User login
AHA scientific statement on rapid evaluation for suspected TIA
TIAs are “warning shots” of a future stroke and require emergency evaluation, Hardik Amin, MD, chair of the writing committee and medical stroke director, Yale New Haven (Conn.) Hospital, said in an AHA podcast.
A key aim of the scientific statement is to help clinicians properly risk-stratify patients with suspected TIA and determine which patients need to be admitted to the hospital and which patients might be safely discharged as long as proper and prompt follow-up has been arranged, Dr. Amin explained.
The statement, published online in the journal Stroke, addresses “how we can identify and be confident in diagnosing a TIA patient and what might suggest an alternative diagnosis,” he added.
Diagnostic challenge
It’s estimated that nearly one in five people who suffer a TIA will have a full-blown stroke within 3 months; close to half of these strokes will happen within 2 days.
The challenge with TIAs is that they can be tough to diagnose because many patients no longer have symptoms when they arrive at the emergency department. There is also no confirmatory test. Limited resources and access to stroke specialists in rural centers may exacerbate these challenges, the authors noted.
The statement pointed out that the F.A.S.T. acronym for stroke symptoms (Face drooping, Arm weakness, Speech difficulty, Time to call 911) can also be used to identify a TIA – even if the symptoms resolve.
The statement also provided guidance on how to tell the difference between a TIA and a TIA mimic.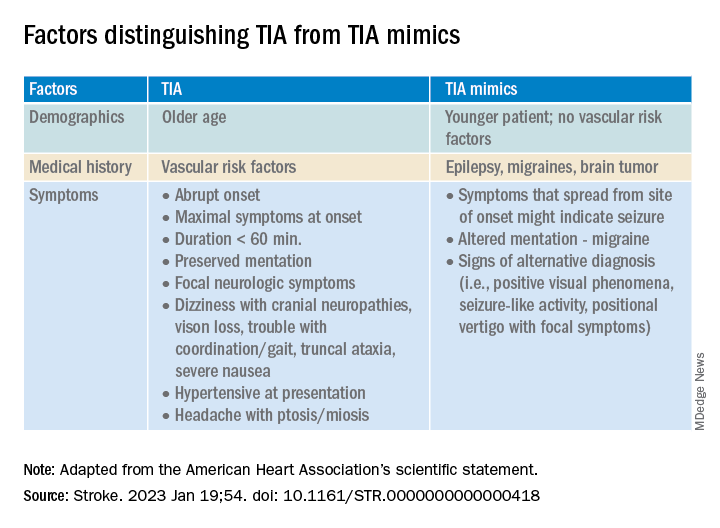
If available, a noncontrast head CT (NCCT) scan should be done initially in the emergency department to evaluate for subacute ischemia, hemorrhage, or mass lesion. Although the sensitivity of NCCT to detect an acute infarct is low, NCCT is useful for ruling out TIA mimics, the writing group said.
Multimodal brain MRI is the “preferred” method to evaluate for acute ischemic infarct and ideally should be obtained within 24 hours of symptom onset, and in most centers will follow an NCCT.
“When MRI cannot be obtained acutely to definitively distinguish TIA from stroke, it remains reasonable to make a clinical diagnosis of TIA in the ED on the basis of a negative NCCT and symptom resolution within 24 hours,” the authors said.
“A potential next step would be hospital admission for MRI, comprehensive workup, and neurology consultation. Other options might include transferring patients to a facility with advanced imaging and vascular neurology expertise or arranging a timely (ideally < 24 hours) outpatient MRI,” they advised.
The statement also provides guidance on the advantages, limitations, and considerations of Doppler ultrasonography, CT angiography, and magnetic resonance angiography for TIA assessment.
Once TIA is diagnosed, a cardiac work-up is advised because of the potential for heart-related factors to cause a TIA.
An individual’s risk of future stroke after TIA can be rapidly assessed using the ABCD2 score, which stratifies patients into low, medium, and high risk based on age, blood pressure, clinical features, duration of symptoms, and diabetes.
“It is up to each center to use the resources available and create a pathway to ensure successful management and disposition of patients with TIA, with the ultimate goal of reducing the risk of future stroke,” the authors concluded.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Emergency Neurovascular Care Committee of the Stroke Council and the Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists, and it is endorsed by the American Association of Neurological Surgeons/Congress of Neurological Surgeons.
A version of this article first appeared on Medscape.com.
TIAs are “warning shots” of a future stroke and require emergency evaluation, Hardik Amin, MD, chair of the writing committee and medical stroke director, Yale New Haven (Conn.) Hospital, said in an AHA podcast.
A key aim of the scientific statement is to help clinicians properly risk-stratify patients with suspected TIA and determine which patients need to be admitted to the hospital and which patients might be safely discharged as long as proper and prompt follow-up has been arranged, Dr. Amin explained.
The statement, published online in the journal Stroke, addresses “how we can identify and be confident in diagnosing a TIA patient and what might suggest an alternative diagnosis,” he added.
Diagnostic challenge
It’s estimated that nearly one in five people who suffer a TIA will have a full-blown stroke within 3 months; close to half of these strokes will happen within 2 days.
The challenge with TIAs is that they can be tough to diagnose because many patients no longer have symptoms when they arrive at the emergency department. There is also no confirmatory test. Limited resources and access to stroke specialists in rural centers may exacerbate these challenges, the authors noted.
The statement pointed out that the F.A.S.T. acronym for stroke symptoms (Face drooping, Arm weakness, Speech difficulty, Time to call 911) can also be used to identify a TIA – even if the symptoms resolve.
The statement also provided guidance on how to tell the difference between a TIA and a TIA mimic.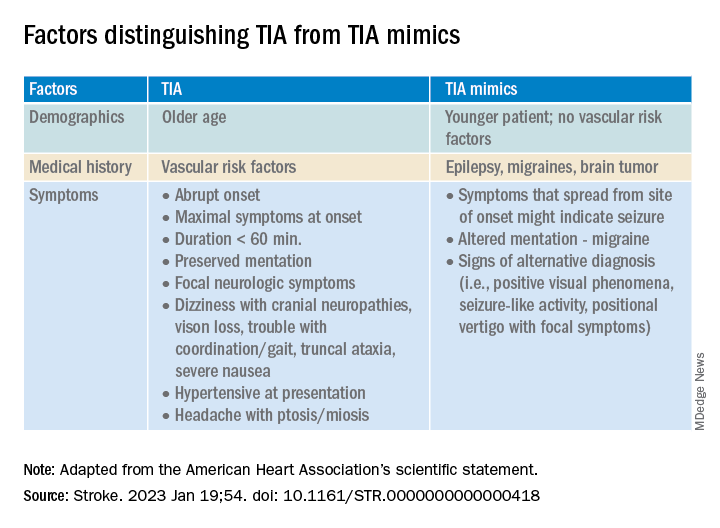
If available, a noncontrast head CT (NCCT) scan should be done initially in the emergency department to evaluate for subacute ischemia, hemorrhage, or mass lesion. Although the sensitivity of NCCT to detect an acute infarct is low, NCCT is useful for ruling out TIA mimics, the writing group said.
Multimodal brain MRI is the “preferred” method to evaluate for acute ischemic infarct and ideally should be obtained within 24 hours of symptom onset, and in most centers will follow an NCCT.
“When MRI cannot be obtained acutely to definitively distinguish TIA from stroke, it remains reasonable to make a clinical diagnosis of TIA in the ED on the basis of a negative NCCT and symptom resolution within 24 hours,” the authors said.
“A potential next step would be hospital admission for MRI, comprehensive workup, and neurology consultation. Other options might include transferring patients to a facility with advanced imaging and vascular neurology expertise or arranging a timely (ideally < 24 hours) outpatient MRI,” they advised.
The statement also provides guidance on the advantages, limitations, and considerations of Doppler ultrasonography, CT angiography, and magnetic resonance angiography for TIA assessment.
Once TIA is diagnosed, a cardiac work-up is advised because of the potential for heart-related factors to cause a TIA.
An individual’s risk of future stroke after TIA can be rapidly assessed using the ABCD2 score, which stratifies patients into low, medium, and high risk based on age, blood pressure, clinical features, duration of symptoms, and diabetes.
“It is up to each center to use the resources available and create a pathway to ensure successful management and disposition of patients with TIA, with the ultimate goal of reducing the risk of future stroke,” the authors concluded.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Emergency Neurovascular Care Committee of the Stroke Council and the Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists, and it is endorsed by the American Association of Neurological Surgeons/Congress of Neurological Surgeons.
A version of this article first appeared on Medscape.com.
TIAs are “warning shots” of a future stroke and require emergency evaluation, Hardik Amin, MD, chair of the writing committee and medical stroke director, Yale New Haven (Conn.) Hospital, said in an AHA podcast.
A key aim of the scientific statement is to help clinicians properly risk-stratify patients with suspected TIA and determine which patients need to be admitted to the hospital and which patients might be safely discharged as long as proper and prompt follow-up has been arranged, Dr. Amin explained.
The statement, published online in the journal Stroke, addresses “how we can identify and be confident in diagnosing a TIA patient and what might suggest an alternative diagnosis,” he added.
Diagnostic challenge
It’s estimated that nearly one in five people who suffer a TIA will have a full-blown stroke within 3 months; close to half of these strokes will happen within 2 days.
The challenge with TIAs is that they can be tough to diagnose because many patients no longer have symptoms when they arrive at the emergency department. There is also no confirmatory test. Limited resources and access to stroke specialists in rural centers may exacerbate these challenges, the authors noted.
The statement pointed out that the F.A.S.T. acronym for stroke symptoms (Face drooping, Arm weakness, Speech difficulty, Time to call 911) can also be used to identify a TIA – even if the symptoms resolve.
The statement also provided guidance on how to tell the difference between a TIA and a TIA mimic.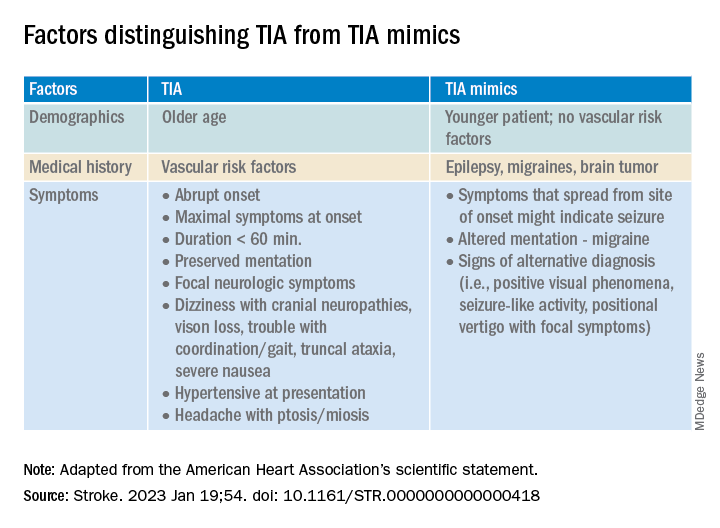
If available, a noncontrast head CT (NCCT) scan should be done initially in the emergency department to evaluate for subacute ischemia, hemorrhage, or mass lesion. Although the sensitivity of NCCT to detect an acute infarct is low, NCCT is useful for ruling out TIA mimics, the writing group said.
Multimodal brain MRI is the “preferred” method to evaluate for acute ischemic infarct and ideally should be obtained within 24 hours of symptom onset, and in most centers will follow an NCCT.
“When MRI cannot be obtained acutely to definitively distinguish TIA from stroke, it remains reasonable to make a clinical diagnosis of TIA in the ED on the basis of a negative NCCT and symptom resolution within 24 hours,” the authors said.
“A potential next step would be hospital admission for MRI, comprehensive workup, and neurology consultation. Other options might include transferring patients to a facility with advanced imaging and vascular neurology expertise or arranging a timely (ideally < 24 hours) outpatient MRI,” they advised.
The statement also provides guidance on the advantages, limitations, and considerations of Doppler ultrasonography, CT angiography, and magnetic resonance angiography for TIA assessment.
Once TIA is diagnosed, a cardiac work-up is advised because of the potential for heart-related factors to cause a TIA.
An individual’s risk of future stroke after TIA can be rapidly assessed using the ABCD2 score, which stratifies patients into low, medium, and high risk based on age, blood pressure, clinical features, duration of symptoms, and diabetes.
“It is up to each center to use the resources available and create a pathway to ensure successful management and disposition of patients with TIA, with the ultimate goal of reducing the risk of future stroke,” the authors concluded.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Emergency Neurovascular Care Committee of the Stroke Council and the Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists, and it is endorsed by the American Association of Neurological Surgeons/Congress of Neurological Surgeons.
A version of this article first appeared on Medscape.com.
FROM STROKE
Do biologics protect against cancer progression in IBD?
in an observational study conducted in Japan.
IBD-associated intestinal cancer is thought to be caused by chronic inflammation of the intestinal mucosa, and controlling inflammation is thought to be effective in reducing cancer risk.
It’s generally considered that biologics do not change the risk of cancer, and whether they lower the risk remains unclear, write Ryo Seishima, MD, PhD, with Keio University in Tokyo, and colleagues. However, few studies have focused on cancer progression, namely, the risk of advanced-stage cancer.
To investigate, researchers reviewed the medical records of 828 patients with UC and 214 with CD who were diagnosed with IBD-associated intestinal neoplasia (dysplasia or cancer) from 1983 to 2020.
Therapeutic agents taken within 1 year before neoplasia diagnosis were classified into three types: biologics (infliximab, vedolizumab, golimumab, and adalimumab), 5-aminosalicylic acid (5-ASA), and immunomodulators.
The primary endpoint was the pathologic cancer stage at the time of diagnosis. Early-stage cancer was defined as either dysplasia or pathologic stage 0/I cancer, and advanced-stage cancer was defined as pathologic stage II/III/IV cancer.
Advanced-stage cancer was found in 297 patients (35.9%) with UC and 159 patients (74.3%) with CD.
The researchers say the higher percentage of advanced cancer in patients with CD rather than in patients with UC may suggest that regular surveillance was not effective for patients with CD or that physicians were less adherent to surveillance intervals. This question merits further study, they suggest.
None of the drug types were significantly associated with cancer stage in the CD cohort, they report.
Benefits seen in UC
In the UC cohort, advanced-stage cancer (vs. early-stage) was significantly associated with less use of biologics (2% vs. 7.7%; P < .001), 5-ASA (75.4% vs. 87.6%; P < .001), and immunomodulators (11.8% vs. 22.4%; P < .001). Steroid use was also significantly lower in the advanced-stage cancer group (26.3% vs. 33.3%; P = .035).
In multivariate analysis that was adjusted for age, diagnosis year, regular surveillance, and histologic type in UC, biologics (odds ratio, 0.11; P < .001) and 5-ASA (OR, 0.63; P = .041) were significantly associated with a lower risk of advanced-stage cancer.
The study was published online in The American Journal of Gastroenterology.
“These results indicate that biologics and 5-ASA are drugs that are potentially associated with a lower risk of advanced cancer in patients with UC but not with CD,” Dr. Seishima and colleagues say.
They also suggest that the mechanism of cancer progression in UC and CD may differ and needs to be investigated further.
Reassuring data with caveats
The study is “interesting and reassuring, but there are a lot of limitations with the study design,” said Ashwin Ananthakrishnan, MD, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who was not involved in the research.
“By focusing only on those who have been diagnosed with cancer, one cannot actually conclude what the risk of cancer is and if these medications reduce the risk of colon cancer, which is a far more important and interesting question,” he said.
Patients undergoing treatment with biologics likely receive closer follow-up, so in these patients, cancers are less likely to be diagnosed at an advanced stage, said Dr. Ananthakrishnan. For that reason, the study can’t clearly establish the degree to which the effect was from medication or surveillance, he added.
As for whether biologics affect the overall risk of cancer development, the study doesn’t change “current thinking that biologics are safe in this setting,” he added.
Erin Forster, MD, MPH, with the Medical University of South Carolina, Charleston, also weighed in on medication safety.
“Prior research has shown that the risk of uncontrolled inflammation outweighs the risk of our current medications,” Dr. Forster, who was not involved in the research, said in an interview.
The study had no specific funding. Dr. Seishima, Dr. Ananthakrishnan, and Dr. Forster have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in an observational study conducted in Japan.
IBD-associated intestinal cancer is thought to be caused by chronic inflammation of the intestinal mucosa, and controlling inflammation is thought to be effective in reducing cancer risk.
It’s generally considered that biologics do not change the risk of cancer, and whether they lower the risk remains unclear, write Ryo Seishima, MD, PhD, with Keio University in Tokyo, and colleagues. However, few studies have focused on cancer progression, namely, the risk of advanced-stage cancer.
To investigate, researchers reviewed the medical records of 828 patients with UC and 214 with CD who were diagnosed with IBD-associated intestinal neoplasia (dysplasia or cancer) from 1983 to 2020.
Therapeutic agents taken within 1 year before neoplasia diagnosis were classified into three types: biologics (infliximab, vedolizumab, golimumab, and adalimumab), 5-aminosalicylic acid (5-ASA), and immunomodulators.
The primary endpoint was the pathologic cancer stage at the time of diagnosis. Early-stage cancer was defined as either dysplasia or pathologic stage 0/I cancer, and advanced-stage cancer was defined as pathologic stage II/III/IV cancer.
Advanced-stage cancer was found in 297 patients (35.9%) with UC and 159 patients (74.3%) with CD.
The researchers say the higher percentage of advanced cancer in patients with CD rather than in patients with UC may suggest that regular surveillance was not effective for patients with CD or that physicians were less adherent to surveillance intervals. This question merits further study, they suggest.
None of the drug types were significantly associated with cancer stage in the CD cohort, they report.
Benefits seen in UC
In the UC cohort, advanced-stage cancer (vs. early-stage) was significantly associated with less use of biologics (2% vs. 7.7%; P < .001), 5-ASA (75.4% vs. 87.6%; P < .001), and immunomodulators (11.8% vs. 22.4%; P < .001). Steroid use was also significantly lower in the advanced-stage cancer group (26.3% vs. 33.3%; P = .035).
In multivariate analysis that was adjusted for age, diagnosis year, regular surveillance, and histologic type in UC, biologics (odds ratio, 0.11; P < .001) and 5-ASA (OR, 0.63; P = .041) were significantly associated with a lower risk of advanced-stage cancer.
The study was published online in The American Journal of Gastroenterology.
“These results indicate that biologics and 5-ASA are drugs that are potentially associated with a lower risk of advanced cancer in patients with UC but not with CD,” Dr. Seishima and colleagues say.
They also suggest that the mechanism of cancer progression in UC and CD may differ and needs to be investigated further.
Reassuring data with caveats
The study is “interesting and reassuring, but there are a lot of limitations with the study design,” said Ashwin Ananthakrishnan, MD, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who was not involved in the research.
“By focusing only on those who have been diagnosed with cancer, one cannot actually conclude what the risk of cancer is and if these medications reduce the risk of colon cancer, which is a far more important and interesting question,” he said.
Patients undergoing treatment with biologics likely receive closer follow-up, so in these patients, cancers are less likely to be diagnosed at an advanced stage, said Dr. Ananthakrishnan. For that reason, the study can’t clearly establish the degree to which the effect was from medication or surveillance, he added.
As for whether biologics affect the overall risk of cancer development, the study doesn’t change “current thinking that biologics are safe in this setting,” he added.
Erin Forster, MD, MPH, with the Medical University of South Carolina, Charleston, also weighed in on medication safety.
“Prior research has shown that the risk of uncontrolled inflammation outweighs the risk of our current medications,” Dr. Forster, who was not involved in the research, said in an interview.
The study had no specific funding. Dr. Seishima, Dr. Ananthakrishnan, and Dr. Forster have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in an observational study conducted in Japan.
IBD-associated intestinal cancer is thought to be caused by chronic inflammation of the intestinal mucosa, and controlling inflammation is thought to be effective in reducing cancer risk.
It’s generally considered that biologics do not change the risk of cancer, and whether they lower the risk remains unclear, write Ryo Seishima, MD, PhD, with Keio University in Tokyo, and colleagues. However, few studies have focused on cancer progression, namely, the risk of advanced-stage cancer.
To investigate, researchers reviewed the medical records of 828 patients with UC and 214 with CD who were diagnosed with IBD-associated intestinal neoplasia (dysplasia or cancer) from 1983 to 2020.
Therapeutic agents taken within 1 year before neoplasia diagnosis were classified into three types: biologics (infliximab, vedolizumab, golimumab, and adalimumab), 5-aminosalicylic acid (5-ASA), and immunomodulators.
The primary endpoint was the pathologic cancer stage at the time of diagnosis. Early-stage cancer was defined as either dysplasia or pathologic stage 0/I cancer, and advanced-stage cancer was defined as pathologic stage II/III/IV cancer.
Advanced-stage cancer was found in 297 patients (35.9%) with UC and 159 patients (74.3%) with CD.
The researchers say the higher percentage of advanced cancer in patients with CD rather than in patients with UC may suggest that regular surveillance was not effective for patients with CD or that physicians were less adherent to surveillance intervals. This question merits further study, they suggest.
None of the drug types were significantly associated with cancer stage in the CD cohort, they report.
Benefits seen in UC
In the UC cohort, advanced-stage cancer (vs. early-stage) was significantly associated with less use of biologics (2% vs. 7.7%; P < .001), 5-ASA (75.4% vs. 87.6%; P < .001), and immunomodulators (11.8% vs. 22.4%; P < .001). Steroid use was also significantly lower in the advanced-stage cancer group (26.3% vs. 33.3%; P = .035).
In multivariate analysis that was adjusted for age, diagnosis year, regular surveillance, and histologic type in UC, biologics (odds ratio, 0.11; P < .001) and 5-ASA (OR, 0.63; P = .041) were significantly associated with a lower risk of advanced-stage cancer.
The study was published online in The American Journal of Gastroenterology.
“These results indicate that biologics and 5-ASA are drugs that are potentially associated with a lower risk of advanced cancer in patients with UC but not with CD,” Dr. Seishima and colleagues say.
They also suggest that the mechanism of cancer progression in UC and CD may differ and needs to be investigated further.
Reassuring data with caveats
The study is “interesting and reassuring, but there are a lot of limitations with the study design,” said Ashwin Ananthakrishnan, MD, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who was not involved in the research.
“By focusing only on those who have been diagnosed with cancer, one cannot actually conclude what the risk of cancer is and if these medications reduce the risk of colon cancer, which is a far more important and interesting question,” he said.
Patients undergoing treatment with biologics likely receive closer follow-up, so in these patients, cancers are less likely to be diagnosed at an advanced stage, said Dr. Ananthakrishnan. For that reason, the study can’t clearly establish the degree to which the effect was from medication or surveillance, he added.
As for whether biologics affect the overall risk of cancer development, the study doesn’t change “current thinking that biologics are safe in this setting,” he added.
Erin Forster, MD, MPH, with the Medical University of South Carolina, Charleston, also weighed in on medication safety.
“Prior research has shown that the risk of uncontrolled inflammation outweighs the risk of our current medications,” Dr. Forster, who was not involved in the research, said in an interview.
The study had no specific funding. Dr. Seishima, Dr. Ananthakrishnan, and Dr. Forster have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
‘Concerning’ uptick in pediatric antipsychotic prescribing
“This study demonstrates a concerning trend in antipsychotic prescribing in children and adolescents,” study investigator Matthias Pierce, PhD, senior research fellow at the University of Manchester (England) Center for Women’s Mental Health, who jointly led the study, said in a news release.
“We do not think the changes in prescribing necessarily relate to changes in clinical need; rather, it may be more likely to reflect changes in prescribing practice by clinicians,” Dr. Pierce said.
The study was published online in The Lancet Psychiatry.
Increase in long-term use
Between 2000 and 2019, prescriptions for antipsychotics nearly doubled from 0.06% to 0.11%.
The investigators note that the U.K.’s National Institute for Health and Care Excellence has approved the use of some antipsychotics in patients younger than age 18 with schizophrenia, bipolar disorder, and severely aggressive behavior attributable to conduct disorder.
However, these data suggest antipsychotics are being prescribed for an increasingly broad range of conditions, most commonly autism, but also for attention-deficit/ hyperactivity disorder, tic disorders like Tourrette syndrome, and learning difficulties.
“Broadening use of antipsychotics in developing young people begs questions about their safety over time and demands more research on this topic,” senior author Kathryn Abel, MBBS, PhD, from the University of Manchester said in the news release.
During the study period, antipsychotic prescribing in primary care increased by an average of 3.3% per year and the rate of first prescriptions increased by 2.2% per year.
The data also suggest that more children and adolescents are taking these powerful drugs for longer periods of time. The proportion receiving antipsychotics for at least 6 months after an initial prescription rose from 41.9% in 2000 to 62.8% in 2018.
Prescribing inequities
From 2009 onwards, more than 90% of prescriptions were for atypical antipsychotics.
Over time, risperidone dominated, with more than 60% of all prescriptions, followed by aripiprazole, quetiapine, olanzapine, and haloperidol as the most prescribed antipsychotics.
Boys and older children aged 15-18 years were most likely to receive an antipsychotic. However, the increasing trends were evident in all groups.
The data also point to inequities in prescribing as a result of deprivation levels, with typical antipsychotics prescribed more frequently in more deprived areas over time.
Dr. Pierce said he hopes this study will “help clinicians to evaluate the prescribing of antipsychotics to children more fully and will encourage them to consider better access to alternatives.”
Dr. Abel noted that antipsychotic medications “continue to have a valuable role in the treatment of serious mental illness. These findings represent a descriptive account of antipsychotic prescribing to children and adolescents in the U.K. today and provide a window onto current practice.”
Findings are no surprise
Emily Simonoff, MD, professor of child and adolescent psychiatry, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, offered perspective on the study in a statement from the U.K. nonprofit Science Media Centre.
“To clinicians, it will not be surprising that the authors demonstrate an increase in rates of prescriptions over that time period, as there has been a steadily emerging evidence base for the benefits of this group of medication for a range of different indications, which has been further supported by new licensing indications and recommendations from NICE,” Dr. Simonoff said.
For example, “there is good evidence for their benefits for other conditions such as irritability in autism spectrum disorder.
“However, it should also be noted that NICE recommendations for their use in many conditions is as part of a multimodal treatment plan, for example including psychological or behavioral interventions. It’s unclear from the study whether such recommendations were being followed or medication was being used on its own,” she added.
Dr. Simonoff also said it’s “reassuring” that prescribing rates remain very low in the youngest children and notes that the authors “rightly highlight the need for high-quality, longer-term studies on efficacy and, most importantly, adverse effects. This should be a research priority.”
The study had no funding. The authors report no relevant financial relationships. Dr. Simonoff is a member of the NICE guideline development group for the management of autism and has published on the efficacy of antipsychotic medication for irritability in autism.
A version of this article first appeared on Medscape.com.
“This study demonstrates a concerning trend in antipsychotic prescribing in children and adolescents,” study investigator Matthias Pierce, PhD, senior research fellow at the University of Manchester (England) Center for Women’s Mental Health, who jointly led the study, said in a news release.
“We do not think the changes in prescribing necessarily relate to changes in clinical need; rather, it may be more likely to reflect changes in prescribing practice by clinicians,” Dr. Pierce said.
The study was published online in The Lancet Psychiatry.
Increase in long-term use
Between 2000 and 2019, prescriptions for antipsychotics nearly doubled from 0.06% to 0.11%.
The investigators note that the U.K.’s National Institute for Health and Care Excellence has approved the use of some antipsychotics in patients younger than age 18 with schizophrenia, bipolar disorder, and severely aggressive behavior attributable to conduct disorder.
However, these data suggest antipsychotics are being prescribed for an increasingly broad range of conditions, most commonly autism, but also for attention-deficit/ hyperactivity disorder, tic disorders like Tourrette syndrome, and learning difficulties.
“Broadening use of antipsychotics in developing young people begs questions about their safety over time and demands more research on this topic,” senior author Kathryn Abel, MBBS, PhD, from the University of Manchester said in the news release.
During the study period, antipsychotic prescribing in primary care increased by an average of 3.3% per year and the rate of first prescriptions increased by 2.2% per year.
The data also suggest that more children and adolescents are taking these powerful drugs for longer periods of time. The proportion receiving antipsychotics for at least 6 months after an initial prescription rose from 41.9% in 2000 to 62.8% in 2018.
Prescribing inequities
From 2009 onwards, more than 90% of prescriptions were for atypical antipsychotics.
Over time, risperidone dominated, with more than 60% of all prescriptions, followed by aripiprazole, quetiapine, olanzapine, and haloperidol as the most prescribed antipsychotics.
Boys and older children aged 15-18 years were most likely to receive an antipsychotic. However, the increasing trends were evident in all groups.
The data also point to inequities in prescribing as a result of deprivation levels, with typical antipsychotics prescribed more frequently in more deprived areas over time.
Dr. Pierce said he hopes this study will “help clinicians to evaluate the prescribing of antipsychotics to children more fully and will encourage them to consider better access to alternatives.”
Dr. Abel noted that antipsychotic medications “continue to have a valuable role in the treatment of serious mental illness. These findings represent a descriptive account of antipsychotic prescribing to children and adolescents in the U.K. today and provide a window onto current practice.”
Findings are no surprise
Emily Simonoff, MD, professor of child and adolescent psychiatry, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, offered perspective on the study in a statement from the U.K. nonprofit Science Media Centre.
“To clinicians, it will not be surprising that the authors demonstrate an increase in rates of prescriptions over that time period, as there has been a steadily emerging evidence base for the benefits of this group of medication for a range of different indications, which has been further supported by new licensing indications and recommendations from NICE,” Dr. Simonoff said.
For example, “there is good evidence for their benefits for other conditions such as irritability in autism spectrum disorder.
“However, it should also be noted that NICE recommendations for their use in many conditions is as part of a multimodal treatment plan, for example including psychological or behavioral interventions. It’s unclear from the study whether such recommendations were being followed or medication was being used on its own,” she added.
Dr. Simonoff also said it’s “reassuring” that prescribing rates remain very low in the youngest children and notes that the authors “rightly highlight the need for high-quality, longer-term studies on efficacy and, most importantly, adverse effects. This should be a research priority.”
The study had no funding. The authors report no relevant financial relationships. Dr. Simonoff is a member of the NICE guideline development group for the management of autism and has published on the efficacy of antipsychotic medication for irritability in autism.
A version of this article first appeared on Medscape.com.
“This study demonstrates a concerning trend in antipsychotic prescribing in children and adolescents,” study investigator Matthias Pierce, PhD, senior research fellow at the University of Manchester (England) Center for Women’s Mental Health, who jointly led the study, said in a news release.
“We do not think the changes in prescribing necessarily relate to changes in clinical need; rather, it may be more likely to reflect changes in prescribing practice by clinicians,” Dr. Pierce said.
The study was published online in The Lancet Psychiatry.
Increase in long-term use
Between 2000 and 2019, prescriptions for antipsychotics nearly doubled from 0.06% to 0.11%.
The investigators note that the U.K.’s National Institute for Health and Care Excellence has approved the use of some antipsychotics in patients younger than age 18 with schizophrenia, bipolar disorder, and severely aggressive behavior attributable to conduct disorder.
However, these data suggest antipsychotics are being prescribed for an increasingly broad range of conditions, most commonly autism, but also for attention-deficit/ hyperactivity disorder, tic disorders like Tourrette syndrome, and learning difficulties.
“Broadening use of antipsychotics in developing young people begs questions about their safety over time and demands more research on this topic,” senior author Kathryn Abel, MBBS, PhD, from the University of Manchester said in the news release.
During the study period, antipsychotic prescribing in primary care increased by an average of 3.3% per year and the rate of first prescriptions increased by 2.2% per year.
The data also suggest that more children and adolescents are taking these powerful drugs for longer periods of time. The proportion receiving antipsychotics for at least 6 months after an initial prescription rose from 41.9% in 2000 to 62.8% in 2018.
Prescribing inequities
From 2009 onwards, more than 90% of prescriptions were for atypical antipsychotics.
Over time, risperidone dominated, with more than 60% of all prescriptions, followed by aripiprazole, quetiapine, olanzapine, and haloperidol as the most prescribed antipsychotics.
Boys and older children aged 15-18 years were most likely to receive an antipsychotic. However, the increasing trends were evident in all groups.
The data also point to inequities in prescribing as a result of deprivation levels, with typical antipsychotics prescribed more frequently in more deprived areas over time.
Dr. Pierce said he hopes this study will “help clinicians to evaluate the prescribing of antipsychotics to children more fully and will encourage them to consider better access to alternatives.”
Dr. Abel noted that antipsychotic medications “continue to have a valuable role in the treatment of serious mental illness. These findings represent a descriptive account of antipsychotic prescribing to children and adolescents in the U.K. today and provide a window onto current practice.”
Findings are no surprise
Emily Simonoff, MD, professor of child and adolescent psychiatry, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, offered perspective on the study in a statement from the U.K. nonprofit Science Media Centre.
“To clinicians, it will not be surprising that the authors demonstrate an increase in rates of prescriptions over that time period, as there has been a steadily emerging evidence base for the benefits of this group of medication for a range of different indications, which has been further supported by new licensing indications and recommendations from NICE,” Dr. Simonoff said.
For example, “there is good evidence for their benefits for other conditions such as irritability in autism spectrum disorder.
“However, it should also be noted that NICE recommendations for their use in many conditions is as part of a multimodal treatment plan, for example including psychological or behavioral interventions. It’s unclear from the study whether such recommendations were being followed or medication was being used on its own,” she added.
Dr. Simonoff also said it’s “reassuring” that prescribing rates remain very low in the youngest children and notes that the authors “rightly highlight the need for high-quality, longer-term studies on efficacy and, most importantly, adverse effects. This should be a research priority.”
The study had no funding. The authors report no relevant financial relationships. Dr. Simonoff is a member of the NICE guideline development group for the management of autism and has published on the efficacy of antipsychotic medication for irritability in autism.
A version of this article first appeared on Medscape.com.
FROM THE LANCET PSYCHIATRY
More support for MDMA-assisted psychotherapy for PTSD
The MAPP2 study is the second randomized, double-blind, placebo-controlled study to demonstrate the safety and efficacy of MDMA-assisted therapy for PTSD.
The investigators confirm results of the MAPP1 study, which were published in Nature Medicine. Patients who received MDMA-assisted psychotherapy in MAPP1 demonstrated greater improvement in PTSD symptoms, mood, and empathy, compared with participants who received psychotherapy with placebo.
The design of the MAPP2 study was similar to that of MAPP1, and its results were similar, the nonprofit Multidisciplinary Association for Psychedelic Studies (MAPS), which sponsored MAPP1 and MAPP2, said in a news release.
No specific results from MAPP2 were provided at this time. The full data from MAPP2 are expected to be published in a peer-reviewed journal later this year, and a new drug application to the U.S. Food and Drug Administration will follow.
The FDA granted breakthrough therapy designation to MDMA as an adjunct to psychotherapy for adults with PTSD in 2017.
MAPS was founded in 1986 to fund and facilitate research into the potential of psychedelic-assisted therapies; to educate the public about psychedelics for medical, social, and spiritual use; and to advocate for drug policy reform.
“When I first articulated a plan to legitimize a psychedelic-assisted therapy through FDA approval, many people said it was impossible,” Rick Doblin, PhD, founder and executive director of MAPS, said in the news release.
“Thirty-seven years later, we are on the precipice of bringing a novel therapy to the millions of Americans living with PTSD who haven’t found relief through current treatments,” said Dr. Doblin.
“The impossible became possible through the bravery of clinical trial participants, the compassion of mental health practitioners, and the generosity of thousands of donors. Today, we can imagine that MDMA-assisted therapy for PTSD may soon be available and accessible to all who could benefit,” Dr. Doblin added.
According to MAPS, phase 2 trials are being planned or conducted regarding the efficacy of MDMA-assisted therapies for substance use disorder and eating disorders, as well as couples therapy and group therapy among veterans.
Currently, no psychedelic-assisted therapy has been approved by the FDA or other regulatory authorities.
A version of this article first appeared on Medscape.com.
The MAPP2 study is the second randomized, double-blind, placebo-controlled study to demonstrate the safety and efficacy of MDMA-assisted therapy for PTSD.
The investigators confirm results of the MAPP1 study, which were published in Nature Medicine. Patients who received MDMA-assisted psychotherapy in MAPP1 demonstrated greater improvement in PTSD symptoms, mood, and empathy, compared with participants who received psychotherapy with placebo.
The design of the MAPP2 study was similar to that of MAPP1, and its results were similar, the nonprofit Multidisciplinary Association for Psychedelic Studies (MAPS), which sponsored MAPP1 and MAPP2, said in a news release.
No specific results from MAPP2 were provided at this time. The full data from MAPP2 are expected to be published in a peer-reviewed journal later this year, and a new drug application to the U.S. Food and Drug Administration will follow.
The FDA granted breakthrough therapy designation to MDMA as an adjunct to psychotherapy for adults with PTSD in 2017.
MAPS was founded in 1986 to fund and facilitate research into the potential of psychedelic-assisted therapies; to educate the public about psychedelics for medical, social, and spiritual use; and to advocate for drug policy reform.
“When I first articulated a plan to legitimize a psychedelic-assisted therapy through FDA approval, many people said it was impossible,” Rick Doblin, PhD, founder and executive director of MAPS, said in the news release.
“Thirty-seven years later, we are on the precipice of bringing a novel therapy to the millions of Americans living with PTSD who haven’t found relief through current treatments,” said Dr. Doblin.
“The impossible became possible through the bravery of clinical trial participants, the compassion of mental health practitioners, and the generosity of thousands of donors. Today, we can imagine that MDMA-assisted therapy for PTSD may soon be available and accessible to all who could benefit,” Dr. Doblin added.
According to MAPS, phase 2 trials are being planned or conducted regarding the efficacy of MDMA-assisted therapies for substance use disorder and eating disorders, as well as couples therapy and group therapy among veterans.
Currently, no psychedelic-assisted therapy has been approved by the FDA or other regulatory authorities.
A version of this article first appeared on Medscape.com.
The MAPP2 study is the second randomized, double-blind, placebo-controlled study to demonstrate the safety and efficacy of MDMA-assisted therapy for PTSD.
The investigators confirm results of the MAPP1 study, which were published in Nature Medicine. Patients who received MDMA-assisted psychotherapy in MAPP1 demonstrated greater improvement in PTSD symptoms, mood, and empathy, compared with participants who received psychotherapy with placebo.
The design of the MAPP2 study was similar to that of MAPP1, and its results were similar, the nonprofit Multidisciplinary Association for Psychedelic Studies (MAPS), which sponsored MAPP1 and MAPP2, said in a news release.
No specific results from MAPP2 were provided at this time. The full data from MAPP2 are expected to be published in a peer-reviewed journal later this year, and a new drug application to the U.S. Food and Drug Administration will follow.
The FDA granted breakthrough therapy designation to MDMA as an adjunct to psychotherapy for adults with PTSD in 2017.
MAPS was founded in 1986 to fund and facilitate research into the potential of psychedelic-assisted therapies; to educate the public about psychedelics for medical, social, and spiritual use; and to advocate for drug policy reform.
“When I first articulated a plan to legitimize a psychedelic-assisted therapy through FDA approval, many people said it was impossible,” Rick Doblin, PhD, founder and executive director of MAPS, said in the news release.
“Thirty-seven years later, we are on the precipice of bringing a novel therapy to the millions of Americans living with PTSD who haven’t found relief through current treatments,” said Dr. Doblin.
“The impossible became possible through the bravery of clinical trial participants, the compassion of mental health practitioners, and the generosity of thousands of donors. Today, we can imagine that MDMA-assisted therapy for PTSD may soon be available and accessible to all who could benefit,” Dr. Doblin added.
According to MAPS, phase 2 trials are being planned or conducted regarding the efficacy of MDMA-assisted therapies for substance use disorder and eating disorders, as well as couples therapy and group therapy among veterans.
Currently, no psychedelic-assisted therapy has been approved by the FDA or other regulatory authorities.
A version of this article first appeared on Medscape.com.
Novel antipsychotic ‘encouraging’ for resistant schizophrenia
The topline results from an exploratory study, which were released by the developer Newron Pharmaceuticals, are “very encouraging,” Stephen R. Marder, MD, professor of psychiatry and biobehavioral sciences at the University of California, Los Angeles, said in a company news release.
“The magnitude of the improvements experienced by these TRS patients, not responding to their current antipsychotic, on evenamide was substantial, improved over time, and was likely to be clinically meaningful,” Dr. Marder said.
First 100 patients
The topline results are based on the first 100 patients enrolled in study 014 and randomly assigned to receive evenamide at 7.5 mg, 15 mg, or 30 mg twice daily, as well as patients in the extension arm (study 015) that have completed 30 weeks.
Key findings released by the company included statistically significant improvement over baseline at 30 weeks (P < .001) in Positive and Negative Syndrome Scale (PANSS) scores, with continued improvement over that seen at 6 weeks.
The proportion of patients with clinically meaningful PANSS improvement at 30 weeks more than doubled from 16.5% at 6 weeks.
In addition, results showed statistically significant improvement (P < .001) at week 30 compared with baseline in illness severity as measured by the Clinical Global Impression of Severity (CGI-S), with continued improvement over that seen at 6 weeks.
The proportion of patients whose illness improved by at least one level of severity was 60% at week 6 and increased approximately by an additional 20% at week 30.
The proportion of patients judged to have clinically meaningful improvement, defined as at least “much improved,” on the Clinical Global Impression of Change (CGI-C) was 27% at week 6 – and increased a further 10% at week 30.
Evenamide was also well tolerated, with few adverse effects reported, and 85 of 100 patients remained on treatment at 30 weeks.
New options ‘desperately needed’
Newron plans to present the full results from study 014 at the European Congress of Psychiatry, scheduled for March 25-28 in Paris.
The extension study 015 is ongoing and will provide results on evenamide treatment for up to 1 year by the second quarter of 2023.
The company reported it expects to launch a randomized, placebo-controlled study (study 003) of the drug in TRS this year.
If the current results are confirmed in the randomized controlled trial, “evenamide would be the first medication that could be added to an antipsychotic to improve symptoms in treatment-refractory schizophrenia,” Dr. Marder said.
New therapeutic options for TRS, which occurs in about one-third of patients, are “desperately needed,” Ravi Anand, MD, chief medical officer at Newron, said in the release.
The reported data, comparing the effect of evenamide at 6 weeks vs. 6 months, “suggest that not only was there sustained improvement in the key measures, but the proportion of patients achieving clinically meaningful improvement increased over time,” Dr. Anand added.
A version of this article first appeared on Medscape.com.
The topline results from an exploratory study, which were released by the developer Newron Pharmaceuticals, are “very encouraging,” Stephen R. Marder, MD, professor of psychiatry and biobehavioral sciences at the University of California, Los Angeles, said in a company news release.
“The magnitude of the improvements experienced by these TRS patients, not responding to their current antipsychotic, on evenamide was substantial, improved over time, and was likely to be clinically meaningful,” Dr. Marder said.
First 100 patients
The topline results are based on the first 100 patients enrolled in study 014 and randomly assigned to receive evenamide at 7.5 mg, 15 mg, or 30 mg twice daily, as well as patients in the extension arm (study 015) that have completed 30 weeks.
Key findings released by the company included statistically significant improvement over baseline at 30 weeks (P < .001) in Positive and Negative Syndrome Scale (PANSS) scores, with continued improvement over that seen at 6 weeks.
The proportion of patients with clinically meaningful PANSS improvement at 30 weeks more than doubled from 16.5% at 6 weeks.
In addition, results showed statistically significant improvement (P < .001) at week 30 compared with baseline in illness severity as measured by the Clinical Global Impression of Severity (CGI-S), with continued improvement over that seen at 6 weeks.
The proportion of patients whose illness improved by at least one level of severity was 60% at week 6 and increased approximately by an additional 20% at week 30.
The proportion of patients judged to have clinically meaningful improvement, defined as at least “much improved,” on the Clinical Global Impression of Change (CGI-C) was 27% at week 6 – and increased a further 10% at week 30.
Evenamide was also well tolerated, with few adverse effects reported, and 85 of 100 patients remained on treatment at 30 weeks.
New options ‘desperately needed’
Newron plans to present the full results from study 014 at the European Congress of Psychiatry, scheduled for March 25-28 in Paris.
The extension study 015 is ongoing and will provide results on evenamide treatment for up to 1 year by the second quarter of 2023.
The company reported it expects to launch a randomized, placebo-controlled study (study 003) of the drug in TRS this year.
If the current results are confirmed in the randomized controlled trial, “evenamide would be the first medication that could be added to an antipsychotic to improve symptoms in treatment-refractory schizophrenia,” Dr. Marder said.
New therapeutic options for TRS, which occurs in about one-third of patients, are “desperately needed,” Ravi Anand, MD, chief medical officer at Newron, said in the release.
The reported data, comparing the effect of evenamide at 6 weeks vs. 6 months, “suggest that not only was there sustained improvement in the key measures, but the proportion of patients achieving clinically meaningful improvement increased over time,” Dr. Anand added.
A version of this article first appeared on Medscape.com.
The topline results from an exploratory study, which were released by the developer Newron Pharmaceuticals, are “very encouraging,” Stephen R. Marder, MD, professor of psychiatry and biobehavioral sciences at the University of California, Los Angeles, said in a company news release.
“The magnitude of the improvements experienced by these TRS patients, not responding to their current antipsychotic, on evenamide was substantial, improved over time, and was likely to be clinically meaningful,” Dr. Marder said.
First 100 patients
The topline results are based on the first 100 patients enrolled in study 014 and randomly assigned to receive evenamide at 7.5 mg, 15 mg, or 30 mg twice daily, as well as patients in the extension arm (study 015) that have completed 30 weeks.
Key findings released by the company included statistically significant improvement over baseline at 30 weeks (P < .001) in Positive and Negative Syndrome Scale (PANSS) scores, with continued improvement over that seen at 6 weeks.
The proportion of patients with clinically meaningful PANSS improvement at 30 weeks more than doubled from 16.5% at 6 weeks.
In addition, results showed statistically significant improvement (P < .001) at week 30 compared with baseline in illness severity as measured by the Clinical Global Impression of Severity (CGI-S), with continued improvement over that seen at 6 weeks.
The proportion of patients whose illness improved by at least one level of severity was 60% at week 6 and increased approximately by an additional 20% at week 30.
The proportion of patients judged to have clinically meaningful improvement, defined as at least “much improved,” on the Clinical Global Impression of Change (CGI-C) was 27% at week 6 – and increased a further 10% at week 30.
Evenamide was also well tolerated, with few adverse effects reported, and 85 of 100 patients remained on treatment at 30 weeks.
New options ‘desperately needed’
Newron plans to present the full results from study 014 at the European Congress of Psychiatry, scheduled for March 25-28 in Paris.
The extension study 015 is ongoing and will provide results on evenamide treatment for up to 1 year by the second quarter of 2023.
The company reported it expects to launch a randomized, placebo-controlled study (study 003) of the drug in TRS this year.
If the current results are confirmed in the randomized controlled trial, “evenamide would be the first medication that could be added to an antipsychotic to improve symptoms in treatment-refractory schizophrenia,” Dr. Marder said.
New therapeutic options for TRS, which occurs in about one-third of patients, are “desperately needed,” Ravi Anand, MD, chief medical officer at Newron, said in the release.
The reported data, comparing the effect of evenamide at 6 weeks vs. 6 months, “suggest that not only was there sustained improvement in the key measures, but the proportion of patients achieving clinically meaningful improvement increased over time,” Dr. Anand added.
A version of this article first appeared on Medscape.com.
Renowned stroke expert Ralph L. Sacco, MD, dies
Ralph L. Sacco, MD, the first neurologist to serve as president of the American Heart Association and the only physician to serve as president of both the AHA and the American Academy of Neurology, died Jan. 17 at the age of 65.
He died of a brain tumor at his home in Amagansett, N.Y., according to an obituary published in Neurology, Circulation, and Stroke.
“Ralph was one of a kind,” Nancy Brown, chief executive officer for the AHA and American Stroke Association, said in a statement. “His leadership was unparalleled, and his warm, generous heart and care transcended his research and clinic to every person fortunate to meet him and likely become a friend,” Ms. Brown said.
In a tweet, Natalia S. Rost, MD, professor of neurology at Harvard Medical School, Boston, called him, “a dear friend, an inspiring colleague, a generous mentor, an astute scientist, a consummate advocate for brain health worldwide.”
Dedicated to improving stroke care
Dr. Sacco was chair of the University of Miami Miller School of Medicine in the department of neurology; the Olemberg Family Chair in Neurological Disorders; professor of neurology, public health sciences, human genetics, and neurosurgery; executive director of the Evelyn F. McKnight Brain Institute; director and multi-principal investigator of the Miami Clinical and Translational Science Institute; and senior associate dean for clinical and translational science.
Dr. Sacco was a population-based researcher in the field of cerebrovascular diseases.
As founder of the Northern Manhattan Study, he paved the way for examining the differences in stroke risk related to race, ethnicity, sex, and neighborhood, and realizing the impact of modifiable lifestyle behaviors, such as alcohol consumption and physical activity, on stroke risk.
Dr. Sacco’s work led to more targeted stroke prevention programs and his “drive and dedication fueled changes that improved stroke research and fostered the development of targeted stroke care delivery, ultimately improving stroke recovery and post-stroke quality of life for many,” the AHA statement said.
Dr. Sacco was also founder and executive director of the Florida Stroke Registry, which consists of 167 Florida stroke centers. He was a member of the National Academy of Medicine.
In an obituary written by Orly Avitzur, MD, current president of the AAN, she notes that he “was the only physician to have become both the president of the AHA (2010-2011) and the AAN (2017-2019), positions that reflected the respect and admiration of professional colleagues earned over the years.”
During his tenure as AAN president, Dr. Sacco led an initiative to ensure that academic neurology, from department chairs to professors to students, knew about the abundance of academy resources available to them, the AAN noted in a statement.
Dr. Sacco was a “strong proponent of enlarging the neurology workforce through the academic pipeline and promoted the concept of the ‘newrologist’ to get people excited in careers in neurology, moving beyond just diagnosis and treatments to include interventions, preventative care, and the future of regenerative care,” the AAN said.
Dr. Sacco received numerous awards throughout his career, most recently the AHA 2022 Distinguished Scientist award. He also received the 2015 Gold Heart Award, the 2011 Distinguished National Leadership Award, and the 2006 William Feinberg Award.
In addition to his husband, Scott Dutcher, Dr. Sacco is survived by his father, Anthony P. Sacco, and his father’s wife, Rosemary; and his four siblings and their families, along with many nieces and nephews.
A version of this article first appeared on Medscape.com.
Ralph L. Sacco, MD, the first neurologist to serve as president of the American Heart Association and the only physician to serve as president of both the AHA and the American Academy of Neurology, died Jan. 17 at the age of 65.
He died of a brain tumor at his home in Amagansett, N.Y., according to an obituary published in Neurology, Circulation, and Stroke.
“Ralph was one of a kind,” Nancy Brown, chief executive officer for the AHA and American Stroke Association, said in a statement. “His leadership was unparalleled, and his warm, generous heart and care transcended his research and clinic to every person fortunate to meet him and likely become a friend,” Ms. Brown said.
In a tweet, Natalia S. Rost, MD, professor of neurology at Harvard Medical School, Boston, called him, “a dear friend, an inspiring colleague, a generous mentor, an astute scientist, a consummate advocate for brain health worldwide.”
Dedicated to improving stroke care
Dr. Sacco was chair of the University of Miami Miller School of Medicine in the department of neurology; the Olemberg Family Chair in Neurological Disorders; professor of neurology, public health sciences, human genetics, and neurosurgery; executive director of the Evelyn F. McKnight Brain Institute; director and multi-principal investigator of the Miami Clinical and Translational Science Institute; and senior associate dean for clinical and translational science.
Dr. Sacco was a population-based researcher in the field of cerebrovascular diseases.
As founder of the Northern Manhattan Study, he paved the way for examining the differences in stroke risk related to race, ethnicity, sex, and neighborhood, and realizing the impact of modifiable lifestyle behaviors, such as alcohol consumption and physical activity, on stroke risk.
Dr. Sacco’s work led to more targeted stroke prevention programs and his “drive and dedication fueled changes that improved stroke research and fostered the development of targeted stroke care delivery, ultimately improving stroke recovery and post-stroke quality of life for many,” the AHA statement said.
Dr. Sacco was also founder and executive director of the Florida Stroke Registry, which consists of 167 Florida stroke centers. He was a member of the National Academy of Medicine.
In an obituary written by Orly Avitzur, MD, current president of the AAN, she notes that he “was the only physician to have become both the president of the AHA (2010-2011) and the AAN (2017-2019), positions that reflected the respect and admiration of professional colleagues earned over the years.”
During his tenure as AAN president, Dr. Sacco led an initiative to ensure that academic neurology, from department chairs to professors to students, knew about the abundance of academy resources available to them, the AAN noted in a statement.
Dr. Sacco was a “strong proponent of enlarging the neurology workforce through the academic pipeline and promoted the concept of the ‘newrologist’ to get people excited in careers in neurology, moving beyond just diagnosis and treatments to include interventions, preventative care, and the future of regenerative care,” the AAN said.
Dr. Sacco received numerous awards throughout his career, most recently the AHA 2022 Distinguished Scientist award. He also received the 2015 Gold Heart Award, the 2011 Distinguished National Leadership Award, and the 2006 William Feinberg Award.
In addition to his husband, Scott Dutcher, Dr. Sacco is survived by his father, Anthony P. Sacco, and his father’s wife, Rosemary; and his four siblings and their families, along with many nieces and nephews.
A version of this article first appeared on Medscape.com.
Ralph L. Sacco, MD, the first neurologist to serve as president of the American Heart Association and the only physician to serve as president of both the AHA and the American Academy of Neurology, died Jan. 17 at the age of 65.
He died of a brain tumor at his home in Amagansett, N.Y., according to an obituary published in Neurology, Circulation, and Stroke.
“Ralph was one of a kind,” Nancy Brown, chief executive officer for the AHA and American Stroke Association, said in a statement. “His leadership was unparalleled, and his warm, generous heart and care transcended his research and clinic to every person fortunate to meet him and likely become a friend,” Ms. Brown said.
In a tweet, Natalia S. Rost, MD, professor of neurology at Harvard Medical School, Boston, called him, “a dear friend, an inspiring colleague, a generous mentor, an astute scientist, a consummate advocate for brain health worldwide.”
Dedicated to improving stroke care
Dr. Sacco was chair of the University of Miami Miller School of Medicine in the department of neurology; the Olemberg Family Chair in Neurological Disorders; professor of neurology, public health sciences, human genetics, and neurosurgery; executive director of the Evelyn F. McKnight Brain Institute; director and multi-principal investigator of the Miami Clinical and Translational Science Institute; and senior associate dean for clinical and translational science.
Dr. Sacco was a population-based researcher in the field of cerebrovascular diseases.
As founder of the Northern Manhattan Study, he paved the way for examining the differences in stroke risk related to race, ethnicity, sex, and neighborhood, and realizing the impact of modifiable lifestyle behaviors, such as alcohol consumption and physical activity, on stroke risk.
Dr. Sacco’s work led to more targeted stroke prevention programs and his “drive and dedication fueled changes that improved stroke research and fostered the development of targeted stroke care delivery, ultimately improving stroke recovery and post-stroke quality of life for many,” the AHA statement said.
Dr. Sacco was also founder and executive director of the Florida Stroke Registry, which consists of 167 Florida stroke centers. He was a member of the National Academy of Medicine.
In an obituary written by Orly Avitzur, MD, current president of the AAN, she notes that he “was the only physician to have become both the president of the AHA (2010-2011) and the AAN (2017-2019), positions that reflected the respect and admiration of professional colleagues earned over the years.”
During his tenure as AAN president, Dr. Sacco led an initiative to ensure that academic neurology, from department chairs to professors to students, knew about the abundance of academy resources available to them, the AAN noted in a statement.
Dr. Sacco was a “strong proponent of enlarging the neurology workforce through the academic pipeline and promoted the concept of the ‘newrologist’ to get people excited in careers in neurology, moving beyond just diagnosis and treatments to include interventions, preventative care, and the future of regenerative care,” the AAN said.
Dr. Sacco received numerous awards throughout his career, most recently the AHA 2022 Distinguished Scientist award. He also received the 2015 Gold Heart Award, the 2011 Distinguished National Leadership Award, and the 2006 William Feinberg Award.
In addition to his husband, Scott Dutcher, Dr. Sacco is survived by his father, Anthony P. Sacco, and his father’s wife, Rosemary; and his four siblings and their families, along with many nieces and nephews.
A version of this article first appeared on Medscape.com.
Diet packed with fast food found hard on the liver
The study finds that getting one-fifth or more of total daily calories from fast food can increase the risk of nonalcoholic fatty liver disease, which can lead to cirrhosis and its complications, including liver failure and liver cancer.
Although the magnitude of association was modest among the general population, “striking” elevations in steatosis were evident among persons with obesity and diabetes who consumed fast food, in comparison with their counterparts who did not have obesity and diabetes, the researchers reported.
“My hope is that this study encourages people to seek out more nutritious, healthy food options and provides information that clinicians can use to counsel their patients, particularly those with underlying metabolic risk factors, of the importance of avoiding foods that are high in fat, carbohydrates, and processed sugars,” lead investigator Ani Kardashian, MD, hepatologist with the University of Southern California, Los Angeles, said in an interview.
“At a policy level, public health efforts are needed to improve access to affordable, healthy, and nutritious food options across the U.S. This is especially important as more people have turned to fast foods during the pandemic and as the price of food as risen dramatically over the past year due to food inflation,” Dr. Kardashian added.
The study was published online in Clinical Gastroenterology and Hepatology.
More fast food, greater steatosis
The findings are based on data from 3,954 adults who participated in the National Health and Nutrition Examination Survey (NHANES) of 2017-2018 and who underwent vibration-controlled transient elastography. Of these participants, data regarding 1- or 2-day dietary recall were available.
Steatosis, the primary outcome, was measured via controlled attenuation parameter (CAP). Two validated cutoffs were utilized (CAP ≥ 263 dB/m and CAP ≥ 285 dB/m).
Of those surveyed, 52% consumed any fast food, and 29% derived 20% or more of their daily calories from fast food.
Fast-food intake of 20% or more of daily calories was significantly associated with greater steatosis after multivariable adjustment, both as a continuous measure (4.6 dB/m higher CAP score) and with respect to the CAP ≥ 263 dB/m cutoff (odds ratio [OR], 1.45).
“The negative effects are particularly severe in people who already have diabetes and obesity,” Dr. Kardashian told this news organization.
For example, with diabetes and fast-food intake of 20% or more of daily calories, the ORs of meeting the CAP ≥ 263 dB/m cutoff and the CAP ≥ 285 dB/m cutoff were 2.3 and 2.48, respectively.
The researchers said their findings are particularly “alarming,” given the overall increase in fast-food consumption over the past 50 years in the United States, regardless of socioeconomic status.
Diet coaching
The finding that fast food has more deleterious impact on those with obesity and diabetes “emphasizes that it is not just one insult but multiple factors that contribute to overall health,” said Nancy Reau, MD, section chief of hepatology at Rush University Medical Center in Chicago.
“This is actually great news, because diet is modifiable, vs. your genetics, which you currently can’t change. This doesn’t mean if you’re lean you can eat whatever you want, but if you are overweight, being careful with your diet does have impact, even if it doesn’t lead to substantial weight changes,” said Dr. Reau, who is not affiliated with the study.
For people who have limited options and need to eat fast food, “there are healthy choices at most restaurants; you just need to be smart about reading labels, watching calories, and ordering the healthier options,” Dr. Reau said in an interview.
Fast food and fatty liver go “hand in hand,” Lisa Ganjhu, DO, gastroenterologist and hepatologist at NYU Langone Health in New York, told this news organization.
“I counsel and coach my patients on healthy diet and exercise, and I’ve been pretty successful,” said Dr. Ganjhu, who was not involved with the study.
“If my patient is eating at McDonald’s a lot, I basically walk through the menu with them and help them find something healthy. When patients see the benefits of cutting out fat and reducing carbohydrates, they are more apt to continue,” Dr. Ganjhu said.
The study was funded by the University of Southern California. Dr. Kardashian, Dr. Reau, and Dr. Ganjhu have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study finds that getting one-fifth or more of total daily calories from fast food can increase the risk of nonalcoholic fatty liver disease, which can lead to cirrhosis and its complications, including liver failure and liver cancer.
Although the magnitude of association was modest among the general population, “striking” elevations in steatosis were evident among persons with obesity and diabetes who consumed fast food, in comparison with their counterparts who did not have obesity and diabetes, the researchers reported.
“My hope is that this study encourages people to seek out more nutritious, healthy food options and provides information that clinicians can use to counsel their patients, particularly those with underlying metabolic risk factors, of the importance of avoiding foods that are high in fat, carbohydrates, and processed sugars,” lead investigator Ani Kardashian, MD, hepatologist with the University of Southern California, Los Angeles, said in an interview.
“At a policy level, public health efforts are needed to improve access to affordable, healthy, and nutritious food options across the U.S. This is especially important as more people have turned to fast foods during the pandemic and as the price of food as risen dramatically over the past year due to food inflation,” Dr. Kardashian added.
The study was published online in Clinical Gastroenterology and Hepatology.
More fast food, greater steatosis
The findings are based on data from 3,954 adults who participated in the National Health and Nutrition Examination Survey (NHANES) of 2017-2018 and who underwent vibration-controlled transient elastography. Of these participants, data regarding 1- or 2-day dietary recall were available.
Steatosis, the primary outcome, was measured via controlled attenuation parameter (CAP). Two validated cutoffs were utilized (CAP ≥ 263 dB/m and CAP ≥ 285 dB/m).
Of those surveyed, 52% consumed any fast food, and 29% derived 20% or more of their daily calories from fast food.
Fast-food intake of 20% or more of daily calories was significantly associated with greater steatosis after multivariable adjustment, both as a continuous measure (4.6 dB/m higher CAP score) and with respect to the CAP ≥ 263 dB/m cutoff (odds ratio [OR], 1.45).
“The negative effects are particularly severe in people who already have diabetes and obesity,” Dr. Kardashian told this news organization.
For example, with diabetes and fast-food intake of 20% or more of daily calories, the ORs of meeting the CAP ≥ 263 dB/m cutoff and the CAP ≥ 285 dB/m cutoff were 2.3 and 2.48, respectively.
The researchers said their findings are particularly “alarming,” given the overall increase in fast-food consumption over the past 50 years in the United States, regardless of socioeconomic status.
Diet coaching
The finding that fast food has more deleterious impact on those with obesity and diabetes “emphasizes that it is not just one insult but multiple factors that contribute to overall health,” said Nancy Reau, MD, section chief of hepatology at Rush University Medical Center in Chicago.
“This is actually great news, because diet is modifiable, vs. your genetics, which you currently can’t change. This doesn’t mean if you’re lean you can eat whatever you want, but if you are overweight, being careful with your diet does have impact, even if it doesn’t lead to substantial weight changes,” said Dr. Reau, who is not affiliated with the study.
For people who have limited options and need to eat fast food, “there are healthy choices at most restaurants; you just need to be smart about reading labels, watching calories, and ordering the healthier options,” Dr. Reau said in an interview.
Fast food and fatty liver go “hand in hand,” Lisa Ganjhu, DO, gastroenterologist and hepatologist at NYU Langone Health in New York, told this news organization.
“I counsel and coach my patients on healthy diet and exercise, and I’ve been pretty successful,” said Dr. Ganjhu, who was not involved with the study.
“If my patient is eating at McDonald’s a lot, I basically walk through the menu with them and help them find something healthy. When patients see the benefits of cutting out fat and reducing carbohydrates, they are more apt to continue,” Dr. Ganjhu said.
The study was funded by the University of Southern California. Dr. Kardashian, Dr. Reau, and Dr. Ganjhu have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study finds that getting one-fifth or more of total daily calories from fast food can increase the risk of nonalcoholic fatty liver disease, which can lead to cirrhosis and its complications, including liver failure and liver cancer.
Although the magnitude of association was modest among the general population, “striking” elevations in steatosis were evident among persons with obesity and diabetes who consumed fast food, in comparison with their counterparts who did not have obesity and diabetes, the researchers reported.
“My hope is that this study encourages people to seek out more nutritious, healthy food options and provides information that clinicians can use to counsel their patients, particularly those with underlying metabolic risk factors, of the importance of avoiding foods that are high in fat, carbohydrates, and processed sugars,” lead investigator Ani Kardashian, MD, hepatologist with the University of Southern California, Los Angeles, said in an interview.
“At a policy level, public health efforts are needed to improve access to affordable, healthy, and nutritious food options across the U.S. This is especially important as more people have turned to fast foods during the pandemic and as the price of food as risen dramatically over the past year due to food inflation,” Dr. Kardashian added.
The study was published online in Clinical Gastroenterology and Hepatology.
More fast food, greater steatosis
The findings are based on data from 3,954 adults who participated in the National Health and Nutrition Examination Survey (NHANES) of 2017-2018 and who underwent vibration-controlled transient elastography. Of these participants, data regarding 1- or 2-day dietary recall were available.
Steatosis, the primary outcome, was measured via controlled attenuation parameter (CAP). Two validated cutoffs were utilized (CAP ≥ 263 dB/m and CAP ≥ 285 dB/m).
Of those surveyed, 52% consumed any fast food, and 29% derived 20% or more of their daily calories from fast food.
Fast-food intake of 20% or more of daily calories was significantly associated with greater steatosis after multivariable adjustment, both as a continuous measure (4.6 dB/m higher CAP score) and with respect to the CAP ≥ 263 dB/m cutoff (odds ratio [OR], 1.45).
“The negative effects are particularly severe in people who already have diabetes and obesity,” Dr. Kardashian told this news organization.
For example, with diabetes and fast-food intake of 20% or more of daily calories, the ORs of meeting the CAP ≥ 263 dB/m cutoff and the CAP ≥ 285 dB/m cutoff were 2.3 and 2.48, respectively.
The researchers said their findings are particularly “alarming,” given the overall increase in fast-food consumption over the past 50 years in the United States, regardless of socioeconomic status.
Diet coaching
The finding that fast food has more deleterious impact on those with obesity and diabetes “emphasizes that it is not just one insult but multiple factors that contribute to overall health,” said Nancy Reau, MD, section chief of hepatology at Rush University Medical Center in Chicago.
“This is actually great news, because diet is modifiable, vs. your genetics, which you currently can’t change. This doesn’t mean if you’re lean you can eat whatever you want, but if you are overweight, being careful with your diet does have impact, even if it doesn’t lead to substantial weight changes,” said Dr. Reau, who is not affiliated with the study.
For people who have limited options and need to eat fast food, “there are healthy choices at most restaurants; you just need to be smart about reading labels, watching calories, and ordering the healthier options,” Dr. Reau said in an interview.
Fast food and fatty liver go “hand in hand,” Lisa Ganjhu, DO, gastroenterologist and hepatologist at NYU Langone Health in New York, told this news organization.
“I counsel and coach my patients on healthy diet and exercise, and I’ve been pretty successful,” said Dr. Ganjhu, who was not involved with the study.
“If my patient is eating at McDonald’s a lot, I basically walk through the menu with them and help them find something healthy. When patients see the benefits of cutting out fat and reducing carbohydrates, they are more apt to continue,” Dr. Ganjhu said.
The study was funded by the University of Southern California. Dr. Kardashian, Dr. Reau, and Dr. Ganjhu have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Can 6 minutes of intense cycling put the brakes on Alzheimer’s?
new research suggests.
In a small study of healthy adults, 6 minutes of high-intensity cycling increased circulating levels of brain-derived neurotrophic factor (BDNF) to a significantly greater extent than prolonged light cycling or fasting.
However, the data do not suggest that 6 minutes of high-intensity exercise “wards off dementia,” cautioned lead investigator Travis Gibbons, MSc, PhD candidate in environmental physiology at the University of Otago (New Zealand), Dunedin, and now postdoctoral fellow at the University of British Columbia – Okanagan, Kelowna.
“Like all science, this is just a small piece that supports a potential mechanistic role for how exercise might improve brain health,” Dr. Gibbons told this news organization.
The findings were published online in the Journal of Physiology.
Targeting BDNF
Both intermittent fasting and exercise have previously been shown to have potent neuroprotective effects; and an acute upregulation of BDNF appears to be a common mechanistic link.
To tease apart the influence of fasting and exercise on BDNF production, Dr. Gibbons and colleagues studied 12 aerobically fit, healthy men (n = 6) and women (n = 6) aged 20-40 years.
In a study that employed a repeated-measures crossover design, they assessed circulating BDNF levels after a 20-hour fast, prolonged (90-min) light cycling, short (6-min) high-intensity cycling, and combined fasting and exercise.
Six minutes of high-intensity exercise appeared to be the most efficient way to increase BDNF.
Fasting for 20 hours led to a ninefold increase in ketone body delivery to the brain but had no effect on any metric of BDNF in peripheral circulation at rest or during exercise.
Six minutes of high-intensity exercise increased every metric of circulating BDNF four to five times more than prolonged low-intensity exercise.
In addition, the increase in plasma-derived BDNF correlated with a sixfold increase in circulating lactate irrespective of feeding or fasting state.
Lactate delivery?
“My leading theory is that, during and following intense exercise, lactate produced by muscles is delivered and consumed by the brain,” Dr. Gibbons noted.
“It takes high-intensity exercise to provoke this ‘cerebral substrate switch’ from glucose to lactate. Critically, this cerebral substrate switch has been shown to contribute to the early processes that upregulate BDNF production in the brain,” he said.
However, “Whether this translates to ‘warding off dementia’ is not clear,” Dr. Gibbons added.
The study also suggests that increases in plasma volume and platelet concentration appear to play a role in concentrating BDNF in the circulation during exercise.
The investigators note that BDNF and other neurotrophic-based pharmaceutical therapies have shown “great promise” in slowing and even arresting neurodegenerative processes in animals, but attempts to harness the protective power of BDNF in human neurodegeneration have thus far failed.
“Whether episodically upregulating BDNF production with intense exercise is an effective strategy to curb age-related cognitive decline in humans is unknown, but animal models indicate that it is and that BDNF plays a primary role,” the researchers write.
Funding for the study was provided by the Healthcare Otago Charitable Trust. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In a small study of healthy adults, 6 minutes of high-intensity cycling increased circulating levels of brain-derived neurotrophic factor (BDNF) to a significantly greater extent than prolonged light cycling or fasting.
However, the data do not suggest that 6 minutes of high-intensity exercise “wards off dementia,” cautioned lead investigator Travis Gibbons, MSc, PhD candidate in environmental physiology at the University of Otago (New Zealand), Dunedin, and now postdoctoral fellow at the University of British Columbia – Okanagan, Kelowna.
“Like all science, this is just a small piece that supports a potential mechanistic role for how exercise might improve brain health,” Dr. Gibbons told this news organization.
The findings were published online in the Journal of Physiology.
Targeting BDNF
Both intermittent fasting and exercise have previously been shown to have potent neuroprotective effects; and an acute upregulation of BDNF appears to be a common mechanistic link.
To tease apart the influence of fasting and exercise on BDNF production, Dr. Gibbons and colleagues studied 12 aerobically fit, healthy men (n = 6) and women (n = 6) aged 20-40 years.
In a study that employed a repeated-measures crossover design, they assessed circulating BDNF levels after a 20-hour fast, prolonged (90-min) light cycling, short (6-min) high-intensity cycling, and combined fasting and exercise.
Six minutes of high-intensity exercise appeared to be the most efficient way to increase BDNF.
Fasting for 20 hours led to a ninefold increase in ketone body delivery to the brain but had no effect on any metric of BDNF in peripheral circulation at rest or during exercise.
Six minutes of high-intensity exercise increased every metric of circulating BDNF four to five times more than prolonged low-intensity exercise.
In addition, the increase in plasma-derived BDNF correlated with a sixfold increase in circulating lactate irrespective of feeding or fasting state.
Lactate delivery?
“My leading theory is that, during and following intense exercise, lactate produced by muscles is delivered and consumed by the brain,” Dr. Gibbons noted.
“It takes high-intensity exercise to provoke this ‘cerebral substrate switch’ from glucose to lactate. Critically, this cerebral substrate switch has been shown to contribute to the early processes that upregulate BDNF production in the brain,” he said.
However, “Whether this translates to ‘warding off dementia’ is not clear,” Dr. Gibbons added.
The study also suggests that increases in plasma volume and platelet concentration appear to play a role in concentrating BDNF in the circulation during exercise.
The investigators note that BDNF and other neurotrophic-based pharmaceutical therapies have shown “great promise” in slowing and even arresting neurodegenerative processes in animals, but attempts to harness the protective power of BDNF in human neurodegeneration have thus far failed.
“Whether episodically upregulating BDNF production with intense exercise is an effective strategy to curb age-related cognitive decline in humans is unknown, but animal models indicate that it is and that BDNF plays a primary role,” the researchers write.
Funding for the study was provided by the Healthcare Otago Charitable Trust. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In a small study of healthy adults, 6 minutes of high-intensity cycling increased circulating levels of brain-derived neurotrophic factor (BDNF) to a significantly greater extent than prolonged light cycling or fasting.
However, the data do not suggest that 6 minutes of high-intensity exercise “wards off dementia,” cautioned lead investigator Travis Gibbons, MSc, PhD candidate in environmental physiology at the University of Otago (New Zealand), Dunedin, and now postdoctoral fellow at the University of British Columbia – Okanagan, Kelowna.
“Like all science, this is just a small piece that supports a potential mechanistic role for how exercise might improve brain health,” Dr. Gibbons told this news organization.
The findings were published online in the Journal of Physiology.
Targeting BDNF
Both intermittent fasting and exercise have previously been shown to have potent neuroprotective effects; and an acute upregulation of BDNF appears to be a common mechanistic link.
To tease apart the influence of fasting and exercise on BDNF production, Dr. Gibbons and colleagues studied 12 aerobically fit, healthy men (n = 6) and women (n = 6) aged 20-40 years.
In a study that employed a repeated-measures crossover design, they assessed circulating BDNF levels after a 20-hour fast, prolonged (90-min) light cycling, short (6-min) high-intensity cycling, and combined fasting and exercise.
Six minutes of high-intensity exercise appeared to be the most efficient way to increase BDNF.
Fasting for 20 hours led to a ninefold increase in ketone body delivery to the brain but had no effect on any metric of BDNF in peripheral circulation at rest or during exercise.
Six minutes of high-intensity exercise increased every metric of circulating BDNF four to five times more than prolonged low-intensity exercise.
In addition, the increase in plasma-derived BDNF correlated with a sixfold increase in circulating lactate irrespective of feeding or fasting state.
Lactate delivery?
“My leading theory is that, during and following intense exercise, lactate produced by muscles is delivered and consumed by the brain,” Dr. Gibbons noted.
“It takes high-intensity exercise to provoke this ‘cerebral substrate switch’ from glucose to lactate. Critically, this cerebral substrate switch has been shown to contribute to the early processes that upregulate BDNF production in the brain,” he said.
However, “Whether this translates to ‘warding off dementia’ is not clear,” Dr. Gibbons added.
The study also suggests that increases in plasma volume and platelet concentration appear to play a role in concentrating BDNF in the circulation during exercise.
The investigators note that BDNF and other neurotrophic-based pharmaceutical therapies have shown “great promise” in slowing and even arresting neurodegenerative processes in animals, but attempts to harness the protective power of BDNF in human neurodegeneration have thus far failed.
“Whether episodically upregulating BDNF production with intense exercise is an effective strategy to curb age-related cognitive decline in humans is unknown, but animal models indicate that it is and that BDNF plays a primary role,” the researchers write.
Funding for the study was provided by the Healthcare Otago Charitable Trust. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF PHYSIOLOGY
‘Clinical paradox’? Bariatric surgery may protect from GI cancers
In fact, an analysis of close to 1 million French adults suggests that the weight-loss surgery may offer some protection against these cancers.
The study results present a “clinical paradox,” according to authors of a commentary published this week along with the study in JAMA Surgery. A procedure known to increase the risk of gastroesophageal reflux disease (GERD), and potentially adenocarcinoma of the distal esophagus and gastroesophageal junction, may help shield patients from esophagogastric cancer.
The study marks “an important step toward improving the understanding of potential lifetime risks of bariatric surgery and overall major health benefits of surgically induced weight loss,” commentary authors Piotr Gorecki, MD, and Michael Zenilman, MD, with Weill Cornell Medicine in New York, write.
Recent data indicate that excess body weight is associated with nearly 8% of cancer cases and 6.5% of cancer deaths. Studies also show that bariatric surgery can reduce the risk of some cancers, but whether this extends to esophageal and gastric cancer remains unclear.
To investigate, the researchers used French national data to compare the incidence of esophageal and gastric cancer in 303,709 mostly female patients with obesity who underwent bariatric surgery and a matched group of 605,140 patients with obesity who did not undergo the surgery.
The mean age of the cohort was about 40 years. The mean period of follow-up was 6 years for the surgery group and 5.6 years for the control arm. A total of 337 patients underwent esophagogastric cancer – 83 in the surgical group and 254 in the control group. Gastric cancer was about two times more common than esophageal cancer (225 vs. 112 patients).
The incidence rate of esophagogastric cancer was higher in the control group than in the surgery group – 6.9 vs. 4.9 cases per 100,000 population per year, for an incidence rate ratio of 1.42 (P = .005).
Bariatric surgery was associated with a significant 24% lower risk of esophagogastric cancer (hazard ratio, 0.76; P = .03) and a 40% lower risk of overall in-hospital mortality, defined as “any death occurring during a hospital stay regardless of the cause” (HR, 0.60; P < .001).
The authors also found no significant difference in cancer outcomes and type of bariatric procedure, which included sleeve gastrectomy, gastric bypass, and adjustable gastric banding.
They note that key study limitations include the retrospective design, limited follow-up period, and lack of histologic data on the specific cancers. In addition, the study population was relatively young, whereas esophageal cancer is more common in older people.
But overall, the findings suggest that bariatric surgery can be performed to treat severe obesity without increasing the risk of esophageal and gastric cancer, the authors conclude.
“It seems that the balance between protective factors (weight loss, metabolic effects, and eradication of H. pylori infection) and risk factors (GERD and bile reflux) for cancer after bariatric surgery is in favor of protective factors,” the authors, led by Andrea Lazzati, MD, PhD, of Centre Hospitalier Intercommunal de Créteil, France, explain.
Although the potential protective mechanisms remain unclear, in their commentary, Dr. Gorecki and Dr. Zenilman suggest that a reduction in chronic inflammation and immunosuppression following bariatric surgery could help explain the results.
Although the study provides “reassurance of the protective clinical benefits of weight loss surgery,” more large-scale studies are needed to “better identify, elucidate, and address the pathophysiological processes of bariatric procedure,” Dr. Gorecki and Dr. Zenilman conclude.
No specific funding for the study was reported. Dr. Lazzati has received personal fees from Johnson & Johnson, Medtronic, and Gore. Dr. Zenilman has received personal fees from Academic Medical Professionals Insurance and Mohamed & Obaid Almulla Group.
A version of this article first appeared on Medscape.com.
In fact, an analysis of close to 1 million French adults suggests that the weight-loss surgery may offer some protection against these cancers.
The study results present a “clinical paradox,” according to authors of a commentary published this week along with the study in JAMA Surgery. A procedure known to increase the risk of gastroesophageal reflux disease (GERD), and potentially adenocarcinoma of the distal esophagus and gastroesophageal junction, may help shield patients from esophagogastric cancer.
The study marks “an important step toward improving the understanding of potential lifetime risks of bariatric surgery and overall major health benefits of surgically induced weight loss,” commentary authors Piotr Gorecki, MD, and Michael Zenilman, MD, with Weill Cornell Medicine in New York, write.
Recent data indicate that excess body weight is associated with nearly 8% of cancer cases and 6.5% of cancer deaths. Studies also show that bariatric surgery can reduce the risk of some cancers, but whether this extends to esophageal and gastric cancer remains unclear.
To investigate, the researchers used French national data to compare the incidence of esophageal and gastric cancer in 303,709 mostly female patients with obesity who underwent bariatric surgery and a matched group of 605,140 patients with obesity who did not undergo the surgery.
The mean age of the cohort was about 40 years. The mean period of follow-up was 6 years for the surgery group and 5.6 years for the control arm. A total of 337 patients underwent esophagogastric cancer – 83 in the surgical group and 254 in the control group. Gastric cancer was about two times more common than esophageal cancer (225 vs. 112 patients).
The incidence rate of esophagogastric cancer was higher in the control group than in the surgery group – 6.9 vs. 4.9 cases per 100,000 population per year, for an incidence rate ratio of 1.42 (P = .005).
Bariatric surgery was associated with a significant 24% lower risk of esophagogastric cancer (hazard ratio, 0.76; P = .03) and a 40% lower risk of overall in-hospital mortality, defined as “any death occurring during a hospital stay regardless of the cause” (HR, 0.60; P < .001).
The authors also found no significant difference in cancer outcomes and type of bariatric procedure, which included sleeve gastrectomy, gastric bypass, and adjustable gastric banding.
They note that key study limitations include the retrospective design, limited follow-up period, and lack of histologic data on the specific cancers. In addition, the study population was relatively young, whereas esophageal cancer is more common in older people.
But overall, the findings suggest that bariatric surgery can be performed to treat severe obesity without increasing the risk of esophageal and gastric cancer, the authors conclude.
“It seems that the balance between protective factors (weight loss, metabolic effects, and eradication of H. pylori infection) and risk factors (GERD and bile reflux) for cancer after bariatric surgery is in favor of protective factors,” the authors, led by Andrea Lazzati, MD, PhD, of Centre Hospitalier Intercommunal de Créteil, France, explain.
Although the potential protective mechanisms remain unclear, in their commentary, Dr. Gorecki and Dr. Zenilman suggest that a reduction in chronic inflammation and immunosuppression following bariatric surgery could help explain the results.
Although the study provides “reassurance of the protective clinical benefits of weight loss surgery,” more large-scale studies are needed to “better identify, elucidate, and address the pathophysiological processes of bariatric procedure,” Dr. Gorecki and Dr. Zenilman conclude.
No specific funding for the study was reported. Dr. Lazzati has received personal fees from Johnson & Johnson, Medtronic, and Gore. Dr. Zenilman has received personal fees from Academic Medical Professionals Insurance and Mohamed & Obaid Almulla Group.
A version of this article first appeared on Medscape.com.
In fact, an analysis of close to 1 million French adults suggests that the weight-loss surgery may offer some protection against these cancers.
The study results present a “clinical paradox,” according to authors of a commentary published this week along with the study in JAMA Surgery. A procedure known to increase the risk of gastroesophageal reflux disease (GERD), and potentially adenocarcinoma of the distal esophagus and gastroesophageal junction, may help shield patients from esophagogastric cancer.
The study marks “an important step toward improving the understanding of potential lifetime risks of bariatric surgery and overall major health benefits of surgically induced weight loss,” commentary authors Piotr Gorecki, MD, and Michael Zenilman, MD, with Weill Cornell Medicine in New York, write.
Recent data indicate that excess body weight is associated with nearly 8% of cancer cases and 6.5% of cancer deaths. Studies also show that bariatric surgery can reduce the risk of some cancers, but whether this extends to esophageal and gastric cancer remains unclear.
To investigate, the researchers used French national data to compare the incidence of esophageal and gastric cancer in 303,709 mostly female patients with obesity who underwent bariatric surgery and a matched group of 605,140 patients with obesity who did not undergo the surgery.
The mean age of the cohort was about 40 years. The mean period of follow-up was 6 years for the surgery group and 5.6 years for the control arm. A total of 337 patients underwent esophagogastric cancer – 83 in the surgical group and 254 in the control group. Gastric cancer was about two times more common than esophageal cancer (225 vs. 112 patients).
The incidence rate of esophagogastric cancer was higher in the control group than in the surgery group – 6.9 vs. 4.9 cases per 100,000 population per year, for an incidence rate ratio of 1.42 (P = .005).
Bariatric surgery was associated with a significant 24% lower risk of esophagogastric cancer (hazard ratio, 0.76; P = .03) and a 40% lower risk of overall in-hospital mortality, defined as “any death occurring during a hospital stay regardless of the cause” (HR, 0.60; P < .001).
The authors also found no significant difference in cancer outcomes and type of bariatric procedure, which included sleeve gastrectomy, gastric bypass, and adjustable gastric banding.
They note that key study limitations include the retrospective design, limited follow-up period, and lack of histologic data on the specific cancers. In addition, the study population was relatively young, whereas esophageal cancer is more common in older people.
But overall, the findings suggest that bariatric surgery can be performed to treat severe obesity without increasing the risk of esophageal and gastric cancer, the authors conclude.
“It seems that the balance between protective factors (weight loss, metabolic effects, and eradication of H. pylori infection) and risk factors (GERD and bile reflux) for cancer after bariatric surgery is in favor of protective factors,” the authors, led by Andrea Lazzati, MD, PhD, of Centre Hospitalier Intercommunal de Créteil, France, explain.
Although the potential protective mechanisms remain unclear, in their commentary, Dr. Gorecki and Dr. Zenilman suggest that a reduction in chronic inflammation and immunosuppression following bariatric surgery could help explain the results.
Although the study provides “reassurance of the protective clinical benefits of weight loss surgery,” more large-scale studies are needed to “better identify, elucidate, and address the pathophysiological processes of bariatric procedure,” Dr. Gorecki and Dr. Zenilman conclude.
No specific funding for the study was reported. Dr. Lazzati has received personal fees from Johnson & Johnson, Medtronic, and Gore. Dr. Zenilman has received personal fees from Academic Medical Professionals Insurance and Mohamed & Obaid Almulla Group.
A version of this article first appeared on Medscape.com.
FROM JAMA SURGERY
Two novel JAK inhibitors show promise in ulcerative colitis
of the two investigational agents.
The study by William J. Sandborn, MD, division of gastroenterology, University of California, San Diego, and colleagues was published online in Clinical Gastroenterology and Hepatology.
Ritlecitinib is a dual inhibitor that selectively inhibits Janus kinase 3 (JAK3) and the TEC family of tyrosine kinases, while brepocitinib is a dual tyrosine kinase 2 (TYK2) and JAK1 inhibitor.
Both agents have demonstrated efficacy and acceptable safety in the treatment of alopecia areata and rheumatoid arthritis and are being evaluated for treating vitiligo, Crohn’s disease, and UC.
The different JAK selectivity profiles of ritlecitinib (JAK3/TEC) and brepocitinib (TYK2/JAK1), compared with other JAK inhibitors, could further the understanding of the role these pathways play in UC, the investigators note.
The VIBRATO study
As part of the phase 2b VIBRATO study, 317 patients with moderate to severe active UC (total Mayo Score ≥ 6) were randomly assigned to an 8-week induction course of once-daily oral ritlecitinib (20, 70, or 200 mg), brepocitinib (10, 30, or 60 mg), or matching placebo.
At week 8, compared with placebo, treatment with ritlecitinib or brepocitinib was associated with significantly lower mean total Mayo Scores (the primary endpoint) and higher rates of clinical remission, endoscopic and histologic improvement, and mucosal healing.
For both drugs, improvement on most metrics was dose dependent, with greater benefit at the highest dose.
For example, the placebo-adjusted mean total Mayo Score at week 8 was −4.6 for ritlecitinib 200 mg (P < .001) and −3.2 for brepocitinib 60 mg (P < .001). Both agents showed a “rapid” onset of action, with significant effects on the partial Mayo Score seen after just 2 weeks of treatment, the authors report.
Modified clinical remission at week 8 (a key secondary endpoint) was achieved in 36% of patients taking ritlecitinib 200 mg and 25.5% of those taking brepocitinib 60 mg (vs. 0% for patients taking placebo).
Endoscopic and histologic improvement, clinical response, mucosal healing, and the patient-reported outcome on the Inflammatory Bowel Disease Questionnaire followed a similar pattern, with a dose-dependent increase in treatment effect observed in most parameters at week 8, compared with placebo.
Longer-term data needed
Both agents were well tolerated with “acceptable short-term safety profiles,” the authors say.
There were no clinically significant findings for any laboratory parameters evaluated. Adverse events were mostly mild.
Infections were observed in 8.7% of patients taking ritlecitinib and 16.9% of those taking brepocitinib, compared with 4% of patients taking placebo. No serious cases of herpes zoster occurred.
One patient taking ritlecitinib suffered myocardial infarction and died, and one patient taking brepocitinib had peripheral artery thrombosis (left tibial artery). Both cases were considered unrelated to the study drug.
“As JAK inhibitors are associated with increased risk of major cardiovascular events and venous thromboembolisms, larger studies are needed for ritlecitinib and brepocitinib to fully understand their safety profiles,” the investigators say.
Limitations of the study include the small sample size and short 8-week treatment period. Longer-term safety and efficacy of both agents are being investigated.
The study was sponsored by Pfizer, which is developing both drugs. Dr. Sandborn and several coauthors have disclosed financial relationships with the company.
A version of this article first appeared on Medscape.com.
of the two investigational agents.
The study by William J. Sandborn, MD, division of gastroenterology, University of California, San Diego, and colleagues was published online in Clinical Gastroenterology and Hepatology.
Ritlecitinib is a dual inhibitor that selectively inhibits Janus kinase 3 (JAK3) and the TEC family of tyrosine kinases, while brepocitinib is a dual tyrosine kinase 2 (TYK2) and JAK1 inhibitor.
Both agents have demonstrated efficacy and acceptable safety in the treatment of alopecia areata and rheumatoid arthritis and are being evaluated for treating vitiligo, Crohn’s disease, and UC.
The different JAK selectivity profiles of ritlecitinib (JAK3/TEC) and brepocitinib (TYK2/JAK1), compared with other JAK inhibitors, could further the understanding of the role these pathways play in UC, the investigators note.
The VIBRATO study
As part of the phase 2b VIBRATO study, 317 patients with moderate to severe active UC (total Mayo Score ≥ 6) were randomly assigned to an 8-week induction course of once-daily oral ritlecitinib (20, 70, or 200 mg), brepocitinib (10, 30, or 60 mg), or matching placebo.
At week 8, compared with placebo, treatment with ritlecitinib or brepocitinib was associated with significantly lower mean total Mayo Scores (the primary endpoint) and higher rates of clinical remission, endoscopic and histologic improvement, and mucosal healing.
For both drugs, improvement on most metrics was dose dependent, with greater benefit at the highest dose.
For example, the placebo-adjusted mean total Mayo Score at week 8 was −4.6 for ritlecitinib 200 mg (P < .001) and −3.2 for brepocitinib 60 mg (P < .001). Both agents showed a “rapid” onset of action, with significant effects on the partial Mayo Score seen after just 2 weeks of treatment, the authors report.
Modified clinical remission at week 8 (a key secondary endpoint) was achieved in 36% of patients taking ritlecitinib 200 mg and 25.5% of those taking brepocitinib 60 mg (vs. 0% for patients taking placebo).
Endoscopic and histologic improvement, clinical response, mucosal healing, and the patient-reported outcome on the Inflammatory Bowel Disease Questionnaire followed a similar pattern, with a dose-dependent increase in treatment effect observed in most parameters at week 8, compared with placebo.
Longer-term data needed
Both agents were well tolerated with “acceptable short-term safety profiles,” the authors say.
There were no clinically significant findings for any laboratory parameters evaluated. Adverse events were mostly mild.
Infections were observed in 8.7% of patients taking ritlecitinib and 16.9% of those taking brepocitinib, compared with 4% of patients taking placebo. No serious cases of herpes zoster occurred.
One patient taking ritlecitinib suffered myocardial infarction and died, and one patient taking brepocitinib had peripheral artery thrombosis (left tibial artery). Both cases were considered unrelated to the study drug.
“As JAK inhibitors are associated with increased risk of major cardiovascular events and venous thromboembolisms, larger studies are needed for ritlecitinib and brepocitinib to fully understand their safety profiles,” the investigators say.
Limitations of the study include the small sample size and short 8-week treatment period. Longer-term safety and efficacy of both agents are being investigated.
The study was sponsored by Pfizer, which is developing both drugs. Dr. Sandborn and several coauthors have disclosed financial relationships with the company.
A version of this article first appeared on Medscape.com.
of the two investigational agents.
The study by William J. Sandborn, MD, division of gastroenterology, University of California, San Diego, and colleagues was published online in Clinical Gastroenterology and Hepatology.
Ritlecitinib is a dual inhibitor that selectively inhibits Janus kinase 3 (JAK3) and the TEC family of tyrosine kinases, while brepocitinib is a dual tyrosine kinase 2 (TYK2) and JAK1 inhibitor.
Both agents have demonstrated efficacy and acceptable safety in the treatment of alopecia areata and rheumatoid arthritis and are being evaluated for treating vitiligo, Crohn’s disease, and UC.
The different JAK selectivity profiles of ritlecitinib (JAK3/TEC) and brepocitinib (TYK2/JAK1), compared with other JAK inhibitors, could further the understanding of the role these pathways play in UC, the investigators note.
The VIBRATO study
As part of the phase 2b VIBRATO study, 317 patients with moderate to severe active UC (total Mayo Score ≥ 6) were randomly assigned to an 8-week induction course of once-daily oral ritlecitinib (20, 70, or 200 mg), brepocitinib (10, 30, or 60 mg), or matching placebo.
At week 8, compared with placebo, treatment with ritlecitinib or brepocitinib was associated with significantly lower mean total Mayo Scores (the primary endpoint) and higher rates of clinical remission, endoscopic and histologic improvement, and mucosal healing.
For both drugs, improvement on most metrics was dose dependent, with greater benefit at the highest dose.
For example, the placebo-adjusted mean total Mayo Score at week 8 was −4.6 for ritlecitinib 200 mg (P < .001) and −3.2 for brepocitinib 60 mg (P < .001). Both agents showed a “rapid” onset of action, with significant effects on the partial Mayo Score seen after just 2 weeks of treatment, the authors report.
Modified clinical remission at week 8 (a key secondary endpoint) was achieved in 36% of patients taking ritlecitinib 200 mg and 25.5% of those taking brepocitinib 60 mg (vs. 0% for patients taking placebo).
Endoscopic and histologic improvement, clinical response, mucosal healing, and the patient-reported outcome on the Inflammatory Bowel Disease Questionnaire followed a similar pattern, with a dose-dependent increase in treatment effect observed in most parameters at week 8, compared with placebo.
Longer-term data needed
Both agents were well tolerated with “acceptable short-term safety profiles,” the authors say.
There were no clinically significant findings for any laboratory parameters evaluated. Adverse events were mostly mild.
Infections were observed in 8.7% of patients taking ritlecitinib and 16.9% of those taking brepocitinib, compared with 4% of patients taking placebo. No serious cases of herpes zoster occurred.
One patient taking ritlecitinib suffered myocardial infarction and died, and one patient taking brepocitinib had peripheral artery thrombosis (left tibial artery). Both cases were considered unrelated to the study drug.
“As JAK inhibitors are associated with increased risk of major cardiovascular events and venous thromboembolisms, larger studies are needed for ritlecitinib and brepocitinib to fully understand their safety profiles,” the investigators say.
Limitations of the study include the small sample size and short 8-week treatment period. Longer-term safety and efficacy of both agents are being investigated.
The study was sponsored by Pfizer, which is developing both drugs. Dr. Sandborn and several coauthors have disclosed financial relationships with the company.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY