User login
When “Different” Is Not OK
ANSWER
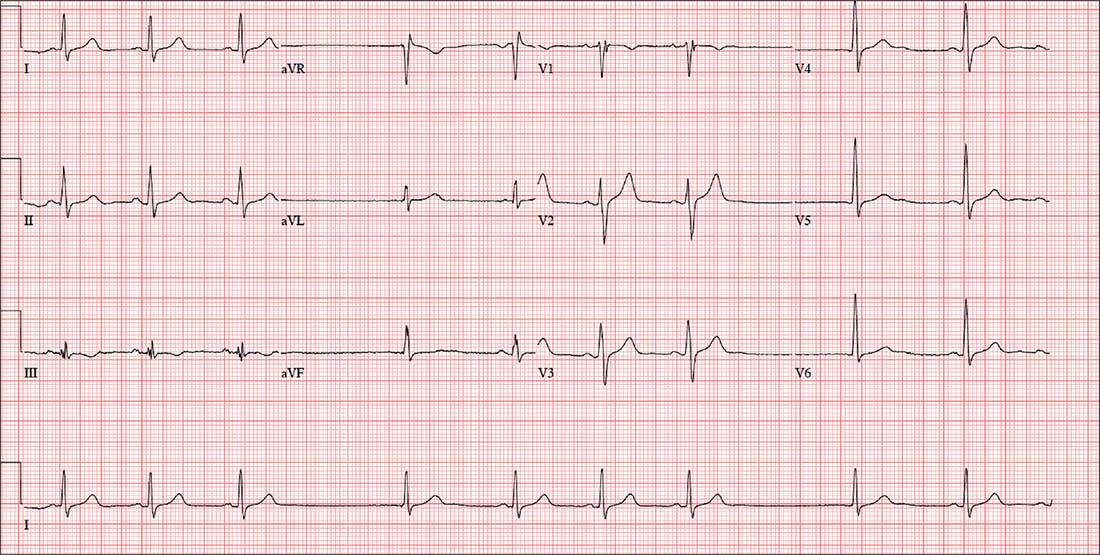
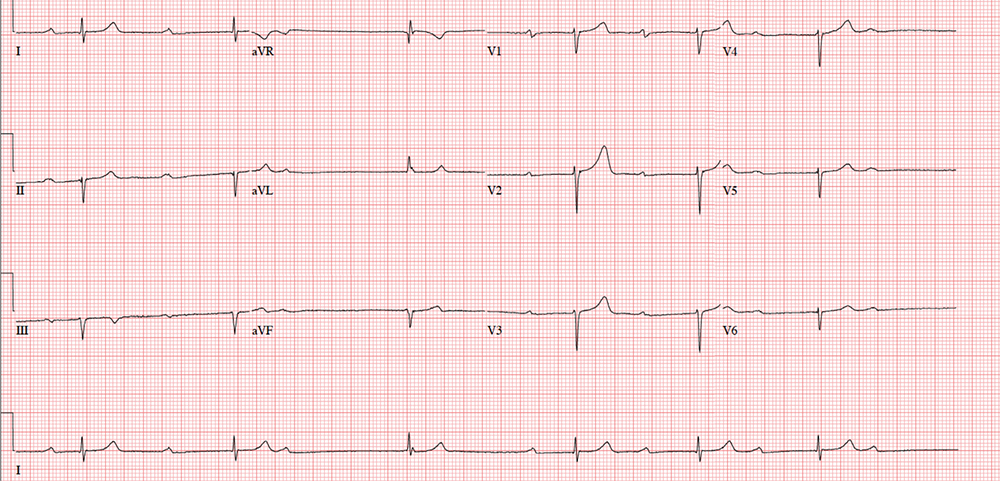
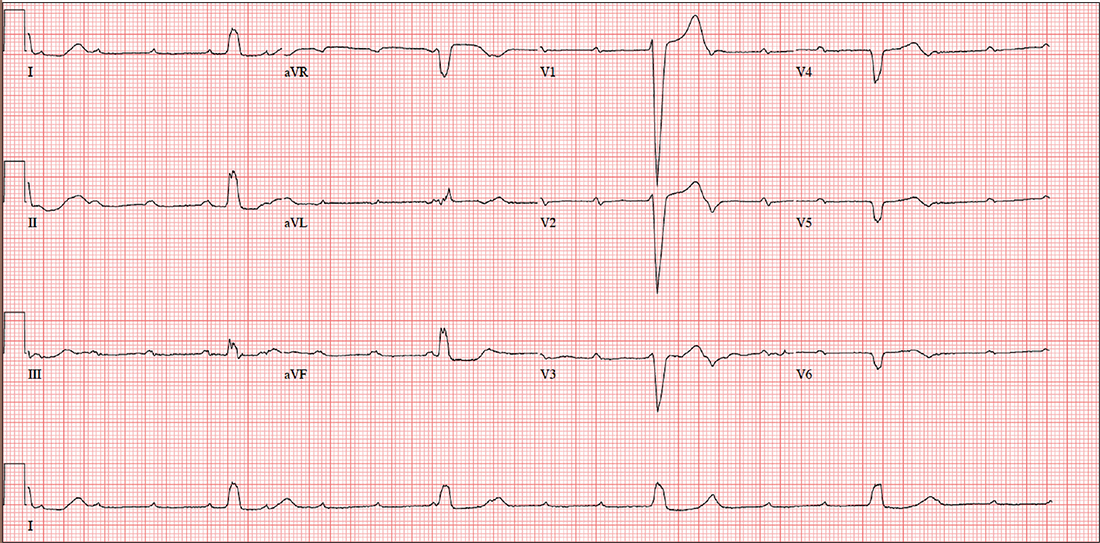
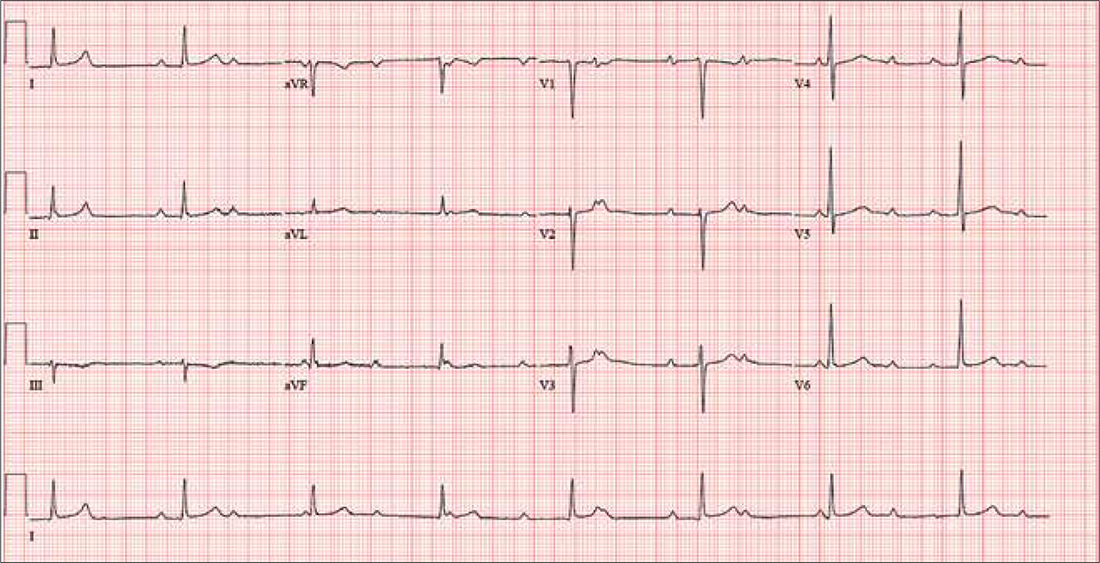
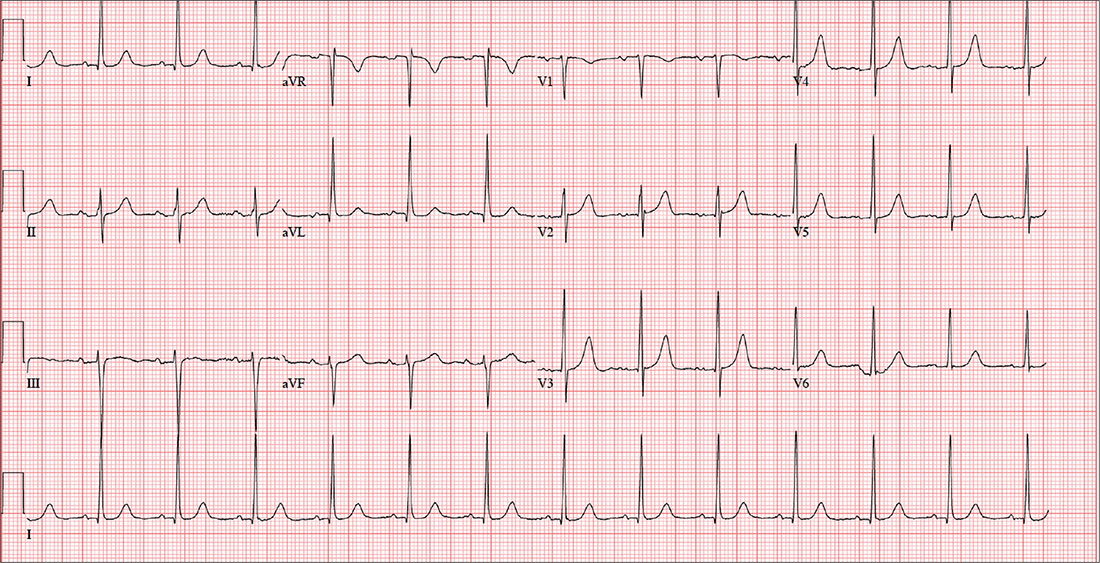
The correct interpretation includes sinus bradycardia, marked sinus arrhythmia, junctional escape beats with sinus arrest or a transient atrioventricular (AV) block, and an intraventricular conduction defect.
Sinus bradycardia is diagnosed based on narrow QRS intervals < 60 beats/min. Marked sinus arrhythmia is indicated by the narrow QRS intervals of similar size but with an irregular rhythm.
When the rate is slow and irregular, rather than use the 300/150/100 method, it is more accurate to count the number of QRS complexes in the rhythm strip and multiply by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). If the patient does not have a pacemaker, a range within two to three beats of the computer measurement is acceptable. In this case, 9 × 6 = 54 beats/min—very close to the interval measured by the computer.
The first three beats on the rhythm strip are sinus with a normal PQRST complex. After that, there is a pause (either sinus arrest or a transient AV block—we can’t tell which) that is interrupted by a junctional escape beat (no P wave, but the QRS is similar to the prior, normal complexes). The fifth, sixth, and seventh beats are normal sinus, followed by another pause with an ensuing junctional escape. The last QRS complex is another sinus beat.
Finally, although the QRS duration (122 ms) is greater than normal, the complexes in leads V1 and V6 do not constitute a right or left bundle branch block.
ANSWER
The correct interpretation includes sinus bradycardia, marked sinus arrhythmia, junctional escape beats with sinus arrest or a transient atrioventricular (AV) block, and an intraventricular conduction defect.
Sinus bradycardia is diagnosed based on narrow QRS intervals < 60 beats/min. Marked sinus arrhythmia is indicated by the narrow QRS intervals of similar size but with an irregular rhythm.
When the rate is slow and irregular, rather than use the 300/150/100 method, it is more accurate to count the number of QRS complexes in the rhythm strip and multiply by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). If the patient does not have a pacemaker, a range within two to three beats of the computer measurement is acceptable. In this case, 9 × 6 = 54 beats/min—very close to the interval measured by the computer.
The first three beats on the rhythm strip are sinus with a normal PQRST complex. After that, there is a pause (either sinus arrest or a transient AV block—we can’t tell which) that is interrupted by a junctional escape beat (no P wave, but the QRS is similar to the prior, normal complexes). The fifth, sixth, and seventh beats are normal sinus, followed by another pause with an ensuing junctional escape. The last QRS complex is another sinus beat.
Finally, although the QRS duration (122 ms) is greater than normal, the complexes in leads V1 and V6 do not constitute a right or left bundle branch block.
ANSWER
The correct interpretation includes sinus bradycardia, marked sinus arrhythmia, junctional escape beats with sinus arrest or a transient atrioventricular (AV) block, and an intraventricular conduction defect.
Sinus bradycardia is diagnosed based on narrow QRS intervals < 60 beats/min. Marked sinus arrhythmia is indicated by the narrow QRS intervals of similar size but with an irregular rhythm.
When the rate is slow and irregular, rather than use the 300/150/100 method, it is more accurate to count the number of QRS complexes in the rhythm strip and multiply by six (an ECG at standard paper speed takes 10 s; 6 × 10 s = 60 s). If the patient does not have a pacemaker, a range within two to three beats of the computer measurement is acceptable. In this case, 9 × 6 = 54 beats/min—very close to the interval measured by the computer.
The first three beats on the rhythm strip are sinus with a normal PQRST complex. After that, there is a pause (either sinus arrest or a transient AV block—we can’t tell which) that is interrupted by a junctional escape beat (no P wave, but the QRS is similar to the prior, normal complexes). The fifth, sixth, and seventh beats are normal sinus, followed by another pause with an ensuing junctional escape. The last QRS complex is another sinus beat.
Finally, although the QRS duration (122 ms) is greater than normal, the complexes in leads V1 and V6 do not constitute a right or left bundle branch block.
For four days, a 66-year-old man with New York Heart Association Class II congestive heart failure has been short of breath. Over the three years he has been your patient, he has generally done well on maximum medical therapy. He has never had a myocardial infarction (MI), atrial fibrillation, or symptoms suggestive of ischemia.
Three months ago, he was hospitalized following a robust meal. At the time, his left ventricular ejection fraction was 42% on echocardiogram, and he was in normal sinus rhythm; he responded quickly to diuresis. This time, he says, he feels “different.” He’s tired and lethargic, he can’t seem to catch his breath, and he just wants to sleep.
Medical history is remarkable for type 2 diabetes and cholecystitis. Surgical history includes a cholecystectomy and an open reduction and internal fixation of a right high ankle fracture. His current medications include metformin, lisinopril, metoprolol, spironolactone, furosemide, potassium chloride, and atorvastatin.
The patient, an accountant at a busy firm, is married with three healthy adult children. He has never smoked, and he drinks alcohol rarely on weekends. His father died during cardiac revascularization surgery at age 58, his mother died of heart failure complications at age 69, and his older brother had an inferior MI at age 68.
Review of systems is remarkable for a recent upper respiratory infection. The patient has also noticed that his abdomen seems distended and his urine output has diminished.
Vital signs include a blood pressure of 98/62 mm Hg; pulse, 50 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 97.6°F. His weight is 224 lb—a 7-lb increase since his last clinic visit—and his height, 68 in.
On physical exam, you note a well-groomed male in mild distress. Pertinent findings include distended neck veins with visible cannon waves and jugular venous distention to 10 cm. There are no carotid bruits. Auscultation of the chest reveals scattered rhonchi in all fields, with bilateral rales in both bases that do not clear with coughing.
Cardiac exam reveals a regular rhythm at a rate of 58 beats/min, with a grade II/VI systolic murmur best heard at the left sternal border. There are no gallops or clicks. On abdominal exam, the liver edge is palpable 2 cm below the right costal margin. Bowel tones are present in all quadrants. There is no hepatojugular reflux or tenderness.
The lower extremities have 3+ pitting edema below the knees. Peripheral pulses are present and equal bilaterally, and there is no cyanosis or clubbing. The neurologic exam reveals mild sensory loss in both feet, with no perception of 2-point discrimination in the toes of the left foot.
An ECG reveals a ventricular rate of 55 beats/min; PR interval, 146 ms; QRS duration, 122 ms; QT/QTc interval, 424/405 ms; P axis, 60°; R axis, 38°; and T axis, 29°. What is your interpretation?
Breaking More Than the Fall
ANSWER
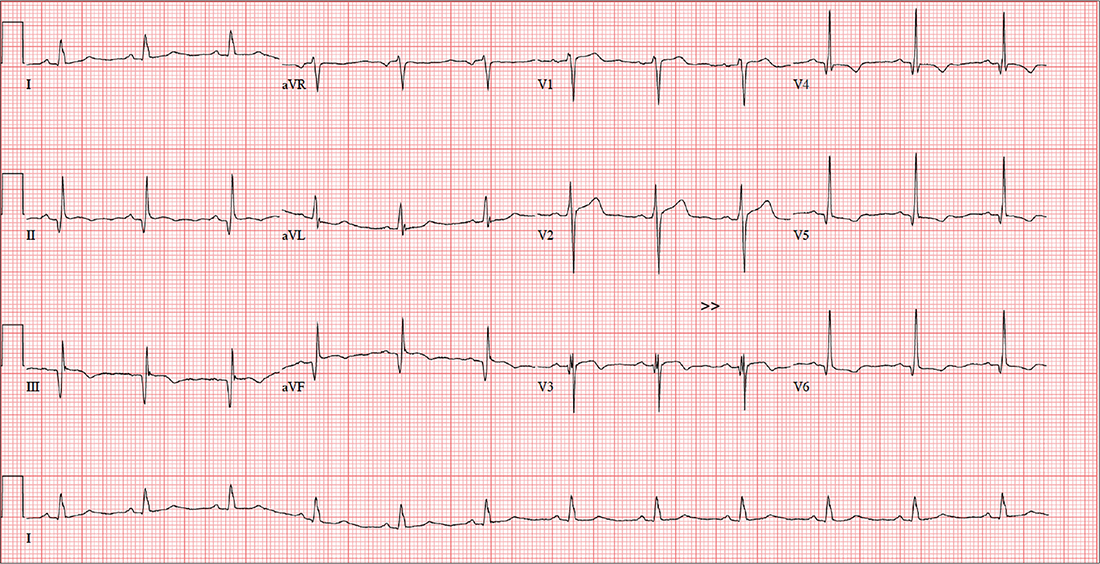
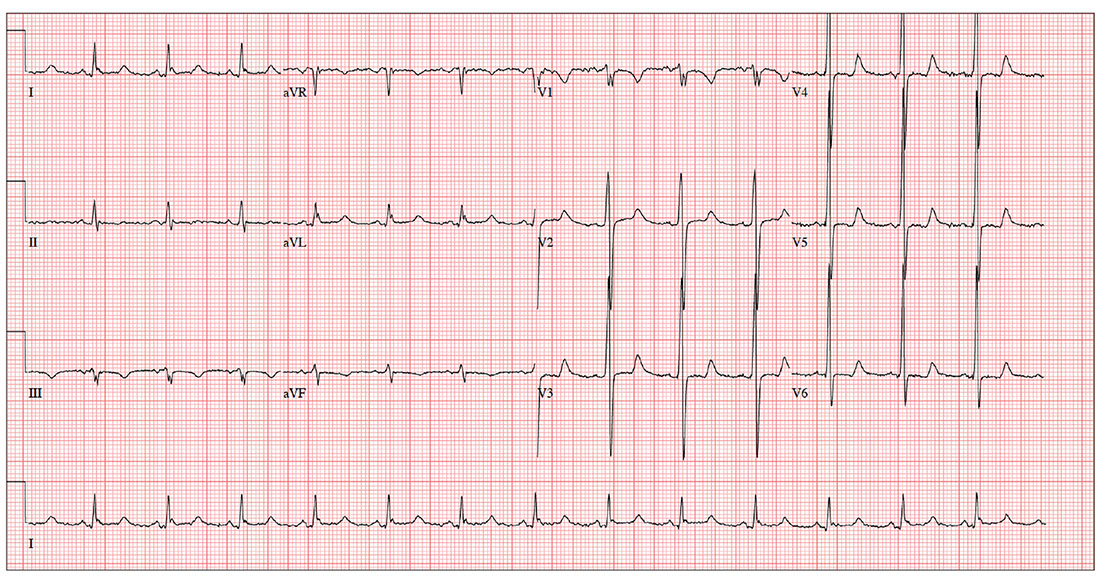
This ECG demonstrates sinus rhythm with premature atrial contractions (PACs), a normal axis, a right bundle branch block, a prolonged QTc interval, and T-wave abnormalities suggestive of lateral ischemia.
Sinus rhythm is indicated by a P wave for every QRS complex and a QRS complex for every P wave with a consistent PR interval.
PACs are seen on the seventh, 10th, and 12th beats on the rhythm strip. Notice that the R-R interval is shortened, the R wave of the PACs is identical to that of sinus rhythm, and there is a compensatory pause following the PAC before the sinus rhythm ensues. The R-wave axis of 26° is within the normal range (–30° to 90°).
A right bundle branch block is identified by a QRS duration > 120 ms (156 ms), an RSR’ “rabbit ear” pattern in the anterior precordial leads (particularly lead V1), and slurred S waves in leads I and aVL. Although opinions vary, a QTc interval > 460 ms in women (> 440 ms in men) is typically considered prolonged. This patient fits that criteria (529 ms). Finally, the ST depressions in leads V4 to V6 suggest lateral ischemia.
A comparison of this ECG to one obtained a year ago showed no difference, with the exception of new-onset PACs. The patient was cleared for surgical repair of her forearm fracture.
ANSWER
This ECG demonstrates sinus rhythm with premature atrial contractions (PACs), a normal axis, a right bundle branch block, a prolonged QTc interval, and T-wave abnormalities suggestive of lateral ischemia.
Sinus rhythm is indicated by a P wave for every QRS complex and a QRS complex for every P wave with a consistent PR interval.
PACs are seen on the seventh, 10th, and 12th beats on the rhythm strip. Notice that the R-R interval is shortened, the R wave of the PACs is identical to that of sinus rhythm, and there is a compensatory pause following the PAC before the sinus rhythm ensues. The R-wave axis of 26° is within the normal range (–30° to 90°).
A right bundle branch block is identified by a QRS duration > 120 ms (156 ms), an RSR’ “rabbit ear” pattern in the anterior precordial leads (particularly lead V1), and slurred S waves in leads I and aVL. Although opinions vary, a QTc interval > 460 ms in women (> 440 ms in men) is typically considered prolonged. This patient fits that criteria (529 ms). Finally, the ST depressions in leads V4 to V6 suggest lateral ischemia.
A comparison of this ECG to one obtained a year ago showed no difference, with the exception of new-onset PACs. The patient was cleared for surgical repair of her forearm fracture.
ANSWER
This ECG demonstrates sinus rhythm with premature atrial contractions (PACs), a normal axis, a right bundle branch block, a prolonged QTc interval, and T-wave abnormalities suggestive of lateral ischemia.
Sinus rhythm is indicated by a P wave for every QRS complex and a QRS complex for every P wave with a consistent PR interval.
PACs are seen on the seventh, 10th, and 12th beats on the rhythm strip. Notice that the R-R interval is shortened, the R wave of the PACs is identical to that of sinus rhythm, and there is a compensatory pause following the PAC before the sinus rhythm ensues. The R-wave axis of 26° is within the normal range (–30° to 90°).
A right bundle branch block is identified by a QRS duration > 120 ms (156 ms), an RSR’ “rabbit ear” pattern in the anterior precordial leads (particularly lead V1), and slurred S waves in leads I and aVL. Although opinions vary, a QTc interval > 460 ms in women (> 440 ms in men) is typically considered prolonged. This patient fits that criteria (529 ms). Finally, the ST depressions in leads V4 to V6 suggest lateral ischemia.
A comparison of this ECG to one obtained a year ago showed no difference, with the exception of new-onset PACs. The patient was cleared for surgical repair of her forearm fracture.
A 74-year-old woman becomes dizzy and slips in the shower. She instinctively extends her left arm and feels a snap as it hits the floor. H
Medical history is remarkable for hypertension, hypothyroidism, renal insufficiency, and benign positional vertigo. The patient denies cardiac history, including angina, dyspnea, or syncope. She describes her prefall dizziness as similar to her vertigo-related symptoms.
Family history is remarkable for hypertension, type 2 diabetes, stroke (mother), and myocardial infarction (brother). Her father’s medical history is unknown.
The patient is a retired high school librarian. She has never smoked or used recreational drugs, but she does enjoy a daily “nightcap” of brandy. Her current medications include furosemide, metoprolol, and levothyroxine. She has no known drug allergies.
She denies any recent infection, including cold or flu. A 12-point review of systems is unremarkable. Vital signs include a blood pressure of 142/88 mm Hg; pulse, 88 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98.4°F. Her height is 5’6” and her weight, 147 lb.
The patient is alert, cooperative, and oriented to person, place, and time. HEENT exam is remarkable for corrective lenses and bilateral hearing aids. There is no obvious sign of head trauma. The neck is supple, and there are no carotid bruits or jugular venous distention. The thyroid is small but palpable. The lungs are clear in all fields without rales, rhonchi, or wheezes.
Cardiac exam reveals a regular rate of 88 beats/min with occasional pauses. There is a soft II/VI murmur of mitral regurgitation heard at the left lower sternal border. There are no extra heart sounds or rubs. The abdomen is soft and nontender. There is no palpable organomegaly.
The extremities demonstrate full range of motion. Pulses are full and equal bilaterally, and there is no peripheral edema. The neurologic exam is intact.
An ECG shows a ventricular rate of 87 beats/min; PR interval, 156 ms; QRS duration, 138 ms; QT/QTc interval, 440/529 ms; P axis, 58°; R axis, 26°; and T axis, 105°. What is your interpretation?
Once Retired, Now Just Tired
ANSWER
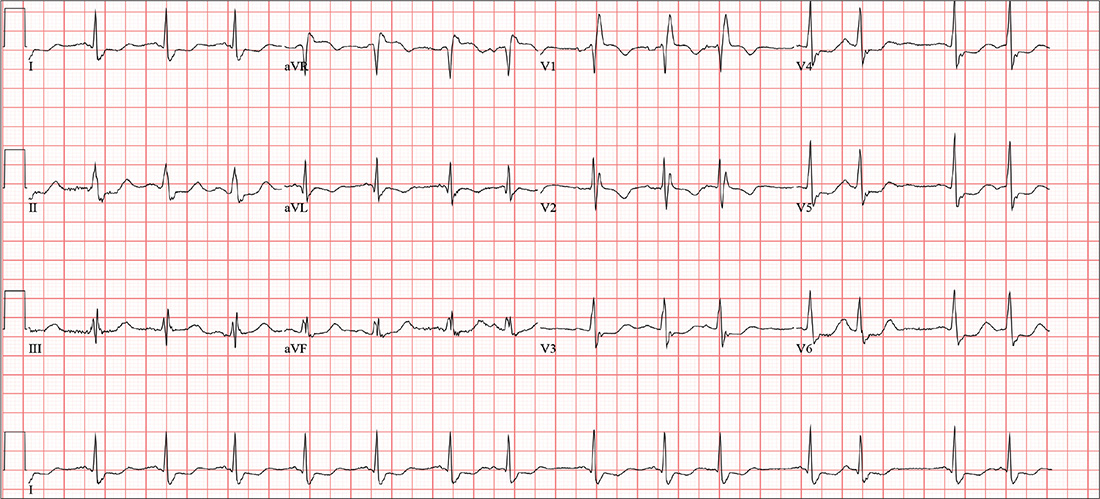
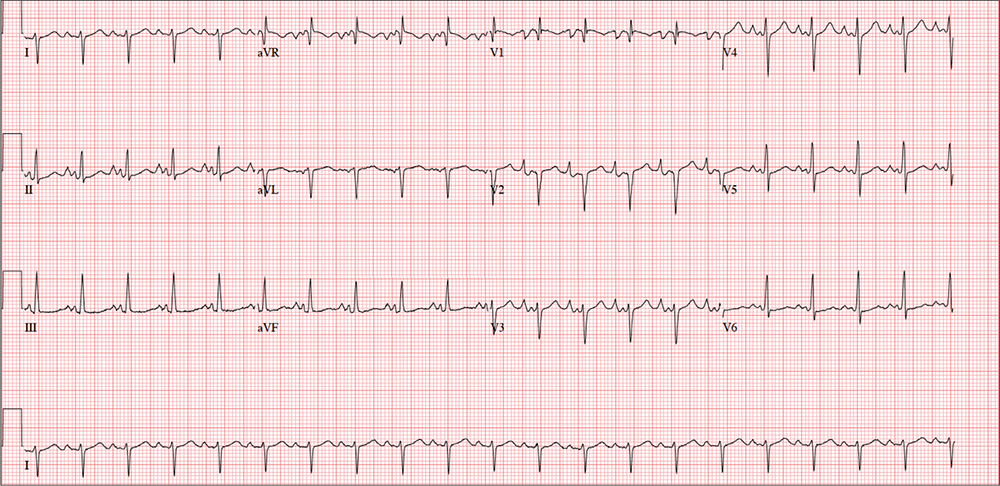
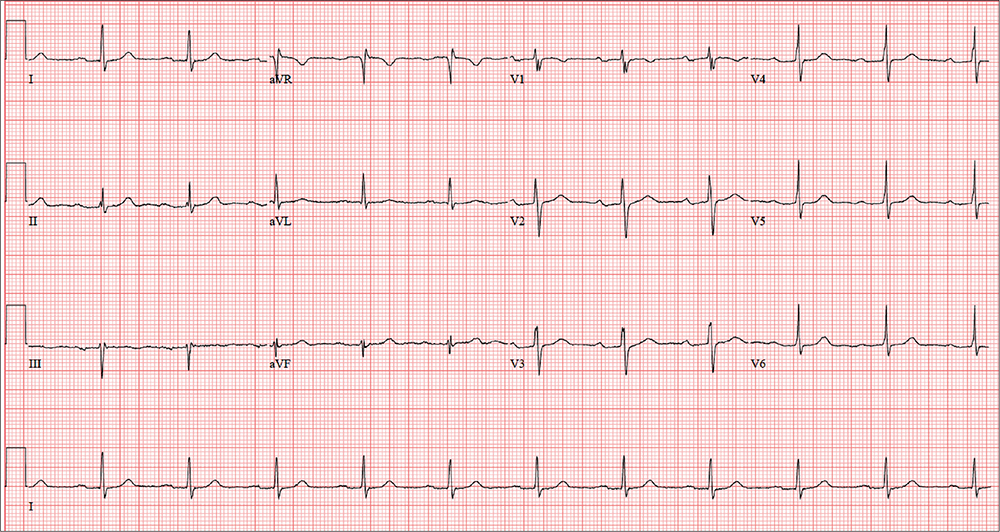
The correct interpretation includes marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I) and occasional junctional escape, left-axis deviation, and evidence of an inferior MI. Poor R-wave progression is also noted in the precordial leads.
Marked sinus bradycardia is seen in the first three and the last four P waves of the rhythm strip. The P-P intervals have a rate of 50 beats/min—different than the overall rate of the QRS complex (remember, “sinus” is synonymous with “P wave”!). The rate of the QRS complex (38 beats/min) is slower than the atrial rate, signifying a block of some sort.
Second-degree AV block is evident from the lengthening PR interval in the first two P-QRS complexes, followed by a P wave with no associated QRS complex. Although the fourth QRS complex in the rhythm strip is narrow and similar in appearance to the others, it’s too far from the previous P wave to have been conducted from the atrium—indicating a junctional escape beat arising from the AV node. (The rhythm returns to second-degree AV block for the remainder of the beats seen on the ECG.)
Left-axis deviation is signified by the R axis of –78° (lower than the normal limit of –30°). The Q waves in leads II, III, and aVF indicate a prior inferior MI. Finally, poor R-wave progression is seen in the precordial leads, with no significant transition between leads V1 and V6.
Although second-degree AV block is not an indication for permanent pacing, symptomatic bradycardia that persists despite medical management is. Because this patient was symptomatic while taking an AV nodal blocking agent (metoprolol), a permanent pacemaker was recommended.
ANSWER
The correct interpretation includes marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I) and occasional junctional escape, left-axis deviation, and evidence of an inferior MI. Poor R-wave progression is also noted in the precordial leads.
Marked sinus bradycardia is seen in the first three and the last four P waves of the rhythm strip. The P-P intervals have a rate of 50 beats/min—different than the overall rate of the QRS complex (remember, “sinus” is synonymous with “P wave”!). The rate of the QRS complex (38 beats/min) is slower than the atrial rate, signifying a block of some sort.
Second-degree AV block is evident from the lengthening PR interval in the first two P-QRS complexes, followed by a P wave with no associated QRS complex. Although the fourth QRS complex in the rhythm strip is narrow and similar in appearance to the others, it’s too far from the previous P wave to have been conducted from the atrium—indicating a junctional escape beat arising from the AV node. (The rhythm returns to second-degree AV block for the remainder of the beats seen on the ECG.)
Left-axis deviation is signified by the R axis of –78° (lower than the normal limit of –30°). The Q waves in leads II, III, and aVF indicate a prior inferior MI. Finally, poor R-wave progression is seen in the precordial leads, with no significant transition between leads V1 and V6.
Although second-degree AV block is not an indication for permanent pacing, symptomatic bradycardia that persists despite medical management is. Because this patient was symptomatic while taking an AV nodal blocking agent (metoprolol), a permanent pacemaker was recommended.
ANSWER
The correct interpretation includes marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I) and occasional junctional escape, left-axis deviation, and evidence of an inferior MI. Poor R-wave progression is also noted in the precordial leads.
Marked sinus bradycardia is seen in the first three and the last four P waves of the rhythm strip. The P-P intervals have a rate of 50 beats/min—different than the overall rate of the QRS complex (remember, “sinus” is synonymous with “P wave”!). The rate of the QRS complex (38 beats/min) is slower than the atrial rate, signifying a block of some sort.
Second-degree AV block is evident from the lengthening PR interval in the first two P-QRS complexes, followed by a P wave with no associated QRS complex. Although the fourth QRS complex in the rhythm strip is narrow and similar in appearance to the others, it’s too far from the previous P wave to have been conducted from the atrium—indicating a junctional escape beat arising from the AV node. (The rhythm returns to second-degree AV block for the remainder of the beats seen on the ECG.)
Left-axis deviation is signified by the R axis of –78° (lower than the normal limit of –30°). The Q waves in leads II, III, and aVF indicate a prior inferior MI. Finally, poor R-wave progression is seen in the precordial leads, with no significant transition between leads V1 and V6.
Although second-degree AV block is not an indication for permanent pacing, symptomatic bradycardia that persists despite medical management is. Because this patient was symptomatic while taking an AV nodal blocking agent (metoprolol), a permanent pacemaker was recommended.
A 72-year-old
Medical history is remarkable for type 2 diabetes, hypercholesterolemia, coronary artery disease, and a remote inferior myocardial infarction (MI) 14 years ago. Surgical history includes a cholecystectomy and an open reduction and internal fixation of a left high ankle fracture.
His current medication list includes metformin, isosorbide dinitrate, metoprolol, and atorvastatin. He has an anaphylactic allergy to sulfa. He cannot give a family history, as he was adopted and does not know his biological family.
The patient, a retired welder, is a recovering alcoholic; he attends Alcoholics Anonymous meetings regularly and has been sober for more than 12 years. He smoked a half-pack of cigarettes each day as a teenager but quit when he got married 52 years ago. He is a widower. His son died in an automobile accident at age 32; his daughter lives nearby and checks on him every day.
Review of systems is remarkable for neuropathic foot pain due to diabetes, recurrent constipation, corrective lenses, and hearing aids. The remainder of the review is noncontributory.
Vital signs include a blood pressure of 112/56 mm Hg; pulse, 40 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 99.2°F. His height is 76 in and his weight, 194 lb. Physical exam reveals an elderly but otherwise healthy-looking male in no distress.
The HEENT exam is remarkable for early cataract formation but is otherwise normal. His dentition is in remarkably excellent health. There is no thyromegaly or jugular venous distention, and the lungs are clear in all fields without wheezes or crackles.
Cardiac exam reveals a roughly normal rate of 40 beats/min. It is difficult to determine whether there is respiratory variation, given the slower rate. There is an early grade II/VI systolic murmur of aortic sclerosis best heard at the left upper sternal border. It does not radiate elsewhere. There are no extra heart sounds or rubs.
The abdomen has well-healed surgical scars with no palpable organomegaly. Bowel sounds are present in all quadrants. A rectal exam reveals impaction of firm stool; the prostate is not palpable given the amount of firm stool present.
The extremities have full range of motion without clubbing, cyanosis, or edema. Peripheral pulses are full bilaterally in both upper and lower extremities. A well-healed surgical scar is present on the left lateral lower extremity, and a plate is palpable beneath the skin. Skin sensitivity testing with 2-point pinprick of the soles and toes of both feet reveals extensive paresthesias. Apart from this, the neurologic exam is grossly normal. There is no evidence of diabetic foot ulcers.
An ECG shows a ventricular rate of 38 beats/min; no discernable PR interval; QRS duration, 78 ms; QT/QTc interval, 434/345 ms; P axis, 25°; R axis, –78°; and T axis, 13°. What is your interpretation?
A (Not So) Humerus Situation
ANSWER
This ECG shows evidence of sinus tachycardia with biatrial enlargement, right-axis deviation, right ventricular hypertrophy, and poor R-wave progression consistent with a septal MI.
Sinus tachycardia is signified by an atrial rate > 100 beats/min. The markedly notched P waves in leads I and II and biphasic P waves in lead V1 suggest biatrial enlargement. Right-axis deviation is diagnosed based on the R axis of 119°, and right ventricular hypertrophy is indicated by the right-axis deviation, a QR pattern in lead V1, and an R wave ≥ 5 mm in lead aVR. All of the above are findings seen with a history of pulmonary hypertension.
Poor R-wave progression in leads V1 to V4 suggests a septal MI of indeterminate age; however, there is no history of previous infarction.
The patient was diagnosed with a complex fracture of the left humerus and referred to orthopedics for repair. At his request, a pulmonary medicine consultation was ordered so that he could establish care in this facility.
ANSWER
This ECG shows evidence of sinus tachycardia with biatrial enlargement, right-axis deviation, right ventricular hypertrophy, and poor R-wave progression consistent with a septal MI.
Sinus tachycardia is signified by an atrial rate > 100 beats/min. The markedly notched P waves in leads I and II and biphasic P waves in lead V1 suggest biatrial enlargement. Right-axis deviation is diagnosed based on the R axis of 119°, and right ventricular hypertrophy is indicated by the right-axis deviation, a QR pattern in lead V1, and an R wave ≥ 5 mm in lead aVR. All of the above are findings seen with a history of pulmonary hypertension.
Poor R-wave progression in leads V1 to V4 suggests a septal MI of indeterminate age; however, there is no history of previous infarction.
The patient was diagnosed with a complex fracture of the left humerus and referred to orthopedics for repair. At his request, a pulmonary medicine consultation was ordered so that he could establish care in this facility.
ANSWER
This ECG shows evidence of sinus tachycardia with biatrial enlargement, right-axis deviation, right ventricular hypertrophy, and poor R-wave progression consistent with a septal MI.
Sinus tachycardia is signified by an atrial rate > 100 beats/min. The markedly notched P waves in leads I and II and biphasic P waves in lead V1 suggest biatrial enlargement. Right-axis deviation is diagnosed based on the R axis of 119°, and right ventricular hypertrophy is indicated by the right-axis deviation, a QR pattern in lead V1, and an R wave ≥ 5 mm in lead aVR. All of the above are findings seen with a history of pulmonary hypertension.
Poor R-wave progression in leads V1 to V4 suggests a septal MI of indeterminate age; however, there is no history of previous infarction.
The patient was diagnosed with a complex fracture of the left humerus and referred to orthopedics for repair. At his request, a pulmonary medicine consultation was ordered so that he could establish care in this facility.
While clearing leaves from his gutters, a 44-year-old man falls approximately 12 feet, hitting his left upper arm on the concrete curb. His neighbor sees him fall and comes quickly to his aid; after stabilizing the arm, the neighbor drives him to your facility. The patient reports feeling and hearing a snap and says he suspects he has fractured his humerus.
Medical history is remarkable for idiopathic pulmonary arterial hypertension, diagnosed at age 30. Symptoms at that time included dyspnea with exercise (and later, at rest), fatigue, palpitations, near-syncope, and lower extremity swelling. He has a pulmonologist at another facility but admits he’s not compliant with medications or appointments because he doesn’t like his doctor. He hasn’t had an exacerbation in the past two months.
Surgical history includes a tonsillectomy as a child.
His current medications include multiple inhalers (he can’t remember any names) and tadalafil, which he takes daily. He’s supposed to take warfarin but says he hasn’t done so for at least six months. He has no known drug allergies.
Two of his four siblings have pulmonary hypertension; the family had genetic testing performed to rule out a gene mutation. His father had cardiac sarcoidosis and died of an arrhythmia. His mother is in good health.
The patient, a welder, is on medical disability. He initially denies smoking, then admits to having two or three cigarettes a day. He drinks three beers a day and “a few more” on the weekends. He denies current illicit drug use but details heavy methamphetamine use in his early 20s.
Review of systems is noncontributory; he says he’s in a lot of pain and “does not want to go into my life story.” He denies shortness of breath or chest pain.
Vital signs include a blood pressure of 162/98 mm Hg; pulse, 120 beats/min; respiratory rate, 18 breaths/min-1; and temperature, 96.4°F. His weight is 214 lb and his height, 74 in.
Physical exam reveals an anxious male in apparent pain, holding his left arm against his side with his right hand. A cursory HEENT exam reveals no obvious trauma. His lungs have scattered crackles in all lung fields. The cardiac exam reveals a regular rhythm at a rate of 120 beats/min. There are no murmurs or rubs. The abdomen is soft and nontender.
The left upper arm has multiple abrasions, and there is point tenderness and swelling in the mid-portion of the humerus. There is no visual evidence of a compound fracture, but the bone appears displaced. Aside from additional abrasions on the left hip and lower leg, the remainder of the physical exam is unremarkable.
Given the history of pulmonary hypertension and findings of tachycardia on physical exam, an ECG is obtained prior to sending the patient to radiology. The ECG reveals a ventricular rate of 122 beats/min; PR interval, 164 ms; QRS duration, 68 ms; QT/QTc interval, 310/441 ms; P axis, 15°; R axis, 119°; and T axis, 37°. What is your interpretation?
From 5K to … the End of the Driveway
ANSWER
The correct interpretation includes sinus tachycardia with complete heart block and an idioventricular rhythm. Careful review of this ECG confirms complete atrioventricular dissociation, which is indicative of complete heart block.
Sinus tachycardia is indicated by a consistent P-P interval at a rate of 110 beats/min, idioventricular rhythm with a regular (but not normal) rate, and prolonged QRS interval of 148 ms. In this patient’s case, the tachycardia was presumed to be due to his upper respiratory infection. He underwent permanent pacemaker placement and resumed his normal activities without restriction.
ANSWER
The correct interpretation includes sinus tachycardia with complete heart block and an idioventricular rhythm. Careful review of this ECG confirms complete atrioventricular dissociation, which is indicative of complete heart block.
Sinus tachycardia is indicated by a consistent P-P interval at a rate of 110 beats/min, idioventricular rhythm with a regular (but not normal) rate, and prolonged QRS interval of 148 ms. In this patient’s case, the tachycardia was presumed to be due to his upper respiratory infection. He underwent permanent pacemaker placement and resumed his normal activities without restriction.
ANSWER
The correct interpretation includes sinus tachycardia with complete heart block and an idioventricular rhythm. Careful review of this ECG confirms complete atrioventricular dissociation, which is indicative of complete heart block.
Sinus tachycardia is indicated by a consistent P-P interval at a rate of 110 beats/min, idioventricular rhythm with a regular (but not normal) rate, and prolonged QRS interval of 148 ms. In this patient’s case, the tachycardia was presumed to be due to his upper respiratory infection. He underwent permanent pacemaker placement and resumed his normal activities without restriction.
Until three weeks ago, this 74-year-old man walked three miles every day without difficulty. But now, shortness of breath forces him to stop walking before he even reaches the end of his driveway. He denies chest pain (at rest or on exertion), palpitations, dyspnea at rest, and paroxysmal nocturnal dyspnea. There have been no recent weight changes.
Four years ago, he was diagnosed with coronary artery disease after experiencing chest pain at rest. A coronary angiography revealed stenosis in the proximal right coronary artery and the second obtuse marginal branch of his circumflex coronary artery; drug-eluting stents were placed, and he has had no further symptoms. An echocardiogram performed at a routine clinic visit six months ago showed mild aortic valve sclerosis, a left ventricular ejection fraction of 64%, and no regional wall motion abnormalities.
Surgical history is also remarkable for an open reduction and stabilization of a right high ankle fracture 10 years ago. Medical history includes type 2 diabetes and hyperlipidemia; treatment has normalized his A1C and his lipid panel.
His current medication list includes metoprolol, isosorbide dinitrate, metformin, and atorvastatin. He has no known drug allergies. He is unaware of any medical issues with his parents or grandparents.
The patient has two adult sons who live abroad and visit once a year. He was married for 53 years but lost his wife to lung cancer three years ago; her diagnosis prompted him to quit his long-term smoking habit. He consumes alcohol socially, having “one or two beers with friends on the weekends,” but denies current or previous use of marijuana or nonprescribed medications.
Review of systems is remarkable for a three-day history of upper respiratory infection with cough and rhinitis. He denies any change in bowel or bladder function.
Vital signs include a blood pressure of 104/54 mm Hg; pulse, 30 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 99.4°F. His weight is 169 lb and his height, 70 in.
On physical exam, you note a thin, healthy-looking male in no acute distress. Pertinent findings include internally inflamed nares and oropharynx, a few scattered rales in both lower lung fields that clear with coughing, and no wheezing. There are no palpable lymph nodes in the head or neck.
Cardiac exam reveals a regular rhythm of 30 beats/min with no murmurs, rubs, or extra heart sounds. The abdomen is soft and nontender. Peripheral pulses are strong and palpable in both upper and lower extremities, and there is no peripheral edema. The neurologic exam is intact, without evidence of diabetic neuropathy.
Given the slow heart rate observed on physical exam, an ECG is ordered. It shows a ventricular rate of 29 beats/min; no discernable PR interval; QRS duration, 148 ms; QT/QTc interval, 584/405 ms; P axis, 64°; R axis, 55°; and T axis, 83°. What is your interpretation?
Taking One for the Team
ANSWER
The correct interpretation of this patient’s ECG includes sinus rhythm with a first-degree atrioventricular (AV) block, otherwise within normal limits. A first-degree AV block is diagnosed based on a PR interval > 200 ms, which represents a prolonged conduction time from the sinus node to the ventricles. A 1:1 ratio of P waves to QRS complexes with consistent PR intervals eliminates the possibility of a second- or third-degree heart block.
First-degree AV block is generally a benign finding. However, care should be taken if the patient ever needs medications to slow AV nodal conduction (ie, ß-blockers, calcium channel blockers).
Finally, it may be tempting to consider Wolff-Parkinson-White syndrome based on the delta wave seen in leads V4 to V6. But this possibility is ruled out by the presence of a first-degree AV block.
ANSWER
The correct interpretation of this patient’s ECG includes sinus rhythm with a first-degree atrioventricular (AV) block, otherwise within normal limits. A first-degree AV block is diagnosed based on a PR interval > 200 ms, which represents a prolonged conduction time from the sinus node to the ventricles. A 1:1 ratio of P waves to QRS complexes with consistent PR intervals eliminates the possibility of a second- or third-degree heart block.
First-degree AV block is generally a benign finding. However, care should be taken if the patient ever needs medications to slow AV nodal conduction (ie, ß-blockers, calcium channel blockers).
Finally, it may be tempting to consider Wolff-Parkinson-White syndrome based on the delta wave seen in leads V4 to V6. But this possibility is ruled out by the presence of a first-degree AV block.
ANSWER
The correct interpretation of this patient’s ECG includes sinus rhythm with a first-degree atrioventricular (AV) block, otherwise within normal limits. A first-degree AV block is diagnosed based on a PR interval > 200 ms, which represents a prolonged conduction time from the sinus node to the ventricles. A 1:1 ratio of P waves to QRS complexes with consistent PR intervals eliminates the possibility of a second- or third-degree heart block.
First-degree AV block is generally a benign finding. However, care should be taken if the patient ever needs medications to slow AV nodal conduction (ie, ß-blockers, calcium channel blockers).
Finally, it may be tempting to consider Wolff-Parkinson-White syndrome based on the delta wave seen in leads V4 to V6. But this possibility is ruled out by the presence of a first-degree AV block.
In an effort to detect cardiopulmonary abnormalities in student athletes, a local university holds a screening event in which an
On exam, he appears in excellent health and has no medical or physical complaints. His medical history is unremarkable. He has participated in sports for most of his life and has never had symptoms of chest pain, dyspnea, shortness of breath, syncope, or near-syncope. An annual physical exam with his primary care provider four months ago provided him with a “clean bill of health.”
His surgical history includes an open reduction and internal fixation of a high ankle fracture, sustained while playing football in college.
The patient is married and has two children, both of whom are in good health. Family history is positive for hypertension, type 2 diabetes, and endometrial cancer. He has never smoked cigarettes and denies illicit drug use aside from trying marijuana in college. He rarely consumes alcohol (just at social events). He is not taking any medications and has no known drug allergies.
The review of systems is significant for a recent (now resolved) upper respiratory illness. He denies any changes in bowel or bladder function, as well as any endocrine, neurologic, or constitutional symptoms.
Vital signs include a blood pressure of 108/64 mm Hg; pulse, 70 beats/min; and respiratory rate, 12 breaths/min-1. His height is 76 in and his weight, 204 lb. Since this is a screening event and not a standard appointment, a complete physical exam is not performed.
The patient’s ECG shows a ventricular rate of 66 beats/min; PR interval, 266 ms; QRS duration, 98 ms; QT/QTc interval, 410/429 ms; P axis, 26°; R axis, –6°; and T axis, 43°. What is your interpretation?
Total Eclipse of the Heart
ANSWER
The correct interpretation includes sinus rhythm with complete heart block and a junctional rhythm. Normal sinus rhythm is evidenced by normal-appearing P waves at a rate of about 66 beats/min, although there is some respiratory variation. There is no correlation of the P waves to the QRS complex. A junctional rhythm is diagnosed based on narrow QRS complexes of normal duration (82 ms). The patient underwent implantation of a dual-chamber pacemaker and had a complete recovery.
ANSWER
The correct interpretation includes sinus rhythm with complete heart block and a junctional rhythm. Normal sinus rhythm is evidenced by normal-appearing P waves at a rate of about 66 beats/min, although there is some respiratory variation. There is no correlation of the P waves to the QRS complex. A junctional rhythm is diagnosed based on narrow QRS complexes of normal duration (82 ms). The patient underwent implantation of a dual-chamber pacemaker and had a complete recovery.
ANSWER
The correct interpretation includes sinus rhythm with complete heart block and a junctional rhythm. Normal sinus rhythm is evidenced by normal-appearing P waves at a rate of about 66 beats/min, although there is some respiratory variation. There is no correlation of the P waves to the QRS complex. A junctional rhythm is diagnosed based on narrow QRS complexes of normal duration (82 ms). The patient underwent implantation of a dual-chamber pacemaker and had a complete recovery.
For the past two months, a 72-year-old man has been experiencing dyspnea on exertion “off and on.” In the past three days, this shortness of breath has been more consistent.
When his son drops by to check on him, the father mentions the problem, noting that although he’s usually quite active, he hasn’t “had the stamina” to finish his current woodworking project. The son, a paramedic, checks his father’s pulse; it is regular, but the rate is below 40 beats/min. The son decides to bring him to the emergency department for evaluation.
His medical history is remarkable for hypertension, gout, and cholelithiasis. He underwent a right orchiectomy secondary to trauma in the remote past and had bilateral total knee replacements four years ago. Since the latter procedure, he has been extremely active; prior to his current complaint, he walked three miles each day.
The patient, a retired minister, lost his wife to cancer four years ago and now lives at home alone. He has four sons—one of whom visits twice a week—and two daughters, all of whom are in good health. He has never smoked and only drinks a glass of wine on holidays.
His current medications include metoprolol XL (25 mg/d) for hypertension and acetaminophen as needed for arthritic joint pain. He denies missing or doubling his medication doses. He is allergic to sulfa, which causes an anaphylactic reaction with significant airway narrowing.
The patient wears corrective lenses and hearing aids. He denies recent changes in bowel or bladder function, extreme temperature changes, productive cough, or constitutional symptoms suggestive of indolent infection.
Vital signs include a regular pulse of 50 beats/min; blood pressure, 104/66 mm Hg; respiratory rate, 14 breaths/min-1; and temperature, 98.4°F. His height is 70 in and his weight, 172 lb.
On physical exam, you notice that the patient tires walking 20 feet from the waiting room to the exam room. Otherwise, he is in no apparent distress. He denies chest pain with exertion or dyspnea at rest. His funduscopic exam is normal, his oropharynx is normal, and he is not missing teeth. There are no carotid bruits. The lungs are clear in all fields without evidence of rales, rhonchi, or crackles.
Cardiac exam reveals a grade II/VI early systolic murmur at the left upper sternal border, which does not radiate to the carotid arteries or the back. The abdomen is scaphoid and soft with no palpable masses. Peripheral pulses are strong bilaterally in all extremities. He has evidence of osteoarthritis in his hands and feet, as well as surgical scars consistent with knee replacements. His neurologic exam is intact.
An ECG reveals a ventricular rate of 47 beats/min; no discernable PR interval; QRS duration, 82 ms; QT/QTc interval, 450/398 ms; P axis, 48°; R axis, 14°; and T axis, 26°. What is your interpretation?
The Ups and Downs of One Man’s Life
ANSWER
The correct interpretation includes normal sinus rhythm, evidence of a previous inferior MI, an anterior MI, and lateral ischemia (evidenced by ST- and T-wave abnormalities in the lateral chest leads).
Normal sinus rhythm is demonstrated by the presence of a P wave for every QRS complex and a QRS complex for every P wave, with a consistent PR interval of 72 beats/min. The Q waves in leads II, III, and aVF indicate an old inferior MI.
Progression of proximal LAD stenosis and an anterior MI is evidenced by the ST segment elevations in leads V1 to V3, and lateral ischemia is represented by ST- and T-wave abnormalities in leads V4 to V6. Note that there are also Q waves in leads V4 to V6, which suggest a previously undiagnosed lateral MI.
ANSWER
The correct interpretation includes normal sinus rhythm, evidence of a previous inferior MI, an anterior MI, and lateral ischemia (evidenced by ST- and T-wave abnormalities in the lateral chest leads).
Normal sinus rhythm is demonstrated by the presence of a P wave for every QRS complex and a QRS complex for every P wave, with a consistent PR interval of 72 beats/min. The Q waves in leads II, III, and aVF indicate an old inferior MI.
Progression of proximal LAD stenosis and an anterior MI is evidenced by the ST segment elevations in leads V1 to V3, and lateral ischemia is represented by ST- and T-wave abnormalities in leads V4 to V6. Note that there are also Q waves in leads V4 to V6, which suggest a previously undiagnosed lateral MI.
ANSWER
The correct interpretation includes normal sinus rhythm, evidence of a previous inferior MI, an anterior MI, and lateral ischemia (evidenced by ST- and T-wave abnormalities in the lateral chest leads).
Normal sinus rhythm is demonstrated by the presence of a P wave for every QRS complex and a QRS complex for every P wave, with a consistent PR interval of 72 beats/min. The Q waves in leads II, III, and aVF indicate an old inferior MI.
Progression of proximal LAD stenosis and an anterior MI is evidenced by the ST segment elevations in leads V1 to V3, and lateral ischemia is represented by ST- and T-wave abnormalities in leads V4 to V6. Note that there are also Q waves in leads V4 to V6, which suggest a previously undiagnosed lateral MI.
A 58-year-old man is concerned that his previously documented coronary atherosclerosis may be progressing. Three days ago, he experienced a dull heaviness in his chest but did not have pain, diaphoresis, shortness of breath, or dyspnea on exertion. Yesterday, he developed sharp substernal chest pain while walking uphill to his office from the parking lot. The pain subsided when he stopped to catch his breath but returned last night as he was pushing the recycling bin from his garage out to the curb. When he rested, it resolved, and he has not experienced any pain so far today.
For more than 30 years, the patient smoked 2.5 packs of cigarettes per day. At age 55, he had an inferior myocardial infarction (MI), prompting him to reduce his smoking habit to less than one pack per day. He was never able to quit completely, though, despite nicotine patches, medication, and hypnosis. For the past six months, he has been under considerable stress, as his business—an automobile parts distributorship he co-owns—filed for bankruptcy; he is now smoking heavily again (2 packs/d) as a result. He is married but separated. He drinks a six-pack of beer over the span of one week. He tried recreational marijuana while in college but denies previous or current illicit drug use.
Apart from the inferior MI and coronary atherosclerosis, the patient’s medical history is remarkable for hypertension, type 2 diabetes, and tobacco abuse. Surgical history is remarkable for a drug-eluting stent placed in the proximal left anterior descending (LAD) coronary artery, laparoscopic cholecystectomy, an amputated left fifth finger from a woodworking accident, and a childhood tonsillectomy.
His current medications include metoprolol XL, isosorbide dinitrate, amlodipine, and metformin. He has no known drug allergies but develops urticaria when chlorhexidine surgical scrub solution is used on his skin.
The review of systems is remarkable for recent weight gain (10 lb over the past two months) and a productive smoker’s cough that improves during the day. The patient denies any urinary or gastrointestinal symptoms, as well as any symptoms suggestive of diabetic neuropathy or endocrine dysfunction.
Vital signs include a blood pressure of 158/94 mm Hg; pulse, 70 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 97.4°F. His height is 67 in and his weight, 254 lb. On physical exam, you note an obese male who smells of cigarette smoke. He wears corrective lenses, and the funduscopic exam is remarkable for arteriovenous nicking.
The thyroid is normal sized without nodules. A faint carotid bruit is present in the left carotid artery. The lung fields reveal coarse rales that change but do not disappear with vigorous coughing. The cardiac exam reveals a regular rate at 70 beats/min, with a soft early diastolic murmur heard at the left lower sternal border. There are no gallops or extra heart sounds.
The abdomen is obese but soft, with no palpable masses. Old surgical scars representing port placement for laparoscopic surgery are evident. The extremities show no evidence of swelling or edema. The fingers of the right hand are stained with nicotine, and a left fifth digit is missing beyond the proximal interphalangeal joint. Peripheral pulses are strong and equal bilaterally. The neurologic exam is grossly normal, with no focal signs. The patient has good sensation in both feet.
An ECG shows a ventricular rate of 72 beats/min; PR interval, 158 ms; QRS duration, 106 ms; QT/QTc interval, 400/438 ms; P axis, 33°; R axis, 38°; T axis, –15°. What is your interpretation?
Knee Pain, Heart Strain?
ANSWER
The correct interpretation includes normal sinus rhythm with left ventricular hypertrophy (LVH) and possible left atrial enlargement. Criteria for LVH include high voltages in the limb leads (R wave in lead I and S wave in lead III ≥ 25 mm) or the precordial leads (S wave in V1 and R wave in V6 ≥ 35 mm). Left atrial enlargement and ST-T wave abnormalities are often seen with LVH. The notched P wave in lead II and biphasic P wave in V1 raise suspicion for left atrial involvement. Finally, repolarization of a hypertrophic left ventricle following systole is responsible for the tall T waves seen in leads
ANSWER
The correct interpretation includes normal sinus rhythm with left ventricular hypertrophy (LVH) and possible left atrial enlargement. Criteria for LVH include high voltages in the limb leads (R wave in lead I and S wave in lead III ≥ 25 mm) or the precordial leads (S wave in V1 and R wave in V6 ≥ 35 mm). Left atrial enlargement and ST-T wave abnormalities are often seen with LVH. The notched P wave in lead II and biphasic P wave in V1 raise suspicion for left atrial involvement. Finally, repolarization of a hypertrophic left ventricle following systole is responsible for the tall T waves seen in leads
ANSWER
The correct interpretation includes normal sinus rhythm with left ventricular hypertrophy (LVH) and possible left atrial enlargement. Criteria for LVH include high voltages in the limb leads (R wave in lead I and S wave in lead III ≥ 25 mm) or the precordial leads (S wave in V1 and R wave in V6 ≥ 35 mm). Left atrial enlargement and ST-T wave abnormalities are often seen with LVH. The notched P wave in lead II and biphasic P wave in V1 raise suspicion for left atrial involvement. Finally, repolarization of a hypertrophic left ventricle following systole is responsible for the tall T waves seen in leads
A 47-year-old man presents for preoperative exam prior to right knee arthroplasty. He twisted his knee while training for a triathlon; MRI showed a bucket handle tear of the medial meniscus.
The patient has been very active throughout his life. Medical history is remarkable for essential hypertension. He has no history of chest pain, palpitations, shortness of breath, syncope, or near-syncope.
Current medications include metoprolol XL (25 mg/d)—which he hasn’t taken in five days, since he hasn’t been able to pick up his refill—and ibuprofen (600 mg tid, prn for knee pain). He denies illicit drug use.
The patient works as an accountant and is married with two children. His parents and grandparents are all alive and well. He has never smoked tobacco but does use marijuana socially on weekends. He also has one to two glasses of wine each night.
Review of systems is noncontributory: no recent colds or flu, bowel or bladder dysfunction, or weight changes. Vital signs include a blood pressure of 138/80 mm Hg; pulse, 80 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98°F. His weight is 194 lb and his height, 75 in. Pertinent physical findings include pain on palpation of the medial aspect of the right knee and a positive McMurray sign.
Bloodwork, a chest x-ray, and an ECG are obtained. The ECG shows a ventricular rate of 79 beats/min; PR interval, 184 ms; QRS duration, 76 ms; QT/QTc intervals, 382/438 ms; P axis, 48°; R axis, –29°; and T axis, 33°. What is your interpretation of this ECG?
Can His Heart Handle a Hip Operation?
ANSWER
The ECG shows evidence of sinus rhythm, left ventricular hypertrophy, and a prolonged QT interval. Although it may be tempting to label the RR’ in lead V1 as right bundle branch block, recall that bundle branch block occurs with a QRS duration > 120 ms, which is not present here.
Left ventricular hypertrophy is demonstrated by high voltages in the precordial leads (S in lead V1 and R in lead V5 or V6 ≥ 35 mm); compare this with the ECG in the May issue of Clinician Reviews (2017;27(5):9, 13). A prolonged QT interval is suggested by a QTc interval of 500 m
The patient’s family history of sudden cardiac death makes these findings particularly concerning; genetic workup should be considered for both the patient and his children.
ANSWER
The ECG shows evidence of sinus rhythm, left ventricular hypertrophy, and a prolonged QT interval. Although it may be tempting to label the RR’ in lead V1 as right bundle branch block, recall that bundle branch block occurs with a QRS duration > 120 ms, which is not present here.
Left ventricular hypertrophy is demonstrated by high voltages in the precordial leads (S in lead V1 and R in lead V5 or V6 ≥ 35 mm); compare this with the ECG in the May issue of Clinician Reviews (2017;27(5):9, 13). A prolonged QT interval is suggested by a QTc interval of 500 m
The patient’s family history of sudden cardiac death makes these findings particularly concerning; genetic workup should be considered for both the patient and his children.
ANSWER
The ECG shows evidence of sinus rhythm, left ventricular hypertrophy, and a prolonged QT interval. Although it may be tempting to label the RR’ in lead V1 as right bundle branch block, recall that bundle branch block occurs with a QRS duration > 120 ms, which is not present here.
Left ventricular hypertrophy is demonstrated by high voltages in the precordial leads (S in lead V1 and R in lead V5 or V6 ≥ 35 mm); compare this with the ECG in the May issue of Clinician Reviews (2017;27(5):9, 13). A prolonged QT interval is suggested by a QTc interval of 500 m
The patient’s family history of sudden cardiac death makes these findings particularly concerning; genetic workup should be considered for both the patient and his children.
For the past three years, a now 62-year-old man has had pain in his left hip. His orthopedic surgeon recommends replacement, so he presents for preoperative assessment.
He has no history of cardiac disease but does have osteoarthritis, obesity, type 2 diabetes, hypertension, and hyperlipidemia. His surgical history is remarkable for a cholecystectomy performed when he was 48.
His medication list includes lisinopril, metoprolol, metformin, glyburide, naproxen, and atorvastatin. He is allergic to sulfa, which has caused anaphylaxis in the past.
The patient works as the warehouse supervisor of a local home improvement store. He is married with three adult children. His brother and uncle both succumbed to sudden cardiac death in their mid-40s. His mother died of a stroke, and his father of a myocardial infarction.
He reports joint pain consistent with osteoarthritis, occasional constipation, and urinary hesitancy. He is hard of hearing, wears corrective lenses, and walks with a limp.
Vital signs include a blood pressure of 148/88 mm Hg; pulse, 83 beats/min; respiratory rate, 12 breaths/min-1; and temperature, 99°F. His weight is 254 lb and his height, 69 in.
Physical exam reveals an obese man in no acute distress. Weber exam lateralizes to the left side. Dentition is in good repair, and his Mallampati score is II. The thyroid is normal, and there is no jugular venous distention. The lungs are clear bilaterally. The cardiac exam reveals a normal rhythm with a grade II/VI early systolic murmur best heard at the left upper sternal border. There are no extra heart sounds or rubs.
The abdomen is obese, with a well-healed surgical scar in the right upper quadrant. There are no masses. Peripheral pulses are strong bilaterally. There is no peripheral edema, and there are no lesions on either foot. Range of motion in the left hip is significantly limited due to pain.
An ECG reveals a ventricular rate of 83 beats/min; PR interval, 110 ms; QRS duration, 102 ms; QT/QTc interval, 426/500 ms; P axis, 4°; R axis, 5°; T axis, –21°. What is your interpretation?