User login
Let’s Dance: A Holistic Approach to Treating Veterans With Posttraumatic Stress Disorder
Dance holds value as a cathartic, therapeutic act.1 Dance and movement therapies may help reduce symptoms of several medical conditions and aid overall motor functioning. Studies have shown that they have been used to improve gait and balance in patients with Parkinson disease.2,3
Many theorists believe in the psychological healing power of dance/movement therapies, and researchers have begun to examine the ability of these therapies to enhance well-being and quality of life. Their findings suggest that dance fosters a sense of well-being, community, mastery, and joy.3-8 Bräuninger found that a 10-week dance/movement intervention reduced stress and improved social relations, general life satisfaction, and physical and psychological health.9 Other research has shown that subjective well-being is maintained through dance in elderly adults.10,11
Dance/movement also has been found helpful in reducing symptoms associated with several psychiatric conditions. Kline and colleagues reported that movement therapy reduced anxiety in populations with severe mental illness.12 Koch and colleagues found larger reductions on depression measures and higher vitality ratings in a dance intervention group compared with music-only and exercise groups.13 An approach integrating yoga and dance/movement was found to improve stress-management skills in people affected by several mental illnesses.14
Compared with the amount of data demonstrating that dance and movement are helpful treatment modalities for psychiatric conditions, there is relatively little empirical evidence that dance or movement is effective in treating posttraumatic stress disorder (PTSD). This is particularly surprising given the somatic or bodily nature of PTSD. Traumatic events trigger significant bodily reactions—flight, fight, or freeze reactions—and PTSD involves reexperiencing bodily sensations, such as hypervigilance, agitation, and elevated arousal.15 Although dance/movement has consistently been used to treat PTSD, the evidence for its effectiveness comes mainly from case studies.16 Further empirical studies are needed to determine whether dance/movement therapies are effective in treating PTSD.
Recently, as part of the VHA patient-centered, innovative care initiative, efforts have been made to augment treating disease with improving wellness and health. For example, the VA Greater Los Angeles Healthcare System (VAGLAHS) has supported Dance for Veterans (DFV), a dance/movement program that uses movement, creativity, relaxation, and social cohesion to treat veterans with serious mental illnesses. In a recent VAGLAHS study of the effect of DFV on patients with chronic schizophrenia, bipolar disorder, major depression, PTSD, and other serious mental illnesses, Wilbur and colleagues found a 25% decrease in stress, self-rated at the beginning and end of each class; in addition, veterans indicated they received long-term benefits from taking the class.17
This pilot study investigated the effectiveness of DFV as an adjunctive treatment for PTSD. The goal of the study was to assess whether the dance class helped reduce stress symptoms in veterans diagnosed with PTSD. As rates of PTSD are much higher in veterans than in the general population, the VA has taken particular interest in the diagnosis and has prioritized treatment of this disorder.18
Toward that end, the VA began a wide-scale national dissemination of 2 empirically validated PTSD-specific treatments: prolonged exposure therapy and cognitive processing therapy. These evidence-based therapies produce clinically significant reductions in PTSD symptoms among veterans.19,20 Nevertheless, concern exists about the dropout rates and tolerability of these manualized trauma-focused treatments.19,21 Patient-centered, integrative treatments are considered less demanding and more enjoyable, but there is little evidence of their effectiveness in PTSD treatment. The VA Los Angeles Ambulatory Care Center (LAACC) had been using DFV as an adjunct treatment for veterans diagnosed with PTSD. This pilot study examined whether participating in the program reduced veterans’ stress levels.
Methods
Development of DFV was a collaborative effort of members of the department of psychiatry at VAGLAHS, dancers in the community, and graduate students in the department of World Arts and Cultures/Dance at the University of California, Los Angeles (UCLA). The first class, in January 2011, was offered to patients in the Psychosocial Rehabilitation and Recovery Program at the West Los Angeles campus of VAGLAHS. The program quickly spread to LAACC, the Sepulveda Ambulatory Care Center, the East Los Angeles Clinic, and other VAGLAHS campuses.
The goals of DFV were to introduce techniques for stress management, enhance participants’ commitment to self-worth, increase participants’ faith in their physical capabilities, encourage focus and self-discipline, build confidence, have participants discover the value of learning new skills, challenge participants to use a variety of learning styles (eg, kinesthetic, aural, musical, visual), create opportunities for active watching and listening, decrease feelings of isolation, improve group (social) and personal awareness, cultivate expressive and emotional range, develop group trust, and improve large and small muscle coordination.22
Class Format
The DFV classes were standardized, and each week followed a consistent structure. Dance for Veterans is a 1-hour class that begins with a greeting and an expression of gratitude as represented by movements developed by individual class members. After listening to an introduction, the seated participants perform yogalike stretches that promote relaxation and improve flexibility. The stretches are followed by rhythm games. Participants repeat and change rhythms to the sounds of upbeat songs, thereby enhancing their observation and listening skills, creativity, and sense of mastery. Then, in Brain Dance, the middle part of the class, memory and coordination are challenged as participants learn a 7-part movement progression.23 Last is a group creative exploration call-and-response activity, usually a game in which the group coordinates participants’ names with their specific individual movements. Each participant says his or her name and creates an individual movement to represent himself or herself; the group then echoes that participant’s name and movement. This activity fosters group cohesion and creativity while improving attention, memory, and a sense of self-worth.
Instructor Training
The 12-week course of DFV classes was led by Dr. Steinberg-Oren and Dr. Krasnova as part of the LAACC general mental health program. The instructors received intensive training in DFV implementation from Sarah Wilbur, a doctoral student in the UCLA department of World Arts and Cultures/Dance and one of the founders of DFV. Training involved written materials and a half-day retreat. Ms. Wilbur modeled the class for 8 weeks. Then she observed the teachers and provided corrective feedback for another 4 weeks. After the 12-week training period, Ms. Wilbur attended class periodically to monitor how closely the instructors were following the prescribed class format and to provide helpful suggestions and new exercises.
Participants
Veterans receiving outpatient psychiatric care for PTSD at LAACC were recruited for the DFV class. They had undergone a thorough psychiatric interview and been found to meet the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM) criteria for PTSD. All underwent physical screening by a primary care provider to rule out preexisting medical conditions that would contraindicate taking the class. Participation was voluntary. Data analysis was approved by the institutional review board of VAGLAHCS.
Data Collection
Sixty-one veterans entered the class on a rolling basis from August 2012 to November 2014. At the participants first class, they completed a demographic questionnaire. For each of the first 12 sessions attended, they were asked to complete the State-Trait Anxiety Inventory (STAI) form Y before and immediately after class.24 The STAI is a self-report questionnaire that measures short-term state anxiety and long-term trait anxiety as characterized by tension, apprehension, nervousness, and worry. It lists the same 20 items twice, first for state anxiety and then for trait anxiety. This valid and reliable measure of generalized anxiety, which has been used in hundreds of research studies, has test–retest intervals ranging from 1 hour to more than 3 months.24,25 Veterans in the study were also asked to provide qualitative feedback on any mood or sense-of-self changes experienced from the time they entered class to once it was completed.
For data analysis, a final sample of 20 veterans was selected. These veterans had completed at least 12 preclass and postclass STAI ratings within the 4-month period. The other 41 veterans in the study were not included in the data analysis because of inconsistent attendance, tardiness, or leaving class without completing a questionnaire. Further, because a large amount of STAI trait data was missing, only state items were analyzed. The data of the veterans who completed their ratings were double-entered to minimize recording errors.
Of the 20 completers (all men), 7 (35%) were African American, 7 (35%) were Hispanic, 5 (25%) were white, and 1 (5%) declined to report race. Completers’ ages ranged from the 40s to the late 70s; 40% (the largest grouping) were between ages 60 and 69 years. Noncompleters’ demographic data were comparable. Of the 41 noncompleters, 14 (34%) were African American, 15 (37%) were Hispanic, 8 (19%) were white, and 4 (10%) were Asian or Pacific Islander. Noncompleters’ ages also ranged from the 40s to the late 70s, with the largest grouping (58%) between ages 60 and 69 years. Thus, the authors did not find any significant differences between completers and noncompleters.
Results
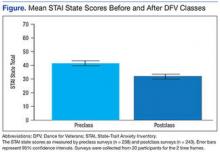
A mixed-effects linear model was used to assess whether participation length (in weeks), testing time (preclass vs postclass), or the interaction of these two variables were significant predictors of state anxiety as measured by STAI. This model included a random intercept by participant to account for differences in baseline stress levels. Analyses revealed a significant main effect of testing time on STAI state scores, t(458) = 7.48, P < .0001, such that class participation appeared to be associated with a mean decrease of 11 points on the state scale (Figure). However, participation length was not a significant predictor of STAI state scores, t(458) = 1.20, P = .233, and there was no interaction effect, t(458) = –0.57, P = .567.
Qualitative Results
Study participants unanimously reported improvements in outlook, well-being, mood, sense of well-being, and interpersonal relationships as a result of taking the DFV class. The most commonly reported preclass–postclass change was an increased sense of camaraderie and belonging. Many participants also expressed reductions in anger and isolation as well as an increase in self/other acceptance. Participants’ comments about the DFV class included, “It makes me forget about everything, and I enjoy myself.” “It relaxes me, makes me smile.” “I’ve made new friends.” “When I came here and tried this group, I felt very nervous. But I came over and over. I am so much more at ease.” “I come to class upset, and I leave with a smile on my face.” “I enjoy the camaraderie. I feel I am part of something.” “The class is helping me by body movement: moving my arms and legs—my attitude just changes.” “It’s a lot of fun!”
Discussion
This hypothesis-generating study examined whether an adjunctive, holistic intervention (dance class) could reduce stress in veterans with PTSD. Results showed significant reductions in state stress levels after DFV class participation. The finding of a significant effect of short-term reduction in state stress levels corroborates the findings from Wilbur and colleagues but with use of a comprehensive, reliable, well-validated measure of stress.17,24,25 This study’s qualitative results are also consistent with the prior qualitative data suggesting improvements in social connection and sense of well-being.
Some experts believe that PTSD-associated symptoms are fairly intractable and that trauma-focused treatments are required to reduce symptoms and promote a sense of well-being. This study did not show sustained reductions in stress levels across class sessions. Nevertheless, the significant state stress reductions that occurred after class suggest that this dance/movement intervention is a helpful adjunctive treatment for enhancing well-being, at least temporarily, in veterans with PTSD. The findings also suggest that veterans can benefit from a single session and need not attend class regularly to see results. Thus, DFV shows promise even on a drop-in basis. Overall, the results of this study provide further impetus to develop and provide more holistic, arts-based programs for veterans diagnosed with PTSD.
Study Limitations
At the beginning of this study, the authors did not expect strong participation of male veterans in a dance class. Surprisingly, 61 veterans enrolled over a period of 2 years 3 months. Nevertheless, the research sample was small, as empirical difficulties were encountered secondary to veterans’ inconsistent attendance and failure to complete ratings in a consistent and timely manner. Therefore, the sample may not have been representative. Research is needed to validate and expand the findings of this study.
Another methodologic concern was lack of a control group. Future studies might use a no-intervention control group and/or comparison groups, including support, meditation, and trauma-focused groups. In addition, veterans were not blinded to the intervention, and the STAI is a self-report survey with face-valid items. Thus, participants may have tried to please the instructors, bringing into question how much social desirability may have accounted for the reductions in stress levels.
The authors also did not examine confounding variables with regard to additional mental health treatments. It would have been helpful to address whether stress reductions were larger for veterans who were also receiving psychiatric medications and/or participating in other mental health groups or individual psychotherapies. The effect of comorbid diagnoses on the reduction in state stress levels also was not examined. Last, the authors did not investigate actual PTSD symptoms (eg, flashbacks, nightmares, hypervigilance, and avoidance). Further studies are needed to measure reductions on the PTSD Checklist for DSM 5 or on other empirical measures of PTSD as a consequence of this class in order to examine its effectiveness in reducing PTSD symptoms.
Qualitative responses from the veterans suggested that DFV promoted quality-of-life and well-being improvements. It would be helpful to assess this quantitatively through control or comparison group studies using measurements that minimize face validity. To understand the mechanism by which this class is effective, research also needs to examine what class-related factors are most effective in promoting positive change. The qualitative data provide glimpses into these factors, but empirical investigation could provide substantive proof of what specific factors are therapeutic.
Conclusion
The VHA has introduced several integrative adjunctive PTSD treatments, including dance, tai chi, mindfulness meditation, breathing/stretching/relaxation, yoga, healing touch, and others with the goal of maximizing veterans’ physical and psychological wellness. Although it seems unlikely that integrative once-a-week treatments lead to sustained reductions in PTSD and other serious psychiatric conditions, it is possible that participating in DFV classes more regularly, as part of adjunctive treatment, could promote a sustained sense of well-being, self-compassion, self-confidence, and sense of belonging. The question still remains whether such programs are effective in promoting well-being. The present study was not conclusive enough to substantiate that claim, but it represents a small step (a dance step) in the right direction, toward a holistic, creative, and well-rounded approach to the treatment of PTSD in veterans.
Acknowledgments
The authors thank the many people involved in Dance for Veterans. Robert Rubin, MD, had the creative foresight to assemble the program; Donna Ames, MD, invited her coauthors to undergo training and provided them with research support; Sarah Wilbur, PhD, (program in Culture and Performance, Department of World Arts and Cultures/Dance, University of California, Los Angeles) developed the class and handbook as well as showed the authors how to run it; Sandra Robertson, RN, MSN, PH-CNS, (principal investigator, Integrative Health and Healing Project, VA T21 Center of Innovation Grant for Patient-Centered Care) provided the funding and initiative to develop and implement the class; and (Christine Suarez Suarez Dance Theatre, Santa Monica, California) developed the class and the handbook and trained instructors.
The authors also thank all the VAGLAHS veterans and staff for their help with the class—especially Andrea Serafin, LCSW; Rosie Dominguez, LCSW; Retha de Johnette, LCSW; and Donna Ames, MD, all part of the Psychosocial Rehabilitation and Recovery Programs; Dana Melching, LCSW, Mental Health Intensive Case Management; and Vanessa Baumann, PhD (Vet Center).
1. Levy FJ. Dance/Movement Therapy: A Healing Art. Reston, VA: American Alliance for Health, Physical Education, Recreation, and Dance; 1992.
2. Marigold DS, Misiaszek JE. Whole-body responses: neural control and implications for rehabilitation and fall prevention. Neuroscientist. 2009;15(1):36-46.
3. Hackney ME, Kantorovich S, Levin R, Earhart GM. Effects of tango on functional mobility in Parkinson's disease: a preliminary study. J Neurol Phys Ther. 2007;31(4):173-179.
4. Ravelin T, Kylmä J, Korhonen T. Dance in mental health nursing: a hybrid concept analysis. Issues Ment Health Nurs. 2006;27(3):307-317.
5. Hackney ME, Earhart GM. Effects of dance on gait and balance in Parkinson's disease: a comparison of partnered and nonpartnered dance movement. Neurorehabil Neural Repair. 2010;24(4):384-392.
6. Heiberger L, Maurer C, Amtage F, et al. Impact of a weekly dance class on the functional mobility and on the quality of life of individuals with Parkinson's disease. Front Aging Neurosci. 2011;3:14.
7. Houston S, McGill A. A mixed-methods study into ballet for people living with Parkinson's. Arts Health. 2013;5(2):103-119.
8. Westheimer O. Why dance for Parkinson's disease. Top Geriatr Rehabil. 2008;24(2):127-140.
9. Bräuninger I. Dance movement therapy group intervention in stress treatment: a randomized controlled trial (RCT). Arts Psychother. 2012;39(5):443-450.
10. Kattenstroth, JC, Kalisch T, Holt S, Tegenthoff M, Dinse HR. Six months of dance intervention enhances postural, sensorimotor, and cognitive performance in elderly without affecting cardio-respiratory functions. Front Aging Neurosci. 2013;5:5.
11. Kattenstroth J-C, Kolankowska I, Kalisch T, Dinse HR. Superior sensory, motor, and cognitive performance in elderly individuals with multi-year dancing activities. Front Aging Neurosci. 2010;2:31.
12. Kline F, Burgoyne RW, Staples F, Moredock P, Snyder V, Ioerger M. A report on the use of movement therapy for chronic, severely disabled outpatients. Arts Psychother. 1977;4(4-5):181-183.
13. Koch SC, Morlinghaus K, Fuchs T. The joy dance: specific effects of a single dance intervention on psychiatric patients with depression. Arts Psychother. 2007;34(4):340-349.
14. Barton EJ. Movement and mindfulness: a formative evaluation of a dance/movement and yoga therapy program with participants experiencing severe mental illness. Am J Dance Ther. 2011;33(2):157-181.
15. van der Kolk BA, McFarlane AC, Weisaeth L, eds. Traumatic Stress: The Effects of Overwhelming Experience on Mind, Body, and Society. New York, NY: Guilford Press; 1996.
16. Foa EB, Keane TM, Friedman MJ, Cohen JA, eds. Effective Treatments for PTSD: Practice Guidelines From the International Society for Traumatic Stress Studies. 2nd ed. New York, NY: Guilford Press; 2009.
17. Wilbur S, Meyer HB, Baker MR, et al. Dance for Veterans: a complementary health program for veterans with serious mental illness. Arts Health. 2015;7(2):96-108.
18. Gradus JL. Epidemiology of PTSD. U.S. Department of Veterans Affairs, PTSD: National Center for PTSD website. http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. Published January 30, 2014. Accessed August 20, 2015.
19. Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, Karlin BE. Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. JAMA Psychiatry. 2013;70(9):949-955.
20. Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J Consult Clin Psychol. 2006;74(5):898-907.
21. Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71(2):134-168.
22. Suarez CA, Wilbur S, Smiarowski K, Rubin RT, Ames D. Dance for Veterans: Music, Movement & Rhythm Manual for Instruction. 2nd ed. Publisher unknown; 2014.
23. Gilbert AG, Gilbert BA, Rossano A. Brain-Compatible Dance Education. Reston, VA: National Dance Association; 2006.
24. Spielberger C. Manual for the State-Trait Anxiety Inventory. Rev ed. Palo Alto, CA: Consulting Psychologists Press; 1983.
25. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011;63(suppl 11):S467-S472.
Dance holds value as a cathartic, therapeutic act.1 Dance and movement therapies may help reduce symptoms of several medical conditions and aid overall motor functioning. Studies have shown that they have been used to improve gait and balance in patients with Parkinson disease.2,3
Many theorists believe in the psychological healing power of dance/movement therapies, and researchers have begun to examine the ability of these therapies to enhance well-being and quality of life. Their findings suggest that dance fosters a sense of well-being, community, mastery, and joy.3-8 Bräuninger found that a 10-week dance/movement intervention reduced stress and improved social relations, general life satisfaction, and physical and psychological health.9 Other research has shown that subjective well-being is maintained through dance in elderly adults.10,11
Dance/movement also has been found helpful in reducing symptoms associated with several psychiatric conditions. Kline and colleagues reported that movement therapy reduced anxiety in populations with severe mental illness.12 Koch and colleagues found larger reductions on depression measures and higher vitality ratings in a dance intervention group compared with music-only and exercise groups.13 An approach integrating yoga and dance/movement was found to improve stress-management skills in people affected by several mental illnesses.14
Compared with the amount of data demonstrating that dance and movement are helpful treatment modalities for psychiatric conditions, there is relatively little empirical evidence that dance or movement is effective in treating posttraumatic stress disorder (PTSD). This is particularly surprising given the somatic or bodily nature of PTSD. Traumatic events trigger significant bodily reactions—flight, fight, or freeze reactions—and PTSD involves reexperiencing bodily sensations, such as hypervigilance, agitation, and elevated arousal.15 Although dance/movement has consistently been used to treat PTSD, the evidence for its effectiveness comes mainly from case studies.16 Further empirical studies are needed to determine whether dance/movement therapies are effective in treating PTSD.
Recently, as part of the VHA patient-centered, innovative care initiative, efforts have been made to augment treating disease with improving wellness and health. For example, the VA Greater Los Angeles Healthcare System (VAGLAHS) has supported Dance for Veterans (DFV), a dance/movement program that uses movement, creativity, relaxation, and social cohesion to treat veterans with serious mental illnesses. In a recent VAGLAHS study of the effect of DFV on patients with chronic schizophrenia, bipolar disorder, major depression, PTSD, and other serious mental illnesses, Wilbur and colleagues found a 25% decrease in stress, self-rated at the beginning and end of each class; in addition, veterans indicated they received long-term benefits from taking the class.17
This pilot study investigated the effectiveness of DFV as an adjunctive treatment for PTSD. The goal of the study was to assess whether the dance class helped reduce stress symptoms in veterans diagnosed with PTSD. As rates of PTSD are much higher in veterans than in the general population, the VA has taken particular interest in the diagnosis and has prioritized treatment of this disorder.18
Toward that end, the VA began a wide-scale national dissemination of 2 empirically validated PTSD-specific treatments: prolonged exposure therapy and cognitive processing therapy. These evidence-based therapies produce clinically significant reductions in PTSD symptoms among veterans.19,20 Nevertheless, concern exists about the dropout rates and tolerability of these manualized trauma-focused treatments.19,21 Patient-centered, integrative treatments are considered less demanding and more enjoyable, but there is little evidence of their effectiveness in PTSD treatment. The VA Los Angeles Ambulatory Care Center (LAACC) had been using DFV as an adjunct treatment for veterans diagnosed with PTSD. This pilot study examined whether participating in the program reduced veterans’ stress levels.
Methods
Development of DFV was a collaborative effort of members of the department of psychiatry at VAGLAHS, dancers in the community, and graduate students in the department of World Arts and Cultures/Dance at the University of California, Los Angeles (UCLA). The first class, in January 2011, was offered to patients in the Psychosocial Rehabilitation and Recovery Program at the West Los Angeles campus of VAGLAHS. The program quickly spread to LAACC, the Sepulveda Ambulatory Care Center, the East Los Angeles Clinic, and other VAGLAHS campuses.
The goals of DFV were to introduce techniques for stress management, enhance participants’ commitment to self-worth, increase participants’ faith in their physical capabilities, encourage focus and self-discipline, build confidence, have participants discover the value of learning new skills, challenge participants to use a variety of learning styles (eg, kinesthetic, aural, musical, visual), create opportunities for active watching and listening, decrease feelings of isolation, improve group (social) and personal awareness, cultivate expressive and emotional range, develop group trust, and improve large and small muscle coordination.22
Class Format
The DFV classes were standardized, and each week followed a consistent structure. Dance for Veterans is a 1-hour class that begins with a greeting and an expression of gratitude as represented by movements developed by individual class members. After listening to an introduction, the seated participants perform yogalike stretches that promote relaxation and improve flexibility. The stretches are followed by rhythm games. Participants repeat and change rhythms to the sounds of upbeat songs, thereby enhancing their observation and listening skills, creativity, and sense of mastery. Then, in Brain Dance, the middle part of the class, memory and coordination are challenged as participants learn a 7-part movement progression.23 Last is a group creative exploration call-and-response activity, usually a game in which the group coordinates participants’ names with their specific individual movements. Each participant says his or her name and creates an individual movement to represent himself or herself; the group then echoes that participant’s name and movement. This activity fosters group cohesion and creativity while improving attention, memory, and a sense of self-worth.
Instructor Training
The 12-week course of DFV classes was led by Dr. Steinberg-Oren and Dr. Krasnova as part of the LAACC general mental health program. The instructors received intensive training in DFV implementation from Sarah Wilbur, a doctoral student in the UCLA department of World Arts and Cultures/Dance and one of the founders of DFV. Training involved written materials and a half-day retreat. Ms. Wilbur modeled the class for 8 weeks. Then she observed the teachers and provided corrective feedback for another 4 weeks. After the 12-week training period, Ms. Wilbur attended class periodically to monitor how closely the instructors were following the prescribed class format and to provide helpful suggestions and new exercises.
Participants
Veterans receiving outpatient psychiatric care for PTSD at LAACC were recruited for the DFV class. They had undergone a thorough psychiatric interview and been found to meet the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM) criteria for PTSD. All underwent physical screening by a primary care provider to rule out preexisting medical conditions that would contraindicate taking the class. Participation was voluntary. Data analysis was approved by the institutional review board of VAGLAHCS.
Data Collection
Sixty-one veterans entered the class on a rolling basis from August 2012 to November 2014. At the participants first class, they completed a demographic questionnaire. For each of the first 12 sessions attended, they were asked to complete the State-Trait Anxiety Inventory (STAI) form Y before and immediately after class.24 The STAI is a self-report questionnaire that measures short-term state anxiety and long-term trait anxiety as characterized by tension, apprehension, nervousness, and worry. It lists the same 20 items twice, first for state anxiety and then for trait anxiety. This valid and reliable measure of generalized anxiety, which has been used in hundreds of research studies, has test–retest intervals ranging from 1 hour to more than 3 months.24,25 Veterans in the study were also asked to provide qualitative feedback on any mood or sense-of-self changes experienced from the time they entered class to once it was completed.
For data analysis, a final sample of 20 veterans was selected. These veterans had completed at least 12 preclass and postclass STAI ratings within the 4-month period. The other 41 veterans in the study were not included in the data analysis because of inconsistent attendance, tardiness, or leaving class without completing a questionnaire. Further, because a large amount of STAI trait data was missing, only state items were analyzed. The data of the veterans who completed their ratings were double-entered to minimize recording errors.
Of the 20 completers (all men), 7 (35%) were African American, 7 (35%) were Hispanic, 5 (25%) were white, and 1 (5%) declined to report race. Completers’ ages ranged from the 40s to the late 70s; 40% (the largest grouping) were between ages 60 and 69 years. Noncompleters’ demographic data were comparable. Of the 41 noncompleters, 14 (34%) were African American, 15 (37%) were Hispanic, 8 (19%) were white, and 4 (10%) were Asian or Pacific Islander. Noncompleters’ ages also ranged from the 40s to the late 70s, with the largest grouping (58%) between ages 60 and 69 years. Thus, the authors did not find any significant differences between completers and noncompleters.
Results
A mixed-effects linear model was used to assess whether participation length (in weeks), testing time (preclass vs postclass), or the interaction of these two variables were significant predictors of state anxiety as measured by STAI. This model included a random intercept by participant to account for differences in baseline stress levels. Analyses revealed a significant main effect of testing time on STAI state scores, t(458) = 7.48, P < .0001, such that class participation appeared to be associated with a mean decrease of 11 points on the state scale (Figure). However, participation length was not a significant predictor of STAI state scores, t(458) = 1.20, P = .233, and there was no interaction effect, t(458) = –0.57, P = .567.
Qualitative Results
Study participants unanimously reported improvements in outlook, well-being, mood, sense of well-being, and interpersonal relationships as a result of taking the DFV class. The most commonly reported preclass–postclass change was an increased sense of camaraderie and belonging. Many participants also expressed reductions in anger and isolation as well as an increase in self/other acceptance. Participants’ comments about the DFV class included, “It makes me forget about everything, and I enjoy myself.” “It relaxes me, makes me smile.” “I’ve made new friends.” “When I came here and tried this group, I felt very nervous. But I came over and over. I am so much more at ease.” “I come to class upset, and I leave with a smile on my face.” “I enjoy the camaraderie. I feel I am part of something.” “The class is helping me by body movement: moving my arms and legs—my attitude just changes.” “It’s a lot of fun!”
Discussion
This hypothesis-generating study examined whether an adjunctive, holistic intervention (dance class) could reduce stress in veterans with PTSD. Results showed significant reductions in state stress levels after DFV class participation. The finding of a significant effect of short-term reduction in state stress levels corroborates the findings from Wilbur and colleagues but with use of a comprehensive, reliable, well-validated measure of stress.17,24,25 This study’s qualitative results are also consistent with the prior qualitative data suggesting improvements in social connection and sense of well-being.
Some experts believe that PTSD-associated symptoms are fairly intractable and that trauma-focused treatments are required to reduce symptoms and promote a sense of well-being. This study did not show sustained reductions in stress levels across class sessions. Nevertheless, the significant state stress reductions that occurred after class suggest that this dance/movement intervention is a helpful adjunctive treatment for enhancing well-being, at least temporarily, in veterans with PTSD. The findings also suggest that veterans can benefit from a single session and need not attend class regularly to see results. Thus, DFV shows promise even on a drop-in basis. Overall, the results of this study provide further impetus to develop and provide more holistic, arts-based programs for veterans diagnosed with PTSD.
Study Limitations
At the beginning of this study, the authors did not expect strong participation of male veterans in a dance class. Surprisingly, 61 veterans enrolled over a period of 2 years 3 months. Nevertheless, the research sample was small, as empirical difficulties were encountered secondary to veterans’ inconsistent attendance and failure to complete ratings in a consistent and timely manner. Therefore, the sample may not have been representative. Research is needed to validate and expand the findings of this study.
Another methodologic concern was lack of a control group. Future studies might use a no-intervention control group and/or comparison groups, including support, meditation, and trauma-focused groups. In addition, veterans were not blinded to the intervention, and the STAI is a self-report survey with face-valid items. Thus, participants may have tried to please the instructors, bringing into question how much social desirability may have accounted for the reductions in stress levels.
The authors also did not examine confounding variables with regard to additional mental health treatments. It would have been helpful to address whether stress reductions were larger for veterans who were also receiving psychiatric medications and/or participating in other mental health groups or individual psychotherapies. The effect of comorbid diagnoses on the reduction in state stress levels also was not examined. Last, the authors did not investigate actual PTSD symptoms (eg, flashbacks, nightmares, hypervigilance, and avoidance). Further studies are needed to measure reductions on the PTSD Checklist for DSM 5 or on other empirical measures of PTSD as a consequence of this class in order to examine its effectiveness in reducing PTSD symptoms.
Qualitative responses from the veterans suggested that DFV promoted quality-of-life and well-being improvements. It would be helpful to assess this quantitatively through control or comparison group studies using measurements that minimize face validity. To understand the mechanism by which this class is effective, research also needs to examine what class-related factors are most effective in promoting positive change. The qualitative data provide glimpses into these factors, but empirical investigation could provide substantive proof of what specific factors are therapeutic.
Conclusion
The VHA has introduced several integrative adjunctive PTSD treatments, including dance, tai chi, mindfulness meditation, breathing/stretching/relaxation, yoga, healing touch, and others with the goal of maximizing veterans’ physical and psychological wellness. Although it seems unlikely that integrative once-a-week treatments lead to sustained reductions in PTSD and other serious psychiatric conditions, it is possible that participating in DFV classes more regularly, as part of adjunctive treatment, could promote a sustained sense of well-being, self-compassion, self-confidence, and sense of belonging. The question still remains whether such programs are effective in promoting well-being. The present study was not conclusive enough to substantiate that claim, but it represents a small step (a dance step) in the right direction, toward a holistic, creative, and well-rounded approach to the treatment of PTSD in veterans.
Acknowledgments
The authors thank the many people involved in Dance for Veterans. Robert Rubin, MD, had the creative foresight to assemble the program; Donna Ames, MD, invited her coauthors to undergo training and provided them with research support; Sarah Wilbur, PhD, (program in Culture and Performance, Department of World Arts and Cultures/Dance, University of California, Los Angeles) developed the class and handbook as well as showed the authors how to run it; Sandra Robertson, RN, MSN, PH-CNS, (principal investigator, Integrative Health and Healing Project, VA T21 Center of Innovation Grant for Patient-Centered Care) provided the funding and initiative to develop and implement the class; and (Christine Suarez Suarez Dance Theatre, Santa Monica, California) developed the class and the handbook and trained instructors.
The authors also thank all the VAGLAHS veterans and staff for their help with the class—especially Andrea Serafin, LCSW; Rosie Dominguez, LCSW; Retha de Johnette, LCSW; and Donna Ames, MD, all part of the Psychosocial Rehabilitation and Recovery Programs; Dana Melching, LCSW, Mental Health Intensive Case Management; and Vanessa Baumann, PhD (Vet Center).
Dance holds value as a cathartic, therapeutic act.1 Dance and movement therapies may help reduce symptoms of several medical conditions and aid overall motor functioning. Studies have shown that they have been used to improve gait and balance in patients with Parkinson disease.2,3
Many theorists believe in the psychological healing power of dance/movement therapies, and researchers have begun to examine the ability of these therapies to enhance well-being and quality of life. Their findings suggest that dance fosters a sense of well-being, community, mastery, and joy.3-8 Bräuninger found that a 10-week dance/movement intervention reduced stress and improved social relations, general life satisfaction, and physical and psychological health.9 Other research has shown that subjective well-being is maintained through dance in elderly adults.10,11
Dance/movement also has been found helpful in reducing symptoms associated with several psychiatric conditions. Kline and colleagues reported that movement therapy reduced anxiety in populations with severe mental illness.12 Koch and colleagues found larger reductions on depression measures and higher vitality ratings in a dance intervention group compared with music-only and exercise groups.13 An approach integrating yoga and dance/movement was found to improve stress-management skills in people affected by several mental illnesses.14
Compared with the amount of data demonstrating that dance and movement are helpful treatment modalities for psychiatric conditions, there is relatively little empirical evidence that dance or movement is effective in treating posttraumatic stress disorder (PTSD). This is particularly surprising given the somatic or bodily nature of PTSD. Traumatic events trigger significant bodily reactions—flight, fight, or freeze reactions—and PTSD involves reexperiencing bodily sensations, such as hypervigilance, agitation, and elevated arousal.15 Although dance/movement has consistently been used to treat PTSD, the evidence for its effectiveness comes mainly from case studies.16 Further empirical studies are needed to determine whether dance/movement therapies are effective in treating PTSD.
Recently, as part of the VHA patient-centered, innovative care initiative, efforts have been made to augment treating disease with improving wellness and health. For example, the VA Greater Los Angeles Healthcare System (VAGLAHS) has supported Dance for Veterans (DFV), a dance/movement program that uses movement, creativity, relaxation, and social cohesion to treat veterans with serious mental illnesses. In a recent VAGLAHS study of the effect of DFV on patients with chronic schizophrenia, bipolar disorder, major depression, PTSD, and other serious mental illnesses, Wilbur and colleagues found a 25% decrease in stress, self-rated at the beginning and end of each class; in addition, veterans indicated they received long-term benefits from taking the class.17
This pilot study investigated the effectiveness of DFV as an adjunctive treatment for PTSD. The goal of the study was to assess whether the dance class helped reduce stress symptoms in veterans diagnosed with PTSD. As rates of PTSD are much higher in veterans than in the general population, the VA has taken particular interest in the diagnosis and has prioritized treatment of this disorder.18
Toward that end, the VA began a wide-scale national dissemination of 2 empirically validated PTSD-specific treatments: prolonged exposure therapy and cognitive processing therapy. These evidence-based therapies produce clinically significant reductions in PTSD symptoms among veterans.19,20 Nevertheless, concern exists about the dropout rates and tolerability of these manualized trauma-focused treatments.19,21 Patient-centered, integrative treatments are considered less demanding and more enjoyable, but there is little evidence of their effectiveness in PTSD treatment. The VA Los Angeles Ambulatory Care Center (LAACC) had been using DFV as an adjunct treatment for veterans diagnosed with PTSD. This pilot study examined whether participating in the program reduced veterans’ stress levels.
Methods
Development of DFV was a collaborative effort of members of the department of psychiatry at VAGLAHS, dancers in the community, and graduate students in the department of World Arts and Cultures/Dance at the University of California, Los Angeles (UCLA). The first class, in January 2011, was offered to patients in the Psychosocial Rehabilitation and Recovery Program at the West Los Angeles campus of VAGLAHS. The program quickly spread to LAACC, the Sepulveda Ambulatory Care Center, the East Los Angeles Clinic, and other VAGLAHS campuses.
The goals of DFV were to introduce techniques for stress management, enhance participants’ commitment to self-worth, increase participants’ faith in their physical capabilities, encourage focus and self-discipline, build confidence, have participants discover the value of learning new skills, challenge participants to use a variety of learning styles (eg, kinesthetic, aural, musical, visual), create opportunities for active watching and listening, decrease feelings of isolation, improve group (social) and personal awareness, cultivate expressive and emotional range, develop group trust, and improve large and small muscle coordination.22
Class Format
The DFV classes were standardized, and each week followed a consistent structure. Dance for Veterans is a 1-hour class that begins with a greeting and an expression of gratitude as represented by movements developed by individual class members. After listening to an introduction, the seated participants perform yogalike stretches that promote relaxation and improve flexibility. The stretches are followed by rhythm games. Participants repeat and change rhythms to the sounds of upbeat songs, thereby enhancing their observation and listening skills, creativity, and sense of mastery. Then, in Brain Dance, the middle part of the class, memory and coordination are challenged as participants learn a 7-part movement progression.23 Last is a group creative exploration call-and-response activity, usually a game in which the group coordinates participants’ names with their specific individual movements. Each participant says his or her name and creates an individual movement to represent himself or herself; the group then echoes that participant’s name and movement. This activity fosters group cohesion and creativity while improving attention, memory, and a sense of self-worth.
Instructor Training
The 12-week course of DFV classes was led by Dr. Steinberg-Oren and Dr. Krasnova as part of the LAACC general mental health program. The instructors received intensive training in DFV implementation from Sarah Wilbur, a doctoral student in the UCLA department of World Arts and Cultures/Dance and one of the founders of DFV. Training involved written materials and a half-day retreat. Ms. Wilbur modeled the class for 8 weeks. Then she observed the teachers and provided corrective feedback for another 4 weeks. After the 12-week training period, Ms. Wilbur attended class periodically to monitor how closely the instructors were following the prescribed class format and to provide helpful suggestions and new exercises.
Participants
Veterans receiving outpatient psychiatric care for PTSD at LAACC were recruited for the DFV class. They had undergone a thorough psychiatric interview and been found to meet the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM) criteria for PTSD. All underwent physical screening by a primary care provider to rule out preexisting medical conditions that would contraindicate taking the class. Participation was voluntary. Data analysis was approved by the institutional review board of VAGLAHCS.
Data Collection
Sixty-one veterans entered the class on a rolling basis from August 2012 to November 2014. At the participants first class, they completed a demographic questionnaire. For each of the first 12 sessions attended, they were asked to complete the State-Trait Anxiety Inventory (STAI) form Y before and immediately after class.24 The STAI is a self-report questionnaire that measures short-term state anxiety and long-term trait anxiety as characterized by tension, apprehension, nervousness, and worry. It lists the same 20 items twice, first for state anxiety and then for trait anxiety. This valid and reliable measure of generalized anxiety, which has been used in hundreds of research studies, has test–retest intervals ranging from 1 hour to more than 3 months.24,25 Veterans in the study were also asked to provide qualitative feedback on any mood or sense-of-self changes experienced from the time they entered class to once it was completed.
For data analysis, a final sample of 20 veterans was selected. These veterans had completed at least 12 preclass and postclass STAI ratings within the 4-month period. The other 41 veterans in the study were not included in the data analysis because of inconsistent attendance, tardiness, or leaving class without completing a questionnaire. Further, because a large amount of STAI trait data was missing, only state items were analyzed. The data of the veterans who completed their ratings were double-entered to minimize recording errors.
Of the 20 completers (all men), 7 (35%) were African American, 7 (35%) were Hispanic, 5 (25%) were white, and 1 (5%) declined to report race. Completers’ ages ranged from the 40s to the late 70s; 40% (the largest grouping) were between ages 60 and 69 years. Noncompleters’ demographic data were comparable. Of the 41 noncompleters, 14 (34%) were African American, 15 (37%) were Hispanic, 8 (19%) were white, and 4 (10%) were Asian or Pacific Islander. Noncompleters’ ages also ranged from the 40s to the late 70s, with the largest grouping (58%) between ages 60 and 69 years. Thus, the authors did not find any significant differences between completers and noncompleters.
Results
A mixed-effects linear model was used to assess whether participation length (in weeks), testing time (preclass vs postclass), or the interaction of these two variables were significant predictors of state anxiety as measured by STAI. This model included a random intercept by participant to account for differences in baseline stress levels. Analyses revealed a significant main effect of testing time on STAI state scores, t(458) = 7.48, P < .0001, such that class participation appeared to be associated with a mean decrease of 11 points on the state scale (Figure). However, participation length was not a significant predictor of STAI state scores, t(458) = 1.20, P = .233, and there was no interaction effect, t(458) = –0.57, P = .567.
Qualitative Results
Study participants unanimously reported improvements in outlook, well-being, mood, sense of well-being, and interpersonal relationships as a result of taking the DFV class. The most commonly reported preclass–postclass change was an increased sense of camaraderie and belonging. Many participants also expressed reductions in anger and isolation as well as an increase in self/other acceptance. Participants’ comments about the DFV class included, “It makes me forget about everything, and I enjoy myself.” “It relaxes me, makes me smile.” “I’ve made new friends.” “When I came here and tried this group, I felt very nervous. But I came over and over. I am so much more at ease.” “I come to class upset, and I leave with a smile on my face.” “I enjoy the camaraderie. I feel I am part of something.” “The class is helping me by body movement: moving my arms and legs—my attitude just changes.” “It’s a lot of fun!”
Discussion
This hypothesis-generating study examined whether an adjunctive, holistic intervention (dance class) could reduce stress in veterans with PTSD. Results showed significant reductions in state stress levels after DFV class participation. The finding of a significant effect of short-term reduction in state stress levels corroborates the findings from Wilbur and colleagues but with use of a comprehensive, reliable, well-validated measure of stress.17,24,25 This study’s qualitative results are also consistent with the prior qualitative data suggesting improvements in social connection and sense of well-being.
Some experts believe that PTSD-associated symptoms are fairly intractable and that trauma-focused treatments are required to reduce symptoms and promote a sense of well-being. This study did not show sustained reductions in stress levels across class sessions. Nevertheless, the significant state stress reductions that occurred after class suggest that this dance/movement intervention is a helpful adjunctive treatment for enhancing well-being, at least temporarily, in veterans with PTSD. The findings also suggest that veterans can benefit from a single session and need not attend class regularly to see results. Thus, DFV shows promise even on a drop-in basis. Overall, the results of this study provide further impetus to develop and provide more holistic, arts-based programs for veterans diagnosed with PTSD.
Study Limitations
At the beginning of this study, the authors did not expect strong participation of male veterans in a dance class. Surprisingly, 61 veterans enrolled over a period of 2 years 3 months. Nevertheless, the research sample was small, as empirical difficulties were encountered secondary to veterans’ inconsistent attendance and failure to complete ratings in a consistent and timely manner. Therefore, the sample may not have been representative. Research is needed to validate and expand the findings of this study.
Another methodologic concern was lack of a control group. Future studies might use a no-intervention control group and/or comparison groups, including support, meditation, and trauma-focused groups. In addition, veterans were not blinded to the intervention, and the STAI is a self-report survey with face-valid items. Thus, participants may have tried to please the instructors, bringing into question how much social desirability may have accounted for the reductions in stress levels.
The authors also did not examine confounding variables with regard to additional mental health treatments. It would have been helpful to address whether stress reductions were larger for veterans who were also receiving psychiatric medications and/or participating in other mental health groups or individual psychotherapies. The effect of comorbid diagnoses on the reduction in state stress levels also was not examined. Last, the authors did not investigate actual PTSD symptoms (eg, flashbacks, nightmares, hypervigilance, and avoidance). Further studies are needed to measure reductions on the PTSD Checklist for DSM 5 or on other empirical measures of PTSD as a consequence of this class in order to examine its effectiveness in reducing PTSD symptoms.
Qualitative responses from the veterans suggested that DFV promoted quality-of-life and well-being improvements. It would be helpful to assess this quantitatively through control or comparison group studies using measurements that minimize face validity. To understand the mechanism by which this class is effective, research also needs to examine what class-related factors are most effective in promoting positive change. The qualitative data provide glimpses into these factors, but empirical investigation could provide substantive proof of what specific factors are therapeutic.
Conclusion
The VHA has introduced several integrative adjunctive PTSD treatments, including dance, tai chi, mindfulness meditation, breathing/stretching/relaxation, yoga, healing touch, and others with the goal of maximizing veterans’ physical and psychological wellness. Although it seems unlikely that integrative once-a-week treatments lead to sustained reductions in PTSD and other serious psychiatric conditions, it is possible that participating in DFV classes more regularly, as part of adjunctive treatment, could promote a sustained sense of well-being, self-compassion, self-confidence, and sense of belonging. The question still remains whether such programs are effective in promoting well-being. The present study was not conclusive enough to substantiate that claim, but it represents a small step (a dance step) in the right direction, toward a holistic, creative, and well-rounded approach to the treatment of PTSD in veterans.
Acknowledgments
The authors thank the many people involved in Dance for Veterans. Robert Rubin, MD, had the creative foresight to assemble the program; Donna Ames, MD, invited her coauthors to undergo training and provided them with research support; Sarah Wilbur, PhD, (program in Culture and Performance, Department of World Arts and Cultures/Dance, University of California, Los Angeles) developed the class and handbook as well as showed the authors how to run it; Sandra Robertson, RN, MSN, PH-CNS, (principal investigator, Integrative Health and Healing Project, VA T21 Center of Innovation Grant for Patient-Centered Care) provided the funding and initiative to develop and implement the class; and (Christine Suarez Suarez Dance Theatre, Santa Monica, California) developed the class and the handbook and trained instructors.
The authors also thank all the VAGLAHS veterans and staff for their help with the class—especially Andrea Serafin, LCSW; Rosie Dominguez, LCSW; Retha de Johnette, LCSW; and Donna Ames, MD, all part of the Psychosocial Rehabilitation and Recovery Programs; Dana Melching, LCSW, Mental Health Intensive Case Management; and Vanessa Baumann, PhD (Vet Center).
1. Levy FJ. Dance/Movement Therapy: A Healing Art. Reston, VA: American Alliance for Health, Physical Education, Recreation, and Dance; 1992.
2. Marigold DS, Misiaszek JE. Whole-body responses: neural control and implications for rehabilitation and fall prevention. Neuroscientist. 2009;15(1):36-46.
3. Hackney ME, Kantorovich S, Levin R, Earhart GM. Effects of tango on functional mobility in Parkinson's disease: a preliminary study. J Neurol Phys Ther. 2007;31(4):173-179.
4. Ravelin T, Kylmä J, Korhonen T. Dance in mental health nursing: a hybrid concept analysis. Issues Ment Health Nurs. 2006;27(3):307-317.
5. Hackney ME, Earhart GM. Effects of dance on gait and balance in Parkinson's disease: a comparison of partnered and nonpartnered dance movement. Neurorehabil Neural Repair. 2010;24(4):384-392.
6. Heiberger L, Maurer C, Amtage F, et al. Impact of a weekly dance class on the functional mobility and on the quality of life of individuals with Parkinson's disease. Front Aging Neurosci. 2011;3:14.
7. Houston S, McGill A. A mixed-methods study into ballet for people living with Parkinson's. Arts Health. 2013;5(2):103-119.
8. Westheimer O. Why dance for Parkinson's disease. Top Geriatr Rehabil. 2008;24(2):127-140.
9. Bräuninger I. Dance movement therapy group intervention in stress treatment: a randomized controlled trial (RCT). Arts Psychother. 2012;39(5):443-450.
10. Kattenstroth, JC, Kalisch T, Holt S, Tegenthoff M, Dinse HR. Six months of dance intervention enhances postural, sensorimotor, and cognitive performance in elderly without affecting cardio-respiratory functions. Front Aging Neurosci. 2013;5:5.
11. Kattenstroth J-C, Kolankowska I, Kalisch T, Dinse HR. Superior sensory, motor, and cognitive performance in elderly individuals with multi-year dancing activities. Front Aging Neurosci. 2010;2:31.
12. Kline F, Burgoyne RW, Staples F, Moredock P, Snyder V, Ioerger M. A report on the use of movement therapy for chronic, severely disabled outpatients. Arts Psychother. 1977;4(4-5):181-183.
13. Koch SC, Morlinghaus K, Fuchs T. The joy dance: specific effects of a single dance intervention on psychiatric patients with depression. Arts Psychother. 2007;34(4):340-349.
14. Barton EJ. Movement and mindfulness: a formative evaluation of a dance/movement and yoga therapy program with participants experiencing severe mental illness. Am J Dance Ther. 2011;33(2):157-181.
15. van der Kolk BA, McFarlane AC, Weisaeth L, eds. Traumatic Stress: The Effects of Overwhelming Experience on Mind, Body, and Society. New York, NY: Guilford Press; 1996.
16. Foa EB, Keane TM, Friedman MJ, Cohen JA, eds. Effective Treatments for PTSD: Practice Guidelines From the International Society for Traumatic Stress Studies. 2nd ed. New York, NY: Guilford Press; 2009.
17. Wilbur S, Meyer HB, Baker MR, et al. Dance for Veterans: a complementary health program for veterans with serious mental illness. Arts Health. 2015;7(2):96-108.
18. Gradus JL. Epidemiology of PTSD. U.S. Department of Veterans Affairs, PTSD: National Center for PTSD website. http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. Published January 30, 2014. Accessed August 20, 2015.
19. Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, Karlin BE. Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. JAMA Psychiatry. 2013;70(9):949-955.
20. Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J Consult Clin Psychol. 2006;74(5):898-907.
21. Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71(2):134-168.
22. Suarez CA, Wilbur S, Smiarowski K, Rubin RT, Ames D. Dance for Veterans: Music, Movement & Rhythm Manual for Instruction. 2nd ed. Publisher unknown; 2014.
23. Gilbert AG, Gilbert BA, Rossano A. Brain-Compatible Dance Education. Reston, VA: National Dance Association; 2006.
24. Spielberger C. Manual for the State-Trait Anxiety Inventory. Rev ed. Palo Alto, CA: Consulting Psychologists Press; 1983.
25. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011;63(suppl 11):S467-S472.
1. Levy FJ. Dance/Movement Therapy: A Healing Art. Reston, VA: American Alliance for Health, Physical Education, Recreation, and Dance; 1992.
2. Marigold DS, Misiaszek JE. Whole-body responses: neural control and implications for rehabilitation and fall prevention. Neuroscientist. 2009;15(1):36-46.
3. Hackney ME, Kantorovich S, Levin R, Earhart GM. Effects of tango on functional mobility in Parkinson's disease: a preliminary study. J Neurol Phys Ther. 2007;31(4):173-179.
4. Ravelin T, Kylmä J, Korhonen T. Dance in mental health nursing: a hybrid concept analysis. Issues Ment Health Nurs. 2006;27(3):307-317.
5. Hackney ME, Earhart GM. Effects of dance on gait and balance in Parkinson's disease: a comparison of partnered and nonpartnered dance movement. Neurorehabil Neural Repair. 2010;24(4):384-392.
6. Heiberger L, Maurer C, Amtage F, et al. Impact of a weekly dance class on the functional mobility and on the quality of life of individuals with Parkinson's disease. Front Aging Neurosci. 2011;3:14.
7. Houston S, McGill A. A mixed-methods study into ballet for people living with Parkinson's. Arts Health. 2013;5(2):103-119.
8. Westheimer O. Why dance for Parkinson's disease. Top Geriatr Rehabil. 2008;24(2):127-140.
9. Bräuninger I. Dance movement therapy group intervention in stress treatment: a randomized controlled trial (RCT). Arts Psychother. 2012;39(5):443-450.
10. Kattenstroth, JC, Kalisch T, Holt S, Tegenthoff M, Dinse HR. Six months of dance intervention enhances postural, sensorimotor, and cognitive performance in elderly without affecting cardio-respiratory functions. Front Aging Neurosci. 2013;5:5.
11. Kattenstroth J-C, Kolankowska I, Kalisch T, Dinse HR. Superior sensory, motor, and cognitive performance in elderly individuals with multi-year dancing activities. Front Aging Neurosci. 2010;2:31.
12. Kline F, Burgoyne RW, Staples F, Moredock P, Snyder V, Ioerger M. A report on the use of movement therapy for chronic, severely disabled outpatients. Arts Psychother. 1977;4(4-5):181-183.
13. Koch SC, Morlinghaus K, Fuchs T. The joy dance: specific effects of a single dance intervention on psychiatric patients with depression. Arts Psychother. 2007;34(4):340-349.
14. Barton EJ. Movement and mindfulness: a formative evaluation of a dance/movement and yoga therapy program with participants experiencing severe mental illness. Am J Dance Ther. 2011;33(2):157-181.
15. van der Kolk BA, McFarlane AC, Weisaeth L, eds. Traumatic Stress: The Effects of Overwhelming Experience on Mind, Body, and Society. New York, NY: Guilford Press; 1996.
16. Foa EB, Keane TM, Friedman MJ, Cohen JA, eds. Effective Treatments for PTSD: Practice Guidelines From the International Society for Traumatic Stress Studies. 2nd ed. New York, NY: Guilford Press; 2009.
17. Wilbur S, Meyer HB, Baker MR, et al. Dance for Veterans: a complementary health program for veterans with serious mental illness. Arts Health. 2015;7(2):96-108.
18. Gradus JL. Epidemiology of PTSD. U.S. Department of Veterans Affairs, PTSD: National Center for PTSD website. http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. Published January 30, 2014. Accessed August 20, 2015.
19. Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, Karlin BE. Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. JAMA Psychiatry. 2013;70(9):949-955.
20. Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J Consult Clin Psychol. 2006;74(5):898-907.
21. Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry. 2008;71(2):134-168.
22. Suarez CA, Wilbur S, Smiarowski K, Rubin RT, Ames D. Dance for Veterans: Music, Movement & Rhythm Manual for Instruction. 2nd ed. Publisher unknown; 2014.
23. Gilbert AG, Gilbert BA, Rossano A. Brain-Compatible Dance Education. Reston, VA: National Dance Association; 2006.
24. Spielberger C. Manual for the State-Trait Anxiety Inventory. Rev ed. Palo Alto, CA: Consulting Psychologists Press; 1983.
25. Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011;63(suppl 11):S467-S472.