User login
MDMA Is Off the Table, So What’s Next for PTSD?
It has been 24 years since a pharmaceutical was last approved for posttraumatic stress disorder (PTSD). The condition is notoriously difficult to treat, with up to 40% patients finding no relief from symptoms through psychotherapy or current medications.
Many clinicians, advocates, and patients had pinned their hopes on the psychedelic drug midomafetamine with assisted therapy (MDMA-AT). However, in August, the US Food and Drug Administration (FDA) rejected it. At this point, it’s unclear when the therapy will be available, if ever.
“Not getting the FDA approval of any drug at this point is a setback for the field,” Lori Davis, MD, a senior research psychiatrist at the Birmingham Veterans Affairs (VA) Health Care System in Birmingham, Alabama, told Medscape Medical News.
Having an FDA-approved product would have helped increase public awareness of PTSD and driven interest in developing new therapies, said Davis, who is also adjunct professor of psychiatry at the Heersink School of Medicine, University of Alabama at Birmingham.
A Treatable Condition
So with MDMA-AT off the table, where does the field go next?
A public meeting in September hosted by the Reagan-Udall Foundation for the FDA in sought to answer that question. Agency officials joined representatives from the Department of Defense (DoD) and VA, patients, advocates, and industry representatives to discuss the current treatment landscape and what can be done to accelerate development of PTSD treatment.
Despite the common belief that PTSD is intractable, it “is a treatable condition,” Paula P. Schnurr, PhD, executive director of the VA National Center for PTSD, said at the meeting.
“There are effective treatments that work well for a lot of people, although not everyone has a satisfactory response,” she added.
The most effective psychotherapies are “trauma-focused,” and include cognitive processing therapy, eye movement desensitization and reprocessing, and prolonged exposure, according to the VA National Center for PTSD.
Three drugs have been approved by the FDA for PTSD: Venlafaxine (Effexor) in 1993, sertraline (Zoloft) in 1999, and paroxetine (Paxil) in 2000.
However, as the September meeting demonstrated, more therapies are needed.
“It’s clear to FDA and the federal government at large that there is an unmet need for safe and effective therapies to treat PTSD,” Bernard Fischer, MD, deputy director of the Division of Psychiatry in the Office of New Drugs at FDA’s Center for Drug Evaluation and Research, said at the meeting.
There is no shortage of research, Fischer added. Nearly 500 trials focused on PTSD are listed on clinicaltrials.gov are recruiting participants now or plan to soon.
Unsurprisingly, one of the primary drivers of PTSD therapeutics research is the VA. About 14% of the 5.7 million veterans who received care through the VA in 2023 had a diagnosis of PTSD.
“The US military is currently losing thousands of service members each year to PTSD- related disability discharges,” US Army Maj. Aaron Wolfgang, MD, a psychiatrist at the Walter Reed National Military Medical Center, said at the meeting. Only about 12%-20% of patients achieve remission with conventional therapies, added Wolfgang, who also is an assistant professor at the Uniformed Services University.
“For these reasons, establishing better treatments for PTSD is not only a matter of humanitarianism but also a pressing matter of national security,” he said.
The VA has committed at least $230 million to more than 140 active research projects in PTSD, Miriam J. Smyth, PhD, acting director of the clinical science, research and development service at the VA, said at the Reagan-Udall meeting.
One of the VA projects is the PTSD psychopharmacology initiative, which began in 2017 and now has 14 active clinical trials, said Smyth, who is also acting director for brain behavior and mental health at the VA. The first study should be finished by 2025.
The Million Veteran Program, with more than 1 million enrollees, has led to the discovery of genes related to re-experiencing traumatic memories and has confirmed that both PTSD and traumatic brain injury are risk factors for dementia, Smyth said.
The DoD has created a novel platform that establishes a common infrastructure for testing multiple drugs, called M-PACT. The platform allows sharing of placebo data across treatment arms. Drugs cycle off the platform if evidence indicates probability of success or failure.
Four trials are actively recruiting veterans and current service members. One is looking at vilazodone, approved in 2011 for major depressive disorder. It is being compared with placebo and fluoxetine in a trial that is currently recruiting.
Another trial will study daridorexant (sold as Quviviq), an orexin receptor antagonist, against placebo. The FDA approved daridorexant in 2022 as an insomnia treatment. A core issue in PTSD is sleep disruption, noted Davis.
New Therapies on the Way
Separately, Davis and colleagues are also studying methylphenidate, the stimulant used for attention-deficit/hyperactivity disorder. It may help with neurocognitive complaints and reduce PTSD symptoms, said Davis.
Because it is generic, few pharmaceutical manufacturers are likely to test it for PTSD, she said. But eventually, their work may lead a company to test newer stimulants for PTSD, she said.
Another potential therapeutic, BNC210, received Fast Track designation for PTSD from the FDA in 2019. Bionomics Limited in Australia will soon launch phase 3 trials of the investigational oral drug, which is a negative allosteric modulator of the alpha-7 nicotinic acetylcholine receptor. In late July, the company announced “ favorable feedback” from the agency on its phase 2 study, which led to the decision to move forward with larger trials.
Researchers at Brigham and Women’s Hospital have just reported that they may have found a target within the brain that will allow for transcranial magnetic stimulation (TMS) to ameliorate PTSD symptoms. They published results of a mapping effort in Nature Neuroscience and reported on one patient who had improved symptoms after receiving TMS for severe PTSD.
But perhaps one of the most promising treatments is a combination of sertraline and the new psychiatric medication brexpiprazole.
Brexpiprazole was developed by Otsuka Pharmaceutical and approved in the United States in 2015 as an adjunctive therapy to antidepressants for major depressive disorder and as a treatment for schizophrenia. In 2023, the FDA approved it for Alzheimer’s-related agitation. However, according to Otsuka, its mechanism of action is unknown.
Its efficacy may be mediated through a combination of partial agonist activity at serotonin 5-HT1A and dopamine D2 receptors, antagonist activity at serotonin 5-HT2A receptors, as well as antagonism of alpha-1B/2C receptors, said the company.
“It is the combination, rather than either alone, that’s going to have that broad synergistic pharmacology that is obviously potent for ameliorating the symptoms of PTSD,” said Davis, who has received consulting fees from Otsuka. “That’s an exciting development.”
Otsuka and partner Lundbeck Pharmaceuticals reported results in May from the companies’ phase 2 and 3 randomized clinical trials. The therapy achieved a statistically significant reduction (P <.05) in PTSD symptoms compared with sertraline plus placebo. This was without any supplemental psychotherapy.
The FDA accepted the companies’ new drug application in June and is expected to make a decision on approval in February 2025.
The Potential of Psychedelics
Though Lykos Therapeutics may have to go back to the drawing board on its MDMA-AT, psychedelics still have potential as PTSD therapies, Smyth said, who added that the VA is continuing to encourage study of MDMA and other psychedelic agents.
The VA issued a call for proposals for research on psychedelics in January, focused on MDMA or psilocybin in combination with psychotherapy. The administration received the first wave of applications early in the summer.
Scientific peer review panels made up of research experts from within and outside the VA have reviewed the applications and funding announcements are expected this fall, Smyth said.
Wolfgang, the Army psychiatrist, said, “Under the psychedelic treatment research clinical trial award, we welcome investigators to apply to what we anticipate will usher in a new era of innovation and hope for service members and their families who need it the most.”
Psychedelic studies are also proceeding without VA funding, as they have for years, when most of the trials were backed by universities or foundations or other private money. Johns Hopkins University is recruiting for a study in which patients would receive psilocybin along with trauma-focused psychotherapy, as is Ohio State University.
London-based Compass Pathways said in May that it successfully completed a phase 2 trial of Comp360, its synthetic psilocybin, in PTSD. The company has started a phase 3 study in treatment-resistant depression but has not given any further updates on PTSD.
Davis said that she believes that the FDA’s rejection of Lykos won’t lead to a shutdown of exploration of psychedelics.
“I think it informs these designs going forward, but it doesn’t eliminate that whole field of research,” she said.
Davis reported receiving consulting fees from Boehringer Ingelheim and Otsuka and research funding from Alkermes, the Patient-Centered Outcomes Research Institute, and the VA. Schnurr, Fischer, Smyth, and Wolfgang reported no relevant disclosures.
A version of this article appeared on Medscape.com.
It has been 24 years since a pharmaceutical was last approved for posttraumatic stress disorder (PTSD). The condition is notoriously difficult to treat, with up to 40% patients finding no relief from symptoms through psychotherapy or current medications.
Many clinicians, advocates, and patients had pinned their hopes on the psychedelic drug midomafetamine with assisted therapy (MDMA-AT). However, in August, the US Food and Drug Administration (FDA) rejected it. At this point, it’s unclear when the therapy will be available, if ever.
“Not getting the FDA approval of any drug at this point is a setback for the field,” Lori Davis, MD, a senior research psychiatrist at the Birmingham Veterans Affairs (VA) Health Care System in Birmingham, Alabama, told Medscape Medical News.
Having an FDA-approved product would have helped increase public awareness of PTSD and driven interest in developing new therapies, said Davis, who is also adjunct professor of psychiatry at the Heersink School of Medicine, University of Alabama at Birmingham.
A Treatable Condition
So with MDMA-AT off the table, where does the field go next?
A public meeting in September hosted by the Reagan-Udall Foundation for the FDA in sought to answer that question. Agency officials joined representatives from the Department of Defense (DoD) and VA, patients, advocates, and industry representatives to discuss the current treatment landscape and what can be done to accelerate development of PTSD treatment.
Despite the common belief that PTSD is intractable, it “is a treatable condition,” Paula P. Schnurr, PhD, executive director of the VA National Center for PTSD, said at the meeting.
“There are effective treatments that work well for a lot of people, although not everyone has a satisfactory response,” she added.
The most effective psychotherapies are “trauma-focused,” and include cognitive processing therapy, eye movement desensitization and reprocessing, and prolonged exposure, according to the VA National Center for PTSD.
Three drugs have been approved by the FDA for PTSD: Venlafaxine (Effexor) in 1993, sertraline (Zoloft) in 1999, and paroxetine (Paxil) in 2000.
However, as the September meeting demonstrated, more therapies are needed.
“It’s clear to FDA and the federal government at large that there is an unmet need for safe and effective therapies to treat PTSD,” Bernard Fischer, MD, deputy director of the Division of Psychiatry in the Office of New Drugs at FDA’s Center for Drug Evaluation and Research, said at the meeting.
There is no shortage of research, Fischer added. Nearly 500 trials focused on PTSD are listed on clinicaltrials.gov are recruiting participants now or plan to soon.
Unsurprisingly, one of the primary drivers of PTSD therapeutics research is the VA. About 14% of the 5.7 million veterans who received care through the VA in 2023 had a diagnosis of PTSD.
“The US military is currently losing thousands of service members each year to PTSD- related disability discharges,” US Army Maj. Aaron Wolfgang, MD, a psychiatrist at the Walter Reed National Military Medical Center, said at the meeting. Only about 12%-20% of patients achieve remission with conventional therapies, added Wolfgang, who also is an assistant professor at the Uniformed Services University.
“For these reasons, establishing better treatments for PTSD is not only a matter of humanitarianism but also a pressing matter of national security,” he said.
The VA has committed at least $230 million to more than 140 active research projects in PTSD, Miriam J. Smyth, PhD, acting director of the clinical science, research and development service at the VA, said at the Reagan-Udall meeting.
One of the VA projects is the PTSD psychopharmacology initiative, which began in 2017 and now has 14 active clinical trials, said Smyth, who is also acting director for brain behavior and mental health at the VA. The first study should be finished by 2025.
The Million Veteran Program, with more than 1 million enrollees, has led to the discovery of genes related to re-experiencing traumatic memories and has confirmed that both PTSD and traumatic brain injury are risk factors for dementia, Smyth said.
The DoD has created a novel platform that establishes a common infrastructure for testing multiple drugs, called M-PACT. The platform allows sharing of placebo data across treatment arms. Drugs cycle off the platform if evidence indicates probability of success or failure.
Four trials are actively recruiting veterans and current service members. One is looking at vilazodone, approved in 2011 for major depressive disorder. It is being compared with placebo and fluoxetine in a trial that is currently recruiting.
Another trial will study daridorexant (sold as Quviviq), an orexin receptor antagonist, against placebo. The FDA approved daridorexant in 2022 as an insomnia treatment. A core issue in PTSD is sleep disruption, noted Davis.
New Therapies on the Way
Separately, Davis and colleagues are also studying methylphenidate, the stimulant used for attention-deficit/hyperactivity disorder. It may help with neurocognitive complaints and reduce PTSD symptoms, said Davis.
Because it is generic, few pharmaceutical manufacturers are likely to test it for PTSD, she said. But eventually, their work may lead a company to test newer stimulants for PTSD, she said.
Another potential therapeutic, BNC210, received Fast Track designation for PTSD from the FDA in 2019. Bionomics Limited in Australia will soon launch phase 3 trials of the investigational oral drug, which is a negative allosteric modulator of the alpha-7 nicotinic acetylcholine receptor. In late July, the company announced “ favorable feedback” from the agency on its phase 2 study, which led to the decision to move forward with larger trials.
Researchers at Brigham and Women’s Hospital have just reported that they may have found a target within the brain that will allow for transcranial magnetic stimulation (TMS) to ameliorate PTSD symptoms. They published results of a mapping effort in Nature Neuroscience and reported on one patient who had improved symptoms after receiving TMS for severe PTSD.
But perhaps one of the most promising treatments is a combination of sertraline and the new psychiatric medication brexpiprazole.
Brexpiprazole was developed by Otsuka Pharmaceutical and approved in the United States in 2015 as an adjunctive therapy to antidepressants for major depressive disorder and as a treatment for schizophrenia. In 2023, the FDA approved it for Alzheimer’s-related agitation. However, according to Otsuka, its mechanism of action is unknown.
Its efficacy may be mediated through a combination of partial agonist activity at serotonin 5-HT1A and dopamine D2 receptors, antagonist activity at serotonin 5-HT2A receptors, as well as antagonism of alpha-1B/2C receptors, said the company.
“It is the combination, rather than either alone, that’s going to have that broad synergistic pharmacology that is obviously potent for ameliorating the symptoms of PTSD,” said Davis, who has received consulting fees from Otsuka. “That’s an exciting development.”
Otsuka and partner Lundbeck Pharmaceuticals reported results in May from the companies’ phase 2 and 3 randomized clinical trials. The therapy achieved a statistically significant reduction (P <.05) in PTSD symptoms compared with sertraline plus placebo. This was without any supplemental psychotherapy.
The FDA accepted the companies’ new drug application in June and is expected to make a decision on approval in February 2025.
The Potential of Psychedelics
Though Lykos Therapeutics may have to go back to the drawing board on its MDMA-AT, psychedelics still have potential as PTSD therapies, Smyth said, who added that the VA is continuing to encourage study of MDMA and other psychedelic agents.
The VA issued a call for proposals for research on psychedelics in January, focused on MDMA or psilocybin in combination with psychotherapy. The administration received the first wave of applications early in the summer.
Scientific peer review panels made up of research experts from within and outside the VA have reviewed the applications and funding announcements are expected this fall, Smyth said.
Wolfgang, the Army psychiatrist, said, “Under the psychedelic treatment research clinical trial award, we welcome investigators to apply to what we anticipate will usher in a new era of innovation and hope for service members and their families who need it the most.”
Psychedelic studies are also proceeding without VA funding, as they have for years, when most of the trials were backed by universities or foundations or other private money. Johns Hopkins University is recruiting for a study in which patients would receive psilocybin along with trauma-focused psychotherapy, as is Ohio State University.
London-based Compass Pathways said in May that it successfully completed a phase 2 trial of Comp360, its synthetic psilocybin, in PTSD. The company has started a phase 3 study in treatment-resistant depression but has not given any further updates on PTSD.
Davis said that she believes that the FDA’s rejection of Lykos won’t lead to a shutdown of exploration of psychedelics.
“I think it informs these designs going forward, but it doesn’t eliminate that whole field of research,” she said.
Davis reported receiving consulting fees from Boehringer Ingelheim and Otsuka and research funding from Alkermes, the Patient-Centered Outcomes Research Institute, and the VA. Schnurr, Fischer, Smyth, and Wolfgang reported no relevant disclosures.
A version of this article appeared on Medscape.com.
It has been 24 years since a pharmaceutical was last approved for posttraumatic stress disorder (PTSD). The condition is notoriously difficult to treat, with up to 40% patients finding no relief from symptoms through psychotherapy or current medications.
Many clinicians, advocates, and patients had pinned their hopes on the psychedelic drug midomafetamine with assisted therapy (MDMA-AT). However, in August, the US Food and Drug Administration (FDA) rejected it. At this point, it’s unclear when the therapy will be available, if ever.
“Not getting the FDA approval of any drug at this point is a setback for the field,” Lori Davis, MD, a senior research psychiatrist at the Birmingham Veterans Affairs (VA) Health Care System in Birmingham, Alabama, told Medscape Medical News.
Having an FDA-approved product would have helped increase public awareness of PTSD and driven interest in developing new therapies, said Davis, who is also adjunct professor of psychiatry at the Heersink School of Medicine, University of Alabama at Birmingham.
A Treatable Condition
So with MDMA-AT off the table, where does the field go next?
A public meeting in September hosted by the Reagan-Udall Foundation for the FDA in sought to answer that question. Agency officials joined representatives from the Department of Defense (DoD) and VA, patients, advocates, and industry representatives to discuss the current treatment landscape and what can be done to accelerate development of PTSD treatment.
Despite the common belief that PTSD is intractable, it “is a treatable condition,” Paula P. Schnurr, PhD, executive director of the VA National Center for PTSD, said at the meeting.
“There are effective treatments that work well for a lot of people, although not everyone has a satisfactory response,” she added.
The most effective psychotherapies are “trauma-focused,” and include cognitive processing therapy, eye movement desensitization and reprocessing, and prolonged exposure, according to the VA National Center for PTSD.
Three drugs have been approved by the FDA for PTSD: Venlafaxine (Effexor) in 1993, sertraline (Zoloft) in 1999, and paroxetine (Paxil) in 2000.
However, as the September meeting demonstrated, more therapies are needed.
“It’s clear to FDA and the federal government at large that there is an unmet need for safe and effective therapies to treat PTSD,” Bernard Fischer, MD, deputy director of the Division of Psychiatry in the Office of New Drugs at FDA’s Center for Drug Evaluation and Research, said at the meeting.
There is no shortage of research, Fischer added. Nearly 500 trials focused on PTSD are listed on clinicaltrials.gov are recruiting participants now or plan to soon.
Unsurprisingly, one of the primary drivers of PTSD therapeutics research is the VA. About 14% of the 5.7 million veterans who received care through the VA in 2023 had a diagnosis of PTSD.
“The US military is currently losing thousands of service members each year to PTSD- related disability discharges,” US Army Maj. Aaron Wolfgang, MD, a psychiatrist at the Walter Reed National Military Medical Center, said at the meeting. Only about 12%-20% of patients achieve remission with conventional therapies, added Wolfgang, who also is an assistant professor at the Uniformed Services University.
“For these reasons, establishing better treatments for PTSD is not only a matter of humanitarianism but also a pressing matter of national security,” he said.
The VA has committed at least $230 million to more than 140 active research projects in PTSD, Miriam J. Smyth, PhD, acting director of the clinical science, research and development service at the VA, said at the Reagan-Udall meeting.
One of the VA projects is the PTSD psychopharmacology initiative, which began in 2017 and now has 14 active clinical trials, said Smyth, who is also acting director for brain behavior and mental health at the VA. The first study should be finished by 2025.
The Million Veteran Program, with more than 1 million enrollees, has led to the discovery of genes related to re-experiencing traumatic memories and has confirmed that both PTSD and traumatic brain injury are risk factors for dementia, Smyth said.
The DoD has created a novel platform that establishes a common infrastructure for testing multiple drugs, called M-PACT. The platform allows sharing of placebo data across treatment arms. Drugs cycle off the platform if evidence indicates probability of success or failure.
Four trials are actively recruiting veterans and current service members. One is looking at vilazodone, approved in 2011 for major depressive disorder. It is being compared with placebo and fluoxetine in a trial that is currently recruiting.
Another trial will study daridorexant (sold as Quviviq), an orexin receptor antagonist, against placebo. The FDA approved daridorexant in 2022 as an insomnia treatment. A core issue in PTSD is sleep disruption, noted Davis.
New Therapies on the Way
Separately, Davis and colleagues are also studying methylphenidate, the stimulant used for attention-deficit/hyperactivity disorder. It may help with neurocognitive complaints and reduce PTSD symptoms, said Davis.
Because it is generic, few pharmaceutical manufacturers are likely to test it for PTSD, she said. But eventually, their work may lead a company to test newer stimulants for PTSD, she said.
Another potential therapeutic, BNC210, received Fast Track designation for PTSD from the FDA in 2019. Bionomics Limited in Australia will soon launch phase 3 trials of the investigational oral drug, which is a negative allosteric modulator of the alpha-7 nicotinic acetylcholine receptor. In late July, the company announced “ favorable feedback” from the agency on its phase 2 study, which led to the decision to move forward with larger trials.
Researchers at Brigham and Women’s Hospital have just reported that they may have found a target within the brain that will allow for transcranial magnetic stimulation (TMS) to ameliorate PTSD symptoms. They published results of a mapping effort in Nature Neuroscience and reported on one patient who had improved symptoms after receiving TMS for severe PTSD.
But perhaps one of the most promising treatments is a combination of sertraline and the new psychiatric medication brexpiprazole.
Brexpiprazole was developed by Otsuka Pharmaceutical and approved in the United States in 2015 as an adjunctive therapy to antidepressants for major depressive disorder and as a treatment for schizophrenia. In 2023, the FDA approved it for Alzheimer’s-related agitation. However, according to Otsuka, its mechanism of action is unknown.
Its efficacy may be mediated through a combination of partial agonist activity at serotonin 5-HT1A and dopamine D2 receptors, antagonist activity at serotonin 5-HT2A receptors, as well as antagonism of alpha-1B/2C receptors, said the company.
“It is the combination, rather than either alone, that’s going to have that broad synergistic pharmacology that is obviously potent for ameliorating the symptoms of PTSD,” said Davis, who has received consulting fees from Otsuka. “That’s an exciting development.”
Otsuka and partner Lundbeck Pharmaceuticals reported results in May from the companies’ phase 2 and 3 randomized clinical trials. The therapy achieved a statistically significant reduction (P <.05) in PTSD symptoms compared with sertraline plus placebo. This was without any supplemental psychotherapy.
The FDA accepted the companies’ new drug application in June and is expected to make a decision on approval in February 2025.
The Potential of Psychedelics
Though Lykos Therapeutics may have to go back to the drawing board on its MDMA-AT, psychedelics still have potential as PTSD therapies, Smyth said, who added that the VA is continuing to encourage study of MDMA and other psychedelic agents.
The VA issued a call for proposals for research on psychedelics in January, focused on MDMA or psilocybin in combination with psychotherapy. The administration received the first wave of applications early in the summer.
Scientific peer review panels made up of research experts from within and outside the VA have reviewed the applications and funding announcements are expected this fall, Smyth said.
Wolfgang, the Army psychiatrist, said, “Under the psychedelic treatment research clinical trial award, we welcome investigators to apply to what we anticipate will usher in a new era of innovation and hope for service members and their families who need it the most.”
Psychedelic studies are also proceeding without VA funding, as they have for years, when most of the trials were backed by universities or foundations or other private money. Johns Hopkins University is recruiting for a study in which patients would receive psilocybin along with trauma-focused psychotherapy, as is Ohio State University.
London-based Compass Pathways said in May that it successfully completed a phase 2 trial of Comp360, its synthetic psilocybin, in PTSD. The company has started a phase 3 study in treatment-resistant depression but has not given any further updates on PTSD.
Davis said that she believes that the FDA’s rejection of Lykos won’t lead to a shutdown of exploration of psychedelics.
“I think it informs these designs going forward, but it doesn’t eliminate that whole field of research,” she said.
Davis reported receiving consulting fees from Boehringer Ingelheim and Otsuka and research funding from Alkermes, the Patient-Centered Outcomes Research Institute, and the VA. Schnurr, Fischer, Smyth, and Wolfgang reported no relevant disclosures.
A version of this article appeared on Medscape.com.
PTSD Comorbidities
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
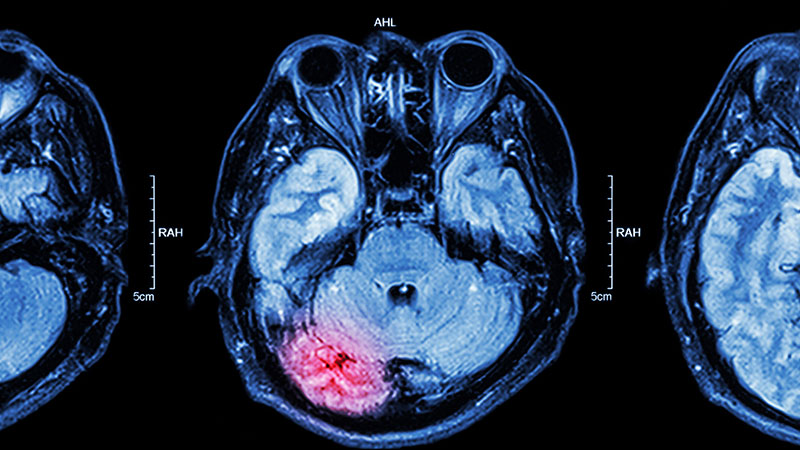
Persistent headaches and nightmares
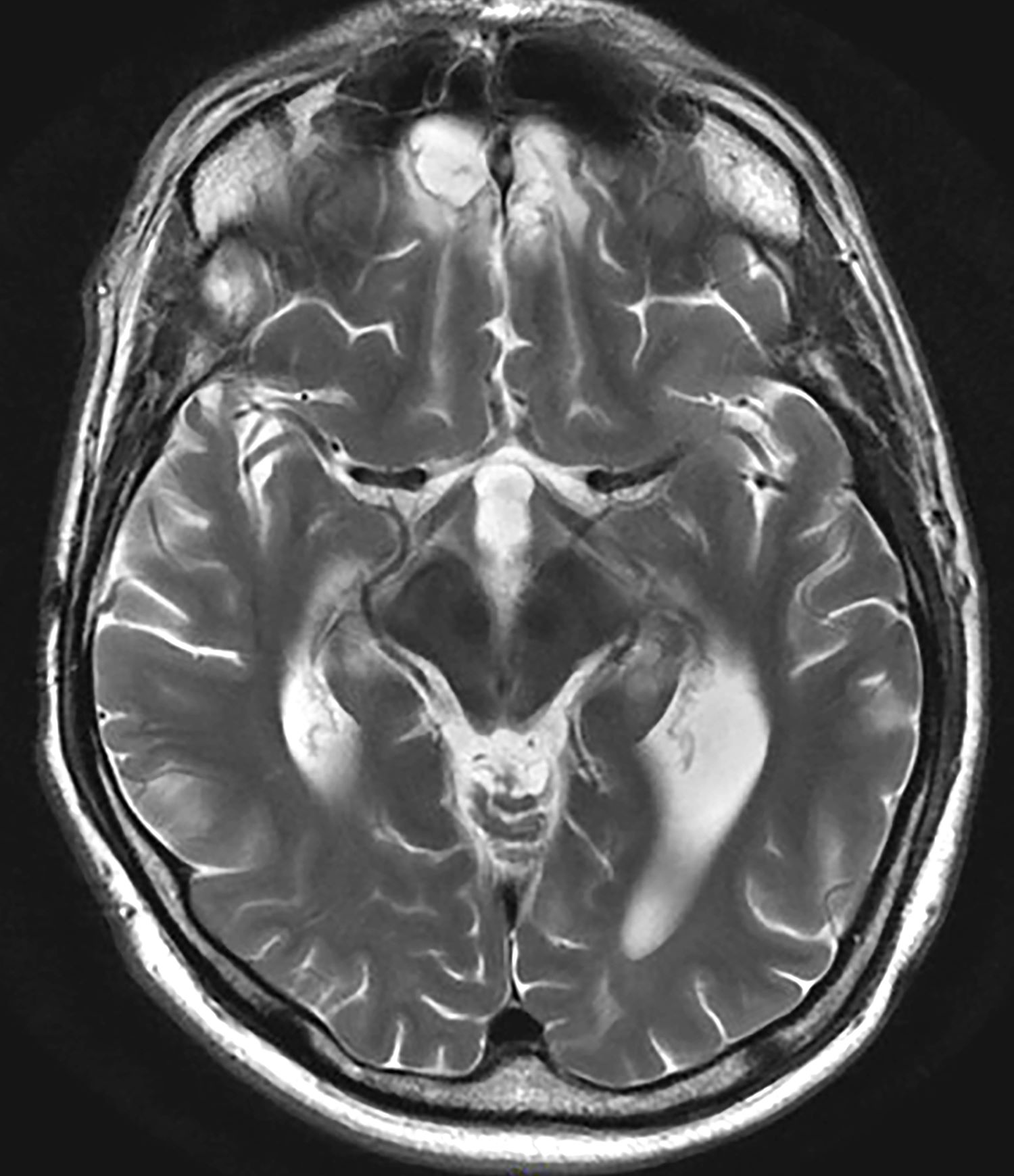
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 15-year-old girl presented to the emergency department with complaints of persistent headaches, nightmares, and difficulty concentrating in school over the past 3 months. The patient had recently experienced a traumatic event, a severe car accident in which a close friend was critically injured. Since the incident, the patient has been exhibiting increased irritability, avoidance of activities that she previously enjoyed, and a noticeable withdrawal from social interactions. Additionally, she reported recurrent flashbacks to the accident, often triggered by sounds resembling car engines. On physical examination, the patient appeared anxious and exhibited hypervigilance. An MRI of the brain was performed to rule out any organic causes of her symptoms, revealing an area of increased signal intensity in the left cerebellar hemisphere (as highlighted in the image).
An Rx for Burnout, Grief, and Illness: Dance
In 2012, Tara Rynders’ sister was diagnosed with acute disseminated encephalomyelitis. For Ms. Rynders, a registered nurse in Denver, Colorado, the news was devastating.
“She was this beautiful 26-year-old woman, strong and healthy, and within 12 hours, she went into a coma and couldn’t move or speak,” Ms. Rynders remembered. She flew to her sister in Reno, Nevada, and moved into her intensive care unit room. The helplessness she felt wasn’t just as a sister, but as a healthcare provider.
“As a nurse, we love to fix things,” Ms. Rynders said. “But when my sister was sick, I couldn’t do anything to fix her. The doctors didn’t even know what was going on.”
When Ms. Rynders’ sister woke from the coma, she couldn’t speak. The only comfort Ms. Rynders could provide was her presence and the ability to put a smile on her sister’s face. So, Ms. Rynders did what came naturally ...
She danced.
In that tiny hospital room, she blasted her sister’s favorite song — “Party in the U.S.A.” by Miley Cyrus — and danced around the room, doing anything she could to make her sister laugh.
And this patient who could not form words found her voice.
“She’d holler so deeply, it almost sounded like she was crying,” Ms. Rynders remembered. “The depths of her grief and the depths of her joy coming out simultaneously. It was really amazing and so healing for both of us.”
Do You Know How Powerful Dancing Really Is?
Ms. Rynders is far from the only healthcare professional who’s discovered the healing power of dance. In recent years, doctors and nurses across the country, from Los Angeles, California, to Atlanta, Georgia; from TikTok’s “Dancing Nurse,” Cindy Jones, to Max Chiu, Nebraska’s breakdancing oncologist, have demonstrated that finding new ways to move your body isn’t just good advice for patients but could be exactly what healthcare providers need to stay mentally and physically healthy.
It comes at a time when the field faces a “mental health crisis,” according to a 2023 report from the Centers for Disease Control and Prevention. Medscape Physician Burnout & Depression Report 2024 found current rates of 49% for burnout and 20% for depression.
And medical professionals are often hesitant about seeking help. Nearly 40% of physicians reported reluctance to seek out mental health treatment over fears of professional repercussions, according to 2024 recommendations by the Mayo Clinic.
The solution? It just might be dancing.
There’s ample evidence. A 2024 study from the University of Sydney, Australia, found that dancing offers more psychological and cognitive benefits — helping with everything from depression to motivation to emotional well-being — than any other type of exercise.
Another study, published in February by
Structured dance, where you learn specific movements, can offer a huge boost to mental health, according to a 2024 University of Sydney study. But so does unchoreographed dancing, where you’re basically just letting your limbs do their own thing. A 2021 study, published in Complementary Therapies in Clinical Practice, found that 95% of dancers who just moved their bodies, regardless of how it looked to the outside world, still had huge benefits with depression, anxiety, and trauma.
How to Turn a Mastectomy Into a Dance Party
Deborah Cohan, MD, 55, an obstetrician at Zuckerberg San Francisco General Hospital and Trauma Center, San Francisco, California, discovered firsthand the power of dance back in 2013. After finding a lump in her breast during a self-exam, Dr. Cohan feared the worst. Days later, her radiologist confirmed she had invasive ductal carcinoma.
“It was a complete shock,” Dr. Cohan remembered. “I took care of myself. I ate right. I had no obvious risk factors. I did work the night shift, and there’s actually an increased risk for breast cancer among ob.gyn. workers who do night shift work. But still, it took me completely by surprise. My kids were 5 and 8 at the time, and I was terrified that they’d grow up without a mom.”
So, Dr. Cohan turned to the only thing that gave her comfort — dance class. Dancing had been an escape for Dr. Cohan since she took her first ballet class at age 3. So, she skipped work and went to her weekly Soul Motion dance class, where she found herself doing the exact opposite of escaping. She embraced her fears.
“I visualized death as a dance partner,” Dr. Cohan said. “I felt a freedom come over my body. It didn’t make sense to me at the time, but it was almost joyful. Not that I was accepting death or anticipating death, but just that I acknowledged its presence. There’s so much pressure among people with cancer to be positive. [But] that’s something that needs to come from within a person, not from outside. Nobody can dictate how someone should be feeling. And as I danced, I was genuinely feeling joy even as I recognized my own fears and didn’t turn away from them. I was experiencing all the emotions at once. It was such a relief to realize this wasn’t all going to be about sadness.”
The experience was so healing for Dr. Cohan that she decided to see if she could bring those same feelings into her bilateral mastectomy. When meeting with her surgical team, Dr. Cohan made an unorthodox request: Could her pre-op include a dance party?
“I asked the anesthesiologist in the pre-op appointment if I could dance, and he said yes,” she remembered, laughing. “And then I checked with the surgeon, and he said yes. And then I asked the perioperative nurse, and he said yes, ‘but only if you don’t make me dance, too’. So somehow it all came together.”
Dr. Cohan decided on the Beyoncé song “Get Me Bodied,” which she says resonated with her because “it’s all about being in your body and being your full self. I was like, that is exactly how I want to show up in the operating room.” The moment the music kicked in and Dr. Cohan broke into dance, all of her stress melted away.
“Even though I’d been given permission to dance, I never expected anybody else to join in,” Dr. Cohan said. But that’s exactly what they did. A friend took a video, which shows Dr. Cohan in a hospital gown and bouffant cap, dancing alongside her surgical and anesthesia teams, all of whom are dressed in scrubs, at Mount Zion Hospital in San Francisco, California.
“It’s weird to say, especially about a mastectomy,” Dr. Cohan said, “but it was one of the most joyful moments of my life.”
The video’s been viewed 8.4 million times and is so inspirational — we dare you to watch it and not want to jump out of your chair to dance — that soon others were following Dr. Cohan’s lead.
- Sixteen-year-old Amari Hall danced to celebrate her successful heart transplant.
- Ana-Alecia Ayala, a 32-year-old uterine cancer survivor, danced along to “Juju on That Beat” to make chemotherapy more tolerable.
- Doreta Norris, a patient with breast cancer, chose “Gangnam Style” to serenade her into surgery.
Bringing Dance to Other Medical Pros
Ms. Rynders realized the true power of dance years before her sister’s illness, when her mother died of cancer. “I’ve always considered myself to be very resilient as a human, but I couldn’t bounce back after my mom died,” she said. “I was nursing full time in the emergency room, and I was sad all the time. And then one day I realized, you know what brings me joy? It’s always been dance.”
She went back to school to get her Master of Fine Arts in Dance from the University of Colorado at Boulder, which she believes helped her heal. “I was actually able to grieve instead of just pretending I was okay,” she said.
Inspired by these experiences, Ms. Rynders founded The Clinic in 2017, a company that provides dance workshops for healthcare professionals struggling with burnout and secondary traumatic stress.
“I see these nurses running down hospital hallways, covered in blood from patients whose lives are literally hanging on a thread,” she said. “They’re dealing with so much stress and grief and hardship. And then to see them with us, playing and laughing — those deep belly laughs that you haven’t done since you were a kid, the deep laughing that comes from deep in your soul. It can be transformational, for them and for you.”
Ms. Rynders remembers one especially healing workshop in which the participants pretended to be astronauts in deep space, using zero gravity to inform their movements. After the exercise, a veteran hospital nurse took Ms. Rynders aside to thank her, mentioning that she was still dealing with grief for her late son, who had died from suicide years earlier.
“She had a lot of guilt around it,” Ms. Rynders remembered. “And she said to me, ‘When I went to space, I felt closer to him.’ It was just this silly little game, but it gave her this lightness that she hadn’t felt in years. She was able to be free and laugh and play and feel close to her son again.”
Good Medicine
Dr. Cohan, who today is cancer free, said her experience made her completely rethink her relationship with patients. She has danced with more than a few of them, though she’s careful never to force it on them. “I never want to project my idea of joy onto others,” she said. “But more than anything, it’s changed my thinking on what it means to take ownership as a patient.”
The one thing Dr. Cohan never wanted as a patient, and the thing she never wants for her own patients, is the loss of agency. “When I danced, I didn’t feel like I was just handing over my body and begrudgingly accepting what was about to happen to me,” she said. “I was taking ownership around my decision, and I felt connected, really connected, to my surgical team.”
As a patient, Dr. Cohan experienced what she calls the “regimented” atmosphere of medicine. “You’re told where to go, what to do, and you have no control over any of it,” recalled Dr. Cohan, who’s now semiretired and runs retreats for women with breast cancer. “But by bringing in dance, it felt really radical that my healthcare team was doing my thing, not the other way around.”
(Re)Learning to Move More Consciously
Healthcare providers need these moments of escape just as much as patients living with disease. The difference is, as Ms. Rynders points out, those in the medical field aren’t always as aware of their emotional distress. “I think if you ask a nurse, ‘How can I help you? What do you need?’ They’re usually like, ‘I don’t know. I don’t even know what I need,’ ” Ms. Rynders said. “Even if they did know what they needed, I think it’s hard to ask for it and even harder to receive it.”
At Ms. Rynders’ workshops, not everybody is comfortable dancing, of course. So, new participants are always given the option just to witness, to be in the room and watch what happens. “But I also really encourage people to take advantage of this opportunity to do something different and disrupt the way we live on a daily basis,” Ms. Rynders said. “Let your brain try something new and be courageous. We’ve only had a few people who sat on the sidelines the whole time.”
It’s not always just about feelings, Dr. Cohan added, but physical relaxation. “Sometimes it’s just about remembering how to move consciously. When I was having surgery, I didn’t just dance to relax myself. I wanted my entire surgical team to be relaxed.”
For Ms. Rynders, every time she dances with her patients, or with fellow healthcare workers, she’s reminded of her sister and the comfort she was able to give her when no amount of medicine would make things better.
“We don’t always need to be fixed by things,” she said. “Sometimes we just need to be present with one another and be with each other. And sometimes, the best way to do that is by dancing till the tears roll down your cheeks.”
A version of this article appeared on Medscape.com.
In 2012, Tara Rynders’ sister was diagnosed with acute disseminated encephalomyelitis. For Ms. Rynders, a registered nurse in Denver, Colorado, the news was devastating.
“She was this beautiful 26-year-old woman, strong and healthy, and within 12 hours, she went into a coma and couldn’t move or speak,” Ms. Rynders remembered. She flew to her sister in Reno, Nevada, and moved into her intensive care unit room. The helplessness she felt wasn’t just as a sister, but as a healthcare provider.
“As a nurse, we love to fix things,” Ms. Rynders said. “But when my sister was sick, I couldn’t do anything to fix her. The doctors didn’t even know what was going on.”
When Ms. Rynders’ sister woke from the coma, she couldn’t speak. The only comfort Ms. Rynders could provide was her presence and the ability to put a smile on her sister’s face. So, Ms. Rynders did what came naturally ...
She danced.
In that tiny hospital room, she blasted her sister’s favorite song — “Party in the U.S.A.” by Miley Cyrus — and danced around the room, doing anything she could to make her sister laugh.
And this patient who could not form words found her voice.
“She’d holler so deeply, it almost sounded like she was crying,” Ms. Rynders remembered. “The depths of her grief and the depths of her joy coming out simultaneously. It was really amazing and so healing for both of us.”
Do You Know How Powerful Dancing Really Is?
Ms. Rynders is far from the only healthcare professional who’s discovered the healing power of dance. In recent years, doctors and nurses across the country, from Los Angeles, California, to Atlanta, Georgia; from TikTok’s “Dancing Nurse,” Cindy Jones, to Max Chiu, Nebraska’s breakdancing oncologist, have demonstrated that finding new ways to move your body isn’t just good advice for patients but could be exactly what healthcare providers need to stay mentally and physically healthy.
It comes at a time when the field faces a “mental health crisis,” according to a 2023 report from the Centers for Disease Control and Prevention. Medscape Physician Burnout & Depression Report 2024 found current rates of 49% for burnout and 20% for depression.
And medical professionals are often hesitant about seeking help. Nearly 40% of physicians reported reluctance to seek out mental health treatment over fears of professional repercussions, according to 2024 recommendations by the Mayo Clinic.
The solution? It just might be dancing.
There’s ample evidence. A 2024 study from the University of Sydney, Australia, found that dancing offers more psychological and cognitive benefits — helping with everything from depression to motivation to emotional well-being — than any other type of exercise.
Another study, published in February by
Structured dance, where you learn specific movements, can offer a huge boost to mental health, according to a 2024 University of Sydney study. But so does unchoreographed dancing, where you’re basically just letting your limbs do their own thing. A 2021 study, published in Complementary Therapies in Clinical Practice, found that 95% of dancers who just moved their bodies, regardless of how it looked to the outside world, still had huge benefits with depression, anxiety, and trauma.
How to Turn a Mastectomy Into a Dance Party
Deborah Cohan, MD, 55, an obstetrician at Zuckerberg San Francisco General Hospital and Trauma Center, San Francisco, California, discovered firsthand the power of dance back in 2013. After finding a lump in her breast during a self-exam, Dr. Cohan feared the worst. Days later, her radiologist confirmed she had invasive ductal carcinoma.
“It was a complete shock,” Dr. Cohan remembered. “I took care of myself. I ate right. I had no obvious risk factors. I did work the night shift, and there’s actually an increased risk for breast cancer among ob.gyn. workers who do night shift work. But still, it took me completely by surprise. My kids were 5 and 8 at the time, and I was terrified that they’d grow up without a mom.”
So, Dr. Cohan turned to the only thing that gave her comfort — dance class. Dancing had been an escape for Dr. Cohan since she took her first ballet class at age 3. So, she skipped work and went to her weekly Soul Motion dance class, where she found herself doing the exact opposite of escaping. She embraced her fears.
“I visualized death as a dance partner,” Dr. Cohan said. “I felt a freedom come over my body. It didn’t make sense to me at the time, but it was almost joyful. Not that I was accepting death or anticipating death, but just that I acknowledged its presence. There’s so much pressure among people with cancer to be positive. [But] that’s something that needs to come from within a person, not from outside. Nobody can dictate how someone should be feeling. And as I danced, I was genuinely feeling joy even as I recognized my own fears and didn’t turn away from them. I was experiencing all the emotions at once. It was such a relief to realize this wasn’t all going to be about sadness.”
The experience was so healing for Dr. Cohan that she decided to see if she could bring those same feelings into her bilateral mastectomy. When meeting with her surgical team, Dr. Cohan made an unorthodox request: Could her pre-op include a dance party?
“I asked the anesthesiologist in the pre-op appointment if I could dance, and he said yes,” she remembered, laughing. “And then I checked with the surgeon, and he said yes. And then I asked the perioperative nurse, and he said yes, ‘but only if you don’t make me dance, too’. So somehow it all came together.”
Dr. Cohan decided on the Beyoncé song “Get Me Bodied,” which she says resonated with her because “it’s all about being in your body and being your full self. I was like, that is exactly how I want to show up in the operating room.” The moment the music kicked in and Dr. Cohan broke into dance, all of her stress melted away.
“Even though I’d been given permission to dance, I never expected anybody else to join in,” Dr. Cohan said. But that’s exactly what they did. A friend took a video, which shows Dr. Cohan in a hospital gown and bouffant cap, dancing alongside her surgical and anesthesia teams, all of whom are dressed in scrubs, at Mount Zion Hospital in San Francisco, California.
“It’s weird to say, especially about a mastectomy,” Dr. Cohan said, “but it was one of the most joyful moments of my life.”
The video’s been viewed 8.4 million times and is so inspirational — we dare you to watch it and not want to jump out of your chair to dance — that soon others were following Dr. Cohan’s lead.
- Sixteen-year-old Amari Hall danced to celebrate her successful heart transplant.
- Ana-Alecia Ayala, a 32-year-old uterine cancer survivor, danced along to “Juju on That Beat” to make chemotherapy more tolerable.
- Doreta Norris, a patient with breast cancer, chose “Gangnam Style” to serenade her into surgery.
Bringing Dance to Other Medical Pros
Ms. Rynders realized the true power of dance years before her sister’s illness, when her mother died of cancer. “I’ve always considered myself to be very resilient as a human, but I couldn’t bounce back after my mom died,” she said. “I was nursing full time in the emergency room, and I was sad all the time. And then one day I realized, you know what brings me joy? It’s always been dance.”
She went back to school to get her Master of Fine Arts in Dance from the University of Colorado at Boulder, which she believes helped her heal. “I was actually able to grieve instead of just pretending I was okay,” she said.
Inspired by these experiences, Ms. Rynders founded The Clinic in 2017, a company that provides dance workshops for healthcare professionals struggling with burnout and secondary traumatic stress.
“I see these nurses running down hospital hallways, covered in blood from patients whose lives are literally hanging on a thread,” she said. “They’re dealing with so much stress and grief and hardship. And then to see them with us, playing and laughing — those deep belly laughs that you haven’t done since you were a kid, the deep laughing that comes from deep in your soul. It can be transformational, for them and for you.”
Ms. Rynders remembers one especially healing workshop in which the participants pretended to be astronauts in deep space, using zero gravity to inform their movements. After the exercise, a veteran hospital nurse took Ms. Rynders aside to thank her, mentioning that she was still dealing with grief for her late son, who had died from suicide years earlier.
“She had a lot of guilt around it,” Ms. Rynders remembered. “And she said to me, ‘When I went to space, I felt closer to him.’ It was just this silly little game, but it gave her this lightness that she hadn’t felt in years. She was able to be free and laugh and play and feel close to her son again.”
Good Medicine
Dr. Cohan, who today is cancer free, said her experience made her completely rethink her relationship with patients. She has danced with more than a few of them, though she’s careful never to force it on them. “I never want to project my idea of joy onto others,” she said. “But more than anything, it’s changed my thinking on what it means to take ownership as a patient.”
The one thing Dr. Cohan never wanted as a patient, and the thing she never wants for her own patients, is the loss of agency. “When I danced, I didn’t feel like I was just handing over my body and begrudgingly accepting what was about to happen to me,” she said. “I was taking ownership around my decision, and I felt connected, really connected, to my surgical team.”
As a patient, Dr. Cohan experienced what she calls the “regimented” atmosphere of medicine. “You’re told where to go, what to do, and you have no control over any of it,” recalled Dr. Cohan, who’s now semiretired and runs retreats for women with breast cancer. “But by bringing in dance, it felt really radical that my healthcare team was doing my thing, not the other way around.”
(Re)Learning to Move More Consciously
Healthcare providers need these moments of escape just as much as patients living with disease. The difference is, as Ms. Rynders points out, those in the medical field aren’t always as aware of their emotional distress. “I think if you ask a nurse, ‘How can I help you? What do you need?’ They’re usually like, ‘I don’t know. I don’t even know what I need,’ ” Ms. Rynders said. “Even if they did know what they needed, I think it’s hard to ask for it and even harder to receive it.”
At Ms. Rynders’ workshops, not everybody is comfortable dancing, of course. So, new participants are always given the option just to witness, to be in the room and watch what happens. “But I also really encourage people to take advantage of this opportunity to do something different and disrupt the way we live on a daily basis,” Ms. Rynders said. “Let your brain try something new and be courageous. We’ve only had a few people who sat on the sidelines the whole time.”
It’s not always just about feelings, Dr. Cohan added, but physical relaxation. “Sometimes it’s just about remembering how to move consciously. When I was having surgery, I didn’t just dance to relax myself. I wanted my entire surgical team to be relaxed.”
For Ms. Rynders, every time she dances with her patients, or with fellow healthcare workers, she’s reminded of her sister and the comfort she was able to give her when no amount of medicine would make things better.
“We don’t always need to be fixed by things,” she said. “Sometimes we just need to be present with one another and be with each other. And sometimes, the best way to do that is by dancing till the tears roll down your cheeks.”
A version of this article appeared on Medscape.com.
In 2012, Tara Rynders’ sister was diagnosed with acute disseminated encephalomyelitis. For Ms. Rynders, a registered nurse in Denver, Colorado, the news was devastating.
“She was this beautiful 26-year-old woman, strong and healthy, and within 12 hours, she went into a coma and couldn’t move or speak,” Ms. Rynders remembered. She flew to her sister in Reno, Nevada, and moved into her intensive care unit room. The helplessness she felt wasn’t just as a sister, but as a healthcare provider.
“As a nurse, we love to fix things,” Ms. Rynders said. “But when my sister was sick, I couldn’t do anything to fix her. The doctors didn’t even know what was going on.”
When Ms. Rynders’ sister woke from the coma, she couldn’t speak. The only comfort Ms. Rynders could provide was her presence and the ability to put a smile on her sister’s face. So, Ms. Rynders did what came naturally ...
She danced.
In that tiny hospital room, she blasted her sister’s favorite song — “Party in the U.S.A.” by Miley Cyrus — and danced around the room, doing anything she could to make her sister laugh.
And this patient who could not form words found her voice.
“She’d holler so deeply, it almost sounded like she was crying,” Ms. Rynders remembered. “The depths of her grief and the depths of her joy coming out simultaneously. It was really amazing and so healing for both of us.”
Do You Know How Powerful Dancing Really Is?
Ms. Rynders is far from the only healthcare professional who’s discovered the healing power of dance. In recent years, doctors and nurses across the country, from Los Angeles, California, to Atlanta, Georgia; from TikTok’s “Dancing Nurse,” Cindy Jones, to Max Chiu, Nebraska’s breakdancing oncologist, have demonstrated that finding new ways to move your body isn’t just good advice for patients but could be exactly what healthcare providers need to stay mentally and physically healthy.
It comes at a time when the field faces a “mental health crisis,” according to a 2023 report from the Centers for Disease Control and Prevention. Medscape Physician Burnout & Depression Report 2024 found current rates of 49% for burnout and 20% for depression.
And medical professionals are often hesitant about seeking help. Nearly 40% of physicians reported reluctance to seek out mental health treatment over fears of professional repercussions, according to 2024 recommendations by the Mayo Clinic.
The solution? It just might be dancing.
There’s ample evidence. A 2024 study from the University of Sydney, Australia, found that dancing offers more psychological and cognitive benefits — helping with everything from depression to motivation to emotional well-being — than any other type of exercise.
Another study, published in February by
Structured dance, where you learn specific movements, can offer a huge boost to mental health, according to a 2024 University of Sydney study. But so does unchoreographed dancing, where you’re basically just letting your limbs do their own thing. A 2021 study, published in Complementary Therapies in Clinical Practice, found that 95% of dancers who just moved their bodies, regardless of how it looked to the outside world, still had huge benefits with depression, anxiety, and trauma.
How to Turn a Mastectomy Into a Dance Party
Deborah Cohan, MD, 55, an obstetrician at Zuckerberg San Francisco General Hospital and Trauma Center, San Francisco, California, discovered firsthand the power of dance back in 2013. After finding a lump in her breast during a self-exam, Dr. Cohan feared the worst. Days later, her radiologist confirmed she had invasive ductal carcinoma.
“It was a complete shock,” Dr. Cohan remembered. “I took care of myself. I ate right. I had no obvious risk factors. I did work the night shift, and there’s actually an increased risk for breast cancer among ob.gyn. workers who do night shift work. But still, it took me completely by surprise. My kids were 5 and 8 at the time, and I was terrified that they’d grow up without a mom.”
So, Dr. Cohan turned to the only thing that gave her comfort — dance class. Dancing had been an escape for Dr. Cohan since she took her first ballet class at age 3. So, she skipped work and went to her weekly Soul Motion dance class, where she found herself doing the exact opposite of escaping. She embraced her fears.
“I visualized death as a dance partner,” Dr. Cohan said. “I felt a freedom come over my body. It didn’t make sense to me at the time, but it was almost joyful. Not that I was accepting death or anticipating death, but just that I acknowledged its presence. There’s so much pressure among people with cancer to be positive. [But] that’s something that needs to come from within a person, not from outside. Nobody can dictate how someone should be feeling. And as I danced, I was genuinely feeling joy even as I recognized my own fears and didn’t turn away from them. I was experiencing all the emotions at once. It was such a relief to realize this wasn’t all going to be about sadness.”
The experience was so healing for Dr. Cohan that she decided to see if she could bring those same feelings into her bilateral mastectomy. When meeting with her surgical team, Dr. Cohan made an unorthodox request: Could her pre-op include a dance party?
“I asked the anesthesiologist in the pre-op appointment if I could dance, and he said yes,” she remembered, laughing. “And then I checked with the surgeon, and he said yes. And then I asked the perioperative nurse, and he said yes, ‘but only if you don’t make me dance, too’. So somehow it all came together.”
Dr. Cohan decided on the Beyoncé song “Get Me Bodied,” which she says resonated with her because “it’s all about being in your body and being your full self. I was like, that is exactly how I want to show up in the operating room.” The moment the music kicked in and Dr. Cohan broke into dance, all of her stress melted away.
“Even though I’d been given permission to dance, I never expected anybody else to join in,” Dr. Cohan said. But that’s exactly what they did. A friend took a video, which shows Dr. Cohan in a hospital gown and bouffant cap, dancing alongside her surgical and anesthesia teams, all of whom are dressed in scrubs, at Mount Zion Hospital in San Francisco, California.
“It’s weird to say, especially about a mastectomy,” Dr. Cohan said, “but it was one of the most joyful moments of my life.”
The video’s been viewed 8.4 million times and is so inspirational — we dare you to watch it and not want to jump out of your chair to dance — that soon others were following Dr. Cohan’s lead.
- Sixteen-year-old Amari Hall danced to celebrate her successful heart transplant.
- Ana-Alecia Ayala, a 32-year-old uterine cancer survivor, danced along to “Juju on That Beat” to make chemotherapy more tolerable.
- Doreta Norris, a patient with breast cancer, chose “Gangnam Style” to serenade her into surgery.
Bringing Dance to Other Medical Pros
Ms. Rynders realized the true power of dance years before her sister’s illness, when her mother died of cancer. “I’ve always considered myself to be very resilient as a human, but I couldn’t bounce back after my mom died,” she said. “I was nursing full time in the emergency room, and I was sad all the time. And then one day I realized, you know what brings me joy? It’s always been dance.”
She went back to school to get her Master of Fine Arts in Dance from the University of Colorado at Boulder, which she believes helped her heal. “I was actually able to grieve instead of just pretending I was okay,” she said.
Inspired by these experiences, Ms. Rynders founded The Clinic in 2017, a company that provides dance workshops for healthcare professionals struggling with burnout and secondary traumatic stress.
“I see these nurses running down hospital hallways, covered in blood from patients whose lives are literally hanging on a thread,” she said. “They’re dealing with so much stress and grief and hardship. And then to see them with us, playing and laughing — those deep belly laughs that you haven’t done since you were a kid, the deep laughing that comes from deep in your soul. It can be transformational, for them and for you.”
Ms. Rynders remembers one especially healing workshop in which the participants pretended to be astronauts in deep space, using zero gravity to inform their movements. After the exercise, a veteran hospital nurse took Ms. Rynders aside to thank her, mentioning that she was still dealing with grief for her late son, who had died from suicide years earlier.
“She had a lot of guilt around it,” Ms. Rynders remembered. “And she said to me, ‘When I went to space, I felt closer to him.’ It was just this silly little game, but it gave her this lightness that she hadn’t felt in years. She was able to be free and laugh and play and feel close to her son again.”
Good Medicine
Dr. Cohan, who today is cancer free, said her experience made her completely rethink her relationship with patients. She has danced with more than a few of them, though she’s careful never to force it on them. “I never want to project my idea of joy onto others,” she said. “But more than anything, it’s changed my thinking on what it means to take ownership as a patient.”
The one thing Dr. Cohan never wanted as a patient, and the thing she never wants for her own patients, is the loss of agency. “When I danced, I didn’t feel like I was just handing over my body and begrudgingly accepting what was about to happen to me,” she said. “I was taking ownership around my decision, and I felt connected, really connected, to my surgical team.”
As a patient, Dr. Cohan experienced what she calls the “regimented” atmosphere of medicine. “You’re told where to go, what to do, and you have no control over any of it,” recalled Dr. Cohan, who’s now semiretired and runs retreats for women with breast cancer. “But by bringing in dance, it felt really radical that my healthcare team was doing my thing, not the other way around.”
(Re)Learning to Move More Consciously
Healthcare providers need these moments of escape just as much as patients living with disease. The difference is, as Ms. Rynders points out, those in the medical field aren’t always as aware of their emotional distress. “I think if you ask a nurse, ‘How can I help you? What do you need?’ They’re usually like, ‘I don’t know. I don’t even know what I need,’ ” Ms. Rynders said. “Even if they did know what they needed, I think it’s hard to ask for it and even harder to receive it.”
At Ms. Rynders’ workshops, not everybody is comfortable dancing, of course. So, new participants are always given the option just to witness, to be in the room and watch what happens. “But I also really encourage people to take advantage of this opportunity to do something different and disrupt the way we live on a daily basis,” Ms. Rynders said. “Let your brain try something new and be courageous. We’ve only had a few people who sat on the sidelines the whole time.”
It’s not always just about feelings, Dr. Cohan added, but physical relaxation. “Sometimes it’s just about remembering how to move consciously. When I was having surgery, I didn’t just dance to relax myself. I wanted my entire surgical team to be relaxed.”
For Ms. Rynders, every time she dances with her patients, or with fellow healthcare workers, she’s reminded of her sister and the comfort she was able to give her when no amount of medicine would make things better.
“We don’t always need to be fixed by things,” she said. “Sometimes we just need to be present with one another and be with each other. And sometimes, the best way to do that is by dancing till the tears roll down your cheeks.”
A version of this article appeared on Medscape.com.
FDA Rejects MDMA-AT for PTSD, but Lykos, Others, Vow to Push on
The Food and Drug Administration’s (FDA) decision not to approve midomafetamine-assisted therapy (MDMA-AT) for posttraumatic stress disorder (PTSD) puts the therapy’s near-term future in doubt, but officials say the rejection may not knock it out of contention as an eventual therapeutic tool for a variety of conditions.
In August the agency declined to approve the drug with currently available study data and requested that the company conduct an additional phase 3 trial. The agency’s action had potentially devastating consequences for MDMA-AT’s sponsor, Lykos Therapeutics, and was a huge disappointment for researchers, clinicians, and patients who were optimistic that it would be a new option for a condition that affects 13-17 million Americans.
For now, no other company is poised to imminently seek FDA approval for MDMA.
Despite the setback, research into MDMA that combines different psychotherapeutic approaches continues. Currently, there are seven US studies actively recruiting participants, and another 13 are registered with an eye toward starting recruitment, as reported on ClinicalTrials.gov.
The lack of FDA approval “actually increases the opportunity now for us to do trials,” said Michael Ostacher, MD, professor of psychiatry and behavioral sciences at Stanford Medicine in California. Researchers won’t have to be sponsored by Lykos to get access to MDMA.
“There’s a lot of energy and interest in doing these studies,” he said in an interview, adding that philanthropic organizations and Veterans Affairs (VA) are contributing funds to support such studies.
The VA provided a statement saying that it “intends to gather rigorous scientific evidence on the potential efficacy and safety of psychedelic compounds when used in conjunction with psychotherapy.” It also noted that “these studies will be conducted under stringent safety protocols and will mark the first time since the 1960’s that VA is funding research on such compounds.”
Rachel Yehuda, PhD, director of the Center for Psychedelic Therapy Research at Icahn School of Medicine at Mount Sinai in New York City, said in an interview that the FDA rejection “raises questions about how to keep the work going.”
Without the FDA’s imprimatur, MDMA remains a schedule 1 drug, which means it has no valid medical use.
“It’s a lot more complicated and expensive to work with a scheduled compound than to work with a compound that has been approved,” Dr. Yehuda said.
Also, without Lykos or another drug company sponsor, investigators have to find an acceptable MDMA source on their own, said Dr. Yehuda, who was an investigator on a study in which Lykos provided MDMA but was not involved in study design, data collection, analysis, or manuscript preparation.
Lykos in Disarray
Within a week of the FDA’s decision, Lykos announced it was cutting its staff by 75% and that Rick Doblin, PhD, the founder and president of the Multidisciplinary Association for Psychedelic Studies (MAPS) that gave rise to Lykos, had resigned from the Lykos board.
A frequently controversial figure, Doblin has been attempting to legitimize MDMA as a therapy since the mid-1980s. He formed a public benefit corporation (PBC) in 2014 with an eye toward FDA approval. The PBC fully separated from MAPS in 2024 and became Lykos.
Although the FDA has left the door open to approval, Lykos has not released the agency’s complete response letter, so it’s not clear exactly what the FDA is seeking. In a statement, the company said it believes the issues “can be addressed with existing data, postapproval requirements, or through reference to the scientific literature.”
Lykos said in an email that it is working on “securing the meeting with the FDA” and that it “will work with the agency to determine what needs to be done to fulfill their requests.”
Soon after the FDA decision, Lykos was hit with another blow. The journal Psychopharmacology retracted an article that pooled six Lykos phase 2 studies, claiming the paper’s authors knew about unethical conduct before submission but did not inform the publisher.
Lykos said the issues could have been addressed through a correction and that it has filed a complaint with the Committee on Publication Ethics. It also noted that the misconduct at issue was reported to the FDA and Health Canada.
“However, we did not disclose the violations to the journal itself, an additional step we should have taken and regret not doing,” the company said. It added that the efficacy data in the paper were not part of the FDA submission.
Author Allison A. Feduccia, PhD, cofounder of Psychedelic Support, agreed with the retraction but disagreed with the wording. In a post on LinkedIn, she said she and other authors were not informed about the misconduct until years after the study’s submission.
Four authors — including Dr. Doblin — disagreed with the retraction.
Dr. Doblin said in a statement that he’d resigned from Lykos to escape the restrictions that came with being a fiduciary. “Now I can advocate and speak freely,” he said, adding that he could also return to his activist roots.
He predicted that Lykos would eventually gain FDA approval. But if Lykos can’t convince the agency, it have the necessary data already in hand; “potential FDA approval is now at least 2 years away, possibly more,” Dr. Doblin said in his statement.
Research Continues
Lykos is not the only company hoping to commercialize MDMA. Toronto-based Awakn Life Sciences has an MDMA preclinical development program for addiction. In addition, some companies are offering MDMA therapy through clinics, such as Numinus in Utah and Sunstone Therapies in Rockville, Maryland.
But Lykos was the closest to bringing a product to market. The company is still a sponsor of four MDMA-related clinical trials, three of which appear to be on hold. One study at the VA San Diego Healthcare System, San Diego, that is actively recruiting is an open-label trial to assess MDMA-AT in combination with brief Cognitive-Behavioral Conjoint Therapy for PTSD.
Those studies are among 13 US trials listed in ClinicalTrials.gov that have not yet begun recruiting and 7 that are actively recruiting.
Among them is a study of MDMA plus exposure therapy, funded by and conducted at Emory University in Atlanta. One of the Emory principal investigators, Barbara Rothbaum, MD, has also been named to a Lykos’ panel that would help ensure oversight of MDMA-AT post FDA approval.
Dr. Ostacher is an investigator in a study planned at VA Palo Alto Health Care System in California, that will compare MDMA-AT with cognitive processing therapy in veterans with severe PTSD. He said it will be open label in an effort to minimize expectation bias and issues with blinding — both problems that tripped up the Lykos application. Although placebo-controlled trials are the gold standard, it’s not ideal when “the purpose of the drug is for it to change how you see the world and yourself,” Dr. Ostacher said.
The study aims to see whether MDMA-AT is better than “a much shorter, less onerous, but quite evidence-based psychotherapy for PTSD,” he said.
The FDA’s decision is not the end of the road, said Dr. Ostacher. “Even though I think this makes for an obvious delay, I don’t think that it’s a permanent one,” he said.
Dr. Yehuda also said she is not ready to give up.
“We don’t plan on stopping — we plan on finding a way,” she said.
“In our experience, this is a very powerful approach that helps a lot of people that haven’t found help using other approaches, and when it’s in the hands of really trusted, experienced, ethical clinicians in a trusted environment, this could be a real game changer for people who have not been able to find belief by traditional methods,” she said.
Dr. Ostacher reported no relevant financial relationships. Dr. Yahuda is the principal investigator on clinical trials for the Center for Psychedelic Psychotherapy and Trauma Research that are sponsored by the Multidisciplinary Association for Psychedelic Studies and COMPASS Pathways.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration’s (FDA) decision not to approve midomafetamine-assisted therapy (MDMA-AT) for posttraumatic stress disorder (PTSD) puts the therapy’s near-term future in doubt, but officials say the rejection may not knock it out of contention as an eventual therapeutic tool for a variety of conditions.
In August the agency declined to approve the drug with currently available study data and requested that the company conduct an additional phase 3 trial. The agency’s action had potentially devastating consequences for MDMA-AT’s sponsor, Lykos Therapeutics, and was a huge disappointment for researchers, clinicians, and patients who were optimistic that it would be a new option for a condition that affects 13-17 million Americans.
For now, no other company is poised to imminently seek FDA approval for MDMA.
Despite the setback, research into MDMA that combines different psychotherapeutic approaches continues. Currently, there are seven US studies actively recruiting participants, and another 13 are registered with an eye toward starting recruitment, as reported on ClinicalTrials.gov.
The lack of FDA approval “actually increases the opportunity now for us to do trials,” said Michael Ostacher, MD, professor of psychiatry and behavioral sciences at Stanford Medicine in California. Researchers won’t have to be sponsored by Lykos to get access to MDMA.
“There’s a lot of energy and interest in doing these studies,” he said in an interview, adding that philanthropic organizations and Veterans Affairs (VA) are contributing funds to support such studies.
The VA provided a statement saying that it “intends to gather rigorous scientific evidence on the potential efficacy and safety of psychedelic compounds when used in conjunction with psychotherapy.” It also noted that “these studies will be conducted under stringent safety protocols and will mark the first time since the 1960’s that VA is funding research on such compounds.”
Rachel Yehuda, PhD, director of the Center for Psychedelic Therapy Research at Icahn School of Medicine at Mount Sinai in New York City, said in an interview that the FDA rejection “raises questions about how to keep the work going.”
Without the FDA’s imprimatur, MDMA remains a schedule 1 drug, which means it has no valid medical use.
“It’s a lot more complicated and expensive to work with a scheduled compound than to work with a compound that has been approved,” Dr. Yehuda said.
Also, without Lykos or another drug company sponsor, investigators have to find an acceptable MDMA source on their own, said Dr. Yehuda, who was an investigator on a study in which Lykos provided MDMA but was not involved in study design, data collection, analysis, or manuscript preparation.
Lykos in Disarray
Within a week of the FDA’s decision, Lykos announced it was cutting its staff by 75% and that Rick Doblin, PhD, the founder and president of the Multidisciplinary Association for Psychedelic Studies (MAPS) that gave rise to Lykos, had resigned from the Lykos board.
A frequently controversial figure, Doblin has been attempting to legitimize MDMA as a therapy since the mid-1980s. He formed a public benefit corporation (PBC) in 2014 with an eye toward FDA approval. The PBC fully separated from MAPS in 2024 and became Lykos.
Although the FDA has left the door open to approval, Lykos has not released the agency’s complete response letter, so it’s not clear exactly what the FDA is seeking. In a statement, the company said it believes the issues “can be addressed with existing data, postapproval requirements, or through reference to the scientific literature.”
Lykos said in an email that it is working on “securing the meeting with the FDA” and that it “will work with the agency to determine what needs to be done to fulfill their requests.”
Soon after the FDA decision, Lykos was hit with another blow. The journal Psychopharmacology retracted an article that pooled six Lykos phase 2 studies, claiming the paper’s authors knew about unethical conduct before submission but did not inform the publisher.
Lykos said the issues could have been addressed through a correction and that it has filed a complaint with the Committee on Publication Ethics. It also noted that the misconduct at issue was reported to the FDA and Health Canada.
“However, we did not disclose the violations to the journal itself, an additional step we should have taken and regret not doing,” the company said. It added that the efficacy data in the paper were not part of the FDA submission.
Author Allison A. Feduccia, PhD, cofounder of Psychedelic Support, agreed with the retraction but disagreed with the wording. In a post on LinkedIn, she said she and other authors were not informed about the misconduct until years after the study’s submission.
Four authors — including Dr. Doblin — disagreed with the retraction.
Dr. Doblin said in a statement that he’d resigned from Lykos to escape the restrictions that came with being a fiduciary. “Now I can advocate and speak freely,” he said, adding that he could also return to his activist roots.
He predicted that Lykos would eventually gain FDA approval. But if Lykos can’t convince the agency, it have the necessary data already in hand; “potential FDA approval is now at least 2 years away, possibly more,” Dr. Doblin said in his statement.
Research Continues
Lykos is not the only company hoping to commercialize MDMA. Toronto-based Awakn Life Sciences has an MDMA preclinical development program for addiction. In addition, some companies are offering MDMA therapy through clinics, such as Numinus in Utah and Sunstone Therapies in Rockville, Maryland.
But Lykos was the closest to bringing a product to market. The company is still a sponsor of four MDMA-related clinical trials, three of which appear to be on hold. One study at the VA San Diego Healthcare System, San Diego, that is actively recruiting is an open-label trial to assess MDMA-AT in combination with brief Cognitive-Behavioral Conjoint Therapy for PTSD.
Those studies are among 13 US trials listed in ClinicalTrials.gov that have not yet begun recruiting and 7 that are actively recruiting.
Among them is a study of MDMA plus exposure therapy, funded by and conducted at Emory University in Atlanta. One of the Emory principal investigators, Barbara Rothbaum, MD, has also been named to a Lykos’ panel that would help ensure oversight of MDMA-AT post FDA approval.
Dr. Ostacher is an investigator in a study planned at VA Palo Alto Health Care System in California, that will compare MDMA-AT with cognitive processing therapy in veterans with severe PTSD. He said it will be open label in an effort to minimize expectation bias and issues with blinding — both problems that tripped up the Lykos application. Although placebo-controlled trials are the gold standard, it’s not ideal when “the purpose of the drug is for it to change how you see the world and yourself,” Dr. Ostacher said.
The study aims to see whether MDMA-AT is better than “a much shorter, less onerous, but quite evidence-based psychotherapy for PTSD,” he said.
The FDA’s decision is not the end of the road, said Dr. Ostacher. “Even though I think this makes for an obvious delay, I don’t think that it’s a permanent one,” he said.
Dr. Yehuda also said she is not ready to give up.
“We don’t plan on stopping — we plan on finding a way,” she said.
“In our experience, this is a very powerful approach that helps a lot of people that haven’t found help using other approaches, and when it’s in the hands of really trusted, experienced, ethical clinicians in a trusted environment, this could be a real game changer for people who have not been able to find belief by traditional methods,” she said.
Dr. Ostacher reported no relevant financial relationships. Dr. Yahuda is the principal investigator on clinical trials for the Center for Psychedelic Psychotherapy and Trauma Research that are sponsored by the Multidisciplinary Association for Psychedelic Studies and COMPASS Pathways.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration’s (FDA) decision not to approve midomafetamine-assisted therapy (MDMA-AT) for posttraumatic stress disorder (PTSD) puts the therapy’s near-term future in doubt, but officials say the rejection may not knock it out of contention as an eventual therapeutic tool for a variety of conditions.
In August the agency declined to approve the drug with currently available study data and requested that the company conduct an additional phase 3 trial. The agency’s action had potentially devastating consequences for MDMA-AT’s sponsor, Lykos Therapeutics, and was a huge disappointment for researchers, clinicians, and patients who were optimistic that it would be a new option for a condition that affects 13-17 million Americans.
For now, no other company is poised to imminently seek FDA approval for MDMA.
Despite the setback, research into MDMA that combines different psychotherapeutic approaches continues. Currently, there are seven US studies actively recruiting participants, and another 13 are registered with an eye toward starting recruitment, as reported on ClinicalTrials.gov.
The lack of FDA approval “actually increases the opportunity now for us to do trials,” said Michael Ostacher, MD, professor of psychiatry and behavioral sciences at Stanford Medicine in California. Researchers won’t have to be sponsored by Lykos to get access to MDMA.
“There’s a lot of energy and interest in doing these studies,” he said in an interview, adding that philanthropic organizations and Veterans Affairs (VA) are contributing funds to support such studies.
The VA provided a statement saying that it “intends to gather rigorous scientific evidence on the potential efficacy and safety of psychedelic compounds when used in conjunction with psychotherapy.” It also noted that “these studies will be conducted under stringent safety protocols and will mark the first time since the 1960’s that VA is funding research on such compounds.”
Rachel Yehuda, PhD, director of the Center for Psychedelic Therapy Research at Icahn School of Medicine at Mount Sinai in New York City, said in an interview that the FDA rejection “raises questions about how to keep the work going.”
Without the FDA’s imprimatur, MDMA remains a schedule 1 drug, which means it has no valid medical use.
“It’s a lot more complicated and expensive to work with a scheduled compound than to work with a compound that has been approved,” Dr. Yehuda said.
Also, without Lykos or another drug company sponsor, investigators have to find an acceptable MDMA source on their own, said Dr. Yehuda, who was an investigator on a study in which Lykos provided MDMA but was not involved in study design, data collection, analysis, or manuscript preparation.
Lykos in Disarray
Within a week of the FDA’s decision, Lykos announced it was cutting its staff by 75% and that Rick Doblin, PhD, the founder and president of the Multidisciplinary Association for Psychedelic Studies (MAPS) that gave rise to Lykos, had resigned from the Lykos board.
A frequently controversial figure, Doblin has been attempting to legitimize MDMA as a therapy since the mid-1980s. He formed a public benefit corporation (PBC) in 2014 with an eye toward FDA approval. The PBC fully separated from MAPS in 2024 and became Lykos.
Although the FDA has left the door open to approval, Lykos has not released the agency’s complete response letter, so it’s not clear exactly what the FDA is seeking. In a statement, the company said it believes the issues “can be addressed with existing data, postapproval requirements, or through reference to the scientific literature.”
Lykos said in an email that it is working on “securing the meeting with the FDA” and that it “will work with the agency to determine what needs to be done to fulfill their requests.”
Soon after the FDA decision, Lykos was hit with another blow. The journal Psychopharmacology retracted an article that pooled six Lykos phase 2 studies, claiming the paper’s authors knew about unethical conduct before submission but did not inform the publisher.
Lykos said the issues could have been addressed through a correction and that it has filed a complaint with the Committee on Publication Ethics. It also noted that the misconduct at issue was reported to the FDA and Health Canada.
“However, we did not disclose the violations to the journal itself, an additional step we should have taken and regret not doing,” the company said. It added that the efficacy data in the paper were not part of the FDA submission.
Author Allison A. Feduccia, PhD, cofounder of Psychedelic Support, agreed with the retraction but disagreed with the wording. In a post on LinkedIn, she said she and other authors were not informed about the misconduct until years after the study’s submission.
Four authors — including Dr. Doblin — disagreed with the retraction.
Dr. Doblin said in a statement that he’d resigned from Lykos to escape the restrictions that came with being a fiduciary. “Now I can advocate and speak freely,” he said, adding that he could also return to his activist roots.
He predicted that Lykos would eventually gain FDA approval. But if Lykos can’t convince the agency, it have the necessary data already in hand; “potential FDA approval is now at least 2 years away, possibly more,” Dr. Doblin said in his statement.
Research Continues
Lykos is not the only company hoping to commercialize MDMA. Toronto-based Awakn Life Sciences has an MDMA preclinical development program for addiction. In addition, some companies are offering MDMA therapy through clinics, such as Numinus in Utah and Sunstone Therapies in Rockville, Maryland.
But Lykos was the closest to bringing a product to market. The company is still a sponsor of four MDMA-related clinical trials, three of which appear to be on hold. One study at the VA San Diego Healthcare System, San Diego, that is actively recruiting is an open-label trial to assess MDMA-AT in combination with brief Cognitive-Behavioral Conjoint Therapy for PTSD.
Those studies are among 13 US trials listed in ClinicalTrials.gov that have not yet begun recruiting and 7 that are actively recruiting.
Among them is a study of MDMA plus exposure therapy, funded by and conducted at Emory University in Atlanta. One of the Emory principal investigators, Barbara Rothbaum, MD, has also been named to a Lykos’ panel that would help ensure oversight of MDMA-AT post FDA approval.
Dr. Ostacher is an investigator in a study planned at VA Palo Alto Health Care System in California, that will compare MDMA-AT with cognitive processing therapy in veterans with severe PTSD. He said it will be open label in an effort to minimize expectation bias and issues with blinding — both problems that tripped up the Lykos application. Although placebo-controlled trials are the gold standard, it’s not ideal when “the purpose of the drug is for it to change how you see the world and yourself,” Dr. Ostacher said.
The study aims to see whether MDMA-AT is better than “a much shorter, less onerous, but quite evidence-based psychotherapy for PTSD,” he said.
The FDA’s decision is not the end of the road, said Dr. Ostacher. “Even though I think this makes for an obvious delay, I don’t think that it’s a permanent one,” he said.
Dr. Yehuda also said she is not ready to give up.
“We don’t plan on stopping — we plan on finding a way,” she said.
“In our experience, this is a very powerful approach that helps a lot of people that haven’t found help using other approaches, and when it’s in the hands of really trusted, experienced, ethical clinicians in a trusted environment, this could be a real game changer for people who have not been able to find belief by traditional methods,” she said.
Dr. Ostacher reported no relevant financial relationships. Dr. Yahuda is the principal investigator on clinical trials for the Center for Psychedelic Psychotherapy and Trauma Research that are sponsored by the Multidisciplinary Association for Psychedelic Studies and COMPASS Pathways.
A version of this article first appeared on Medscape.com.
Involuntary flashbacks
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 28-year-old man presented to the emergency department following a high-speed motor vehicle accident 2 months ago. He sustained no major physical injuries but had minor lacerations and bruising. The patient reported feeling unusually irritable and having difficulty sleeping since the accident, citing frequent flashbacks to the accident and occasional nightmares. He has started to feel more anxious and withdrawn, losing interest in hobbies such as swimming and biking that he previously enjoyed.
The patient's medical history is unremarkable, with no previous psychiatric or neurologic conditions. His neurologic examination was normal. An initial axial T2-weighted brain MRI demonstrated multiple small areas of hemorrhage, indicative of a diffuse axonal injury or shear-type injury. Despite the lack of significant physical injuries, the patient expressed ongoing distress related to the traumatic event.
Persistent mood swings
The most likely diagnosis for this patient is veteran posttraumatic stress disorder (PTSD), given his history of combat exposure and symptoms, such as severe headaches, difficulty concentrating, mood swings, nightmares, flashbacks, increased startle response, and hypervigilance. MRI findings showing significant changes in the limbic system and hippocampal regions support this diagnosis. Other potential diagnoses, like traumatic brain injury, chronic migraine, and major depressive disorder, are less likely because of their inability to account for the full range of his symptoms and specific MRI abnormalities.
PTSD, experienced by a subset of individuals after exposure to life-threatening events, has a lifetime prevalence of 4%-7% and a current prevalence of 1%-3%, with higher rates in older women, those with more trauma, and combat veterans. Nearly half of US veterans are aged 65 or older, many being Vietnam-era veterans at elevated risk for PTSD. Prevalence rates in older veterans range between 1% and 22%.
PTSD is characterized by intrusive thoughts, flashbacks, nightmares, avoidance of reminders, hypervigilance, and sleep difficulties, significantly disrupting interpersonal and occupational functioning. Screening tools like the primary care (PC) PTSD-5 and PCL-5, used in primary care settings, are effective for early detection, provisional diagnosis, and monitoring of symptom changes. The clinician-administered PTSD scale for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition DSM-5 (CAPS-5) is the gold standard for diagnosis, particularly among veterans, with multimethod assessments combining self-report measures and semi-structured interviews recommended for accuracy. The DSM-5 criteria for PTSD diagnosis describe exposure to traumatic events, intrusion symptoms, avoidance behaviors, negative mood, and altered arousal, with symptoms persisting for over a month and causing significant distress or functional impairment.
Research has identified consistent anatomical and functional changes in PTSD patients, such as smaller hippocampi, decreased corpus callosum and prefrontal cortex, increased amygdala reactivity, and decreased prefrontal cortex activity. PTSD, linked to alterations in brain regions involved in fear learning and memory, shows diminished structural integrity in executive function areas, reduced cortical volumes in the cingulate brain cortex and frontal regions, and reduced white matter integrity in key brain pathways. Neuroimaging findings, however, are primarily used for research currently and have yet to be widely implemented in clinical guidelines.
International PTSD treatment guidelines consistently recognize trauma-focused cognitive-behavioral therapies (CBTs), such as cognitive processing therapy (CPT), prolonged exposure (PE), and eye movement desensitization and reprocessing (EMDR) as the gold standard. Recent guidelines have expanded the list of recommended treatments: The 2023 Department of Veterans Affairs and Department of Defense guidelines in the United States also endorse therapies like written narrative exposure and brief eclectic therapy. Internationally, guidelines do not perfectly coincide, as the 2018 update from the United Kingdom's National Institute for Health and Care Excellence (NICE) gives the highest recommendations to PE and CPT but rates EMDR slightly lower for military veterans because of limited evidence. Overall, guidelines consistently advocate for trauma-focused psychological interventions as the primary treatment for PTSD.
Guidelines from NICE and the World Health Organization do not recommend medications as the primary treatment; the American Psychiatric Association and the US Department of Veterans Affairs support selective serotonin reuptake inhibitors and prazosin but advise against benzodiazepines. Inpatient care may be necessary for individuals who pose a danger to themselves or others, or for those with severe PTSD from childhood abuse, to aid in emotional regulation and treatment.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The most likely diagnosis for this patient is veteran posttraumatic stress disorder (PTSD), given his history of combat exposure and symptoms, such as severe headaches, difficulty concentrating, mood swings, nightmares, flashbacks, increased startle response, and hypervigilance. MRI findings showing significant changes in the limbic system and hippocampal regions support this diagnosis. Other potential diagnoses, like traumatic brain injury, chronic migraine, and major depressive disorder, are less likely because of their inability to account for the full range of his symptoms and specific MRI abnormalities.
PTSD, experienced by a subset of individuals after exposure to life-threatening events, has a lifetime prevalence of 4%-7% and a current prevalence of 1%-3%, with higher rates in older women, those with more trauma, and combat veterans. Nearly half of US veterans are aged 65 or older, many being Vietnam-era veterans at elevated risk for PTSD. Prevalence rates in older veterans range between 1% and 22%.
PTSD is characterized by intrusive thoughts, flashbacks, nightmares, avoidance of reminders, hypervigilance, and sleep difficulties, significantly disrupting interpersonal and occupational functioning. Screening tools like the primary care (PC) PTSD-5 and PCL-5, used in primary care settings, are effective for early detection, provisional diagnosis, and monitoring of symptom changes. The clinician-administered PTSD scale for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition DSM-5 (CAPS-5) is the gold standard for diagnosis, particularly among veterans, with multimethod assessments combining self-report measures and semi-structured interviews recommended for accuracy. The DSM-5 criteria for PTSD diagnosis describe exposure to traumatic events, intrusion symptoms, avoidance behaviors, negative mood, and altered arousal, with symptoms persisting for over a month and causing significant distress or functional impairment.
Research has identified consistent anatomical and functional changes in PTSD patients, such as smaller hippocampi, decreased corpus callosum and prefrontal cortex, increased amygdala reactivity, and decreased prefrontal cortex activity. PTSD, linked to alterations in brain regions involved in fear learning and memory, shows diminished structural integrity in executive function areas, reduced cortical volumes in the cingulate brain cortex and frontal regions, and reduced white matter integrity in key brain pathways. Neuroimaging findings, however, are primarily used for research currently and have yet to be widely implemented in clinical guidelines.
International PTSD treatment guidelines consistently recognize trauma-focused cognitive-behavioral therapies (CBTs), such as cognitive processing therapy (CPT), prolonged exposure (PE), and eye movement desensitization and reprocessing (EMDR) as the gold standard. Recent guidelines have expanded the list of recommended treatments: The 2023 Department of Veterans Affairs and Department of Defense guidelines in the United States also endorse therapies like written narrative exposure and brief eclectic therapy. Internationally, guidelines do not perfectly coincide, as the 2018 update from the United Kingdom's National Institute for Health and Care Excellence (NICE) gives the highest recommendations to PE and CPT but rates EMDR slightly lower for military veterans because of limited evidence. Overall, guidelines consistently advocate for trauma-focused psychological interventions as the primary treatment for PTSD.
Guidelines from NICE and the World Health Organization do not recommend medications as the primary treatment; the American Psychiatric Association and the US Department of Veterans Affairs support selective serotonin reuptake inhibitors and prazosin but advise against benzodiazepines. Inpatient care may be necessary for individuals who pose a danger to themselves or others, or for those with severe PTSD from childhood abuse, to aid in emotional regulation and treatment.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The most likely diagnosis for this patient is veteran posttraumatic stress disorder (PTSD), given his history of combat exposure and symptoms, such as severe headaches, difficulty concentrating, mood swings, nightmares, flashbacks, increased startle response, and hypervigilance. MRI findings showing significant changes in the limbic system and hippocampal regions support this diagnosis. Other potential diagnoses, like traumatic brain injury, chronic migraine, and major depressive disorder, are less likely because of their inability to account for the full range of his symptoms and specific MRI abnormalities.
PTSD, experienced by a subset of individuals after exposure to life-threatening events, has a lifetime prevalence of 4%-7% and a current prevalence of 1%-3%, with higher rates in older women, those with more trauma, and combat veterans. Nearly half of US veterans are aged 65 or older, many being Vietnam-era veterans at elevated risk for PTSD. Prevalence rates in older veterans range between 1% and 22%.
PTSD is characterized by intrusive thoughts, flashbacks, nightmares, avoidance of reminders, hypervigilance, and sleep difficulties, significantly disrupting interpersonal and occupational functioning. Screening tools like the primary care (PC) PTSD-5 and PCL-5, used in primary care settings, are effective for early detection, provisional diagnosis, and monitoring of symptom changes. The clinician-administered PTSD scale for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition DSM-5 (CAPS-5) is the gold standard for diagnosis, particularly among veterans, with multimethod assessments combining self-report measures and semi-structured interviews recommended for accuracy. The DSM-5 criteria for PTSD diagnosis describe exposure to traumatic events, intrusion symptoms, avoidance behaviors, negative mood, and altered arousal, with symptoms persisting for over a month and causing significant distress or functional impairment.
Research has identified consistent anatomical and functional changes in PTSD patients, such as smaller hippocampi, decreased corpus callosum and prefrontal cortex, increased amygdala reactivity, and decreased prefrontal cortex activity. PTSD, linked to alterations in brain regions involved in fear learning and memory, shows diminished structural integrity in executive function areas, reduced cortical volumes in the cingulate brain cortex and frontal regions, and reduced white matter integrity in key brain pathways. Neuroimaging findings, however, are primarily used for research currently and have yet to be widely implemented in clinical guidelines.
International PTSD treatment guidelines consistently recognize trauma-focused cognitive-behavioral therapies (CBTs), such as cognitive processing therapy (CPT), prolonged exposure (PE), and eye movement desensitization and reprocessing (EMDR) as the gold standard. Recent guidelines have expanded the list of recommended treatments: The 2023 Department of Veterans Affairs and Department of Defense guidelines in the United States also endorse therapies like written narrative exposure and brief eclectic therapy. Internationally, guidelines do not perfectly coincide, as the 2018 update from the United Kingdom's National Institute for Health and Care Excellence (NICE) gives the highest recommendations to PE and CPT but rates EMDR slightly lower for military veterans because of limited evidence. Overall, guidelines consistently advocate for trauma-focused psychological interventions as the primary treatment for PTSD.
Guidelines from NICE and the World Health Organization do not recommend medications as the primary treatment; the American Psychiatric Association and the US Department of Veterans Affairs support selective serotonin reuptake inhibitors and prazosin but advise against benzodiazepines. Inpatient care may be necessary for individuals who pose a danger to themselves or others, or for those with severe PTSD from childhood abuse, to aid in emotional regulation and treatment.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 35-year-old male veteran presents with a history of severe headaches, difficulty concentrating, and persistent mood swings. He served multiple tours in a combat zone, where he was exposed to several traumatic events, including the loss of close friends. His medical history reveals previous diagnoses of insomnia and anxiety, for which he has been prescribed various medications over the years with limited success. During his clinical evaluation, he describes frequent nightmares and flashbacks related to his time in service. He reports an increased startle response and hypervigilance, often feeling on edge and irritable. A recent MRI of the brain, as shown in the image here, reveals significant changes in the limbic system, with abnormalities in the hippocampal regions. Laboratory tests and physical exams are otherwise unremarkable, but his mental health assessment indicates severe distress, which is affecting his daily functioning and interpersonal relationships.
PTSD Workup
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
PTSD: The Basics
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
PTSD Needs a New Name, Experts Say — Here’s Why
In a bid to reduce stigma and improve treatment rates, for inclusion in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). The APA’s policy is that a rolling name change is available if the current term is determined to be harmful.
Currently led by anesthesiologist Eugene Lipov, MD, clinical assistant professor, University of Illinois Chicago, and chief medical officer of Stella Center, also in Chicago, the formal request for the proposed name change to the APA’s DSM-5-TR Steering Committee in August 2023.
The APA Steering Committee rejected the proposed name change in November 2023, citing a “lack of convincing evidence.” However, Dr. Lipov and colleagues remain undeterred and continue to advocate for the change.
“The word ‘disorder’ is both imprecise and stigmatizing,” Dr. Lipov said. “Because of stigma, many people with PTSD — especially those in the military — don’t get help, which my research has demonstrated.”
Patients are more likely to seek help if their symptoms are framed as manifestations of an injury that is diagnosable and treatable, like a broken leg, Dr. Lipov said. “Stigma can kill in very real ways, since delayed care or lack of care can directly lead to suicides, thus satisfying the reduce harm requirement for the name change.”
Neurobiology of Trauma
Dr. Lipov grew up with a veteran father affected by PTSD and a mother with debilitating depression who eventually took her life. “I understand the impact of trauma very well,” he said.
Although not a psychiatrist, Dr. Lipov pioneered a highly successful treatment for PTSD by adapting an anesthetic technique — the stellate ganglion block (SGB) — to reverse many trauma symptoms through the process of “rebooting.”
This involves reversing the activity of the sympathetic nervous system — the fight-or-flight response — to the pretrauma state by anesthetizing the sympathetic ganglion in the neck. Investigating how SGB can help ameliorate the symptoms of PTSD led him to investigate and describe the neurobiology of PTSD and the mechanism of action of SGB.
The impact of SGD on PTSD was supported by a small neuroimaging study demonstrating that the right amygdala — the area of the brain associated with the fear response — was overactivated in patients with PTSD but that this region was deactivated after the administration of SGB, Dr. Lipov said.
“I believe that psychiatric conditions are actually physiologic brain changes that can be measured by advanced neuroimaging technologies and then physiologically treated,” he stated.
He noted that a growing body of literature suggests that use of the SGB for PTSD can be effective “because PTSD has a neurobiological basis and is essentially caused by an actual injury to the brain.”
A Natural Response, Not a Disorder
Dr. Lipov’s clinical work treating PTSD as a brain injury led him to connect with Frank Ochberg, MD, a founding board member of the International Society for Traumatic Stress Studies, former associate director of the National Institute of Mental Health, and former director of the Michigan Department of Mental Health.
In 2012, Dr. Ochberg teamed up with retired Army General Peter Chiarelli and Jonathan Shay, MD, PhD, author of Achilles in Vietnam: Combat Trauma and the Undoing of Character, to petition the DSM-5 Steering Committee to change the name of PTSD to PTSI in the upcoming DSM-5.
Dr. Ochberg explained that Gen. Chiarelli believed the term “disorder” suggests a preexisting issue prior to enlistment, potentially making an individual appear “weak.” He noted that this stigma is particularly troubling for military personnel, who often avoid seeking so they are not perceived as vulnerable, which can lead to potentially dire consequences, including suicide.
“We received endorsements from many quarters, not only advocates for service members or veterans,” Dr. Ochberg said.
This included feminists like Gloria Steinem, who championed the rights of women who had survived rape, incest, and domestic violence. As one advocate put it: “The natural human reaction to a life-threatening event should not be labeled a disorder.”
The DSM-5 Steering Committee declined to change the name. “Their feeling was that if we change the word ‘disorder’ to something else, we’d have to change every condition in the DSM that’s called a ‘disorder’. And they felt there really was nothing wrong with the word,” said Dr. Ochberg.
However, Dr. Lipov noted that other diagnoses have undergone name changes in the DSM for the sake of accuracy or stigma reduction. For example, the term mental retardation (DSM-IV) was changed to intellectual disability in DSM-5, and gender identity disorder was changed to gender dysphoria.
A decade later, Dr. Lipov decided to try again. To bolster his contention, he conducted a telephone survey of 1025 individuals. Of these, about 50% had a PTSD diagnosis.
Approximately two thirds of respondents agreed that a name change to PTSI would reduce the stigma associated with the term “PTSD.” Over half said it would increase the likelihood they would seek medical help. Those diagnosed with PTSD were most likely to endorse the name change.
Dr. Lipov conducts an ongoing survey of psychiatrists to ascertain their views on the potential name change and hopes to include findings in future research and communication with the DSM-5 Steering Committee. In addition, he has developed a new survey that expands upon his original survey, which specifically looked at individuals with PTSD.
“The new survey includes a wide range of people, many of whom have never been diagnosed. One of the questions we ask is whether they’ve ever heard of PTSD, and then we ask them about their reaction to the term,” he said.
A Barrier to Care
Psychiatrist Marcel Green, MD, director of Hudson Mind in New York City, refers to himself as an “interventional psychiatrist,” as he employs a comprehensive approach that includes not only medication and psychotherapy but also specialized techniques like SBG for severe anxiety-related physical symptoms and certain pain conditions.
Dr. Green, who is not involved in the name change initiative, agrees that the term “disorder” carries more stigma than “injury” for many groups, including those who have experienced childhood trauma, those struggling with substance abuse, or who are from backgrounds or peer groups where seeking mental health care is stigmatized.
Patients like these “are looking to me to give them a language to frame what they’re going through, and I tell them their symptoms are consistent with PTSD,” he said. “But they tell me don’t see themselves as having a disorder, which hinders their pursuit of care.”
Framing the condition as an “injury” also aligns with the approach of using biologic interventions to address the injury. Dr. Green has found SGB helpful in treating substance abuse disorder too, “which is a form of escape from the hyperactivation that accompanies PTSD.” And after the procedure, “they’re more receptive to therapy.”
Unfortunately, said Dr. Lipov, the DSM Steering Committee rejected his proposed name change, stating that the “concept of disorder as a dividing line from, eg, normal reactions to stress, is a core concept in the DSM, and the term has only rarely been removed.”
Moreover, the committee “did not see sufficient evidence ... that the name PTSD is stigmatizing and actually deters people with the disorder from seeking treatment who would not be deterred from doing so by PTSI.”
‘An Avenue for Dignity’
Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness (NAMI), noted that the organization does not have an official position on this issue. However, he shared his own personal perspective.
There may be merit in the proposed name change, said Dr. Duckworth, but more evidence is needed. “If it’s clear, after rigorous studies have been performed and there’s compelling data, that calling it a ‘disorder’ rather than an ‘injury’ is actually preventing people from getting the care they need, then it merits serious attention.”
If so, Dr. Duckworth would be “interested in having a conversation with the policy team at NAMI to start to see if we could activate the DSM Committee.”
Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto in Ontario, Canada, and head of the Mood Disorders Psychopharmacology Unit, said the name change initiative is a “really interesting proposal.”
Dr. McIntyre, chairman and executive director of the Brain and Cognition Discovery Foundation, also in Toronto, who is not involved in the initiative, has also heard “many people say that the term ‘disorder’ is stigmatizing and might even come across as pejorative in some ways.”
By contrast, “the word ‘injury’ parallels physical injury, and what we currently call ‘PTSD’ is a psychological or emotional injury no less devastating than torn tissue or broken bones,” added Dr. McIntyre, who is also the chairman of the board of the Depression and Bipolar Support Alliance.
Dr. Ochberg agreed. “In the military, ‘injury’ opens up an avenue for dignity, for a medal. Being injured and learning how to deal with an injury is part of having yet another honorable task that comes from being an honorable person who did an honorable thing.”
While disappointed, Dr. Lipov does not plan to give up on his vision. “I will continue to amass evidence that the word ‘PTSD’ is stigmatizing and indeed does prevent people from seeking care and will resubmit the proposal to the DSM Steering Committee when I have gathered a larger body of compelling evidence.”
Currently, Dr. Lipov is in active discussions with the special operations force of the US Army to obtain more evidence. “This will be the follow-up to bolster the opinion of Peter Chiarelli,” he said. “It is known that suicide and PTSD are highly related. This is especially urgent and relevant because recent data suggest suicide rate of military personnel in the VA may be as high as 44 per day,” Dr. Lipov said.
Dr. Lipov is the chief medical officer and an investor in the Stella Center. Dr. Green performs SGBs as part of his psychiatric practice. Drs. Ochberg, McIntyre, and Duckworth reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
In a bid to reduce stigma and improve treatment rates, for inclusion in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). The APA’s policy is that a rolling name change is available if the current term is determined to be harmful.
Currently led by anesthesiologist Eugene Lipov, MD, clinical assistant professor, University of Illinois Chicago, and chief medical officer of Stella Center, also in Chicago, the formal request for the proposed name change to the APA’s DSM-5-TR Steering Committee in August 2023.
The APA Steering Committee rejected the proposed name change in November 2023, citing a “lack of convincing evidence.” However, Dr. Lipov and colleagues remain undeterred and continue to advocate for the change.
“The word ‘disorder’ is both imprecise and stigmatizing,” Dr. Lipov said. “Because of stigma, many people with PTSD — especially those in the military — don’t get help, which my research has demonstrated.”
Patients are more likely to seek help if their symptoms are framed as manifestations of an injury that is diagnosable and treatable, like a broken leg, Dr. Lipov said. “Stigma can kill in very real ways, since delayed care or lack of care can directly lead to suicides, thus satisfying the reduce harm requirement for the name change.”
Neurobiology of Trauma
Dr. Lipov grew up with a veteran father affected by PTSD and a mother with debilitating depression who eventually took her life. “I understand the impact of trauma very well,” he said.
Although not a psychiatrist, Dr. Lipov pioneered a highly successful treatment for PTSD by adapting an anesthetic technique — the stellate ganglion block (SGB) — to reverse many trauma symptoms through the process of “rebooting.”
This involves reversing the activity of the sympathetic nervous system — the fight-or-flight response — to the pretrauma state by anesthetizing the sympathetic ganglion in the neck. Investigating how SGB can help ameliorate the symptoms of PTSD led him to investigate and describe the neurobiology of PTSD and the mechanism of action of SGB.
The impact of SGD on PTSD was supported by a small neuroimaging study demonstrating that the right amygdala — the area of the brain associated with the fear response — was overactivated in patients with PTSD but that this region was deactivated after the administration of SGB, Dr. Lipov said.
“I believe that psychiatric conditions are actually physiologic brain changes that can be measured by advanced neuroimaging technologies and then physiologically treated,” he stated.
He noted that a growing body of literature suggests that use of the SGB for PTSD can be effective “because PTSD has a neurobiological basis and is essentially caused by an actual injury to the brain.”
A Natural Response, Not a Disorder
Dr. Lipov’s clinical work treating PTSD as a brain injury led him to connect with Frank Ochberg, MD, a founding board member of the International Society for Traumatic Stress Studies, former associate director of the National Institute of Mental Health, and former director of the Michigan Department of Mental Health.
In 2012, Dr. Ochberg teamed up with retired Army General Peter Chiarelli and Jonathan Shay, MD, PhD, author of Achilles in Vietnam: Combat Trauma and the Undoing of Character, to petition the DSM-5 Steering Committee to change the name of PTSD to PTSI in the upcoming DSM-5.
Dr. Ochberg explained that Gen. Chiarelli believed the term “disorder” suggests a preexisting issue prior to enlistment, potentially making an individual appear “weak.” He noted that this stigma is particularly troubling for military personnel, who often avoid seeking so they are not perceived as vulnerable, which can lead to potentially dire consequences, including suicide.
“We received endorsements from many quarters, not only advocates for service members or veterans,” Dr. Ochberg said.
This included feminists like Gloria Steinem, who championed the rights of women who had survived rape, incest, and domestic violence. As one advocate put it: “The natural human reaction to a life-threatening event should not be labeled a disorder.”
The DSM-5 Steering Committee declined to change the name. “Their feeling was that if we change the word ‘disorder’ to something else, we’d have to change every condition in the DSM that’s called a ‘disorder’. And they felt there really was nothing wrong with the word,” said Dr. Ochberg.
However, Dr. Lipov noted that other diagnoses have undergone name changes in the DSM for the sake of accuracy or stigma reduction. For example, the term mental retardation (DSM-IV) was changed to intellectual disability in DSM-5, and gender identity disorder was changed to gender dysphoria.
A decade later, Dr. Lipov decided to try again. To bolster his contention, he conducted a telephone survey of 1025 individuals. Of these, about 50% had a PTSD diagnosis.
Approximately two thirds of respondents agreed that a name change to PTSI would reduce the stigma associated with the term “PTSD.” Over half said it would increase the likelihood they would seek medical help. Those diagnosed with PTSD were most likely to endorse the name change.
Dr. Lipov conducts an ongoing survey of psychiatrists to ascertain their views on the potential name change and hopes to include findings in future research and communication with the DSM-5 Steering Committee. In addition, he has developed a new survey that expands upon his original survey, which specifically looked at individuals with PTSD.
“The new survey includes a wide range of people, many of whom have never been diagnosed. One of the questions we ask is whether they’ve ever heard of PTSD, and then we ask them about their reaction to the term,” he said.
A Barrier to Care
Psychiatrist Marcel Green, MD, director of Hudson Mind in New York City, refers to himself as an “interventional psychiatrist,” as he employs a comprehensive approach that includes not only medication and psychotherapy but also specialized techniques like SBG for severe anxiety-related physical symptoms and certain pain conditions.
Dr. Green, who is not involved in the name change initiative, agrees that the term “disorder” carries more stigma than “injury” for many groups, including those who have experienced childhood trauma, those struggling with substance abuse, or who are from backgrounds or peer groups where seeking mental health care is stigmatized.
Patients like these “are looking to me to give them a language to frame what they’re going through, and I tell them their symptoms are consistent with PTSD,” he said. “But they tell me don’t see themselves as having a disorder, which hinders their pursuit of care.”
Framing the condition as an “injury” also aligns with the approach of using biologic interventions to address the injury. Dr. Green has found SGB helpful in treating substance abuse disorder too, “which is a form of escape from the hyperactivation that accompanies PTSD.” And after the procedure, “they’re more receptive to therapy.”
Unfortunately, said Dr. Lipov, the DSM Steering Committee rejected his proposed name change, stating that the “concept of disorder as a dividing line from, eg, normal reactions to stress, is a core concept in the DSM, and the term has only rarely been removed.”
Moreover, the committee “did not see sufficient evidence ... that the name PTSD is stigmatizing and actually deters people with the disorder from seeking treatment who would not be deterred from doing so by PTSI.”
‘An Avenue for Dignity’
Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness (NAMI), noted that the organization does not have an official position on this issue. However, he shared his own personal perspective.
There may be merit in the proposed name change, said Dr. Duckworth, but more evidence is needed. “If it’s clear, after rigorous studies have been performed and there’s compelling data, that calling it a ‘disorder’ rather than an ‘injury’ is actually preventing people from getting the care they need, then it merits serious attention.”
If so, Dr. Duckworth would be “interested in having a conversation with the policy team at NAMI to start to see if we could activate the DSM Committee.”
Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto in Ontario, Canada, and head of the Mood Disorders Psychopharmacology Unit, said the name change initiative is a “really interesting proposal.”
Dr. McIntyre, chairman and executive director of the Brain and Cognition Discovery Foundation, also in Toronto, who is not involved in the initiative, has also heard “many people say that the term ‘disorder’ is stigmatizing and might even come across as pejorative in some ways.”
By contrast, “the word ‘injury’ parallels physical injury, and what we currently call ‘PTSD’ is a psychological or emotional injury no less devastating than torn tissue or broken bones,” added Dr. McIntyre, who is also the chairman of the board of the Depression and Bipolar Support Alliance.
Dr. Ochberg agreed. “In the military, ‘injury’ opens up an avenue for dignity, for a medal. Being injured and learning how to deal with an injury is part of having yet another honorable task that comes from being an honorable person who did an honorable thing.”
While disappointed, Dr. Lipov does not plan to give up on his vision. “I will continue to amass evidence that the word ‘PTSD’ is stigmatizing and indeed does prevent people from seeking care and will resubmit the proposal to the DSM Steering Committee when I have gathered a larger body of compelling evidence.”
Currently, Dr. Lipov is in active discussions with the special operations force of the US Army to obtain more evidence. “This will be the follow-up to bolster the opinion of Peter Chiarelli,” he said. “It is known that suicide and PTSD are highly related. This is especially urgent and relevant because recent data suggest suicide rate of military personnel in the VA may be as high as 44 per day,” Dr. Lipov said.
Dr. Lipov is the chief medical officer and an investor in the Stella Center. Dr. Green performs SGBs as part of his psychiatric practice. Drs. Ochberg, McIntyre, and Duckworth reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
In a bid to reduce stigma and improve treatment rates, for inclusion in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR). The APA’s policy is that a rolling name change is available if the current term is determined to be harmful.
Currently led by anesthesiologist Eugene Lipov, MD, clinical assistant professor, University of Illinois Chicago, and chief medical officer of Stella Center, also in Chicago, the formal request for the proposed name change to the APA’s DSM-5-TR Steering Committee in August 2023.
The APA Steering Committee rejected the proposed name change in November 2023, citing a “lack of convincing evidence.” However, Dr. Lipov and colleagues remain undeterred and continue to advocate for the change.
“The word ‘disorder’ is both imprecise and stigmatizing,” Dr. Lipov said. “Because of stigma, many people with PTSD — especially those in the military — don’t get help, which my research has demonstrated.”
Patients are more likely to seek help if their symptoms are framed as manifestations of an injury that is diagnosable and treatable, like a broken leg, Dr. Lipov said. “Stigma can kill in very real ways, since delayed care or lack of care can directly lead to suicides, thus satisfying the reduce harm requirement for the name change.”
Neurobiology of Trauma
Dr. Lipov grew up with a veteran father affected by PTSD and a mother with debilitating depression who eventually took her life. “I understand the impact of trauma very well,” he said.
Although not a psychiatrist, Dr. Lipov pioneered a highly successful treatment for PTSD by adapting an anesthetic technique — the stellate ganglion block (SGB) — to reverse many trauma symptoms through the process of “rebooting.”
This involves reversing the activity of the sympathetic nervous system — the fight-or-flight response — to the pretrauma state by anesthetizing the sympathetic ganglion in the neck. Investigating how SGB can help ameliorate the symptoms of PTSD led him to investigate and describe the neurobiology of PTSD and the mechanism of action of SGB.
The impact of SGD on PTSD was supported by a small neuroimaging study demonstrating that the right amygdala — the area of the brain associated with the fear response — was overactivated in patients with PTSD but that this region was deactivated after the administration of SGB, Dr. Lipov said.
“I believe that psychiatric conditions are actually physiologic brain changes that can be measured by advanced neuroimaging technologies and then physiologically treated,” he stated.
He noted that a growing body of literature suggests that use of the SGB for PTSD can be effective “because PTSD has a neurobiological basis and is essentially caused by an actual injury to the brain.”
A Natural Response, Not a Disorder
Dr. Lipov’s clinical work treating PTSD as a brain injury led him to connect with Frank Ochberg, MD, a founding board member of the International Society for Traumatic Stress Studies, former associate director of the National Institute of Mental Health, and former director of the Michigan Department of Mental Health.
In 2012, Dr. Ochberg teamed up with retired Army General Peter Chiarelli and Jonathan Shay, MD, PhD, author of Achilles in Vietnam: Combat Trauma and the Undoing of Character, to petition the DSM-5 Steering Committee to change the name of PTSD to PTSI in the upcoming DSM-5.
Dr. Ochberg explained that Gen. Chiarelli believed the term “disorder” suggests a preexisting issue prior to enlistment, potentially making an individual appear “weak.” He noted that this stigma is particularly troubling for military personnel, who often avoid seeking so they are not perceived as vulnerable, which can lead to potentially dire consequences, including suicide.
“We received endorsements from many quarters, not only advocates for service members or veterans,” Dr. Ochberg said.
This included feminists like Gloria Steinem, who championed the rights of women who had survived rape, incest, and domestic violence. As one advocate put it: “The natural human reaction to a life-threatening event should not be labeled a disorder.”
The DSM-5 Steering Committee declined to change the name. “Their feeling was that if we change the word ‘disorder’ to something else, we’d have to change every condition in the DSM that’s called a ‘disorder’. And they felt there really was nothing wrong with the word,” said Dr. Ochberg.
However, Dr. Lipov noted that other diagnoses have undergone name changes in the DSM for the sake of accuracy or stigma reduction. For example, the term mental retardation (DSM-IV) was changed to intellectual disability in DSM-5, and gender identity disorder was changed to gender dysphoria.
A decade later, Dr. Lipov decided to try again. To bolster his contention, he conducted a telephone survey of 1025 individuals. Of these, about 50% had a PTSD diagnosis.
Approximately two thirds of respondents agreed that a name change to PTSI would reduce the stigma associated with the term “PTSD.” Over half said it would increase the likelihood they would seek medical help. Those diagnosed with PTSD were most likely to endorse the name change.
Dr. Lipov conducts an ongoing survey of psychiatrists to ascertain their views on the potential name change and hopes to include findings in future research and communication with the DSM-5 Steering Committee. In addition, he has developed a new survey that expands upon his original survey, which specifically looked at individuals with PTSD.
“The new survey includes a wide range of people, many of whom have never been diagnosed. One of the questions we ask is whether they’ve ever heard of PTSD, and then we ask them about their reaction to the term,” he said.
A Barrier to Care
Psychiatrist Marcel Green, MD, director of Hudson Mind in New York City, refers to himself as an “interventional psychiatrist,” as he employs a comprehensive approach that includes not only medication and psychotherapy but also specialized techniques like SBG for severe anxiety-related physical symptoms and certain pain conditions.
Dr. Green, who is not involved in the name change initiative, agrees that the term “disorder” carries more stigma than “injury” for many groups, including those who have experienced childhood trauma, those struggling with substance abuse, or who are from backgrounds or peer groups where seeking mental health care is stigmatized.
Patients like these “are looking to me to give them a language to frame what they’re going through, and I tell them their symptoms are consistent with PTSD,” he said. “But they tell me don’t see themselves as having a disorder, which hinders their pursuit of care.”
Framing the condition as an “injury” also aligns with the approach of using biologic interventions to address the injury. Dr. Green has found SGB helpful in treating substance abuse disorder too, “which is a form of escape from the hyperactivation that accompanies PTSD.” And after the procedure, “they’re more receptive to therapy.”
Unfortunately, said Dr. Lipov, the DSM Steering Committee rejected his proposed name change, stating that the “concept of disorder as a dividing line from, eg, normal reactions to stress, is a core concept in the DSM, and the term has only rarely been removed.”
Moreover, the committee “did not see sufficient evidence ... that the name PTSD is stigmatizing and actually deters people with the disorder from seeking treatment who would not be deterred from doing so by PTSI.”
‘An Avenue for Dignity’
Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness (NAMI), noted that the organization does not have an official position on this issue. However, he shared his own personal perspective.
There may be merit in the proposed name change, said Dr. Duckworth, but more evidence is needed. “If it’s clear, after rigorous studies have been performed and there’s compelling data, that calling it a ‘disorder’ rather than an ‘injury’ is actually preventing people from getting the care they need, then it merits serious attention.”
If so, Dr. Duckworth would be “interested in having a conversation with the policy team at NAMI to start to see if we could activate the DSM Committee.”
Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto in Ontario, Canada, and head of the Mood Disorders Psychopharmacology Unit, said the name change initiative is a “really interesting proposal.”
Dr. McIntyre, chairman and executive director of the Brain and Cognition Discovery Foundation, also in Toronto, who is not involved in the initiative, has also heard “many people say that the term ‘disorder’ is stigmatizing and might even come across as pejorative in some ways.”
By contrast, “the word ‘injury’ parallels physical injury, and what we currently call ‘PTSD’ is a psychological or emotional injury no less devastating than torn tissue or broken bones,” added Dr. McIntyre, who is also the chairman of the board of the Depression and Bipolar Support Alliance.
Dr. Ochberg agreed. “In the military, ‘injury’ opens up an avenue for dignity, for a medal. Being injured and learning how to deal with an injury is part of having yet another honorable task that comes from being an honorable person who did an honorable thing.”
While disappointed, Dr. Lipov does not plan to give up on his vision. “I will continue to amass evidence that the word ‘PTSD’ is stigmatizing and indeed does prevent people from seeking care and will resubmit the proposal to the DSM Steering Committee when I have gathered a larger body of compelling evidence.”
Currently, Dr. Lipov is in active discussions with the special operations force of the US Army to obtain more evidence. “This will be the follow-up to bolster the opinion of Peter Chiarelli,” he said. “It is known that suicide and PTSD are highly related. This is especially urgent and relevant because recent data suggest suicide rate of military personnel in the VA may be as high as 44 per day,” Dr. Lipov said.
Dr. Lipov is the chief medical officer and an investor in the Stella Center. Dr. Green performs SGBs as part of his psychiatric practice. Drs. Ochberg, McIntyre, and Duckworth reported no relevant financial relationships.
A version of this article appeared on Medscape.com.