first tertile, 1.1 for patients in the second tertile, but only 0.29 per person per 100 measurements for patients in the third tertile. The average number of glucose measurements >200 mg/dL per person was 2.9 per 100 measurements for patients in the first tertile, 22.7 for patients in the second tertile, and 60.0 for patients in the third tertile (not shown).
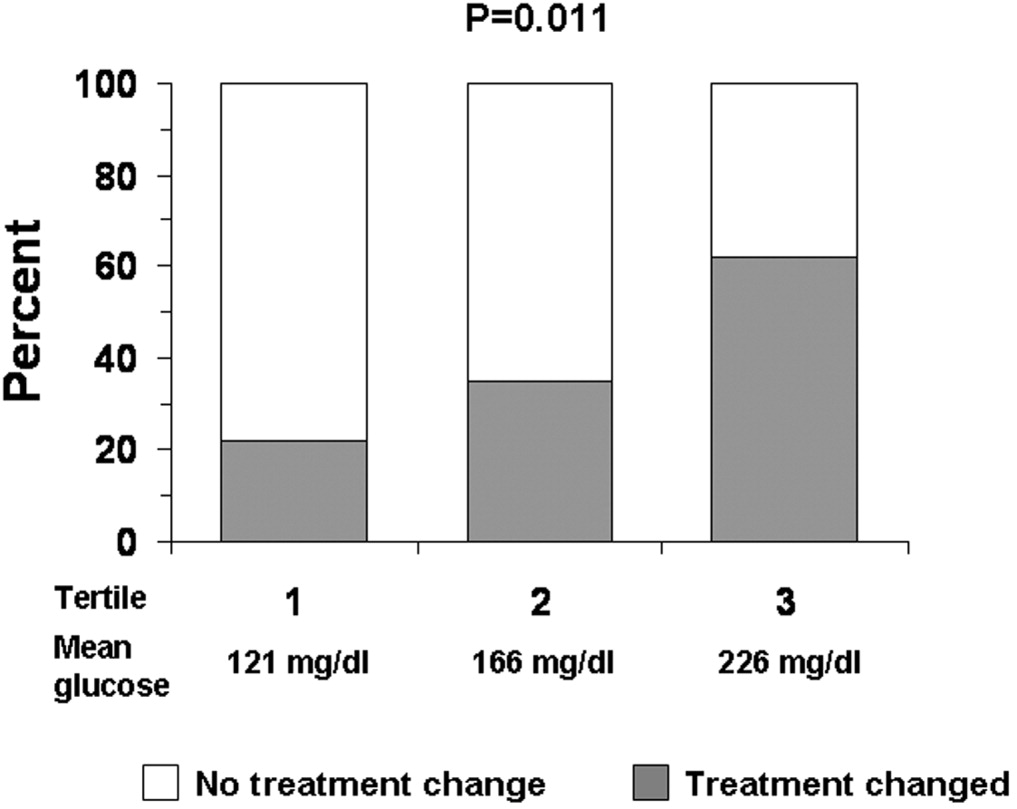
DISCUSSION
Just as clinical trials in the outpatient setting have demonstrated the benefits of good glycemic control,2830 recent studies have also suggested that treatment of hyperglycemia during hospitalization can improve outcomes.10, 11 Consequently, there has been increased attention to the management of glucose in the hospital, with recognition of the need for inpatient‐specific standards for diabetes care.10, 11, 31 Optimization of management and of education about diabetes and hyperglycemia in the hospital requires better understanding of current care practices in order to determine where to direct interventions.
Nearly all the 90 patients whose records we reviewed had preexisting diabetes or a known potential glucose abnormality that was documented either at the time of, or just prior to, hospital admission. The observation that most patients had orders for bedside glucose monitoring also indicated that practitioners were aware of the diagnosis when the patient was admitted. Although clinicians seemed to be aware of the potential problem of glucoseand the majority of clinicians did some trackinga substantial number of hospitalizations (nearly 40%) had no documentation of diabetes or hyperglycemia after admission. If diabetes was not the principal reason for hospitalization, it is possible that the primary team did not focus on managing hyperglycemia. Nonetheless, the hospital encounter does represent an opportunity to address glucose management and perhaps improve care and outcomes, even if the patient was admitted for an unrelated condition.32 Because the average length of stay was almost 5 days, there should have been sufficient time to address diabetes in most patients.
Although most patients had the condition of their diabetes documented in their discharge notes, a substantial proportion of the discharge notes did not mention an outpatient plan to follow up on the diabetes or hyperglycemia. A recent study suggested that direct referral for outpatient diabetes services increased the chances of patient follow‐up.33 Educating practitioners about the need to emphasize to patients the importance of diabetes postdischarge care is a program that could be developed and implemented in the hospital setting.
Although bedside glucose monitoring was appropriately ordered in most instances, the actual recording of values and the assessment of glucose control were documented in the records of only about half the patients during their hospitalizations. Moreover, even among patients who had high bedside glucose levels, changes in therapy often did not occur. Clinician concern about inducing hypoglycemia in hospitalized patients has been cited as a factor limiting the intensification of treatment for diabetes.34 The frequency in our facility of documented low blood glucose values was small, although there may have been unrecognized episodes. However, missed events were probably unusual, given the daily average of 4 bedside glucose measurements per patient, ongoing nursing staff contact with patients, and a formal policy to document and treat hypoglycemia. We found that hyperglycemia was far more common than hypoglycemia and that there were likely many opportunities to control blood glucose more rigorously.
Practitioners appeared to be responding to hypoglycemia, as a large proportion of the patients with a glucose reading of <70 mg/dL had a change in therapy. However, the response to hyperglycemia was delayedthe odds of therapy being changed were significant only for patients whose glucose levels were in the third tertile. Despite evidence of hyperglycemia and the low frequency of hypoglycemia of those whose glucose levels were in the second and third tertiles, a substantial proportion of patients did not have their therapy changed. Combined with the observation that glucose data and diabetes were often not documented, our data suggest that there may be a problem of clinical inertia in the inpatient setting. Clinical inertia has been defined as not initiating or intensifying therapy when doing so is indicated.35, 36 Other reports have also documented clinical inertia in the outpatient environment.23, 3741 Overcoming clinical inertia, at least in regard to diabetes management, can improve glycemic control in patients.35 To improve the management of hyperglycemia in the hospital, educational interventions must be developed to teach health care practitioners effective strategies for glucose reduction. We did not quantify the changes in therapy (eg, how much insulin was changed or in what direction), only whether a change had been made. The observation that the proportion of cases on insulin at discharge was less than on admission day suggests that there may actually have been deintensification of therapy taking placesome of the cases in which therapy was changed, therefore, likely included instances of negative therapeutic momentum despite evidence of hyperglycemia. The control of inpatient hyperglycemia will likely require frequent changes in therapy, as it does in the outpatient setting, and detailed information about treatment strategies actually employed will be necessary to design educational programs.
One limitation of our analysis was that the study was retrospective, which did not allow assessment of the reasons underlying the behavior of the clinicians, such as why they did not document diabetes or change therapy. We selected a 5% sample for our study as per common methods.20, 25, 26 Thus, although the 90 patients making up the sample were randomly selected and were not different demographically from the larger population of patients admitted with diabetes, the number of cases we reviewed was small compared with the actual number of discharged patients with diabetes. Cases were diagnosed by diagnosis codes; therefore, it is likely that some diabetes cases were missed, and other patients with hyperglycemia may not have had the diagnosis even documented.8, 24 Our study design and sample size precluded a comparison of outcomes between cases with in which a consultant was involved with those in which a consultant was not involved or a comparison of cases according to type of consultant involved.1216 Finally, our study focused on noncritically ill patients; thus, our findings cannot be generalized to care provided in the intensive care unit.
There are no definitive guidelines on what method (ie, blood or bedside glucose) should be used to evaluate glycemic control in the hospital. The methods we used here can serve as means to benchmark and track improvement in glycemic control. The observations that most patients had bedside glucose monitoring ordered and that the frequency of these measurements was high compared with the frequency of actual blood glucose assessments support the idea that practitioners favored this method to evaluate the level of glycemic control in the hospital. In practice, it is bedside glucose evaluation that clinicians use to make decisions about day‐to‐day treatment of hyperglycemia. In our facility, the method for bedside glucose monitoring is standardized and is part of a quality assurance program. Moreover, the high average frequency of bedside blood glucose determination increased the chance of detecting hyper‐ and hypoglycemic events.
Current guidelines provide suggestions about target pre‐ and postprandial glucose levels for noncritically ill patients.11 However, these targets are not universally recognized.42 For instance, the Institutes for Healthcare Improvement's Prevent Surgical Site Infections initiative defines a glucose level of <200 mg/dL as its target perioperative glucose control level.43 In practice, it can be difficult to assess glucose control in terms of pre‐ and postprandial categories. Although bedside glucose monitoring in our facility is typically ordered before meals and at bedtime, in many cases prolonged periods of patient fasting, disrupted meal schedules, mismatching insulin with meals, and use of continuous parental and enteral nutritional support all make it difficult to assess pre‐ and postprandial glycemic control retrospectively. Hence, we used as our measures the value of the bedside glucose averaged over the length of the hospital stay and the number of hyper‐ and hypoglycemic events.
In general, our study was hampered by a lack of hospital‐specific process measures to evaluate the quality of inpatient diabetes care. Process measures such as the frequency of hemoglobin A1c monitoring or performance of ophthalmologic examinations,1723 which are commonly used to assess quality of diabetes care in the outpatient arena, may not be optimal variables for evaluating care in the hospital. New methods to guide efforts to improve the quality of inpatient management of diabetes and hyperglycemia are needed.
Despite these limitations, our analysis was helpful in providing direction about how to enhance the care of hospitalized patients with hyperglycemia or known diabetes. Constructing institution‐specific management guidelines for the care of inpatient diabetes and hyperglycemia would provide a yardstick against which to measure the care provided by both the hospital and the individual clinician. Educational programs can be developed to increase awareness among practitioners of the importance of inpatient glucose control and of the need to improve ongoing documentation of the problem. Exploring practitioner barriers to treatment of inpatient hyperglycemia should be an essential component of this educational process. Finally, consensus strategies on when to initiate and change therapy should be designed so that hyperglycemia in the hospital can be managed more effectively. All these areas must be addressed to assure delivery of the highest‐quality inpatient care to patients with diabetes.
- ,,,,.Diabetes‐related hospitalization and hospital utilization. In:Diabetes in America: National Diabetes Data Group.2nd ed.Bethesda (MD):National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases;1995:553–563.
- .Hospitalization in the United States, 1997: HCUP fact book no. 1: diagnosis, charges, length of stay, insurance coverage, discharge status, inhospital deaths.Rockville (MD):Agency for Healthcare Research and Quality;2000.
- Centers for Disease Control and Prevention. Hospitalization for diabetes as first‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmfirst/table1.htm. Accessed: June 2,2005.
- Centers for Disease Control and Prevention. Hospitalizations for diabetes as any‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed: June 2,2005.
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26:1421–1426.
- ,,,.Excess costs of medical care for patients with diabetes in a managed care population.Diabetes Care.1997;20:1396–1402.
- ,,,American Diabetes Association.Economic costs of diabetes in the US in 2002.Diabetes Care.2003;26:917–932.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,,,,American Diabetes Association Diabetes in Hospitals Writing Committee, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591. Erratum in: Diabetes Care. 2004;27:856 and Diabetes Care. 2004;27:1255.
- ,,,,,,American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control, et al.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10:77–82.
- ,,,.Effect of physician specialty on outcomes in diabetic ketoacidosis.Diabetes Care.1999;22:1790–1795.
- ,,,.Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes.Am J Med.1995;99:22–28.
- ,,.Effects of an intervention by a diabetes team in hospitalized patients with diabetes.Diabetes Care.1997;20:1553–1555.
- ,.Nursing case management: an innovative model of care for hospitalized patients with diabetes.Diabetes Educ.1993;19:517–521.
- ,,,,.Evaluation of a hospital diabetes specialist nursing service: a randomized controlled trial.Diabet Med.2001;18:301–307.
- ,,,,,.Variation in office‐based quality. A claims‐based profile of care provided to Medicare patients with diabetes.JAMA.1995;273:1503–1508.
- ,,,,,, et al.Outpatient management of diabetes mellitus in five Arizona Medicare managed care plans.Am J Med Qual.1996;11:87–93.
- ,,,.Quality of outpatient care provided to diabetic patients: a health maintenance organization experience.Diabetes Care.1996;19:601–6.
- United States General Accounting Office: report to the Chairman, Subcommittee on Health and Environment, Committee on Commerce, House of Representatives.Medicare: most beneficiaries with diabetes do not receive recommended monitoring services. GAO/HEHS‐97–48.1997.
- ,,,,.Care of patients with type II diabetes: a study of family physicians' compliance with clinical practice guidelines.J Fam Pract.1997;44:374–381.
- ,,,,,.A diabetes report card for the United States: quality of care in the 1990s.Ann Intern Med.2002;136:565–574.
- ,,,University HealthSystem Consortium (UHC) Diabetes Benchmarking Project Team.Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change.Diabetes Care.2005;28:337–442.
- ,,,.An audit of the management and outcome of hospital inpatients with diabetes: resource planning implications for the diabetes care team.Diabet Med.1992;9:753–755.
- .Improving outcomes in public health practice: strategy and methods.Gaithersburg (MD):Aspen Publishers;1997:175–213.
- ,,,,,.Outpatient diabetes management of Medicare beneficiaries in four Mississippi fee‐for‐service primary care clinics.J Miss State Med Assoc.1999;40:8–13.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- The Diabetes Control and Complications Trial Research Group.The effect of intensive treatment of diabetes on the development and progression of long‐term complications in insulin‐dependent diabetes mellitus.N Engl J Med.1993;329:977–986.
- UK Prospective Diabetes Study (UKPDS) Group.Intensive blood‐glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33).Lancet.1998;352:837–53. Erratum in: Lancet. 1999;354:602.
- UK Prospective Diabetes Study (UKPDS) Group.Effect of intensive blood‐glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34).Lancet.1998;352:854–65. Erratum in: Lancet. 1998;352:1557.
- ,,.Current standards of care for inpatient glycemic management and metabolic control: is it time for definite standards and targets?Endocr Pract.2004;10(Suppl 2):10–12.
- ,.Windows of opportunity to improve diabetes care when patients with diabetes are hospitalized for other conditions.Diabetes Care.2001;24:1371–1376.
- ,,, et al.Inpatient to outpatient transfer of care in urban patients with diabetes: patterns and determinants of immediate postdischarge follow‐up.Arch Intern Med.2004;164:447–453.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10(Suppl 2):89–99.
- ,,, et al.Diabetes in urban African‐Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes.Diabetes Care.1999;22:1494–1500.
- ,,, et al.Clinical inertia.Ann Intern Med.2001;135:825–834.
- .Management of older hypertensive patients: is there a difference in approach?J Clin Hypertens (Greenwich).2003;5(Suppl 4):11–16.
- ,,, et al.Narrowing the gap in hypertension: effectiveness of a complex antihypertensive program in the elderly.Dis Manag.2004;7:235–243.
- ,,, et al.Clinical inertia in the management of Type 2 diabetes metabolic risk factors.Diabet Med.2004;21:150–155.
- ,.Clinical inertia: errors of omission in drug therapy.Am J Health Syst Pharm.2004;61:401–404.
- .Overcome clinical inertia to control systolic blood pressure.Arch Intern Med.2003;163:2677–2678.
- ,.Counterpoint: inpatient glucose management: a premature call to arms?Diabetes Care.2005;28:976–979.
- Institute for Healthcare Improvement. Getting started kit: prevent surgical site infections. Available from: www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed June 2,2005.
- ,,,,.Diabetes‐related hospitalization and hospital utilization. In:Diabetes in America: National Diabetes Data Group.2nd ed.Bethesda (MD):National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases;1995:553–563.
- .Hospitalization in the United States, 1997: HCUP fact book no. 1: diagnosis, charges, length of stay, insurance coverage, discharge status, inhospital deaths.Rockville (MD):Agency for Healthcare Research and Quality;2000.
- Centers for Disease Control and Prevention. Hospitalization for diabetes as first‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmfirst/table1.htm. Accessed: June 2,2005.
- Centers for Disease Control and Prevention. Hospitalizations for diabetes as any‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed: June 2,2005.
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26:1421–1426.
- ,,,.Excess costs of medical care for patients with diabetes in a managed care population.Diabetes Care.1997;20:1396–1402.
- ,,,American Diabetes Association.Economic costs of diabetes in the US in 2002.Diabetes Care.2003;26:917–932.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,,,,American Diabetes Association Diabetes in Hospitals Writing Committee, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591. Erratum in: Diabetes Care. 2004;27:856 and Diabetes Care. 2004;27:1255.
- ,,,,,,American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control, et al.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10:77–82.
- ,,,.Effect of physician specialty on outcomes in diabetic ketoacidosis.Diabetes Care.1999;22:1790–1795.
- ,,,.Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes.Am J Med.1995;99:22–28.
- ,,.Effects of an intervention by a diabetes team in hospitalized patients with diabetes.Diabetes Care.1997;20:1553–1555.
- ,.Nursing case management: an innovative model of care for hospitalized patients with diabetes.Diabetes Educ.1993;19:517–521.
- ,,,,.Evaluation of a hospital diabetes specialist nursing service: a randomized controlled trial.Diabet Med.2001;18:301–307.
- ,,,,,.Variation in office‐based quality. A claims‐based profile of care provided to Medicare patients with diabetes.JAMA.1995;273:1503–1508.
- ,,,,,, et al.Outpatient management of diabetes mellitus in five Arizona Medicare managed care plans.Am J Med Qual.1996;11:87–93.
- ,,,.Quality of outpatient care provided to diabetic patients: a health maintenance organization experience.Diabetes Care.1996;19:601–6.
- United States General Accounting Office: report to the Chairman, Subcommittee on Health and Environment, Committee on Commerce, House of Representatives.Medicare: most beneficiaries with diabetes do not receive recommended monitoring services. GAO/HEHS‐97–48.1997.
- ,,,,.Care of patients with type II diabetes: a study of family physicians' compliance with clinical practice guidelines.J Fam Pract.1997;44:374–381.
- ,,,,,.A diabetes report card for the United States: quality of care in the 1990s.Ann Intern Med.2002;136:565–574.
- ,,,University HealthSystem Consortium (UHC) Diabetes Benchmarking Project Team.Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change.Diabetes Care.2005;28:337–442.
- ,,,.An audit of the management and outcome of hospital inpatients with diabetes: resource planning implications for the diabetes care team.Diabet Med.1992;9:753–755.
- .Improving outcomes in public health practice: strategy and methods.Gaithersburg (MD):Aspen Publishers;1997:175–213.
- ,,,,,.Outpatient diabetes management of Medicare beneficiaries in four Mississippi fee‐for‐service primary care clinics.J Miss State Med Assoc.1999;40:8–13.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- The Diabetes Control and Complications Trial Research Group.The effect of intensive treatment of diabetes on the development and progression of long‐term complications in insulin‐dependent diabetes mellitus.N Engl J Med.1993;329:977–986.
- UK Prospective Diabetes Study (UKPDS) Group.Intensive blood‐glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33).Lancet.1998;352:837–53. Erratum in: Lancet. 1999;354:602.
- UK Prospective Diabetes Study (UKPDS) Group.Effect of intensive blood‐glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34).Lancet.1998;352:854–65. Erratum in: Lancet. 1998;352:1557.
- ,,.Current standards of care for inpatient glycemic management and metabolic control: is it time for definite standards and targets?Endocr Pract.2004;10(Suppl 2):10–12.
- ,.Windows of opportunity to improve diabetes care when patients with diabetes are hospitalized for other conditions.Diabetes Care.2001;24:1371–1376.
- ,,, et al.Inpatient to outpatient transfer of care in urban patients with diabetes: patterns and determinants of immediate postdischarge follow‐up.Arch Intern Med.2004;164:447–453.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10(Suppl 2):89–99.
- ,,, et al.Diabetes in urban African‐Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes.Diabetes Care.1999;22:1494–1500.
- ,,, et al.Clinical inertia.Ann Intern Med.2001;135:825–834.
- .Management of older hypertensive patients: is there a difference in approach?J Clin Hypertens (Greenwich).2003;5(Suppl 4):11–16.
- ,,, et al.Narrowing the gap in hypertension: effectiveness of a complex antihypertensive program in the elderly.Dis Manag.2004;7:235–243.
- ,,, et al.Clinical inertia in the management of Type 2 diabetes metabolic risk factors.Diabet Med.2004;21:150–155.
- ,.Clinical inertia: errors of omission in drug therapy.Am J Health Syst Pharm.2004;61:401–404.
- .Overcome clinical inertia to control systolic blood pressure.Arch Intern Med.2003;163:2677–2678.
- ,.Counterpoint: inpatient glucose management: a premature call to arms?Diabetes Care.2005;28:976–979.
- Institute for Healthcare Improvement. Getting started kit: prevent surgical site infections. Available from: www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed June 2,2005.
Copyright © 2006 Society of Hospital Medicine