Article
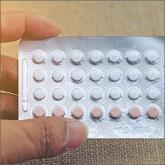
Can unintended pregnancies be reduced by dispensing a year’s worth of hormonal contraception?
- Author:
- Nellie Wirsing, MD
- Carrie Pierce, MD
- Joan Nashelsky, MLS
EVIDENCE-BASED ANSWER: Probably, although studies that looked directly at this outcome are limited. A systematic review showed that women who...
Article
How often should you follow up on a patient with newly diagnosed hypothyroidism?
- Author:
- Nellie Wirsing, MD
- Andrew Hamilton, MLS
EVIDENCE-BASED ANSWER: Six to 8 weeks after the start of levothyroxine therapy you should reexamine patients and measure their serum thyroid-...
