User login
Now Available: The 2017 JHM Core Competencies Compendium.
Want all 52 Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
Want all 52 Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
Want all 52 Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
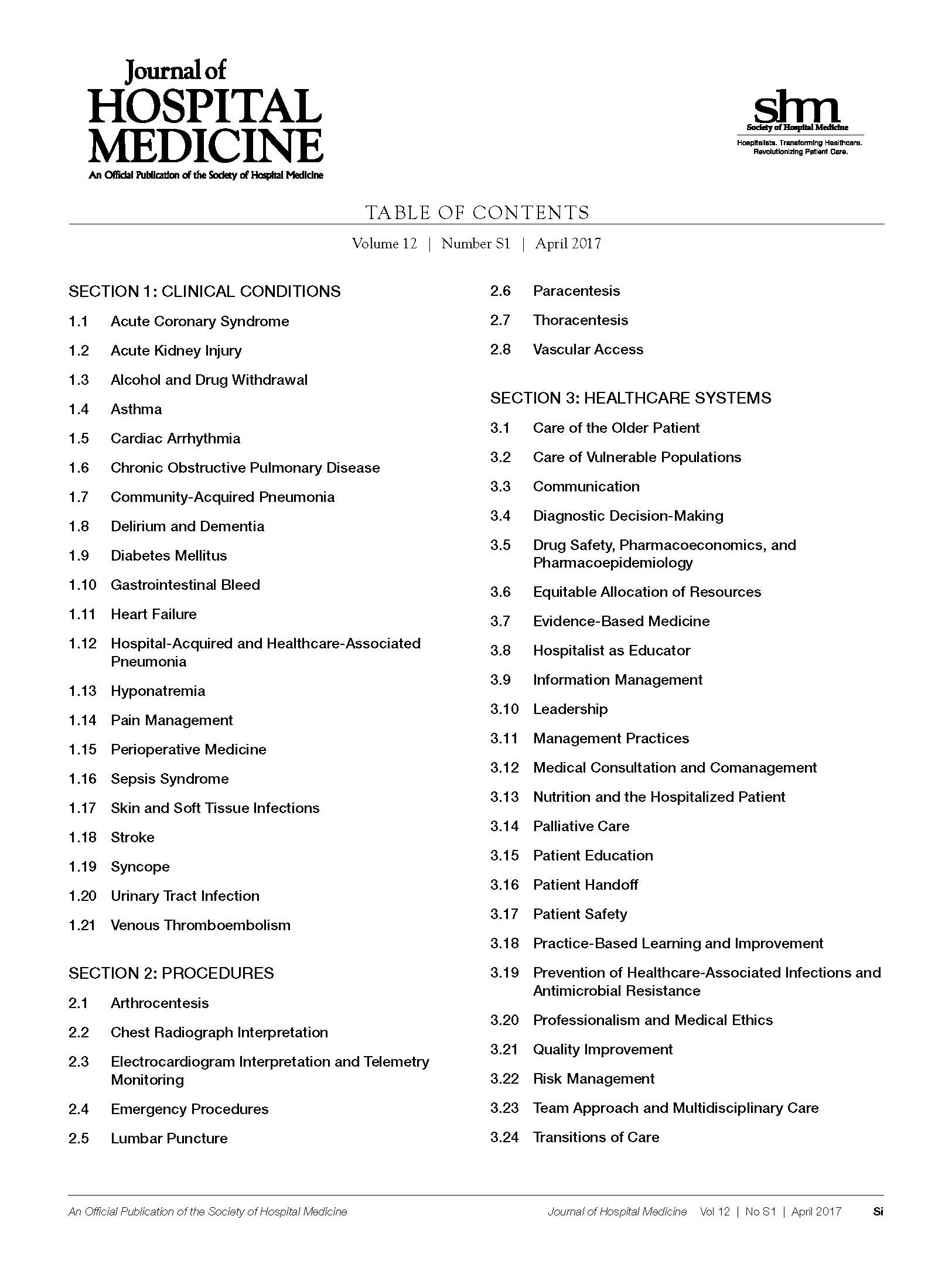
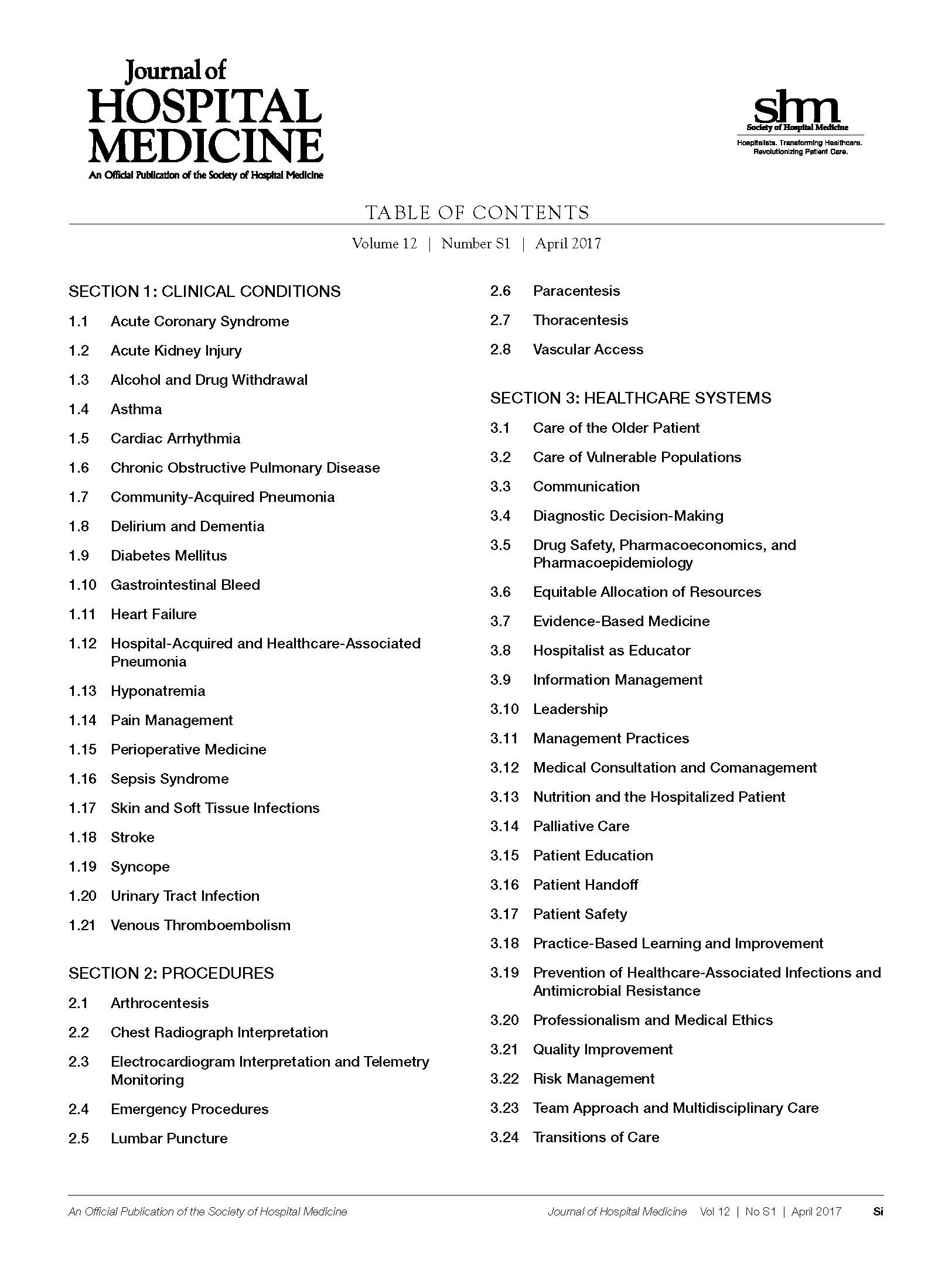
The 2017 JHM Core Competencies Table of Contents.
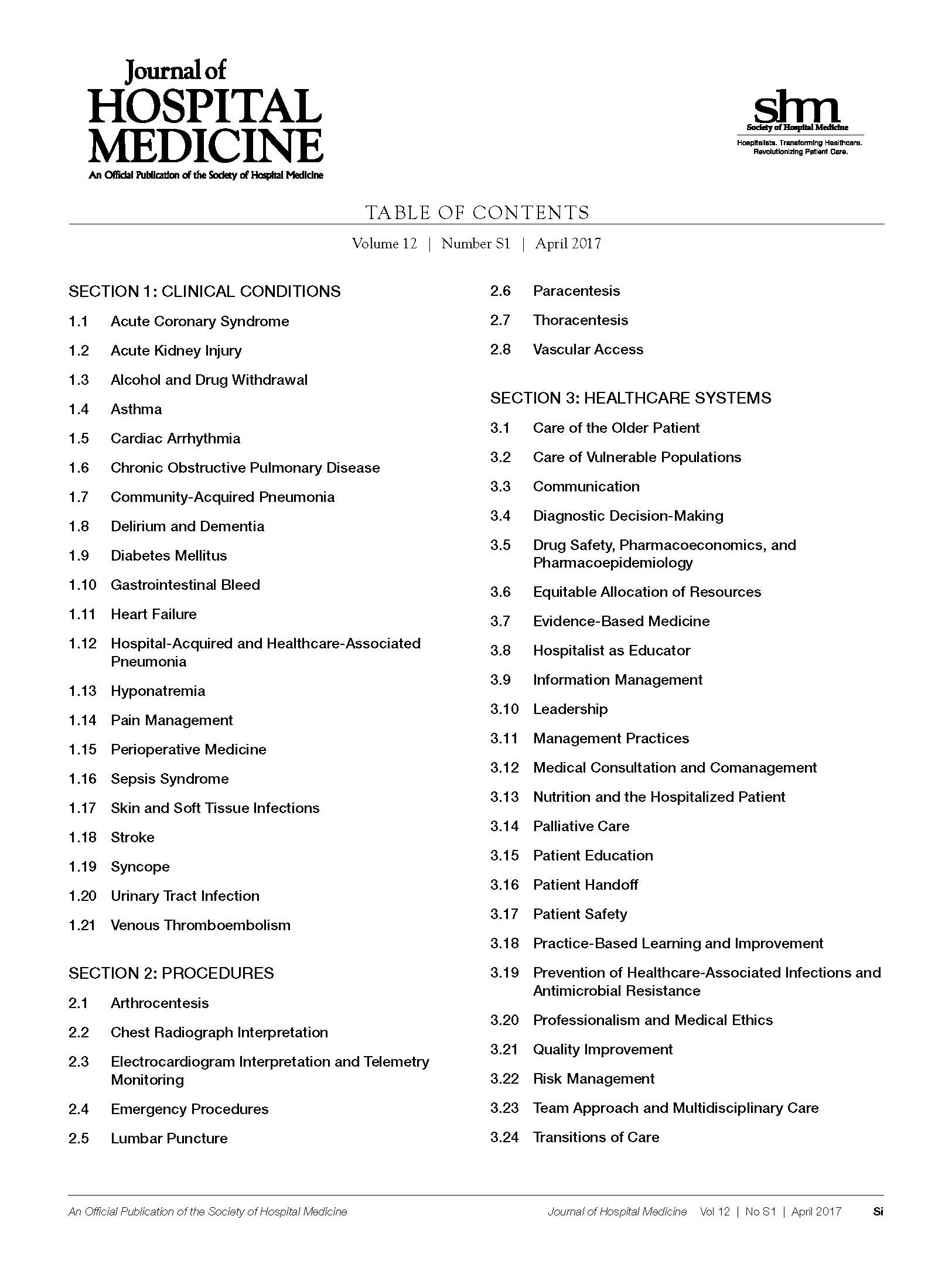
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
Acute Kidney Injury. 2017 Hospital Medicine Revised Core Competencies
Acute kidney injury (AKI), also known as acute renal failure (ARF), is a decline in renal function over a period of hours or days that results in the accumulation of nitrogenous waste products and an impaired ability to maintain fluid/electrolyte/acid-base homeostasis. Epidemiologic studies of AKI are confounded by inconsistent definitions and underreporting. The average incidence is estimated to be 23.8 cases per 1000 hospital discharges.1Approximately 5% to 20% of critically ill patients experience AKI during the course of their illness.2 AKI may present in isolation, develop as a complication of other comorbid illness, or result as a deleterious adverse effect of treatment or diagnostic interventions. Uncomplicated AKI is associated with a mortality rate of up to 10%.3-6 Patients with AKI and multiorgan failure have mortality rates higher than 50%.3-6 AKI is associated with an increased length of hospital stay; a rise in serum creatinine of 0.5 mg/dL or greater while hospitalized confers a 3.5-day increase in length of stay.7 Hospitalists facilitate the expeditious evaluation and management of AKI to improve patient outcomes, optimize resource use, and reduce length of stay. Hospitalists can also advocate and initiate preventive strategies to reduce the incidence of secondary AKI.
KNOWLEDGE
Hospitalists should be able to:
Describe the symptoms and signs of AKI.
Describe and differentiate pathophysiologic causes of AKI including prerenal, intrinsic renal, and postrenal processes.
Differentiate among the causes of prerenal, intrinsic renal, and postrenal types of AKI.
Describe a logical sequence of indicated tests required to evaluate etiologies of AKI based on classification of AKI type.
List common potentially nephrotoxic agents that can cause or worsen AKI.
Explain the indications, contraindications, and mechanisms of action of the interventions used to treat AKI.
Explain the indications, contraindications, benefits, and risks of acute hemodialysis.
Recognize indications for specialty consultation for AKI and the role of nephrology and/or urology specialists.
Describe criteria, including specific measures of clinical stability, that must be met before discharging patients with AKI.
Explain the specific goals that should be met to ensure safe transitions of care for patients with AKI.
SKILLS
Hospitalists should be able to:
Assess patients with suspected AKI in a timely manner and manage or comanage the patient with the primary requesting service.
Elicit a thorough and relevant medical history with emphasis on factors predisposing or contributing to the development of AKI.
Review all drug use including prescription and over-the-counter medications, herbal remedies, nutritional supplements, and illicit drugs to identify common potential nephrotoxins.
Perform a physical examination to assess volume status and to identify underlying comorbid states that may predispose to the development of AKI.
Order and interpret results of indicated diagnostic studies that may include urinalysis and microscopic sediment analysis, urinary diagnostic indices, urinary protein excretion, serologic evaluation, and renal imaging.
Interpret common clinical, laboratory, and imaging findings used to evaluate and follow the severity of AKI.
Diagnose common complications, such as electrolyte abnormalities, that occur with AKI and institute corrective measures.
Calculate estimated creatinine clearance for medication dosage adjustments when indicated.
Identify patients at risk for developing AKI and institute appropriate preventive measures including avoidance of unnecessary radiographic contrast exposure and adherence to evidence-based interventions to reduce the risk of contrast-induced nephropathy.
Coordinate appropriate nutritional and metabolic interventions.
Formulate an AKI treatment plan tailored to the individual patient, which may include fluid management, pharmacologic agents, nutritional recommendations, and patient education.
Identify and treat factors that may complicate the management of AKI, including extreme blood pressure, underlying infections, and the sequelae of electrolyte abnormalities.
Communicate with patients and families to explain the cause and prognosis of AKI.
Communicate with patients and families to explain the rationale for the use of radiographic tests and procedures and the benefit and potential adverse effects of radiographic contrast agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, nutrition, and pharmacy services, in the care of patients with AKI that begins at admission and continues through all care transitions.
Follow evidence-based recommendations, protocols, and risk-stratification tools for the treatment of AKI.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Advocate for, establish, and support initiatives to reduce the incidence of iatrogenic AKI.
Lead, coordinate, and/or participate in multidisciplinary teams (including nephrology, nursing, pharmacy, and nutrition services) to improve processes that facilitate early identification of AKI and improved patient outcomes.
Lead, coordinate, and/or participate in multidisciplinary initiatives to promote patient safety and optimize management strategies for AKI.
1. Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992-2001. J Am Soc Nephrol. 2006;17(4):1135-1142.
2. Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30(9):2051-2058.
3. Cosentino F, Chaff C, Piedmonte M. Risk factors influencing survival in ICU acute renal failure. Nephrol Dial Transplant. 1994;9(Suppl 4):179-182.
4. Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT. Hospital-acquired renal insufficiency: a prospective study. Am H Med. 1983;74(2):243-248.
5. Liano F, Junco E, Pascual J, Madero R, Verde E. The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group. Kidney Int Suppl. 1998;66:S16-S24.
6. Shusterman N, Strom BL, Murray TG, Morrison G, West SL, Maislin G. Risk factors and outcome of hospital-acquired acute renal failure. Clinical epidemiologic study. Am J Med. 1987;83(1):65-71.
7. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16(11):3365-3370.
Acute kidney injury (AKI), also known as acute renal failure (ARF), is a decline in renal function over a period of hours or days that results in the accumulation of nitrogenous waste products and an impaired ability to maintain fluid/electrolyte/acid-base homeostasis. Epidemiologic studies of AKI are confounded by inconsistent definitions and underreporting. The average incidence is estimated to be 23.8 cases per 1000 hospital discharges.1Approximately 5% to 20% of critically ill patients experience AKI during the course of their illness.2 AKI may present in isolation, develop as a complication of other comorbid illness, or result as a deleterious adverse effect of treatment or diagnostic interventions. Uncomplicated AKI is associated with a mortality rate of up to 10%.3-6 Patients with AKI and multiorgan failure have mortality rates higher than 50%.3-6 AKI is associated with an increased length of hospital stay; a rise in serum creatinine of 0.5 mg/dL or greater while hospitalized confers a 3.5-day increase in length of stay.7 Hospitalists facilitate the expeditious evaluation and management of AKI to improve patient outcomes, optimize resource use, and reduce length of stay. Hospitalists can also advocate and initiate preventive strategies to reduce the incidence of secondary AKI.
KNOWLEDGE
Hospitalists should be able to:
Describe the symptoms and signs of AKI.
Describe and differentiate pathophysiologic causes of AKI including prerenal, intrinsic renal, and postrenal processes.
Differentiate among the causes of prerenal, intrinsic renal, and postrenal types of AKI.
Describe a logical sequence of indicated tests required to evaluate etiologies of AKI based on classification of AKI type.
List common potentially nephrotoxic agents that can cause or worsen AKI.
Explain the indications, contraindications, and mechanisms of action of the interventions used to treat AKI.
Explain the indications, contraindications, benefits, and risks of acute hemodialysis.
Recognize indications for specialty consultation for AKI and the role of nephrology and/or urology specialists.
Describe criteria, including specific measures of clinical stability, that must be met before discharging patients with AKI.
Explain the specific goals that should be met to ensure safe transitions of care for patients with AKI.
SKILLS
Hospitalists should be able to:
Assess patients with suspected AKI in a timely manner and manage or comanage the patient with the primary requesting service.
Elicit a thorough and relevant medical history with emphasis on factors predisposing or contributing to the development of AKI.
Review all drug use including prescription and over-the-counter medications, herbal remedies, nutritional supplements, and illicit drugs to identify common potential nephrotoxins.
Perform a physical examination to assess volume status and to identify underlying comorbid states that may predispose to the development of AKI.
Order and interpret results of indicated diagnostic studies that may include urinalysis and microscopic sediment analysis, urinary diagnostic indices, urinary protein excretion, serologic evaluation, and renal imaging.
Interpret common clinical, laboratory, and imaging findings used to evaluate and follow the severity of AKI.
Diagnose common complications, such as electrolyte abnormalities, that occur with AKI and institute corrective measures.
Calculate estimated creatinine clearance for medication dosage adjustments when indicated.
Identify patients at risk for developing AKI and institute appropriate preventive measures including avoidance of unnecessary radiographic contrast exposure and adherence to evidence-based interventions to reduce the risk of contrast-induced nephropathy.
Coordinate appropriate nutritional and metabolic interventions.
Formulate an AKI treatment plan tailored to the individual patient, which may include fluid management, pharmacologic agents, nutritional recommendations, and patient education.
Identify and treat factors that may complicate the management of AKI, including extreme blood pressure, underlying infections, and the sequelae of electrolyte abnormalities.
Communicate with patients and families to explain the cause and prognosis of AKI.
Communicate with patients and families to explain the rationale for the use of radiographic tests and procedures and the benefit and potential adverse effects of radiographic contrast agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, nutrition, and pharmacy services, in the care of patients with AKI that begins at admission and continues through all care transitions.
Follow evidence-based recommendations, protocols, and risk-stratification tools for the treatment of AKI.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Advocate for, establish, and support initiatives to reduce the incidence of iatrogenic AKI.
Lead, coordinate, and/or participate in multidisciplinary teams (including nephrology, nursing, pharmacy, and nutrition services) to improve processes that facilitate early identification of AKI and improved patient outcomes.
Lead, coordinate, and/or participate in multidisciplinary initiatives to promote patient safety and optimize management strategies for AKI.
Acute kidney injury (AKI), also known as acute renal failure (ARF), is a decline in renal function over a period of hours or days that results in the accumulation of nitrogenous waste products and an impaired ability to maintain fluid/electrolyte/acid-base homeostasis. Epidemiologic studies of AKI are confounded by inconsistent definitions and underreporting. The average incidence is estimated to be 23.8 cases per 1000 hospital discharges.1Approximately 5% to 20% of critically ill patients experience AKI during the course of their illness.2 AKI may present in isolation, develop as a complication of other comorbid illness, or result as a deleterious adverse effect of treatment or diagnostic interventions. Uncomplicated AKI is associated with a mortality rate of up to 10%.3-6 Patients with AKI and multiorgan failure have mortality rates higher than 50%.3-6 AKI is associated with an increased length of hospital stay; a rise in serum creatinine of 0.5 mg/dL or greater while hospitalized confers a 3.5-day increase in length of stay.7 Hospitalists facilitate the expeditious evaluation and management of AKI to improve patient outcomes, optimize resource use, and reduce length of stay. Hospitalists can also advocate and initiate preventive strategies to reduce the incidence of secondary AKI.
KNOWLEDGE
Hospitalists should be able to:
Describe the symptoms and signs of AKI.
Describe and differentiate pathophysiologic causes of AKI including prerenal, intrinsic renal, and postrenal processes.
Differentiate among the causes of prerenal, intrinsic renal, and postrenal types of AKI.
Describe a logical sequence of indicated tests required to evaluate etiologies of AKI based on classification of AKI type.
List common potentially nephrotoxic agents that can cause or worsen AKI.
Explain the indications, contraindications, and mechanisms of action of the interventions used to treat AKI.
Explain the indications, contraindications, benefits, and risks of acute hemodialysis.
Recognize indications for specialty consultation for AKI and the role of nephrology and/or urology specialists.
Describe criteria, including specific measures of clinical stability, that must be met before discharging patients with AKI.
Explain the specific goals that should be met to ensure safe transitions of care for patients with AKI.
SKILLS
Hospitalists should be able to:
Assess patients with suspected AKI in a timely manner and manage or comanage the patient with the primary requesting service.
Elicit a thorough and relevant medical history with emphasis on factors predisposing or contributing to the development of AKI.
Review all drug use including prescription and over-the-counter medications, herbal remedies, nutritional supplements, and illicit drugs to identify common potential nephrotoxins.
Perform a physical examination to assess volume status and to identify underlying comorbid states that may predispose to the development of AKI.
Order and interpret results of indicated diagnostic studies that may include urinalysis and microscopic sediment analysis, urinary diagnostic indices, urinary protein excretion, serologic evaluation, and renal imaging.
Interpret common clinical, laboratory, and imaging findings used to evaluate and follow the severity of AKI.
Diagnose common complications, such as electrolyte abnormalities, that occur with AKI and institute corrective measures.
Calculate estimated creatinine clearance for medication dosage adjustments when indicated.
Identify patients at risk for developing AKI and institute appropriate preventive measures including avoidance of unnecessary radiographic contrast exposure and adherence to evidence-based interventions to reduce the risk of contrast-induced nephropathy.
Coordinate appropriate nutritional and metabolic interventions.
Formulate an AKI treatment plan tailored to the individual patient, which may include fluid management, pharmacologic agents, nutritional recommendations, and patient education.
Identify and treat factors that may complicate the management of AKI, including extreme blood pressure, underlying infections, and the sequelae of electrolyte abnormalities.
Communicate with patients and families to explain the cause and prognosis of AKI.
Communicate with patients and families to explain the rationale for the use of radiographic tests and procedures and the benefit and potential adverse effects of radiographic contrast agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, nutrition, and pharmacy services, in the care of patients with AKI that begins at admission and continues through all care transitions.
Follow evidence-based recommendations, protocols, and risk-stratification tools for the treatment of AKI.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Advocate for, establish, and support initiatives to reduce the incidence of iatrogenic AKI.
Lead, coordinate, and/or participate in multidisciplinary teams (including nephrology, nursing, pharmacy, and nutrition services) to improve processes that facilitate early identification of AKI and improved patient outcomes.
Lead, coordinate, and/or participate in multidisciplinary initiatives to promote patient safety and optimize management strategies for AKI.
1. Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992-2001. J Am Soc Nephrol. 2006;17(4):1135-1142.
2. Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30(9):2051-2058.
3. Cosentino F, Chaff C, Piedmonte M. Risk factors influencing survival in ICU acute renal failure. Nephrol Dial Transplant. 1994;9(Suppl 4):179-182.
4. Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT. Hospital-acquired renal insufficiency: a prospective study. Am H Med. 1983;74(2):243-248.
5. Liano F, Junco E, Pascual J, Madero R, Verde E. The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group. Kidney Int Suppl. 1998;66:S16-S24.
6. Shusterman N, Strom BL, Murray TG, Morrison G, West SL, Maislin G. Risk factors and outcome of hospital-acquired acute renal failure. Clinical epidemiologic study. Am J Med. 1987;83(1):65-71.
7. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16(11):3365-3370.
1. Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992-2001. J Am Soc Nephrol. 2006;17(4):1135-1142.
2. Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30(9):2051-2058.
3. Cosentino F, Chaff C, Piedmonte M. Risk factors influencing survival in ICU acute renal failure. Nephrol Dial Transplant. 1994;9(Suppl 4):179-182.
4. Hou SH, Bushinsky DA, Wish JB, Cohen JJ, Harrington JT. Hospital-acquired renal insufficiency: a prospective study. Am H Med. 1983;74(2):243-248.
5. Liano F, Junco E, Pascual J, Madero R, Verde E. The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group. Kidney Int Suppl. 1998;66:S16-S24.
6. Shusterman N, Strom BL, Murray TG, Morrison G, West SL, Maislin G. Risk factors and outcome of hospital-acquired acute renal failure. Clinical epidemiologic study. Am J Med. 1987;83(1):65-71.
7. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16(11):3365-3370.
© 2017 Society of Hospital Medicine
Alcohol and Drug Withdrawal. 2017 Hospital Medicine Revised Core Competencies
Alcohol and drug withdrawal is a set of signs and symptoms that develops in association with sudden cessation or reduction in the use of alcohol or a number of prescription (particularly opioids and benzodiazepines), over-the-counter (OTC), or illicit drugs. Withdrawal syndromes encompass a broad range of symptoms from mild anxiety and tremulousness to more serious manifestations such as delirium tremens, which occurs in up to 5% of alcohol-dependent persons who undergo withdrawal.1 Withdrawal may occur before hospitalization or during the course of hospitalization. Alcohol- and substance-related disorders account for more than 400,000 hospital discharges each year and are associated with a mean length of stay of approximately 4.6 days.2 Alcohol and drug dependence is often an end product of a combination of biopsychosocial influences, and in most cases, a multidisciplinary approach is necessary to successfully treat affected individuals. Hospitalists can lead their institutions in evidence-based treatment protocols that improve care, reduce costs and length of stay, and facilitate better overall outcomes in patients with substance-related withdrawal syndromes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Describe the effects of drug and alcohol withdrawal on medical illness and the effects of medical illness on substance withdrawal.
Recognize the symptoms and signs of alcohol and drug withdrawal, including withdrawal from prescription and OTC drugs.
Recognize the medical complications from substance use and dependence.
Determine when consultation with a medical toxicologist or expert is necessary.
Distinguish alcohol or drug withdrawal from other causes of delirium.
Differentiate delirium tremens from other alcohol withdrawal syndromes.
Differentiate the clinical manifestations of alcohol or drug intoxication from those of withdrawal.
Recognize different characteristic withdrawal syndromes, such as abstinence syndrome of opioid withdrawal and delirium tremens of alcohol withdrawal.
Describe the tests indicated to evaluate alcohol or drug withdrawal.
Identify patients at increased risk for drug and alcohol withdrawal according to current diagnostic criteria.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat acute alcohol and drug withdrawal.
Identify local trends in illicit drug use.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with drug or alcohol withdrawal.
Explain patient characteristics that portend a poor prognosis.
Explain patient characteristics that indicate a requirement for a higher level of care and/or monitoring.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, with emphasis on substance use.
Assess patients with suspected alcohol or drug withdrawal in a timely manner, identify the level of care required, and manage or comanage the patient with the primary requesting service.
Perform a rapid, efficient, and targeted physical examination to assess for alcohol or drug withdrawal and determine whether life-threatening comorbidities are present.
Assess for common comorbidities in patients with a history of alcohol and drug use.
Formulate a treatment plan tailored to the individual patient, which may include appropriate pharmacologic agents and dosing, route of administration, and nutritional supplementation.
Integrate existing literature and federal regulations into the management of patients with opioid withdrawal syndromes. For patients who are undergoing existing treatment for opioid dependency, communicate with outpatient treatment centers and integrate dosing regimens into care management.
Manage withdrawal syndromes in patients with concomitant medical or surgical issues.
Diagnose oversedation and other complications associated with withdrawal therapies.
Recommend the use of restraints and direct observation to ensure patient safety when appropriate.
Reassure, reorient, and frequently monitor patients in a calm environment.
Use the acute hospitalization as an opportunity to counsel patients about abstinence, recovery, and the medical risks of drug and alcohol use.
Initiate preventive measures before discharge, including alcohol and drug cessation measures.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transition of care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include psychiatry, pharmacy, nursing, and social services, in the treatment of patients with substance use or dependency.
Follow evidence-based national recommendations to guide diagnosis, monitoring, and treatment of withdrawal symptoms.
Act in a nonjudgmental manner when managing the hospitalized patient with substance use.
Establish and maintain an open dialogue with patients and families regarding care goals and limitations.
Appreciate and document the value of appropriate treatment in reducing mortality, duration of delirium, time required to control agitation, adequate control of delirium, treatment of complications, and cost.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams, which may include psychiatry and toxicology, to improve patient safety and management strategies for patients with substance abuse.
Lead, coordinate, and/or participate in the development and promotion of guidelines and/or pathways that facilitate efficient and timely evaluation and treatment of patients with alcohol and drug withdrawal.
Promote the development and use of evidence-based guidelines and protocols for the treatment of withdrawal syndromes.
Advocate for hospital resources to improve the care of patients with substance withdrawal and the environment in which the care is delivered.
Establish relationships with and develop knowledge of community-based organizations that provide support to patients with substance use disorders.
Promote awareness of substance use disorders and screening for them.
Coordinate initiatives to address the increased risk of readmissions associated with substance and polysubstance abuse.
1. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278(2):144-151.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed May 2015.
Alcohol and drug withdrawal is a set of signs and symptoms that develops in association with sudden cessation or reduction in the use of alcohol or a number of prescription (particularly opioids and benzodiazepines), over-the-counter (OTC), or illicit drugs. Withdrawal syndromes encompass a broad range of symptoms from mild anxiety and tremulousness to more serious manifestations such as delirium tremens, which occurs in up to 5% of alcohol-dependent persons who undergo withdrawal.1 Withdrawal may occur before hospitalization or during the course of hospitalization. Alcohol- and substance-related disorders account for more than 400,000 hospital discharges each year and are associated with a mean length of stay of approximately 4.6 days.2 Alcohol and drug dependence is often an end product of a combination of biopsychosocial influences, and in most cases, a multidisciplinary approach is necessary to successfully treat affected individuals. Hospitalists can lead their institutions in evidence-based treatment protocols that improve care, reduce costs and length of stay, and facilitate better overall outcomes in patients with substance-related withdrawal syndromes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Describe the effects of drug and alcohol withdrawal on medical illness and the effects of medical illness on substance withdrawal.
Recognize the symptoms and signs of alcohol and drug withdrawal, including withdrawal from prescription and OTC drugs.
Recognize the medical complications from substance use and dependence.
Determine when consultation with a medical toxicologist or expert is necessary.
Distinguish alcohol or drug withdrawal from other causes of delirium.
Differentiate delirium tremens from other alcohol withdrawal syndromes.
Differentiate the clinical manifestations of alcohol or drug intoxication from those of withdrawal.
Recognize different characteristic withdrawal syndromes, such as abstinence syndrome of opioid withdrawal and delirium tremens of alcohol withdrawal.
Describe the tests indicated to evaluate alcohol or drug withdrawal.
Identify patients at increased risk for drug and alcohol withdrawal according to current diagnostic criteria.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat acute alcohol and drug withdrawal.
Identify local trends in illicit drug use.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with drug or alcohol withdrawal.
Explain patient characteristics that portend a poor prognosis.
Explain patient characteristics that indicate a requirement for a higher level of care and/or monitoring.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, with emphasis on substance use.
Assess patients with suspected alcohol or drug withdrawal in a timely manner, identify the level of care required, and manage or comanage the patient with the primary requesting service.
Perform a rapid, efficient, and targeted physical examination to assess for alcohol or drug withdrawal and determine whether life-threatening comorbidities are present.
Assess for common comorbidities in patients with a history of alcohol and drug use.
Formulate a treatment plan tailored to the individual patient, which may include appropriate pharmacologic agents and dosing, route of administration, and nutritional supplementation.
Integrate existing literature and federal regulations into the management of patients with opioid withdrawal syndromes. For patients who are undergoing existing treatment for opioid dependency, communicate with outpatient treatment centers and integrate dosing regimens into care management.
Manage withdrawal syndromes in patients with concomitant medical or surgical issues.
Diagnose oversedation and other complications associated with withdrawal therapies.
Recommend the use of restraints and direct observation to ensure patient safety when appropriate.
Reassure, reorient, and frequently monitor patients in a calm environment.
Use the acute hospitalization as an opportunity to counsel patients about abstinence, recovery, and the medical risks of drug and alcohol use.
Initiate preventive measures before discharge, including alcohol and drug cessation measures.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transition of care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include psychiatry, pharmacy, nursing, and social services, in the treatment of patients with substance use or dependency.
Follow evidence-based national recommendations to guide diagnosis, monitoring, and treatment of withdrawal symptoms.
Act in a nonjudgmental manner when managing the hospitalized patient with substance use.
Establish and maintain an open dialogue with patients and families regarding care goals and limitations.
Appreciate and document the value of appropriate treatment in reducing mortality, duration of delirium, time required to control agitation, adequate control of delirium, treatment of complications, and cost.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams, which may include psychiatry and toxicology, to improve patient safety and management strategies for patients with substance abuse.
Lead, coordinate, and/or participate in the development and promotion of guidelines and/or pathways that facilitate efficient and timely evaluation and treatment of patients with alcohol and drug withdrawal.
Promote the development and use of evidence-based guidelines and protocols for the treatment of withdrawal syndromes.
Advocate for hospital resources to improve the care of patients with substance withdrawal and the environment in which the care is delivered.
Establish relationships with and develop knowledge of community-based organizations that provide support to patients with substance use disorders.
Promote awareness of substance use disorders and screening for them.
Coordinate initiatives to address the increased risk of readmissions associated with substance and polysubstance abuse.
Alcohol and drug withdrawal is a set of signs and symptoms that develops in association with sudden cessation or reduction in the use of alcohol or a number of prescription (particularly opioids and benzodiazepines), over-the-counter (OTC), or illicit drugs. Withdrawal syndromes encompass a broad range of symptoms from mild anxiety and tremulousness to more serious manifestations such as delirium tremens, which occurs in up to 5% of alcohol-dependent persons who undergo withdrawal.1 Withdrawal may occur before hospitalization or during the course of hospitalization. Alcohol- and substance-related disorders account for more than 400,000 hospital discharges each year and are associated with a mean length of stay of approximately 4.6 days.2 Alcohol and drug dependence is often an end product of a combination of biopsychosocial influences, and in most cases, a multidisciplinary approach is necessary to successfully treat affected individuals. Hospitalists can lead their institutions in evidence-based treatment protocols that improve care, reduce costs and length of stay, and facilitate better overall outcomes in patients with substance-related withdrawal syndromes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Describe the effects of drug and alcohol withdrawal on medical illness and the effects of medical illness on substance withdrawal.
Recognize the symptoms and signs of alcohol and drug withdrawal, including withdrawal from prescription and OTC drugs.
Recognize the medical complications from substance use and dependence.
Determine when consultation with a medical toxicologist or expert is necessary.
Distinguish alcohol or drug withdrawal from other causes of delirium.
Differentiate delirium tremens from other alcohol withdrawal syndromes.
Differentiate the clinical manifestations of alcohol or drug intoxication from those of withdrawal.
Recognize different characteristic withdrawal syndromes, such as abstinence syndrome of opioid withdrawal and delirium tremens of alcohol withdrawal.
Describe the tests indicated to evaluate alcohol or drug withdrawal.
Identify patients at increased risk for drug and alcohol withdrawal according to current diagnostic criteria.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat acute alcohol and drug withdrawal.
Identify local trends in illicit drug use.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with drug or alcohol withdrawal.
Explain patient characteristics that portend a poor prognosis.
Explain patient characteristics that indicate a requirement for a higher level of care and/or monitoring.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, with emphasis on substance use.
Assess patients with suspected alcohol or drug withdrawal in a timely manner, identify the level of care required, and manage or comanage the patient with the primary requesting service.
Perform a rapid, efficient, and targeted physical examination to assess for alcohol or drug withdrawal and determine whether life-threatening comorbidities are present.
Assess for common comorbidities in patients with a history of alcohol and drug use.
Formulate a treatment plan tailored to the individual patient, which may include appropriate pharmacologic agents and dosing, route of administration, and nutritional supplementation.
Integrate existing literature and federal regulations into the management of patients with opioid withdrawal syndromes. For patients who are undergoing existing treatment for opioid dependency, communicate with outpatient treatment centers and integrate dosing regimens into care management.
Manage withdrawal syndromes in patients with concomitant medical or surgical issues.
Diagnose oversedation and other complications associated with withdrawal therapies.
Recommend the use of restraints and direct observation to ensure patient safety when appropriate.
Reassure, reorient, and frequently monitor patients in a calm environment.
Use the acute hospitalization as an opportunity to counsel patients about abstinence, recovery, and the medical risks of drug and alcohol use.
Initiate preventive measures before discharge, including alcohol and drug cessation measures.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transition of care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include psychiatry, pharmacy, nursing, and social services, in the treatment of patients with substance use or dependency.
Follow evidence-based national recommendations to guide diagnosis, monitoring, and treatment of withdrawal symptoms.
Act in a nonjudgmental manner when managing the hospitalized patient with substance use.
Establish and maintain an open dialogue with patients and families regarding care goals and limitations.
Appreciate and document the value of appropriate treatment in reducing mortality, duration of delirium, time required to control agitation, adequate control of delirium, treatment of complications, and cost.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams, which may include psychiatry and toxicology, to improve patient safety and management strategies for patients with substance abuse.
Lead, coordinate, and/or participate in the development and promotion of guidelines and/or pathways that facilitate efficient and timely evaluation and treatment of patients with alcohol and drug withdrawal.
Promote the development and use of evidence-based guidelines and protocols for the treatment of withdrawal syndromes.
Advocate for hospital resources to improve the care of patients with substance withdrawal and the environment in which the care is delivered.
Establish relationships with and develop knowledge of community-based organizations that provide support to patients with substance use disorders.
Promote awareness of substance use disorders and screening for them.
Coordinate initiatives to address the increased risk of readmissions associated with substance and polysubstance abuse.
1. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278(2):144-151.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed May 2015.
1. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278(2):144-151.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed May 2015.
© 2017 Society of Hospital Medicine
Asthma. 2017 Hospital Medicine Revised Core Competencies
Asthma is a chronic disease characterized by airway inflammation and reversible airflow limitation. It is one of the most common chronic conditions and it leads to marked morbidity and mortality in hospitalized patients. In the United States, 1 in 12 persons has asthma and nearly 50% of affected individuals experience an asthma exacerbation each year, accounting for 1.8 million emergency department visits.1,2 Annually, more than 400,000 hospital discharges occur with asthma as the primary diagnosis, with an average length of stay of 3.2 days.2Hospitalists are central to the provision of care for patients with asthma through the use of evidence-based approaches to manage acute exacerbations and to prevent their recurrence. Hospitalists should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to improve efficiency and quality of care and to reduce readmission rates and morbidity and mortality from asthma.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define asthma and describe the pathophysiologic processes that lead to reversible airway obstruction and inflammation.
Identify precipitants of asthma exacerbation, including environmental and occupational exposures.
Recognize the clinical presentation of asthma exacerbation and differentiate it from other acute respiratory and nonrespiratory syndromes.
Describe the role of diagnostic testing, including peak flow monitoring, used for evaluation of asthma exacerbation.
Recognize indications for specialty consultation, including pulmonary and allergy medicine.
Describe evidence-based therapies for the treatment of asthma exacerbations, which may include bronchodilators, systemic corticosteroids, and oxygen.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat asthma.
Recognize signs and symptoms of impending respiratory failure.
Explain the indications for invasive and noninvasive ventilatory support.
List the risk factors for disease severity and death from asthma.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify triggers of asthma and symptoms consistent with asthma exacerbation.
Perform a targeted physical examination to elicit signs consistent with asthma exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Select appropriate diagnostic studies to evaluate severity of asthma exacerbation and interpret the results.
Recognize indications for transfer to the intensive care unit, including impending respiratory failure, and coordinate intubation or noninvasive mechanical ventilation when indicated.
Prescribe appropriate evidence-based pharmacologic therapies during asthma exacerbation, recommending the most appropriate route, dose, frequency, and duration of treatment.
Communicate with patients and families to explain the natural history and prognosis of asthma.
Facilitate discharge planning early during hospitalization.
Develop an asthma action plan in preparation for discharge.
Educate patients and families regarding the indications and appropriate use of daily use inhalers and rescue inhalers for asthmatic control.
Ensure that patients receive training of proper inhaler and peak flow techniques before hospital discharge.
Communicate with patients and families to explain symptoms and signs that should prompt emergent medical attention.
Communicate with patients and families to explain the goals of care, including clinical stability criteria, the importance of preventive measures (such as smoking cessation, avoidance of second-hand smoke, appropriate vaccinations, and modification of environmental exposures), and required follow-up care.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with asthma exacerbation.
Follow evidence-based recommendations for the treatment of patients with asthma exacerbations.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Contribute to and/or develop educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for asthma exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead, coordinate, and/or participate in efforts to educate staff on the importance of smoking cessation counseling and other preventive measures.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists and respiratory therapists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with asthma.
1. Centers for Disease Control and Prevention. CDC Vital Signs: Asthma in the US. Available at: http://www.cdc.gov/vitalsigns/asthma/. Accessed June 2015.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
Asthma is a chronic disease characterized by airway inflammation and reversible airflow limitation. It is one of the most common chronic conditions and it leads to marked morbidity and mortality in hospitalized patients. In the United States, 1 in 12 persons has asthma and nearly 50% of affected individuals experience an asthma exacerbation each year, accounting for 1.8 million emergency department visits.1,2 Annually, more than 400,000 hospital discharges occur with asthma as the primary diagnosis, with an average length of stay of 3.2 days.2Hospitalists are central to the provision of care for patients with asthma through the use of evidence-based approaches to manage acute exacerbations and to prevent their recurrence. Hospitalists should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to improve efficiency and quality of care and to reduce readmission rates and morbidity and mortality from asthma.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define asthma and describe the pathophysiologic processes that lead to reversible airway obstruction and inflammation.
Identify precipitants of asthma exacerbation, including environmental and occupational exposures.
Recognize the clinical presentation of asthma exacerbation and differentiate it from other acute respiratory and nonrespiratory syndromes.
Describe the role of diagnostic testing, including peak flow monitoring, used for evaluation of asthma exacerbation.
Recognize indications for specialty consultation, including pulmonary and allergy medicine.
Describe evidence-based therapies for the treatment of asthma exacerbations, which may include bronchodilators, systemic corticosteroids, and oxygen.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat asthma.
Recognize signs and symptoms of impending respiratory failure.
Explain the indications for invasive and noninvasive ventilatory support.
List the risk factors for disease severity and death from asthma.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify triggers of asthma and symptoms consistent with asthma exacerbation.
Perform a targeted physical examination to elicit signs consistent with asthma exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Select appropriate diagnostic studies to evaluate severity of asthma exacerbation and interpret the results.
Recognize indications for transfer to the intensive care unit, including impending respiratory failure, and coordinate intubation or noninvasive mechanical ventilation when indicated.
Prescribe appropriate evidence-based pharmacologic therapies during asthma exacerbation, recommending the most appropriate route, dose, frequency, and duration of treatment.
Communicate with patients and families to explain the natural history and prognosis of asthma.
Facilitate discharge planning early during hospitalization.
Develop an asthma action plan in preparation for discharge.
Educate patients and families regarding the indications and appropriate use of daily use inhalers and rescue inhalers for asthmatic control.
Ensure that patients receive training of proper inhaler and peak flow techniques before hospital discharge.
Communicate with patients and families to explain symptoms and signs that should prompt emergent medical attention.
Communicate with patients and families to explain the goals of care, including clinical stability criteria, the importance of preventive measures (such as smoking cessation, avoidance of second-hand smoke, appropriate vaccinations, and modification of environmental exposures), and required follow-up care.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with asthma exacerbation.
Follow evidence-based recommendations for the treatment of patients with asthma exacerbations.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Contribute to and/or develop educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for asthma exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead, coordinate, and/or participate in efforts to educate staff on the importance of smoking cessation counseling and other preventive measures.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists and respiratory therapists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with asthma.
Asthma is a chronic disease characterized by airway inflammation and reversible airflow limitation. It is one of the most common chronic conditions and it leads to marked morbidity and mortality in hospitalized patients. In the United States, 1 in 12 persons has asthma and nearly 50% of affected individuals experience an asthma exacerbation each year, accounting for 1.8 million emergency department visits.1,2 Annually, more than 400,000 hospital discharges occur with asthma as the primary diagnosis, with an average length of stay of 3.2 days.2Hospitalists are central to the provision of care for patients with asthma through the use of evidence-based approaches to manage acute exacerbations and to prevent their recurrence. Hospitalists should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to improve efficiency and quality of care and to reduce readmission rates and morbidity and mortality from asthma.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define asthma and describe the pathophysiologic processes that lead to reversible airway obstruction and inflammation.
Identify precipitants of asthma exacerbation, including environmental and occupational exposures.
Recognize the clinical presentation of asthma exacerbation and differentiate it from other acute respiratory and nonrespiratory syndromes.
Describe the role of diagnostic testing, including peak flow monitoring, used for evaluation of asthma exacerbation.
Recognize indications for specialty consultation, including pulmonary and allergy medicine.
Describe evidence-based therapies for the treatment of asthma exacerbations, which may include bronchodilators, systemic corticosteroids, and oxygen.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat asthma.
Recognize signs and symptoms of impending respiratory failure.
Explain the indications for invasive and noninvasive ventilatory support.
List the risk factors for disease severity and death from asthma.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify triggers of asthma and symptoms consistent with asthma exacerbation.
Perform a targeted physical examination to elicit signs consistent with asthma exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Select appropriate diagnostic studies to evaluate severity of asthma exacerbation and interpret the results.
Recognize indications for transfer to the intensive care unit, including impending respiratory failure, and coordinate intubation or noninvasive mechanical ventilation when indicated.
Prescribe appropriate evidence-based pharmacologic therapies during asthma exacerbation, recommending the most appropriate route, dose, frequency, and duration of treatment.
Communicate with patients and families to explain the natural history and prognosis of asthma.
Facilitate discharge planning early during hospitalization.
Develop an asthma action plan in preparation for discharge.
Educate patients and families regarding the indications and appropriate use of daily use inhalers and rescue inhalers for asthmatic control.
Ensure that patients receive training of proper inhaler and peak flow techniques before hospital discharge.
Communicate with patients and families to explain symptoms and signs that should prompt emergent medical attention.
Communicate with patients and families to explain the goals of care, including clinical stability criteria, the importance of preventive measures (such as smoking cessation, avoidance of second-hand smoke, appropriate vaccinations, and modification of environmental exposures), and required follow-up care.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with asthma exacerbation.
Follow evidence-based recommendations for the treatment of patients with asthma exacerbations.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Contribute to and/or develop educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for asthma exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead, coordinate, and/or participate in efforts to educate staff on the importance of smoking cessation counseling and other preventive measures.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists and respiratory therapists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with asthma.
1. Centers for Disease Control and Prevention. CDC Vital Signs: Asthma in the US. Available at: http://www.cdc.gov/vitalsigns/asthma/. Accessed June 2015.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
1. Centers for Disease Control and Prevention. CDC Vital Signs: Asthma in the US. Available at: http://www.cdc.gov/vitalsigns/asthma/. Accessed June 2015.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
© 2017 Society of Hospital Medicine
Cardiac Arrhythmia. 2017 Hospital Medicine Revised Core Competencies
Cardiac arrhythmias are a group of conditions characterized by an abnormal heart rate or rhythm. These are common and affect approximately 5% of the population in the United States. More than 250,000 Americans die each year of sudden cardiac arrest, and most cases are thought to be due to ventricular fibrillation or ventricular tachycardia.1 Several cardiac arrhythmias can cause instability, prompting hospitalization, or they may result from complications during hospitalization. Annually, more than 740,000 hospital discharges are associated with a primary diagnosis of cardiac arrhythmia.2 Hospitalists identify and treat all types of arrhythmias, coordinate specialty and primary care resources, and transition patients safely and cost-effectively through the acute hospitalization and into the outpatient setting.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Identify and differentiate the common clinical presentations of both benign and pathologic arrhythmias.
Explain the causes of atrial and ventricular arrhythmias.
Describe the indicated tests required to evaluate arrhythmias.
Explain how medications, metabolic abnormalities, and medical comorbidities may precipitate various arrhythmias.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat cardiac arrhythmias. Discuss the management options and goals for patients hospitalized with arrhythmias.
Describe the patient characteristics and comorbid conditions that predict outcomes in patients with arrhythmias.
Recognize indications for specialty consultation, which may include cardiology and cardiac electrophysiology.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
Recall appropriate indications for both initiation and discontinuation of continuous telemetry monitoring in the hospitalized patient.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, including medications, family history, and social history.
Perform a targeted physical examination with emphasis on identifying signs associated with hemodynamic instability, tissue perfusion, and occult cardiac and vascular disease.
Identify common benign and pathologic arrhythmias on electrocardiography, rhythm strips, and continuous telemetry monitoring.
Determine the appropriate level of care required based on risk stratification of patients with cardiac arrhythmias.
Identify and prioritize high-risk arrhythmias that require urgent intervention and implement emergency protocols as indicated.
Formulate patient-specific and evidence-based care plans incorporating diagnostic findings, prognosis, and patient characteristics.
Develop patient-specific care plans that may include rate-controlling interventions, cardioversion, defibrillation, or implantable medical devices.
Communicate with patients and families to explain the natural history and prognosis of cardiac arrhythmias.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain drug interactions for antiarrhythmic drugs and the importance of strict adherence to medication regimens and laboratory monitoring.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include primary care, cardiology, nursing, and social services, in the care of patients with cardiac arrhythmias that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of cardiac arrhythmias.
Acknowledge and ameliorate patient discomfort from uncontrolled arrhythmias and electrical cardioversion therapies.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop patient care guidelines and/or pathways on the basis of peer-reviewed outcomes research, patient and physician satisfaction, and cost.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, The Joint Commission, American Heart Association, American College of Cardiology, Agency for Healthcare Research and Quality).
Lead, coordinate, and/or participate in quality improvement initiatives to promote early identification of arrhythmias, reduce preventable complications, and promote appropriate use of telemetry resources.
Cardiac arrhythmias are a group of conditions characterized by an abnormal heart rate or rhythm. These are common and affect approximately 5% of the population in the United States. More than 250,000 Americans die each year of sudden cardiac arrest, and most cases are thought to be due to ventricular fibrillation or ventricular tachycardia.1 Several cardiac arrhythmias can cause instability, prompting hospitalization, or they may result from complications during hospitalization. Annually, more than 740,000 hospital discharges are associated with a primary diagnosis of cardiac arrhythmia.2 Hospitalists identify and treat all types of arrhythmias, coordinate specialty and primary care resources, and transition patients safely and cost-effectively through the acute hospitalization and into the outpatient setting.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Identify and differentiate the common clinical presentations of both benign and pathologic arrhythmias.
Explain the causes of atrial and ventricular arrhythmias.
Describe the indicated tests required to evaluate arrhythmias.
Explain how medications, metabolic abnormalities, and medical comorbidities may precipitate various arrhythmias.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat cardiac arrhythmias. Discuss the management options and goals for patients hospitalized with arrhythmias.
Describe the patient characteristics and comorbid conditions that predict outcomes in patients with arrhythmias.
Recognize indications for specialty consultation, which may include cardiology and cardiac electrophysiology.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
Recall appropriate indications for both initiation and discontinuation of continuous telemetry monitoring in the hospitalized patient.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, including medications, family history, and social history.
Perform a targeted physical examination with emphasis on identifying signs associated with hemodynamic instability, tissue perfusion, and occult cardiac and vascular disease.
Identify common benign and pathologic arrhythmias on electrocardiography, rhythm strips, and continuous telemetry monitoring.
Determine the appropriate level of care required based on risk stratification of patients with cardiac arrhythmias.
Identify and prioritize high-risk arrhythmias that require urgent intervention and implement emergency protocols as indicated.
Formulate patient-specific and evidence-based care plans incorporating diagnostic findings, prognosis, and patient characteristics.
Develop patient-specific care plans that may include rate-controlling interventions, cardioversion, defibrillation, or implantable medical devices.
Communicate with patients and families to explain the natural history and prognosis of cardiac arrhythmias.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain drug interactions for antiarrhythmic drugs and the importance of strict adherence to medication regimens and laboratory monitoring.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include primary care, cardiology, nursing, and social services, in the care of patients with cardiac arrhythmias that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of cardiac arrhythmias.
Acknowledge and ameliorate patient discomfort from uncontrolled arrhythmias and electrical cardioversion therapies.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop patient care guidelines and/or pathways on the basis of peer-reviewed outcomes research, patient and physician satisfaction, and cost.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, The Joint Commission, American Heart Association, American College of Cardiology, Agency for Healthcare Research and Quality).
Lead, coordinate, and/or participate in quality improvement initiatives to promote early identification of arrhythmias, reduce preventable complications, and promote appropriate use of telemetry resources.
Cardiac arrhythmias are a group of conditions characterized by an abnormal heart rate or rhythm. These are common and affect approximately 5% of the population in the United States. More than 250,000 Americans die each year of sudden cardiac arrest, and most cases are thought to be due to ventricular fibrillation or ventricular tachycardia.1 Several cardiac arrhythmias can cause instability, prompting hospitalization, or they may result from complications during hospitalization. Annually, more than 740,000 hospital discharges are associated with a primary diagnosis of cardiac arrhythmia.2 Hospitalists identify and treat all types of arrhythmias, coordinate specialty and primary care resources, and transition patients safely and cost-effectively through the acute hospitalization and into the outpatient setting.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Identify and differentiate the common clinical presentations of both benign and pathologic arrhythmias.
Explain the causes of atrial and ventricular arrhythmias.
Describe the indicated tests required to evaluate arrhythmias.
Explain how medications, metabolic abnormalities, and medical comorbidities may precipitate various arrhythmias.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat cardiac arrhythmias. Discuss the management options and goals for patients hospitalized with arrhythmias.
Describe the patient characteristics and comorbid conditions that predict outcomes in patients with arrhythmias.
Recognize indications for specialty consultation, which may include cardiology and cardiac electrophysiology.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
Recall appropriate indications for both initiation and discontinuation of continuous telemetry monitoring in the hospitalized patient.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history, including medications, family history, and social history.
Perform a targeted physical examination with emphasis on identifying signs associated with hemodynamic instability, tissue perfusion, and occult cardiac and vascular disease.
Identify common benign and pathologic arrhythmias on electrocardiography, rhythm strips, and continuous telemetry monitoring.
Determine the appropriate level of care required based on risk stratification of patients with cardiac arrhythmias.
Identify and prioritize high-risk arrhythmias that require urgent intervention and implement emergency protocols as indicated.
Formulate patient-specific and evidence-based care plans incorporating diagnostic findings, prognosis, and patient characteristics.
Develop patient-specific care plans that may include rate-controlling interventions, cardioversion, defibrillation, or implantable medical devices.
Communicate with patients and families to explain the natural history and prognosis of cardiac arrhythmias.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain drug interactions for antiarrhythmic drugs and the importance of strict adherence to medication regimens and laboratory monitoring.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include primary care, cardiology, nursing, and social services, in the care of patients with cardiac arrhythmias that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of cardiac arrhythmias.
Acknowledge and ameliorate patient discomfort from uncontrolled arrhythmias and electrical cardioversion therapies.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop patient care guidelines and/or pathways on the basis of peer-reviewed outcomes research, patient and physician satisfaction, and cost.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, The Joint Commission, American Heart Association, American College of Cardiology, Agency for Healthcare Research and Quality).
Lead, coordinate, and/or participate in quality improvement initiatives to promote early identification of arrhythmias, reduce preventable complications, and promote appropriate use of telemetry resources.
© 2017 Society of Hospital Medicine
Chronic Obstructive Pulmonary Disease. 2017 Hospital Medicine Revised Core Competencies
Chronic obstructive pulmonary disease (COPD) is a heterogeneous group of respiratory conditions, predominantly composed of chronic bronchitis and emphysema. COPD is defined by airflow limitation that is not completely reversible, and it is associated with an abnormal airway inflammatory response. Exposure to tobacco smoke is the main risk factor. COPD affects more than 12 million Americans and is the third leading cause of death in the United States. A COPD exacerbation is defined as an increase in the usual symptoms of COPD that is beyond day-to-day variations and leads to a change in medication and often results in hospitalization. Annually, more than 670,000 hospital discharges occur with COPD as the primary diagnosis, and nearly 1 of every 5 hospitalized patients 40 years or older has COPD.1,2The average length of stay is 4.3 days.1 COPD is a substantial cause of disability and carries a large economic burden, accounting for almost $17 billion of total hospital charges billed to Medicare each year.3 The early detection and prompt treatment of exacerbations are essential to ensure optimal outcomes and to reduce the burden of COPD. Hospitalists use evidence-based approaches to optimize care, and they should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to reduce readmission rates and mortality from COPD exacerbations.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define COPD and describe the pathophysiologic processes that lead to small airway obstruction and alveolar destruction.
Describe potential precipitants of exacerbation, including both infectious and noninfectious etiologies.
Differentiate the clinical presentation of a COPD exacerbation from asthma, heart failure, and other acute respiratory and nonrespiratory syndromes.
List the indicators of disease severity.
Describe the role of diagnostic testing used for the evaluation of COPD.
Describe the role of pulmonary function tests in the treatment of a COPD exacerbation.
Distinguish the medical management of patients with COPD exacerbations from that of patients with stable COPD.
Recognize indications for specialty consultation, which may include pulmonary medicine.
Describe the evidence-based therapies for treatment of COPD exacerbations, which may include bronchodilators, systemic corticosteroids, oxygen, and antibiotics.
Identify the potential risks of supplemental oxygen therapy, including development of hypercarbia in patients with chronic respiratory acidosis.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat COPD.
Describe and differentiate the means of ventilatory support, including the use of noninvasive positive pressure ventilation in COPD exacerbation.
Recognize anxiety and depression as important comorbid conditions that negatively affect outcomes.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with a COPD exacerbation and etiologic precipitants.
Perform a targeted physical examination to elicit signs consistent with a COPD exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Diagnose a COPD exacerbation on the basis of history, physical examination, and radiographic data.
Select and interpret appropriate diagnostic studies to evaluate the severity of a COPD exacerbation.
Recognize symptoms, signs, and severity of impending respiratory failure and select the indicated evidence-based ventilatory approach.
Select patients with COPD exacerbation who would benefit from use of positive pressure ventilation and identify those in whom this intervention is contraindicated.
Prescribe appropriate evidence-based pharmacologic therapies during COPD exacerbation, recommending the most appropriate drug route, dose, frequency, and duration of treatment.
Address treatment preferences, including advance directives early during hospital stay; implement end-of-life decisions by patients and/or families when indicated or desired.
Evaluate COPD in perioperative risk assessment, recommend measures to optimize perioperative management of COPD, and manage postoperative complications related to underlying COPD.
Identify patients with COPD who may benefit from pulmonary rehabilitation.
Communicate with patients and families to explain the natural history and prognosis of COPD.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Ensure that patients receive training on proper inhaler techniques and use before hospital discharge.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with a COPD exacerbation, beginning at admission and continuing through all care transitions.
Engage in a collaborative way with primary care physicians and emergency physicians in making admission decisions.
Promote and encourage preventive strategies, including smoking cessation, vaccinations, and venous thromboembolism prophylaxis.
Establish and maintain an open dialogue with patients and/or families regarding goals and limitations of care, including palliative care and end-of-life wishes.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with COPD.
Lead, coordinate, and/or participate in the development of educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for COPD exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead efforts to educate patients and staff on the importance of smoking cessation and other preventive measures.
1. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
2. Wier LM, Elizhauser A, Pfuntner A, Au DH. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Overview of Hospitalizations Among Patients With COPD, 2008. Statistical Brief #106. Rockville, MD; Agency for Health Care Policy and Research (US). 2011. Available at: http://www.ncbi.nlm.nih.gov/books/NBK53969/. Accessed June 2015.
3. Agency for Healthcare Research and Quality. Chronic obstructive pulmonary disease (COPD): hospital 30-day, all-cause, risk-standardized mortality rate following acute exacerbation of COPD. Available at http://www.qualitymeasures.ahrq.gov/content.aspx?id=48198. Accessed June 2015.
Chronic obstructive pulmonary disease (COPD) is a heterogeneous group of respiratory conditions, predominantly composed of chronic bronchitis and emphysema. COPD is defined by airflow limitation that is not completely reversible, and it is associated with an abnormal airway inflammatory response. Exposure to tobacco smoke is the main risk factor. COPD affects more than 12 million Americans and is the third leading cause of death in the United States. A COPD exacerbation is defined as an increase in the usual symptoms of COPD that is beyond day-to-day variations and leads to a change in medication and often results in hospitalization. Annually, more than 670,000 hospital discharges occur with COPD as the primary diagnosis, and nearly 1 of every 5 hospitalized patients 40 years or older has COPD.1,2The average length of stay is 4.3 days.1 COPD is a substantial cause of disability and carries a large economic burden, accounting for almost $17 billion of total hospital charges billed to Medicare each year.3 The early detection and prompt treatment of exacerbations are essential to ensure optimal outcomes and to reduce the burden of COPD. Hospitalists use evidence-based approaches to optimize care, and they should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to reduce readmission rates and mortality from COPD exacerbations.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define COPD and describe the pathophysiologic processes that lead to small airway obstruction and alveolar destruction.
Describe potential precipitants of exacerbation, including both infectious and noninfectious etiologies.
Differentiate the clinical presentation of a COPD exacerbation from asthma, heart failure, and other acute respiratory and nonrespiratory syndromes.
List the indicators of disease severity.
Describe the role of diagnostic testing used for the evaluation of COPD.
Describe the role of pulmonary function tests in the treatment of a COPD exacerbation.
Distinguish the medical management of patients with COPD exacerbations from that of patients with stable COPD.
Recognize indications for specialty consultation, which may include pulmonary medicine.
Describe the evidence-based therapies for treatment of COPD exacerbations, which may include bronchodilators, systemic corticosteroids, oxygen, and antibiotics.
Identify the potential risks of supplemental oxygen therapy, including development of hypercarbia in patients with chronic respiratory acidosis.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat COPD.
Describe and differentiate the means of ventilatory support, including the use of noninvasive positive pressure ventilation in COPD exacerbation.
Recognize anxiety and depression as important comorbid conditions that negatively affect outcomes.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with a COPD exacerbation and etiologic precipitants.
Perform a targeted physical examination to elicit signs consistent with a COPD exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Diagnose a COPD exacerbation on the basis of history, physical examination, and radiographic data.
Select and interpret appropriate diagnostic studies to evaluate the severity of a COPD exacerbation.
Recognize symptoms, signs, and severity of impending respiratory failure and select the indicated evidence-based ventilatory approach.
Select patients with COPD exacerbation who would benefit from use of positive pressure ventilation and identify those in whom this intervention is contraindicated.
Prescribe appropriate evidence-based pharmacologic therapies during COPD exacerbation, recommending the most appropriate drug route, dose, frequency, and duration of treatment.
Address treatment preferences, including advance directives early during hospital stay; implement end-of-life decisions by patients and/or families when indicated or desired.
Evaluate COPD in perioperative risk assessment, recommend measures to optimize perioperative management of COPD, and manage postoperative complications related to underlying COPD.
Identify patients with COPD who may benefit from pulmonary rehabilitation.
Communicate with patients and families to explain the natural history and prognosis of COPD.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Ensure that patients receive training on proper inhaler techniques and use before hospital discharge.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with a COPD exacerbation, beginning at admission and continuing through all care transitions.
Engage in a collaborative way with primary care physicians and emergency physicians in making admission decisions.
Promote and encourage preventive strategies, including smoking cessation, vaccinations, and venous thromboembolism prophylaxis.
Establish and maintain an open dialogue with patients and/or families regarding goals and limitations of care, including palliative care and end-of-life wishes.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with COPD.
Lead, coordinate, and/or participate in the development of educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for COPD exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead efforts to educate patients and staff on the importance of smoking cessation and other preventive measures.
Chronic obstructive pulmonary disease (COPD) is a heterogeneous group of respiratory conditions, predominantly composed of chronic bronchitis and emphysema. COPD is defined by airflow limitation that is not completely reversible, and it is associated with an abnormal airway inflammatory response. Exposure to tobacco smoke is the main risk factor. COPD affects more than 12 million Americans and is the third leading cause of death in the United States. A COPD exacerbation is defined as an increase in the usual symptoms of COPD that is beyond day-to-day variations and leads to a change in medication and often results in hospitalization. Annually, more than 670,000 hospital discharges occur with COPD as the primary diagnosis, and nearly 1 of every 5 hospitalized patients 40 years or older has COPD.1,2The average length of stay is 4.3 days.1 COPD is a substantial cause of disability and carries a large economic burden, accounting for almost $17 billion of total hospital charges billed to Medicare each year.3 The early detection and prompt treatment of exacerbations are essential to ensure optimal outcomes and to reduce the burden of COPD. Hospitalists use evidence-based approaches to optimize care, and they should strive to lead multidisciplinary teams to develop institutional guidelines and/or care pathways to reduce readmission rates and mortality from COPD exacerbations.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define COPD and describe the pathophysiologic processes that lead to small airway obstruction and alveolar destruction.
Describe potential precipitants of exacerbation, including both infectious and noninfectious etiologies.
Differentiate the clinical presentation of a COPD exacerbation from asthma, heart failure, and other acute respiratory and nonrespiratory syndromes.
List the indicators of disease severity.
Describe the role of diagnostic testing used for the evaluation of COPD.
Describe the role of pulmonary function tests in the treatment of a COPD exacerbation.
Distinguish the medical management of patients with COPD exacerbations from that of patients with stable COPD.
Recognize indications for specialty consultation, which may include pulmonary medicine.
Describe the evidence-based therapies for treatment of COPD exacerbations, which may include bronchodilators, systemic corticosteroids, oxygen, and antibiotics.
Identify the potential risks of supplemental oxygen therapy, including development of hypercarbia in patients with chronic respiratory acidosis.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat COPD.
Describe and differentiate the means of ventilatory support, including the use of noninvasive positive pressure ventilation in COPD exacerbation.
Recognize anxiety and depression as important comorbid conditions that negatively affect outcomes.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with a COPD exacerbation and etiologic precipitants.
Perform a targeted physical examination to elicit signs consistent with a COPD exacerbation, differentiate findings from those of other mimicking conditions, and assess illness severity.
Diagnose a COPD exacerbation on the basis of history, physical examination, and radiographic data.
Select and interpret appropriate diagnostic studies to evaluate the severity of a COPD exacerbation.
Recognize symptoms, signs, and severity of impending respiratory failure and select the indicated evidence-based ventilatory approach.
Select patients with COPD exacerbation who would benefit from use of positive pressure ventilation and identify those in whom this intervention is contraindicated.
Prescribe appropriate evidence-based pharmacologic therapies during COPD exacerbation, recommending the most appropriate drug route, dose, frequency, and duration of treatment.
Address treatment preferences, including advance directives early during hospital stay; implement end-of-life decisions by patients and/or families when indicated or desired.
Evaluate COPD in perioperative risk assessment, recommend measures to optimize perioperative management of COPD, and manage postoperative complications related to underlying COPD.
Identify patients with COPD who may benefit from pulmonary rehabilitation.
Communicate with patients and families to explain the natural history and prognosis of COPD.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain discharge medications, potential adverse effects, duration of therapy and dosing, and taper schedule.
Ensure that patients receive training on proper inhaler techniques and use before hospital discharge.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
Provide and coordinate resources to ensure safe transition from the hospital to arranged follow-up care.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include pulmonary medicine, respiratory therapy, nursing, and social services, in the care of patients with a COPD exacerbation, beginning at admission and continuing through all care transitions.
Engage in a collaborative way with primary care physicians and emergency physicians in making admission decisions.
Promote and encourage preventive strategies, including smoking cessation, vaccinations, and venous thromboembolism prophylaxis.
Establish and maintain an open dialogue with patients and/or families regarding goals and limitations of care, including palliative care and end-of-life wishes.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with pulmonologists, to promote patient safety and optimize cost-effective diagnostic and management strategies for patients with COPD.
Lead, coordinate, and/or participate in the development of educational modules, order sets, and/or pathways that facilitate use of evidence-based strategies for COPD exacerbation in the emergency department and the hospital, with goals of improving outcomes, decreasing length of stay, and reducing rehospitalization rates.
Lead efforts to educate patients and staff on the importance of smoking cessation and other preventive measures.
1. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
2. Wier LM, Elizhauser A, Pfuntner A, Au DH. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Overview of Hospitalizations Among Patients With COPD, 2008. Statistical Brief #106. Rockville, MD; Agency for Health Care Policy and Research (US). 2011. Available at: http://www.ncbi.nlm.nih.gov/books/NBK53969/. Accessed June 2015.
3. Agency for Healthcare Research and Quality. Chronic obstructive pulmonary disease (COPD): hospital 30-day, all-cause, risk-standardized mortality rate following acute exacerbation of COPD. Available at http://www.qualitymeasures.ahrq.gov/content.aspx?id=48198. Accessed June 2015.
1. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed June 2015.
2. Wier LM, Elizhauser A, Pfuntner A, Au DH. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Overview of Hospitalizations Among Patients With COPD, 2008. Statistical Brief #106. Rockville, MD; Agency for Health Care Policy and Research (US). 2011. Available at: http://www.ncbi.nlm.nih.gov/books/NBK53969/. Accessed June 2015.
3. Agency for Healthcare Research and Quality. Chronic obstructive pulmonary disease (COPD): hospital 30-day, all-cause, risk-standardized mortality rate following acute exacerbation of COPD. Available at http://www.qualitymeasures.ahrq.gov/content.aspx?id=48198. Accessed June 2015.
© 2017 Society of Hospital Medicine
Community-Acquired Pneumonia. 2017 Hospital Medicine Revised Core Competencies
Community-acquired pneumonia (CAP) is an infection of the lung parenchyma that occurs in the community or is diagnosed within 48 hours of hospital admission. CAP is a common and potentially life-threatening infection, and it is a leading cause of death from infectious diseases. Approximately 25% of persons with CAP require hospitalization, and 10% to 20% of these patients require admission to the intensive care unit.1-3 The mortality rate ranges from about 13% in hospitalized patients to 36% in patients admitted to the intensive care unit.1-3 CAP is a curable condition and an organized approach to management is likely to improve clinical results and reduce mortality. Pneumonia outcome measures are used to evaluate performance of healthcare providers and organizations. Hospitalists apply evidence-based guidelines to the management of patients hospitalized with pneumonia and lead initiatives to improve quality of care and reduce practice variability.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define CAP, list the likely etiologies and the signs and symptoms, and distinguish CAP from hospital-acquired pneumonia and healthcare-associated pneumonia.
Describe other causes of pulmonary infiltrates on radiographic studies.
Describe the tests indicated to evaluate and treat CAP.
Explain indications for respiratory isolation.
Identify patients with comorbidities (such as immunocompromise, diabetes mellitus, and extremes of age) who are at high risk of a complicated course.
Identify specific pathogens that predispose patients to a complicated course.
Recognize indications for specialty consultation.
Describe indicated therapeutic modalities for CAP, including oxygen therapy, respiratory care modalities, appropriate antimicrobial selection and duration, and other evidence-based treatments.
Predict patient risk for morbidity and mortality from CAP using a validated risk score.
Explain goals for hospital discharge, including evidence-based measures of clinical stability for safe care transition.
Describe factors associated with a nonresponding pneumonia.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with CAP and demographic factors that may predispose patients to CAP.
Perform a targeted physical examination to elicit signs consistent with CAP and differentiate it from other mimicking conditions.
Order and interpret laboratory, microbiologic, and radiologic studies to confirm the diagnosis of CAP and risk stratify patients.
Apply evidence-based tools (such as the Pneumonia Severity Index) to triage decisions and identify factors that support the need for intensive care unit admission.
Initiate empiric antimicrobials for CAP on the basis of illness severity and evidence-based national guidelines, incorporating local resistance patterns.
Formulate a subsequent treatment plan that includes narrowing antimicrobial therapies on the basis of available culture data and patient response to treatment.
Recognize the criteria for clinical stability, including the appropriate deescalation of treatment such as transitioning from parenteral to oral antimicrobials.
Recognize and address complications of CAP and/or inadequate response to therapy, including respiratory failure and parapneumonic effusions.
Communicate with patients and families to explain the pathophysiology and prognosis of CAP.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain the use and potential adverse effects of pharmacologic agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures such as smoking cessation), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Recognize and address barriers to follow-up care and anticipated postdischarge requirements.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, respiratory therapy, nutrition, and pharmacy services, to the care of patients with CAP through all care transitions.
Follow evidence-based recommendations for the treatment of patients with CAP.
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with infectious disease and pulmonary specialists, to promote patient safety and cost-effective diagnostic and management strategies for patients with CAP.
Lead, coordinate, and/or participate in efforts to identify, address, and monitor quality indicators for CAP.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, Centers for Medicare & Medicaid Services, Infectious Diseases Society of America, American Thoracic Society).
Integrate evidence-based clinical severity scores and clinical judgment into admission decisions.
Lead efforts to educate staff on the importance of smoking cessation counseling, vaccinations, and other preventive measures.
1. File TM Jr, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;122(2):130-141.
2. Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996;275(2):134.
3. Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, et al; American Thoracic Society. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163(7):1730-1754.
Community-acquired pneumonia (CAP) is an infection of the lung parenchyma that occurs in the community or is diagnosed within 48 hours of hospital admission. CAP is a common and potentially life-threatening infection, and it is a leading cause of death from infectious diseases. Approximately 25% of persons with CAP require hospitalization, and 10% to 20% of these patients require admission to the intensive care unit.1-3 The mortality rate ranges from about 13% in hospitalized patients to 36% in patients admitted to the intensive care unit.1-3 CAP is a curable condition and an organized approach to management is likely to improve clinical results and reduce mortality. Pneumonia outcome measures are used to evaluate performance of healthcare providers and organizations. Hospitalists apply evidence-based guidelines to the management of patients hospitalized with pneumonia and lead initiatives to improve quality of care and reduce practice variability.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define CAP, list the likely etiologies and the signs and symptoms, and distinguish CAP from hospital-acquired pneumonia and healthcare-associated pneumonia.
Describe other causes of pulmonary infiltrates on radiographic studies.
Describe the tests indicated to evaluate and treat CAP.
Explain indications for respiratory isolation.
Identify patients with comorbidities (such as immunocompromise, diabetes mellitus, and extremes of age) who are at high risk of a complicated course.
Identify specific pathogens that predispose patients to a complicated course.
Recognize indications for specialty consultation.
Describe indicated therapeutic modalities for CAP, including oxygen therapy, respiratory care modalities, appropriate antimicrobial selection and duration, and other evidence-based treatments.
Predict patient risk for morbidity and mortality from CAP using a validated risk score.
Explain goals for hospital discharge, including evidence-based measures of clinical stability for safe care transition.
Describe factors associated with a nonresponding pneumonia.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with CAP and demographic factors that may predispose patients to CAP.
Perform a targeted physical examination to elicit signs consistent with CAP and differentiate it from other mimicking conditions.
Order and interpret laboratory, microbiologic, and radiologic studies to confirm the diagnosis of CAP and risk stratify patients.
Apply evidence-based tools (such as the Pneumonia Severity Index) to triage decisions and identify factors that support the need for intensive care unit admission.
Initiate empiric antimicrobials for CAP on the basis of illness severity and evidence-based national guidelines, incorporating local resistance patterns.
Formulate a subsequent treatment plan that includes narrowing antimicrobial therapies on the basis of available culture data and patient response to treatment.
Recognize the criteria for clinical stability, including the appropriate deescalation of treatment such as transitioning from parenteral to oral antimicrobials.
Recognize and address complications of CAP and/or inadequate response to therapy, including respiratory failure and parapneumonic effusions.
Communicate with patients and families to explain the pathophysiology and prognosis of CAP.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain the use and potential adverse effects of pharmacologic agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures such as smoking cessation), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Recognize and address barriers to follow-up care and anticipated postdischarge requirements.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, respiratory therapy, nutrition, and pharmacy services, to the care of patients with CAP through all care transitions.
Follow evidence-based recommendations for the treatment of patients with CAP.
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with infectious disease and pulmonary specialists, to promote patient safety and cost-effective diagnostic and management strategies for patients with CAP.
Lead, coordinate, and/or participate in efforts to identify, address, and monitor quality indicators for CAP.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, Centers for Medicare & Medicaid Services, Infectious Diseases Society of America, American Thoracic Society).
Integrate evidence-based clinical severity scores and clinical judgment into admission decisions.
Lead efforts to educate staff on the importance of smoking cessation counseling, vaccinations, and other preventive measures.
Community-acquired pneumonia (CAP) is an infection of the lung parenchyma that occurs in the community or is diagnosed within 48 hours of hospital admission. CAP is a common and potentially life-threatening infection, and it is a leading cause of death from infectious diseases. Approximately 25% of persons with CAP require hospitalization, and 10% to 20% of these patients require admission to the intensive care unit.1-3 The mortality rate ranges from about 13% in hospitalized patients to 36% in patients admitted to the intensive care unit.1-3 CAP is a curable condition and an organized approach to management is likely to improve clinical results and reduce mortality. Pneumonia outcome measures are used to evaluate performance of healthcare providers and organizations. Hospitalists apply evidence-based guidelines to the management of patients hospitalized with pneumonia and lead initiatives to improve quality of care and reduce practice variability.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define CAP, list the likely etiologies and the signs and symptoms, and distinguish CAP from hospital-acquired pneumonia and healthcare-associated pneumonia.
Describe other causes of pulmonary infiltrates on radiographic studies.
Describe the tests indicated to evaluate and treat CAP.
Explain indications for respiratory isolation.
Identify patients with comorbidities (such as immunocompromise, diabetes mellitus, and extremes of age) who are at high risk of a complicated course.
Identify specific pathogens that predispose patients to a complicated course.
Recognize indications for specialty consultation.
Describe indicated therapeutic modalities for CAP, including oxygen therapy, respiratory care modalities, appropriate antimicrobial selection and duration, and other evidence-based treatments.
Predict patient risk for morbidity and mortality from CAP using a validated risk score.
Explain goals for hospital discharge, including evidence-based measures of clinical stability for safe care transition.
Describe factors associated with a nonresponding pneumonia.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history to identify symptoms consistent with CAP and demographic factors that may predispose patients to CAP.
Perform a targeted physical examination to elicit signs consistent with CAP and differentiate it from other mimicking conditions.
Order and interpret laboratory, microbiologic, and radiologic studies to confirm the diagnosis of CAP and risk stratify patients.
Apply evidence-based tools (such as the Pneumonia Severity Index) to triage decisions and identify factors that support the need for intensive care unit admission.
Initiate empiric antimicrobials for CAP on the basis of illness severity and evidence-based national guidelines, incorporating local resistance patterns.
Formulate a subsequent treatment plan that includes narrowing antimicrobial therapies on the basis of available culture data and patient response to treatment.
Recognize the criteria for clinical stability, including the appropriate deescalation of treatment such as transitioning from parenteral to oral antimicrobials.
Recognize and address complications of CAP and/or inadequate response to therapy, including respiratory failure and parapneumonic effusions.
Communicate with patients and families to explain the pathophysiology and prognosis of CAP.
Communicate with patients and families to explain tests and procedures and their indications and to obtain informed consent.
Communicate with patients and families to explain the use and potential adverse effects of pharmacologic agents.
Facilitate discharge planning early during hospitalization.
Communicate with patients and families to explain the goals of care (including clinical stability criteria, the importance of preventive measures such as smoking cessation), discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Recognize and address barriers to follow-up care and anticipated postdischarge requirements.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, respiratory therapy, nutrition, and pharmacy services, to the care of patients with CAP through all care transitions.
Follow evidence-based recommendations for the treatment of patients with CAP.
Work collaboratively with primary care physicians and emergency physicians in making admission decisions.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaborative efforts with infectious disease and pulmonary specialists, to promote patient safety and cost-effective diagnostic and management strategies for patients with CAP.
Lead, coordinate, and/or participate in efforts to identify, address, and monitor quality indicators for CAP.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations (eg, Centers for Medicare & Medicaid Services, Infectious Diseases Society of America, American Thoracic Society).
Integrate evidence-based clinical severity scores and clinical judgment into admission decisions.
Lead efforts to educate staff on the importance of smoking cessation counseling, vaccinations, and other preventive measures.
1. File TM Jr, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;122(2):130-141.
2. Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996;275(2):134.
3. Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, et al; American Thoracic Society. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163(7):1730-1754.
1. File TM Jr, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;122(2):130-141.
2. Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA. 1996;275(2):134.
3. Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, et al; American Thoracic Society. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163(7):1730-1754.
© 2017 Society of Hospital Medicine
Delirium and Dementia. 2017 Hospital Medicine Revised Core Competencies
DELIRIUM
Delirium is defined as an acute, transient, global disorder of cognition. In two-thirds of cases, delirium occurs in patients with baseline vulnerability, including those with underlying dementia.1 Although up to 30% of older medical patients experience delirium during hospitalization, this condition is unrecognized in nearly two-thirds of cases.2-4 Patients with delirium experience an average increase in length of hospital stay of 8 days and mortality rates that are twice as high as those of patients without delirium.5,6 In addition, delirium is associated with high rates of functional and cognitive decline and skilled nursing facility placement after hospitalization. The cost of caring for patients with delirium has a marked impact on individual patients, families, and hospital systems. Hospitalists lead their institutions in the development of screening and prevention protocols for patients at risk for delirium, as well as in the promotion of safe treatment approaches. Hospitalists also develop strategies to operationalize cost-effective delirium prevention programs that improve outcomes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
DELIRIUM KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate delirium from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate delirium.
Describe the causes of delirium in the hospital setting including environmental and iatrogenic risk factors.
Identify medications known to precipitate delirium.
Recognize the indications for specialty consultations.
Describe methods for the prevention of delirium.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat delirium.
Describe nonpharmacologic therapies to manage delirium.
Describe the complications of delirium in the hospitalized patient.
Discuss the multifaceted impact that delirium has on patients and their families.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
DELIRIUM SKILLS
Hospitalists should be able to:
Predict a patient’s risk for the development of delirium on the basis of initial history and physical examination.
Perform appropriate screening for delirium.
Develop active strategies to reduce delirium in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected delirium in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Perform a focused evaluation for the underlying etiology of delirium and institute prompt treatment to lessen its severity.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with delirium.
Lead multidisciplinary teams to develop and implement care plans for patients with delirium.
Develop an appropriate pharmacologic plan to manage delirium.
Develop an appropriate nonpharmacologic plan to manage delirium.
Develop an appropriate management plan for patients with delirium in the postoperative setting.
Document an appropriate treatment plan to reduce mortality, limit the duration of delirium and the time required to control agitation, maintain adequate control of delirium, address complications, and manage cost of treatment.
Use a patient- and family-centered approach in the care of older inpatients.
Establish goals and boundaries of care with patients and their families.
Communicate with patients and families to explain the history and prognosis of delirium.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DELIRIUM ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with delirium that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of delirium and its causes.
Value a patient- and family-centered approach in the care of older inpatients.
DELIRIUM SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for delirium.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration with geriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with delirium.
DEMENTIA
Dementia is defined as a chronic, often progressive, decline in cognitive function, eventually limiting daily activities. Dementia is a common comorbidity in the hospitalized older patient. Alzheimer disease is the most prevalent form of dementia in older patients, and it accounts for up to 80% of cases.7,8 More than 5 million persons older than 65 years have Alzheimer disease in the United States.7,8 Patients with dementia are at increased risk for delirium, falls, and functional decline during hospitalization. Patients with baseline cognitive impairment have prolonged lengths of stay and complex needs after discharge. Agitation and behavioral symptoms of dementia can be exacerbated in the hospital setting and are often difficult to manage. Care of the patient with dementia requires that hospitalists engage in a multidisciplinary approach to inpatient and transitional care. Hospitalists may also become involved in hospital quality and safety initiatives that pertain to areas such as restraint use and fall prevention.
DEMENTIA KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate dementia from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate dementia.
Describe the causes of potentially reversible dementias or dementia-like conditions.
List indications, contraindications, and mechanisms of action of pharmacologic agents used to treat dementia.
Describe nonpharmacologic therapies to manage dementia symptoms.
Recognize the indications for specialty consultations.
Describe the complications of dementia in the hospitalized patient.
Discuss the multifaceted impact that dementia has on patients and their families.
Explain goals for hospital discharge including specific measures of clinical stability for safe care transition.
DEMENTIA SKILLS
Hospitalists should be able to:
Perform appropriate screening for dementia.
Develop active strategies to reduce development of delirium in patients with dementia in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected dementia in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Assess patients for potentially reversible causes of dementia or dementia-like conditions. Assess severity of cognitive impairment and perform a focused evaluation for the underlying etiology of dementia when appropriate.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with dementia.
Formulate and lead multidisciplinary teams to develop and implement care plans for patients with dementia.
Develop an appropriate pharmacologic plan to manage dementia.
Develop an appropriate nonpharmacologic plan to manage dementia.
Use a patient- and family-centered approach in the care of older inpatients.
Communicate with patients and families to explain the history and prognosis of dementia.
Use evidence-based methods and tools to assess patients’ medical decision-making capacity.
Defend patients’ right to autonomy when so qualified.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DEMENTIA ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with dementia that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of dementia and its causes.
Value a patient- and family-centered approach to educate and engage families and caregivers in the care of older inpatients.
Responsibly address and respect end-of-life care wishes for patients with advanced dementia.
DEMENTIA SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for poor outcomes related to dementia.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration withgeriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with dementia.
1. Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7-21.
2. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97(3):278-288.
3. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242.
4. Francis J. Delirium in older patients. J Am Geriatr Soc. 1992;40(8):829-838.
5. Cole MG, Primeau FJ. Prognosis of delirium in elderly hospital patients. CMAJ. 1993;149(1):41.
6. McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162(4):457-463.
7. Alzheimer’s Association. 2014 Alzheimer’s disease facts and figures. Available at: https://www.alz.org/downloads/Facts_Figures_2014.pdf. Accessed July 2015.
8. Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-1122.
DELIRIUM
Delirium is defined as an acute, transient, global disorder of cognition. In two-thirds of cases, delirium occurs in patients with baseline vulnerability, including those with underlying dementia.1 Although up to 30% of older medical patients experience delirium during hospitalization, this condition is unrecognized in nearly two-thirds of cases.2-4 Patients with delirium experience an average increase in length of hospital stay of 8 days and mortality rates that are twice as high as those of patients without delirium.5,6 In addition, delirium is associated with high rates of functional and cognitive decline and skilled nursing facility placement after hospitalization. The cost of caring for patients with delirium has a marked impact on individual patients, families, and hospital systems. Hospitalists lead their institutions in the development of screening and prevention protocols for patients at risk for delirium, as well as in the promotion of safe treatment approaches. Hospitalists also develop strategies to operationalize cost-effective delirium prevention programs that improve outcomes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
DELIRIUM KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate delirium from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate delirium.
Describe the causes of delirium in the hospital setting including environmental and iatrogenic risk factors.
Identify medications known to precipitate delirium.
Recognize the indications for specialty consultations.
Describe methods for the prevention of delirium.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat delirium.
Describe nonpharmacologic therapies to manage delirium.
Describe the complications of delirium in the hospitalized patient.
Discuss the multifaceted impact that delirium has on patients and their families.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
DELIRIUM SKILLS
Hospitalists should be able to:
Predict a patient’s risk for the development of delirium on the basis of initial history and physical examination.
Perform appropriate screening for delirium.
Develop active strategies to reduce delirium in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected delirium in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Perform a focused evaluation for the underlying etiology of delirium and institute prompt treatment to lessen its severity.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with delirium.
Lead multidisciplinary teams to develop and implement care plans for patients with delirium.
Develop an appropriate pharmacologic plan to manage delirium.
Develop an appropriate nonpharmacologic plan to manage delirium.
Develop an appropriate management plan for patients with delirium in the postoperative setting.
Document an appropriate treatment plan to reduce mortality, limit the duration of delirium and the time required to control agitation, maintain adequate control of delirium, address complications, and manage cost of treatment.
Use a patient- and family-centered approach in the care of older inpatients.
Establish goals and boundaries of care with patients and their families.
Communicate with patients and families to explain the history and prognosis of delirium.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DELIRIUM ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with delirium that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of delirium and its causes.
Value a patient- and family-centered approach in the care of older inpatients.
DELIRIUM SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for delirium.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration with geriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with delirium.
DEMENTIA
Dementia is defined as a chronic, often progressive, decline in cognitive function, eventually limiting daily activities. Dementia is a common comorbidity in the hospitalized older patient. Alzheimer disease is the most prevalent form of dementia in older patients, and it accounts for up to 80% of cases.7,8 More than 5 million persons older than 65 years have Alzheimer disease in the United States.7,8 Patients with dementia are at increased risk for delirium, falls, and functional decline during hospitalization. Patients with baseline cognitive impairment have prolonged lengths of stay and complex needs after discharge. Agitation and behavioral symptoms of dementia can be exacerbated in the hospital setting and are often difficult to manage. Care of the patient with dementia requires that hospitalists engage in a multidisciplinary approach to inpatient and transitional care. Hospitalists may also become involved in hospital quality and safety initiatives that pertain to areas such as restraint use and fall prevention.
DEMENTIA KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate dementia from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate dementia.
Describe the causes of potentially reversible dementias or dementia-like conditions.
List indications, contraindications, and mechanisms of action of pharmacologic agents used to treat dementia.
Describe nonpharmacologic therapies to manage dementia symptoms.
Recognize the indications for specialty consultations.
Describe the complications of dementia in the hospitalized patient.
Discuss the multifaceted impact that dementia has on patients and their families.
Explain goals for hospital discharge including specific measures of clinical stability for safe care transition.
DEMENTIA SKILLS
Hospitalists should be able to:
Perform appropriate screening for dementia.
Develop active strategies to reduce development of delirium in patients with dementia in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected dementia in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Assess patients for potentially reversible causes of dementia or dementia-like conditions. Assess severity of cognitive impairment and perform a focused evaluation for the underlying etiology of dementia when appropriate.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with dementia.
Formulate and lead multidisciplinary teams to develop and implement care plans for patients with dementia.
Develop an appropriate pharmacologic plan to manage dementia.
Develop an appropriate nonpharmacologic plan to manage dementia.
Use a patient- and family-centered approach in the care of older inpatients.
Communicate with patients and families to explain the history and prognosis of dementia.
Use evidence-based methods and tools to assess patients’ medical decision-making capacity.
Defend patients’ right to autonomy when so qualified.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DEMENTIA ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with dementia that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of dementia and its causes.
Value a patient- and family-centered approach to educate and engage families and caregivers in the care of older inpatients.
Responsibly address and respect end-of-life care wishes for patients with advanced dementia.
DEMENTIA SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for poor outcomes related to dementia.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration withgeriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with dementia.
DELIRIUM
Delirium is defined as an acute, transient, global disorder of cognition. In two-thirds of cases, delirium occurs in patients with baseline vulnerability, including those with underlying dementia.1 Although up to 30% of older medical patients experience delirium during hospitalization, this condition is unrecognized in nearly two-thirds of cases.2-4 Patients with delirium experience an average increase in length of hospital stay of 8 days and mortality rates that are twice as high as those of patients without delirium.5,6 In addition, delirium is associated with high rates of functional and cognitive decline and skilled nursing facility placement after hospitalization. The cost of caring for patients with delirium has a marked impact on individual patients, families, and hospital systems. Hospitalists lead their institutions in the development of screening and prevention protocols for patients at risk for delirium, as well as in the promotion of safe treatment approaches. Hospitalists also develop strategies to operationalize cost-effective delirium prevention programs that improve outcomes.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
DELIRIUM KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate delirium from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate delirium.
Describe the causes of delirium in the hospital setting including environmental and iatrogenic risk factors.
Identify medications known to precipitate delirium.
Recognize the indications for specialty consultations.
Describe methods for the prevention of delirium.
Explain indications, contraindications, and mechanisms of action of pharmacologic agents used to treat delirium.
Describe nonpharmacologic therapies to manage delirium.
Describe the complications of delirium in the hospitalized patient.
Discuss the multifaceted impact that delirium has on patients and their families.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transitions.
DELIRIUM SKILLS
Hospitalists should be able to:
Predict a patient’s risk for the development of delirium on the basis of initial history and physical examination.
Perform appropriate screening for delirium.
Develop active strategies to reduce delirium in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected delirium in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Perform a focused evaluation for the underlying etiology of delirium and institute prompt treatment to lessen its severity.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with delirium.
Lead multidisciplinary teams to develop and implement care plans for patients with delirium.
Develop an appropriate pharmacologic plan to manage delirium.
Develop an appropriate nonpharmacologic plan to manage delirium.
Develop an appropriate management plan for patients with delirium in the postoperative setting.
Document an appropriate treatment plan to reduce mortality, limit the duration of delirium and the time required to control agitation, maintain adequate control of delirium, address complications, and manage cost of treatment.
Use a patient- and family-centered approach in the care of older inpatients.
Establish goals and boundaries of care with patients and their families.
Communicate with patients and families to explain the history and prognosis of delirium.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DELIRIUM ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with delirium that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of delirium and its causes.
Value a patient- and family-centered approach in the care of older inpatients.
DELIRIUM SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for delirium.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration with geriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with delirium.
DEMENTIA
Dementia is defined as a chronic, often progressive, decline in cognitive function, eventually limiting daily activities. Dementia is a common comorbidity in the hospitalized older patient. Alzheimer disease is the most prevalent form of dementia in older patients, and it accounts for up to 80% of cases.7,8 More than 5 million persons older than 65 years have Alzheimer disease in the United States.7,8 Patients with dementia are at increased risk for delirium, falls, and functional decline during hospitalization. Patients with baseline cognitive impairment have prolonged lengths of stay and complex needs after discharge. Agitation and behavioral symptoms of dementia can be exacerbated in the hospital setting and are often difficult to manage. Care of the patient with dementia requires that hospitalists engage in a multidisciplinary approach to inpatient and transitional care. Hospitalists may also become involved in hospital quality and safety initiatives that pertain to areas such as restraint use and fall prevention.
DEMENTIA KNOWLEDGE
Hospitalists should be able to:
Define delirium and dementia and distinguish between them.
Differentiate dementia from other causes of cognitive impairment, confusion, or psychosis.
Describe the indicated tests required to evaluate dementia.
Describe the causes of potentially reversible dementias or dementia-like conditions.
List indications, contraindications, and mechanisms of action of pharmacologic agents used to treat dementia.
Describe nonpharmacologic therapies to manage dementia symptoms.
Recognize the indications for specialty consultations.
Describe the complications of dementia in the hospitalized patient.
Discuss the multifaceted impact that dementia has on patients and their families.
Explain goals for hospital discharge including specific measures of clinical stability for safe care transition.
DEMENTIA SKILLS
Hospitalists should be able to:
Perform appropriate screening for dementia.
Develop active strategies to reduce development of delirium in patients with dementia in the hospital setting by identifying known patient risk factors that may precipitate delirium.
Assess patients with suspected dementia in a timely manner, identify the level of care required, and manage or comanage patients with the primary requesting service.
Assess patients for potentially reversible causes of dementia or dementia-like conditions. Assess severity of cognitive impairment and perform a focused evaluation for the underlying etiology of dementia when appropriate.
Determine the best setting within the hospital to initiate, monitor, evaluate, and treat patients with dementia.
Formulate and lead multidisciplinary teams to develop and implement care plans for patients with dementia.
Develop an appropriate pharmacologic plan to manage dementia.
Develop an appropriate nonpharmacologic plan to manage dementia.
Use a patient- and family-centered approach in the care of older inpatients.
Communicate with patients and families to explain the history and prognosis of dementia.
Use evidence-based methods and tools to assess patients’ medical decision-making capacity.
Defend patients’ right to autonomy when so qualified.
Facilitate discharge planning early in the hospitalization, including communicating with the primary care provider and presenting the patient and family with contact information for follow-up care, support, and rehabilitation.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
DEMENTIA ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach to the care of patients with dementia that begins at admission and continues through all care transitions.
Follow evidence-based recommendations to guide diagnosis, monitoring, and treatment of dementia and its causes.
Value a patient- and family-centered approach to educate and engage families and caregivers in the care of older inpatients.
Responsibly address and respect end-of-life care wishes for patients with advanced dementia.
DEMENTIA SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams to develop early treatment protocols.
Lead, coordinate, and/or participate in multidisciplinary initiatives to implement screening and prevention protocols for patients at risk for poor outcomes related to dementia.
Lead, coordinate, and/or participate in multidisciplinary initiatives, which may include collaboration withgeriatricians, to promote patient safety and cost-effective diagnostic and management strategies for older patients.
Engage stakeholders in hospital initiatives to improve safety and quality in the care of patients with dementia.
1. Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7-21.
2. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97(3):278-288.
3. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242.
4. Francis J. Delirium in older patients. J Am Geriatr Soc. 1992;40(8):829-838.
5. Cole MG, Primeau FJ. Prognosis of delirium in elderly hospital patients. CMAJ. 1993;149(1):41.
6. McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162(4):457-463.
7. Alzheimer’s Association. 2014 Alzheimer’s disease facts and figures. Available at: https://www.alz.org/downloads/Facts_Figures_2014.pdf. Accessed July 2015.
8. Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-1122.
1. Cole MG. Delirium in elderly patients. Am J Geriatr Psychiatry. 2004;12(1):7-21.
2. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97(3):278-288.
3. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242.
4. Francis J. Delirium in older patients. J Am Geriatr Soc. 1992;40(8):829-838.
5. Cole MG, Primeau FJ. Prognosis of delirium in elderly hospital patients. CMAJ. 1993;149(1):41.
6. McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162(4):457-463.
7. Alzheimer’s Association. 2014 Alzheimer’s disease facts and figures. Available at: https://www.alz.org/downloads/Facts_Figures_2014.pdf. Accessed July 2015.
8. Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119-1122.
© 2017 Society of Hospital Medicine
Diabetes Mellitus. 2017 Hospital Medicine Revised Core Competencies
Diabetes mellitus is a disease characterized by abnormal insulin production or disordered glucose metabolism and is a comorbid condition of many hospitalized patients. Diabetic ketoacidosis (DKA) and hyperglycemia hyperosmolar state (HHS) are extreme presentations of diabetes mellitus that require hospitalization. Diabetes mellitus is present in nearly 10% of the US population, and it is more common in older adults, affecting at least 25% of persons older than 65 years.1 Type 2 diabetes mellitus accounts for 90% to 95% of all diagnosed cases of diabetes in adults.1 Annually, more than 700,000 hospital discharges occur with diabetes mellitus or DKA as the primary diagnosis.2 Hospitalists care for diabetic patients and optimize glycemic control in the hospital setting. They stabilize and treat DKA and HHS. The inpatient setting provides an opportunity to institute therapies to slow disease progression, prevent disease complications, and provide diabetes education to improve quality of life and limit complications leading to readmission. Hospitalists use evidence-based approaches to optimize care and lead multidisciplinary teams to develop institutional guidelines or care pathways to optimize glycemic control.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define diabetes mellitus and explain the pathophysiologic processes that lead to hyperglycemia, DKA, and HHS.
Describe the impact of hyperglycemia on immune function and wound healing.
Describe the effect of DKA and HHS on intravascular volume status, electrolytes, and acid–base balance.
Describe the clinical presentation and laboratory findings of DKA and HHS.
Describe the indicated tests to evaluate and diagnose DKA and HHS.
Explain the physiologic stressors and medications that adversely affect glycemic control.
Explain the precipitating factors of DKA and HSS.
Identify the goals of glycemic control in hospitalized patients in various settings, including critically ill and surgical patients.
Recognize the indications for managing DKA and HHS in an intensive care unit.
Recognize indications for early specialty consultation, which may include endocrinology and nutrition.
Summarize the indications, contraindications, and mechanisms of action of pharmacologic agents used to treat diabetes mellitus.
Recognize features that indicate disease severity.
Recognize the impact of suboptimal glycemic control on other concurrent medical conditions and illness.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history and review the medical record to identify factors that can affect glycemic control.
Estimate the level of previous glycemic control, adherence to medication regimen, and social influences that may affect the quality of glycemic control in hospitalized patients.
Perform a comprehensive physical examination to identify possible precipitants of hyperglycemia, DKA, or HHS.
Select and interpret indicated studies in patients suspected of having DKA or HHS, including relevant metabolic and acid–base measurements.
Develop an individualized management plan for patients with controlled and uncontrolled diabetes mellitus, DKA, HHS, and any associated complications.
Adjust medications and dosages to achieve optimal glycemic control and minimize adverse effects.
Evaluate and treat the signs and symptoms of hypoglycemia (especially neuroglycopenia).
Direct the perioperative management of the diabetic patient, and when necessary, manage or comanage the patient with the primary requesting service.
Assess caloric and nutritional needs and recommend a suitable diet.
Assess hospitalized patients for undiagnosed diabetes mellitus.
Recognize and address the effects of various diabetic complications such as neuropathic pain.
Communicate with patients and families to explain the natural history and prognosis of diabetes mellitus.
Communicate with patients and families to explain potential long-term complications of diabetes mellitus and preventive strategies, including foot and eye care.
Communicate with patients and families to explain the importance of glycemic control and factors that affect it such as adhering to medication regimens and self-monitoring, following dietary and exercise recommendations, and attending routine follow-up appointments.
Communicate with patients and families to explain the potential adverse effects or adverse interactions of diabetes medications, including hypoglycemia.
Facilitate discharge planning early in the admission process.
Recommend appropriate postdischarge care, which may include endocrinology, ophthalmology, and podiatry.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians, including the need for continued nutrition and diabetic counseling.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, nutrition, social services, and diabetes education, to the care of patients with diabetes that begins at admission and continues through all care transitions.
Follow evidence-based recommendations in the treatment of inpatients with diabetes mellitus.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams, which may include nursing, nutrition, and endocrinology, to promote quality and cost-effective diabetes management.
Lead, coordinate, and/or participate in efforts to develop guidelines and protocols that standardize the assessment and management of uncontrolled diabetes mellitus, DKA, and HHS.
Lead, coordinate, and/or participate in initiatives to standardize hospital formulary-based diabetes therapies to reduce the likelihood of an adverse drug event.
Lead, coordinate, and/or participate in efforts to develop guidelines and/or protocols to optimize glycemic control in hospitalized patients including suitable regimens in critically ill medical and surgical patients.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services; 2014.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed July 2015.
Diabetes mellitus is a disease characterized by abnormal insulin production or disordered glucose metabolism and is a comorbid condition of many hospitalized patients. Diabetic ketoacidosis (DKA) and hyperglycemia hyperosmolar state (HHS) are extreme presentations of diabetes mellitus that require hospitalization. Diabetes mellitus is present in nearly 10% of the US population, and it is more common in older adults, affecting at least 25% of persons older than 65 years.1 Type 2 diabetes mellitus accounts for 90% to 95% of all diagnosed cases of diabetes in adults.1 Annually, more than 700,000 hospital discharges occur with diabetes mellitus or DKA as the primary diagnosis.2 Hospitalists care for diabetic patients and optimize glycemic control in the hospital setting. They stabilize and treat DKA and HHS. The inpatient setting provides an opportunity to institute therapies to slow disease progression, prevent disease complications, and provide diabetes education to improve quality of life and limit complications leading to readmission. Hospitalists use evidence-based approaches to optimize care and lead multidisciplinary teams to develop institutional guidelines or care pathways to optimize glycemic control.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define diabetes mellitus and explain the pathophysiologic processes that lead to hyperglycemia, DKA, and HHS.
Describe the impact of hyperglycemia on immune function and wound healing.
Describe the effect of DKA and HHS on intravascular volume status, electrolytes, and acid–base balance.
Describe the clinical presentation and laboratory findings of DKA and HHS.
Describe the indicated tests to evaluate and diagnose DKA and HHS.
Explain the physiologic stressors and medications that adversely affect glycemic control.
Explain the precipitating factors of DKA and HSS.
Identify the goals of glycemic control in hospitalized patients in various settings, including critically ill and surgical patients.
Recognize the indications for managing DKA and HHS in an intensive care unit.
Recognize indications for early specialty consultation, which may include endocrinology and nutrition.
Summarize the indications, contraindications, and mechanisms of action of pharmacologic agents used to treat diabetes mellitus.
Recognize features that indicate disease severity.
Recognize the impact of suboptimal glycemic control on other concurrent medical conditions and illness.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history and review the medical record to identify factors that can affect glycemic control.
Estimate the level of previous glycemic control, adherence to medication regimen, and social influences that may affect the quality of glycemic control in hospitalized patients.
Perform a comprehensive physical examination to identify possible precipitants of hyperglycemia, DKA, or HHS.
Select and interpret indicated studies in patients suspected of having DKA or HHS, including relevant metabolic and acid–base measurements.
Develop an individualized management plan for patients with controlled and uncontrolled diabetes mellitus, DKA, HHS, and any associated complications.
Adjust medications and dosages to achieve optimal glycemic control and minimize adverse effects.
Evaluate and treat the signs and symptoms of hypoglycemia (especially neuroglycopenia).
Direct the perioperative management of the diabetic patient, and when necessary, manage or comanage the patient with the primary requesting service.
Assess caloric and nutritional needs and recommend a suitable diet.
Assess hospitalized patients for undiagnosed diabetes mellitus.
Recognize and address the effects of various diabetic complications such as neuropathic pain.
Communicate with patients and families to explain the natural history and prognosis of diabetes mellitus.
Communicate with patients and families to explain potential long-term complications of diabetes mellitus and preventive strategies, including foot and eye care.
Communicate with patients and families to explain the importance of glycemic control and factors that affect it such as adhering to medication regimens and self-monitoring, following dietary and exercise recommendations, and attending routine follow-up appointments.
Communicate with patients and families to explain the potential adverse effects or adverse interactions of diabetes medications, including hypoglycemia.
Facilitate discharge planning early in the admission process.
Recommend appropriate postdischarge care, which may include endocrinology, ophthalmology, and podiatry.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians, including the need for continued nutrition and diabetic counseling.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, nutrition, social services, and diabetes education, to the care of patients with diabetes that begins at admission and continues through all care transitions.
Follow evidence-based recommendations in the treatment of inpatients with diabetes mellitus.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams, which may include nursing, nutrition, and endocrinology, to promote quality and cost-effective diabetes management.
Lead, coordinate, and/or participate in efforts to develop guidelines and protocols that standardize the assessment and management of uncontrolled diabetes mellitus, DKA, and HHS.
Lead, coordinate, and/or participate in initiatives to standardize hospital formulary-based diabetes therapies to reduce the likelihood of an adverse drug event.
Lead, coordinate, and/or participate in efforts to develop guidelines and/or protocols to optimize glycemic control in hospitalized patients including suitable regimens in critically ill medical and surgical patients.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations.
Diabetes mellitus is a disease characterized by abnormal insulin production or disordered glucose metabolism and is a comorbid condition of many hospitalized patients. Diabetic ketoacidosis (DKA) and hyperglycemia hyperosmolar state (HHS) are extreme presentations of diabetes mellitus that require hospitalization. Diabetes mellitus is present in nearly 10% of the US population, and it is more common in older adults, affecting at least 25% of persons older than 65 years.1 Type 2 diabetes mellitus accounts for 90% to 95% of all diagnosed cases of diabetes in adults.1 Annually, more than 700,000 hospital discharges occur with diabetes mellitus or DKA as the primary diagnosis.2 Hospitalists care for diabetic patients and optimize glycemic control in the hospital setting. They stabilize and treat DKA and HHS. The inpatient setting provides an opportunity to institute therapies to slow disease progression, prevent disease complications, and provide diabetes education to improve quality of life and limit complications leading to readmission. Hospitalists use evidence-based approaches to optimize care and lead multidisciplinary teams to develop institutional guidelines or care pathways to optimize glycemic control.
Want all 52 JHM Core Competency articles in an easy-to-read compendium? Order your copy now from Amazon.com.
KNOWLEDGE
Hospitalists should be able to:
Define diabetes mellitus and explain the pathophysiologic processes that lead to hyperglycemia, DKA, and HHS.
Describe the impact of hyperglycemia on immune function and wound healing.
Describe the effect of DKA and HHS on intravascular volume status, electrolytes, and acid–base balance.
Describe the clinical presentation and laboratory findings of DKA and HHS.
Describe the indicated tests to evaluate and diagnose DKA and HHS.
Explain the physiologic stressors and medications that adversely affect glycemic control.
Explain the precipitating factors of DKA and HSS.
Identify the goals of glycemic control in hospitalized patients in various settings, including critically ill and surgical patients.
Recognize the indications for managing DKA and HHS in an intensive care unit.
Recognize indications for early specialty consultation, which may include endocrinology and nutrition.
Summarize the indications, contraindications, and mechanisms of action of pharmacologic agents used to treat diabetes mellitus.
Recognize features that indicate disease severity.
Recognize the impact of suboptimal glycemic control on other concurrent medical conditions and illness.
Explain goals for hospital discharge, including specific measures of clinical stability for safe care transition.
SKILLS
Hospitalists should be able to:
Elicit a thorough and relevant medical history and review the medical record to identify factors that can affect glycemic control.
Estimate the level of previous glycemic control, adherence to medication regimen, and social influences that may affect the quality of glycemic control in hospitalized patients.
Perform a comprehensive physical examination to identify possible precipitants of hyperglycemia, DKA, or HHS.
Select and interpret indicated studies in patients suspected of having DKA or HHS, including relevant metabolic and acid–base measurements.
Develop an individualized management plan for patients with controlled and uncontrolled diabetes mellitus, DKA, HHS, and any associated complications.
Adjust medications and dosages to achieve optimal glycemic control and minimize adverse effects.
Evaluate and treat the signs and symptoms of hypoglycemia (especially neuroglycopenia).
Direct the perioperative management of the diabetic patient, and when necessary, manage or comanage the patient with the primary requesting service.
Assess caloric and nutritional needs and recommend a suitable diet.
Assess hospitalized patients for undiagnosed diabetes mellitus.
Recognize and address the effects of various diabetic complications such as neuropathic pain.
Communicate with patients and families to explain the natural history and prognosis of diabetes mellitus.
Communicate with patients and families to explain potential long-term complications of diabetes mellitus and preventive strategies, including foot and eye care.
Communicate with patients and families to explain the importance of glycemic control and factors that affect it such as adhering to medication regimens and self-monitoring, following dietary and exercise recommendations, and attending routine follow-up appointments.
Communicate with patients and families to explain the potential adverse effects or adverse interactions of diabetes medications, including hypoglycemia.
Facilitate discharge planning early in the admission process.
Recommend appropriate postdischarge care, which may include endocrinology, ophthalmology, and podiatry.
Communicate with patients and families to explain the goals of care, discharge instructions, and management after hospital discharge to ensure safe follow-up and transitions of care.
Document the treatment plan and provide clear discharge instructions for postdischarge clinicians, including the need for continued nutrition and diabetic counseling.
ATTITUDES
Hospitalists should be able to:
Employ a multidisciplinary approach, which may include nursing, nutrition, social services, and diabetes education, to the care of patients with diabetes that begins at admission and continues through all care transitions.
Follow evidence-based recommendations in the treatment of inpatients with diabetes mellitus.
SYSTEM ORGANIZATION AND IMPROVEMENT
To improve efficiency and quality within their organizations, hospitalists should:
Lead, coordinate, and/or participate in multidisciplinary teams, which may include nursing, nutrition, and endocrinology, to promote quality and cost-effective diabetes management.
Lead, coordinate, and/or participate in efforts to develop guidelines and protocols that standardize the assessment and management of uncontrolled diabetes mellitus, DKA, and HHS.
Lead, coordinate, and/or participate in initiatives to standardize hospital formulary-based diabetes therapies to reduce the likelihood of an adverse drug event.
Lead, coordinate, and/or participate in efforts to develop guidelines and/or protocols to optimize glycemic control in hospitalized patients including suitable regimens in critically ill medical and surgical patients.
Implement systems to ensure hospital-wide adherence to national standards and document those measures as specified by recognized organizations.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services; 2014.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed July 2015.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services; 2014.
2. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project. U.S. Department of Health & Human Services. Available at: http://hcupnet.ahrq.gov/. Accessed July 2015.
© 2017 Society of Hospital Medicine