User login
Auditory musical hallucinations: When a patient complains, ‘I hear a symphony!’
Nonpsychotic auditory musical hallucinations—hearing singing voices, musical tones, song lyrics, or instrumental music—occur in >20% of outpatients who have a diagnosis of an anxiety, affective, or schizophrenic disorder, with the highest prevalence (41%) in patients with obsessive-compulsive disorder (OCD).1 OCD comorbidity with other psychiatric disorders increases the frequency of auditory musical hallucinations. Auditory musical hallucinations mainly affect older (mean age, 61.5 years) females who have tinnitus and severe, high-frequency, sensorineural hearing loss.1 Auditory musical hallucinations occur in psychiatric diseases, ictal states of complex partial seizures, abnormalities of the auditory cortex, thalamic infarcts, subarachnoid hemorrhage, tumors of the brain stem, intoxication, and progressive deafness.1,2
What patients report hearing
Some patients identify 1 musical instrument that dominates others. The musical tones are reported to have a vibrating quality, similar to the sound produced by blowing air through a paper-covered comb. Some patients hear singing voices, predominantly deep in tone, although the words usually are not clear.
Patients with auditory musical hallucinations associated with deafness may not have dementia or psychosis. Both sensorineural and conductive involvement indicates a mixed type of deafness. Pure tone audiograms show a bilateral loss of >30 decibels, affecting the higher and lower ranges.2,3 Cerebral atrophy and microangiopathic changes are common co-occurring findings on MRI.
Treatment options
Reassure your patient that the experience is not necessarily associated with a psychotic disorder. Perform a complete history, physical, and neurologic examination. Rule out unilateral symptoms, tinnitus, and hearing loss. If she (he) is experiencing unilateral symptoms, pulsatile tinnitus, unilateral hearing loss, and a constant feeling of unsteadiness, further evaluation is necessary to exclude underlying pathology. Treating concurrent insomnia, depression, or anxiety might resolve the hallucinations.4
Nonpharmacotherapeutic treatments include hearing amplification, and masking tinnitus with a hearing aid emitting low-volume music or sounds of nature (ie, rainfall).4 Two cases have reported successful carbamazepine therapy; 2 other cases demonstrated success with clomipramine.5 Frequently, symptoms spontaneously remit.
Consider electroconvulsive therapy (ECT) for patients with musical hallucinations that are refractory to medical treatment and cause distress; 3 patients with concurrent major depressive disorder showed improvement after ECT.6 Antipsychotics are not recommended as first-line treatment.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hermesh H, Konas S, Shiloh R, et al. Musical hallucinations: prevalence in psychotic and nonpsychotic outpatients. J Clin Psychiatry. 2004;65(2):191-197.
2. Schakenraad SM, Teunisse RJ, Olde Rikkert MG. Musical hallucinations in psychiatric patients. Int J Geriatr Psychiatry. 2006;21(4):394-397.
3. Evers S, Ellger T. The clinical spectrum of musical hallucinations. J Neurol Sci. 2004;227(1):55-65.
4. Zegarra NM, Cuetter AC, Briones DF, et al. Nonpsychotic auditory musical hallucinations in elderly persons with progressive deafness. Clin Geriatr. 2007;15(11):33-37.
5. Mahendran R. The psychopathology of musical hallucinations. Singapore Med J. 2007;48(2):e68-e70.
6. Wengel SP, Burke WJ, Holemon D. Musical hallucinations. The sounds of silence? J Am Geriatr Soc. 1989;37(2):163-166.
Nonpsychotic auditory musical hallucinations—hearing singing voices, musical tones, song lyrics, or instrumental music—occur in >20% of outpatients who have a diagnosis of an anxiety, affective, or schizophrenic disorder, with the highest prevalence (41%) in patients with obsessive-compulsive disorder (OCD).1 OCD comorbidity with other psychiatric disorders increases the frequency of auditory musical hallucinations. Auditory musical hallucinations mainly affect older (mean age, 61.5 years) females who have tinnitus and severe, high-frequency, sensorineural hearing loss.1 Auditory musical hallucinations occur in psychiatric diseases, ictal states of complex partial seizures, abnormalities of the auditory cortex, thalamic infarcts, subarachnoid hemorrhage, tumors of the brain stem, intoxication, and progressive deafness.1,2
What patients report hearing
Some patients identify 1 musical instrument that dominates others. The musical tones are reported to have a vibrating quality, similar to the sound produced by blowing air through a paper-covered comb. Some patients hear singing voices, predominantly deep in tone, although the words usually are not clear.
Patients with auditory musical hallucinations associated with deafness may not have dementia or psychosis. Both sensorineural and conductive involvement indicates a mixed type of deafness. Pure tone audiograms show a bilateral loss of >30 decibels, affecting the higher and lower ranges.2,3 Cerebral atrophy and microangiopathic changes are common co-occurring findings on MRI.
Treatment options
Reassure your patient that the experience is not necessarily associated with a psychotic disorder. Perform a complete history, physical, and neurologic examination. Rule out unilateral symptoms, tinnitus, and hearing loss. If she (he) is experiencing unilateral symptoms, pulsatile tinnitus, unilateral hearing loss, and a constant feeling of unsteadiness, further evaluation is necessary to exclude underlying pathology. Treating concurrent insomnia, depression, or anxiety might resolve the hallucinations.4
Nonpharmacotherapeutic treatments include hearing amplification, and masking tinnitus with a hearing aid emitting low-volume music or sounds of nature (ie, rainfall).4 Two cases have reported successful carbamazepine therapy; 2 other cases demonstrated success with clomipramine.5 Frequently, symptoms spontaneously remit.
Consider electroconvulsive therapy (ECT) for patients with musical hallucinations that are refractory to medical treatment and cause distress; 3 patients with concurrent major depressive disorder showed improvement after ECT.6 Antipsychotics are not recommended as first-line treatment.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Nonpsychotic auditory musical hallucinations—hearing singing voices, musical tones, song lyrics, or instrumental music—occur in >20% of outpatients who have a diagnosis of an anxiety, affective, or schizophrenic disorder, with the highest prevalence (41%) in patients with obsessive-compulsive disorder (OCD).1 OCD comorbidity with other psychiatric disorders increases the frequency of auditory musical hallucinations. Auditory musical hallucinations mainly affect older (mean age, 61.5 years) females who have tinnitus and severe, high-frequency, sensorineural hearing loss.1 Auditory musical hallucinations occur in psychiatric diseases, ictal states of complex partial seizures, abnormalities of the auditory cortex, thalamic infarcts, subarachnoid hemorrhage, tumors of the brain stem, intoxication, and progressive deafness.1,2
What patients report hearing
Some patients identify 1 musical instrument that dominates others. The musical tones are reported to have a vibrating quality, similar to the sound produced by blowing air through a paper-covered comb. Some patients hear singing voices, predominantly deep in tone, although the words usually are not clear.
Patients with auditory musical hallucinations associated with deafness may not have dementia or psychosis. Both sensorineural and conductive involvement indicates a mixed type of deafness. Pure tone audiograms show a bilateral loss of >30 decibels, affecting the higher and lower ranges.2,3 Cerebral atrophy and microangiopathic changes are common co-occurring findings on MRI.
Treatment options
Reassure your patient that the experience is not necessarily associated with a psychotic disorder. Perform a complete history, physical, and neurologic examination. Rule out unilateral symptoms, tinnitus, and hearing loss. If she (he) is experiencing unilateral symptoms, pulsatile tinnitus, unilateral hearing loss, and a constant feeling of unsteadiness, further evaluation is necessary to exclude underlying pathology. Treating concurrent insomnia, depression, or anxiety might resolve the hallucinations.4
Nonpharmacotherapeutic treatments include hearing amplification, and masking tinnitus with a hearing aid emitting low-volume music or sounds of nature (ie, rainfall).4 Two cases have reported successful carbamazepine therapy; 2 other cases demonstrated success with clomipramine.5 Frequently, symptoms spontaneously remit.
Consider electroconvulsive therapy (ECT) for patients with musical hallucinations that are refractory to medical treatment and cause distress; 3 patients with concurrent major depressive disorder showed improvement after ECT.6 Antipsychotics are not recommended as first-line treatment.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hermesh H, Konas S, Shiloh R, et al. Musical hallucinations: prevalence in psychotic and nonpsychotic outpatients. J Clin Psychiatry. 2004;65(2):191-197.
2. Schakenraad SM, Teunisse RJ, Olde Rikkert MG. Musical hallucinations in psychiatric patients. Int J Geriatr Psychiatry. 2006;21(4):394-397.
3. Evers S, Ellger T. The clinical spectrum of musical hallucinations. J Neurol Sci. 2004;227(1):55-65.
4. Zegarra NM, Cuetter AC, Briones DF, et al. Nonpsychotic auditory musical hallucinations in elderly persons with progressive deafness. Clin Geriatr. 2007;15(11):33-37.
5. Mahendran R. The psychopathology of musical hallucinations. Singapore Med J. 2007;48(2):e68-e70.
6. Wengel SP, Burke WJ, Holemon D. Musical hallucinations. The sounds of silence? J Am Geriatr Soc. 1989;37(2):163-166.
1. Hermesh H, Konas S, Shiloh R, et al. Musical hallucinations: prevalence in psychotic and nonpsychotic outpatients. J Clin Psychiatry. 2004;65(2):191-197.
2. Schakenraad SM, Teunisse RJ, Olde Rikkert MG. Musical hallucinations in psychiatric patients. Int J Geriatr Psychiatry. 2006;21(4):394-397.
3. Evers S, Ellger T. The clinical spectrum of musical hallucinations. J Neurol Sci. 2004;227(1):55-65.
4. Zegarra NM, Cuetter AC, Briones DF, et al. Nonpsychotic auditory musical hallucinations in elderly persons with progressive deafness. Clin Geriatr. 2007;15(11):33-37.
5. Mahendran R. The psychopathology of musical hallucinations. Singapore Med J. 2007;48(2):e68-e70.
6. Wengel SP, Burke WJ, Holemon D. Musical hallucinations. The sounds of silence? J Am Geriatr Soc. 1989;37(2):163-166.
Problematic pruritus: Seeking a cure for psychogenic itch
Psychogenic itch—an excessive impulse to scratch, gouge, or pick at skin in the absence of dermatologic cause—is common among psychiatric inpatients, but can be challenging to assess and manage in outpatients. Patients with psychogenic itch predominantly are female, with average age of onset between 30 and 45 years.1 Psychiatric disorders associated with psychogenic itch include depression, obsessive-compulsive disorder, anxiety, somatoform disorders, mania, psychosis, and substance abuse.2 Body dysmorphic disorder, trichotillomania, kleptomania, and borderline personality disorder may be comorbid in patients with psychogenic itch.3
Characteristics of psychogenic itch
Consider psychogenic itch in patients who have recurring physical symptoms and demand examination despite repeated negative results. Other indicators include psychological factors—loss of a loved one, unemployment, relocation, etc.—that may be associated with onset, severity, elicitation, or maintenance of the itching; impairments in the patient’s social or professional life; and marked preoccupation with itching or the state of her (his) skin. Characteristically, itching can be provoked by emotional triggers, most notably during stages of excitement, and also by mechanical or chemical stimuli.
Skin changes associated with psychogenic itch often are found on areas accessible to the patient’s hand: face, arms, legs, abdomen, thighs, upper back, and shoulders. These changes can be seen in varying stages, from discrete superficial excoriations, erosions, and ulcers to thick, darkened nodules and colorless atrophic scars. Patients often complain of burning. In some cases, a patient uses a tool or instrument to autoaggressively manipulate his (her) skin in response to tingling or stabbing sensations. Artificial lesions or eczemas brought on by self-
manipulation can occur. Stress, life changes, or inhibited rage may be evoking the burning sensation and subsequent complaints.
Interventions to consider
After you have ruled out other causes of pruritus and made a diagnosis of psychogenic itch, educate your patient about the multifactorial etiology. Explain possible associations between skin disorders and unconscious reaction patterns, and the role of emotional and cognitive stimuli.
Moisturizing the skin can help the dryness associated with repetitive scratching. Consider prescribing an antihistamine, moisturizer, topical steroid, antibiotic, or
occlusive dressing.
Some pharmacological properties of antidepressants that are not related to their antidepressant activity—eg, the histamine-1 blocking effect of tricyclic antidepressants—are beneficial for treating psychogenic itch.4 Sedating antihistamines (hydroxyzine) and antidepressants (doxepin) may help break cycles of itching and depression or itching and scratching.4 Tricyclic antidepressants also are recommended for treating burning, stabbing, or tingling sensations.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32-41.
2. Krishnan A, Koo J. Psyche, opioids, and itch: therapeutic consequences. Dermatol Ther. 2005;18(4):314-322.
3. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
4. Gupta MA, Guptat AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol Venereol. 2001;15(6):512-518.
Psychogenic itch—an excessive impulse to scratch, gouge, or pick at skin in the absence of dermatologic cause—is common among psychiatric inpatients, but can be challenging to assess and manage in outpatients. Patients with psychogenic itch predominantly are female, with average age of onset between 30 and 45 years.1 Psychiatric disorders associated with psychogenic itch include depression, obsessive-compulsive disorder, anxiety, somatoform disorders, mania, psychosis, and substance abuse.2 Body dysmorphic disorder, trichotillomania, kleptomania, and borderline personality disorder may be comorbid in patients with psychogenic itch.3
Characteristics of psychogenic itch
Consider psychogenic itch in patients who have recurring physical symptoms and demand examination despite repeated negative results. Other indicators include psychological factors—loss of a loved one, unemployment, relocation, etc.—that may be associated with onset, severity, elicitation, or maintenance of the itching; impairments in the patient’s social or professional life; and marked preoccupation with itching or the state of her (his) skin. Characteristically, itching can be provoked by emotional triggers, most notably during stages of excitement, and also by mechanical or chemical stimuli.
Skin changes associated with psychogenic itch often are found on areas accessible to the patient’s hand: face, arms, legs, abdomen, thighs, upper back, and shoulders. These changes can be seen in varying stages, from discrete superficial excoriations, erosions, and ulcers to thick, darkened nodules and colorless atrophic scars. Patients often complain of burning. In some cases, a patient uses a tool or instrument to autoaggressively manipulate his (her) skin in response to tingling or stabbing sensations. Artificial lesions or eczemas brought on by self-
manipulation can occur. Stress, life changes, or inhibited rage may be evoking the burning sensation and subsequent complaints.
Interventions to consider
After you have ruled out other causes of pruritus and made a diagnosis of psychogenic itch, educate your patient about the multifactorial etiology. Explain possible associations between skin disorders and unconscious reaction patterns, and the role of emotional and cognitive stimuli.
Moisturizing the skin can help the dryness associated with repetitive scratching. Consider prescribing an antihistamine, moisturizer, topical steroid, antibiotic, or
occlusive dressing.
Some pharmacological properties of antidepressants that are not related to their antidepressant activity—eg, the histamine-1 blocking effect of tricyclic antidepressants—are beneficial for treating psychogenic itch.4 Sedating antihistamines (hydroxyzine) and antidepressants (doxepin) may help break cycles of itching and depression or itching and scratching.4 Tricyclic antidepressants also are recommended for treating burning, stabbing, or tingling sensations.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Psychogenic itch—an excessive impulse to scratch, gouge, or pick at skin in the absence of dermatologic cause—is common among psychiatric inpatients, but can be challenging to assess and manage in outpatients. Patients with psychogenic itch predominantly are female, with average age of onset between 30 and 45 years.1 Psychiatric disorders associated with psychogenic itch include depression, obsessive-compulsive disorder, anxiety, somatoform disorders, mania, psychosis, and substance abuse.2 Body dysmorphic disorder, trichotillomania, kleptomania, and borderline personality disorder may be comorbid in patients with psychogenic itch.3
Characteristics of psychogenic itch
Consider psychogenic itch in patients who have recurring physical symptoms and demand examination despite repeated negative results. Other indicators include psychological factors—loss of a loved one, unemployment, relocation, etc.—that may be associated with onset, severity, elicitation, or maintenance of the itching; impairments in the patient’s social or professional life; and marked preoccupation with itching or the state of her (his) skin. Characteristically, itching can be provoked by emotional triggers, most notably during stages of excitement, and also by mechanical or chemical stimuli.
Skin changes associated with psychogenic itch often are found on areas accessible to the patient’s hand: face, arms, legs, abdomen, thighs, upper back, and shoulders. These changes can be seen in varying stages, from discrete superficial excoriations, erosions, and ulcers to thick, darkened nodules and colorless atrophic scars. Patients often complain of burning. In some cases, a patient uses a tool or instrument to autoaggressively manipulate his (her) skin in response to tingling or stabbing sensations. Artificial lesions or eczemas brought on by self-
manipulation can occur. Stress, life changes, or inhibited rage may be evoking the burning sensation and subsequent complaints.
Interventions to consider
After you have ruled out other causes of pruritus and made a diagnosis of psychogenic itch, educate your patient about the multifactorial etiology. Explain possible associations between skin disorders and unconscious reaction patterns, and the role of emotional and cognitive stimuli.
Moisturizing the skin can help the dryness associated with repetitive scratching. Consider prescribing an antihistamine, moisturizer, topical steroid, antibiotic, or
occlusive dressing.
Some pharmacological properties of antidepressants that are not related to their antidepressant activity—eg, the histamine-1 blocking effect of tricyclic antidepressants—are beneficial for treating psychogenic itch.4 Sedating antihistamines (hydroxyzine) and antidepressants (doxepin) may help break cycles of itching and depression or itching and scratching.4 Tricyclic antidepressants also are recommended for treating burning, stabbing, or tingling sensations.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32-41.
2. Krishnan A, Koo J. Psyche, opioids, and itch: therapeutic consequences. Dermatol Ther. 2005;18(4):314-322.
3. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
4. Gupta MA, Guptat AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol Venereol. 2001;15(6):512-518.
1. Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32-41.
2. Krishnan A, Koo J. Psyche, opioids, and itch: therapeutic consequences. Dermatol Ther. 2005;18(4):314-322.
3. Arnold LM, Auchenbach MB, McElroy SL. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs. 2001;15(5):351-359.
4. Gupta MA, Guptat AK. The use of antidepressant drugs in dermatology. J Eur Acad Dermatol Venereol. 2001;15(6):512-518.
Adoption by mentally ill individuals: What to recommend
Ms. T, age 28, wishes to adopt a child. She has a history of bipolar disorder, but has been stable for several years. She asks her psychiatrist if her diagnosis will disqualify her as a potential parent. She also wants to know how the psychiatrist can help with the adoption process because he has been treating her long-term and is familiar with her psychiatric history.
Many adults with a history of psychiatric illness prefer to adopt rather than have biological children. Their preference may be fueled by concerns regarding psychiatric destabilization during pregnancy or fear of psychotropic-induced fetal teratogenicity. Child adoption laws vary from state to state. Although some licensed adoption agencies sympathize with potential adoptive parents with a history of mental illness, the law usually considers the following factors:
• the potential adopter’s emotional ties to the child
• their parenting skills
• emotional needs of the child
• the potential adopter’s desire to maintain continuity of the child’s care
• permanence of the family unit of the proposed home
• the physical, moral, and mental fitness of the potential parent.
The psychiatrist’s role
So long as the adoptee’s well-being is the reason for adoption, and the adoption is in the “best interest of the child,”1 a history of mental illness does not necessarily exclude an individual from adopting a child. The psychiatrist needs to consider the potential adopter’s motives, intellectual capacity, and judgment with regards to caregiving. The psychiatrist needs to assess the degree to which the patient’s mental disorder may or may not interfere with their parenting. The clinician also needs to consider potential changes that may occur in the adopter’s personal life, work hours, recreational and social activities, and sleep patterns.
It also is important to estimate the changes that an adoption may cause in the potential adopter’s living arrangements, daily schedule, and life events such as family vacations. Based on knowledge of the patient’s psychiatric history, a clinician may need to consider whether adoption-related stress could destabilize or exacerbate the potential parent’s psychiatric condition.2 Other psychosocial factors of importance are the reliability of the adopter’s support system, their history of previous child-rearing success, care-taking arrangements, etc.1
What to consider
The potential adoptee’s unique needs also should be considered. Is the child physically handicapped or mentally challenged, and is your patient capable of handling these issues? Would there be a good temperament fit between the potential adoptive parent and child?
Because child adoption laws vary from state to state, there are no established criteria for determining the eligibility of an individual with a history of mental illness. The success of a child adoption by an individual with a history of mental illness will depend on state laws and the policy of the adoption agency. Some U.S. states and territories (Alaska, Arizona, California, Kentucky, North Dakota, and Puerto Rico) regard parental mental illness as “aggravated circumstances.”1
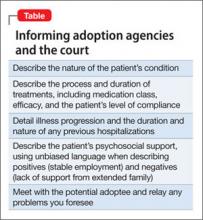
Although psychiatrists are not expected to be able to accurately predict the future, courts and adoption agencies may request a psychiatrist’s professional opinion on a specific adoption. See the Table for a list of suggested information to share when approached by an adoption agency or court.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Bacani-Oropilla T, Lippmann SB, Turns DM. Should the mentally ill adopt children? How physicians can influence the decision. Postgrad Med. 1988;84(6):201-205.
2. Linn L. Clinical manifestations of psychiatric disorder: the Homes-Rahe scale of stress of adjusting to change. In: Fredman A, Kaplan H, Sadock B, eds. Modern synopsis of comprehensive textbook of psychiatry, II. 2nd ed. Baltimore, MD: Williams & Wilkins; 1976:785.
Ms. T, age 28, wishes to adopt a child. She has a history of bipolar disorder, but has been stable for several years. She asks her psychiatrist if her diagnosis will disqualify her as a potential parent. She also wants to know how the psychiatrist can help with the adoption process because he has been treating her long-term and is familiar with her psychiatric history.
Many adults with a history of psychiatric illness prefer to adopt rather than have biological children. Their preference may be fueled by concerns regarding psychiatric destabilization during pregnancy or fear of psychotropic-induced fetal teratogenicity. Child adoption laws vary from state to state. Although some licensed adoption agencies sympathize with potential adoptive parents with a history of mental illness, the law usually considers the following factors:
• the potential adopter’s emotional ties to the child
• their parenting skills
• emotional needs of the child
• the potential adopter’s desire to maintain continuity of the child’s care
• permanence of the family unit of the proposed home
• the physical, moral, and mental fitness of the potential parent.
The psychiatrist’s role
So long as the adoptee’s well-being is the reason for adoption, and the adoption is in the “best interest of the child,”1 a history of mental illness does not necessarily exclude an individual from adopting a child. The psychiatrist needs to consider the potential adopter’s motives, intellectual capacity, and judgment with regards to caregiving. The psychiatrist needs to assess the degree to which the patient’s mental disorder may or may not interfere with their parenting. The clinician also needs to consider potential changes that may occur in the adopter’s personal life, work hours, recreational and social activities, and sleep patterns.
It also is important to estimate the changes that an adoption may cause in the potential adopter’s living arrangements, daily schedule, and life events such as family vacations. Based on knowledge of the patient’s psychiatric history, a clinician may need to consider whether adoption-related stress could destabilize or exacerbate the potential parent’s psychiatric condition.2 Other psychosocial factors of importance are the reliability of the adopter’s support system, their history of previous child-rearing success, care-taking arrangements, etc.1
What to consider
The potential adoptee’s unique needs also should be considered. Is the child physically handicapped or mentally challenged, and is your patient capable of handling these issues? Would there be a good temperament fit between the potential adoptive parent and child?
Because child adoption laws vary from state to state, there are no established criteria for determining the eligibility of an individual with a history of mental illness. The success of a child adoption by an individual with a history of mental illness will depend on state laws and the policy of the adoption agency. Some U.S. states and territories (Alaska, Arizona, California, Kentucky, North Dakota, and Puerto Rico) regard parental mental illness as “aggravated circumstances.”1
Although psychiatrists are not expected to be able to accurately predict the future, courts and adoption agencies may request a psychiatrist’s professional opinion on a specific adoption. See the Table for a list of suggested information to share when approached by an adoption agency or court.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Ms. T, age 28, wishes to adopt a child. She has a history of bipolar disorder, but has been stable for several years. She asks her psychiatrist if her diagnosis will disqualify her as a potential parent. She also wants to know how the psychiatrist can help with the adoption process because he has been treating her long-term and is familiar with her psychiatric history.
Many adults with a history of psychiatric illness prefer to adopt rather than have biological children. Their preference may be fueled by concerns regarding psychiatric destabilization during pregnancy or fear of psychotropic-induced fetal teratogenicity. Child adoption laws vary from state to state. Although some licensed adoption agencies sympathize with potential adoptive parents with a history of mental illness, the law usually considers the following factors:
• the potential adopter’s emotional ties to the child
• their parenting skills
• emotional needs of the child
• the potential adopter’s desire to maintain continuity of the child’s care
• permanence of the family unit of the proposed home
• the physical, moral, and mental fitness of the potential parent.
The psychiatrist’s role
So long as the adoptee’s well-being is the reason for adoption, and the adoption is in the “best interest of the child,”1 a history of mental illness does not necessarily exclude an individual from adopting a child. The psychiatrist needs to consider the potential adopter’s motives, intellectual capacity, and judgment with regards to caregiving. The psychiatrist needs to assess the degree to which the patient’s mental disorder may or may not interfere with their parenting. The clinician also needs to consider potential changes that may occur in the adopter’s personal life, work hours, recreational and social activities, and sleep patterns.
It also is important to estimate the changes that an adoption may cause in the potential adopter’s living arrangements, daily schedule, and life events such as family vacations. Based on knowledge of the patient’s psychiatric history, a clinician may need to consider whether adoption-related stress could destabilize or exacerbate the potential parent’s psychiatric condition.2 Other psychosocial factors of importance are the reliability of the adopter’s support system, their history of previous child-rearing success, care-taking arrangements, etc.1
What to consider
The potential adoptee’s unique needs also should be considered. Is the child physically handicapped or mentally challenged, and is your patient capable of handling these issues? Would there be a good temperament fit between the potential adoptive parent and child?
Because child adoption laws vary from state to state, there are no established criteria for determining the eligibility of an individual with a history of mental illness. The success of a child adoption by an individual with a history of mental illness will depend on state laws and the policy of the adoption agency. Some U.S. states and territories (Alaska, Arizona, California, Kentucky, North Dakota, and Puerto Rico) regard parental mental illness as “aggravated circumstances.”1
Although psychiatrists are not expected to be able to accurately predict the future, courts and adoption agencies may request a psychiatrist’s professional opinion on a specific adoption. See the Table for a list of suggested information to share when approached by an adoption agency or court.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Bacani-Oropilla T, Lippmann SB, Turns DM. Should the mentally ill adopt children? How physicians can influence the decision. Postgrad Med. 1988;84(6):201-205.
2. Linn L. Clinical manifestations of psychiatric disorder: the Homes-Rahe scale of stress of adjusting to change. In: Fredman A, Kaplan H, Sadock B, eds. Modern synopsis of comprehensive textbook of psychiatry, II. 2nd ed. Baltimore, MD: Williams & Wilkins; 1976:785.
1. Bacani-Oropilla T, Lippmann SB, Turns DM. Should the mentally ill adopt children? How physicians can influence the decision. Postgrad Med. 1988;84(6):201-205.
2. Linn L. Clinical manifestations of psychiatric disorder: the Homes-Rahe scale of stress of adjusting to change. In: Fredman A, Kaplan H, Sadock B, eds. Modern synopsis of comprehensive textbook of psychiatry, II. 2nd ed. Baltimore, MD: Williams & Wilkins; 1976:785.
8 tips for talking to parents and children about school shootings
In the aftermath of a school shooting, parents and teachers may seek a psychiatrist’s advice on how to best discuss these incidents with children. We offer guidelines on what to tell concerned parents, educators, and other adults who may interact with children affected by a school shooting.
6 tips for interacting with children
1. Talk about the event. Instruct adults to ask children to share their feelings about the incident and to show genuine interest in listening to the child’s thoughts and point of view. Adults shouldn’t pretend the event hasn’t occurred or isn’t serious. Children may be more worried if they think adults are too afraid to tell them what is happening. It is important to gently correct any misinformation older students may have received via social media.1
2. Reinforce that home is a safe haven. Overwhelming emotions and uncertainty can bring about a sense of insecurity in children. Children may come home seeking a safe environment. Advise parents to plan a night where family members participate in a favorite family activity.1 Tell parents to remind their children that trust-worthy adults—parents, emergency workers, police, firefighters, doctors, and the military—are helping provide safety, comfort, and support.2
3. Limit television time. If children are exposed to the news, parents should watch it with them briefly, but avoid letting children rewatch the same event repetitively. Constant exposure to the event may heighten a child’s anxiety and fears.
4. Maintain a normal routine. Tell parents they should maintain, as best they can, their normal routine for dinner, homework, chores, and bedtime, but to remain flexible.2 Children may have a hard time concentrating on schoolwork or falling asleep. Advise parents to spend extra time reading or playing quiet games with their children, particularly at bedtime. These activities are calming, foster a sense of closeness and security, and reinforce a feeling of normalcy.
5. Encourage emotions. Instruct parents to explain to their children that all feelings are okay and normal, and to let children talk about their feelings and help put them into perspective.1 Children may need help in expressing these feelings, so be patient. If an incident happened at the child’s school, teachers and administrators may conduct group sessions to help children express their concerns about being back in school.
6. Seek creativity or spirituality. Encourage parents and other adults to provide a creative outlet for children, such as making get well cards or sending letters to the survivors and their families. Writing thank you letters to doctors, nurses, fire-fighters, and police officers also may be comforting.1,2 Suggest that parents encourage their children to pray or think hopeful thoughts for the victims and their families.
2 tips for interacting with adults
7. Recommend they take care of themselves. Explain to adult caregivers that because children learn by observing, they shouldn’t ignore their own feelings of anxiety, grief, and anger. By expressing their emotions in a productive manner, adults will be better able to support their children. Encourage adults to talk to friends, family, religious leaders, or mental health counselors.
8. Advise adults to be alert for children who may need professional help. Tell them to be vigilant when monitoring a child’s emotional state. Children who may benefit from mental health counseling after a tragedy may exhibit warning signs, such as changes in behavior, appetite, and sleep patterns, which may indicate the child is experiencing grief, anxiety, or discomfort.
Remind adults to be aware of children who are at greater risk for mental health issues, including those who are already struggling with other recent traumatic experiences—past traumatic experiences, personal loss, depression, or other mental illness.1 Be particularly observant for children who may be at risk of suicide.1,2 Professional counseling may be needed for a child who is experiencing an emotional reaction that lasts >1 month and is impacting his or her daily functioning.1
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American Psychological Association. Helping your children manage distress in the aftermath of a shooting. http://www.apa.org/helpcenter/aftermath.aspx. Updated April 2011. Accessed February 15, 2013.
2. National Association of School Psychologists resources. A national tragedy: helping children cope. http://www.nasponline.org/resources/crisis_safety/terror_general.aspx. Published September 2001. Accessed February 15, 2013.
In the aftermath of a school shooting, parents and teachers may seek a psychiatrist’s advice on how to best discuss these incidents with children. We offer guidelines on what to tell concerned parents, educators, and other adults who may interact with children affected by a school shooting.
6 tips for interacting with children
1. Talk about the event. Instruct adults to ask children to share their feelings about the incident and to show genuine interest in listening to the child’s thoughts and point of view. Adults shouldn’t pretend the event hasn’t occurred or isn’t serious. Children may be more worried if they think adults are too afraid to tell them what is happening. It is important to gently correct any misinformation older students may have received via social media.1
2. Reinforce that home is a safe haven. Overwhelming emotions and uncertainty can bring about a sense of insecurity in children. Children may come home seeking a safe environment. Advise parents to plan a night where family members participate in a favorite family activity.1 Tell parents to remind their children that trust-worthy adults—parents, emergency workers, police, firefighters, doctors, and the military—are helping provide safety, comfort, and support.2
3. Limit television time. If children are exposed to the news, parents should watch it with them briefly, but avoid letting children rewatch the same event repetitively. Constant exposure to the event may heighten a child’s anxiety and fears.
4. Maintain a normal routine. Tell parents they should maintain, as best they can, their normal routine for dinner, homework, chores, and bedtime, but to remain flexible.2 Children may have a hard time concentrating on schoolwork or falling asleep. Advise parents to spend extra time reading or playing quiet games with their children, particularly at bedtime. These activities are calming, foster a sense of closeness and security, and reinforce a feeling of normalcy.
5. Encourage emotions. Instruct parents to explain to their children that all feelings are okay and normal, and to let children talk about their feelings and help put them into perspective.1 Children may need help in expressing these feelings, so be patient. If an incident happened at the child’s school, teachers and administrators may conduct group sessions to help children express their concerns about being back in school.
6. Seek creativity or spirituality. Encourage parents and other adults to provide a creative outlet for children, such as making get well cards or sending letters to the survivors and their families. Writing thank you letters to doctors, nurses, fire-fighters, and police officers also may be comforting.1,2 Suggest that parents encourage their children to pray or think hopeful thoughts for the victims and their families.
2 tips for interacting with adults
7. Recommend they take care of themselves. Explain to adult caregivers that because children learn by observing, they shouldn’t ignore their own feelings of anxiety, grief, and anger. By expressing their emotions in a productive manner, adults will be better able to support their children. Encourage adults to talk to friends, family, religious leaders, or mental health counselors.
8. Advise adults to be alert for children who may need professional help. Tell them to be vigilant when monitoring a child’s emotional state. Children who may benefit from mental health counseling after a tragedy may exhibit warning signs, such as changes in behavior, appetite, and sleep patterns, which may indicate the child is experiencing grief, anxiety, or discomfort.
Remind adults to be aware of children who are at greater risk for mental health issues, including those who are already struggling with other recent traumatic experiences—past traumatic experiences, personal loss, depression, or other mental illness.1 Be particularly observant for children who may be at risk of suicide.1,2 Professional counseling may be needed for a child who is experiencing an emotional reaction that lasts >1 month and is impacting his or her daily functioning.1
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
In the aftermath of a school shooting, parents and teachers may seek a psychiatrist’s advice on how to best discuss these incidents with children. We offer guidelines on what to tell concerned parents, educators, and other adults who may interact with children affected by a school shooting.
6 tips for interacting with children
1. Talk about the event. Instruct adults to ask children to share their feelings about the incident and to show genuine interest in listening to the child’s thoughts and point of view. Adults shouldn’t pretend the event hasn’t occurred or isn’t serious. Children may be more worried if they think adults are too afraid to tell them what is happening. It is important to gently correct any misinformation older students may have received via social media.1
2. Reinforce that home is a safe haven. Overwhelming emotions and uncertainty can bring about a sense of insecurity in children. Children may come home seeking a safe environment. Advise parents to plan a night where family members participate in a favorite family activity.1 Tell parents to remind their children that trust-worthy adults—parents, emergency workers, police, firefighters, doctors, and the military—are helping provide safety, comfort, and support.2
3. Limit television time. If children are exposed to the news, parents should watch it with them briefly, but avoid letting children rewatch the same event repetitively. Constant exposure to the event may heighten a child’s anxiety and fears.
4. Maintain a normal routine. Tell parents they should maintain, as best they can, their normal routine for dinner, homework, chores, and bedtime, but to remain flexible.2 Children may have a hard time concentrating on schoolwork or falling asleep. Advise parents to spend extra time reading or playing quiet games with their children, particularly at bedtime. These activities are calming, foster a sense of closeness and security, and reinforce a feeling of normalcy.
5. Encourage emotions. Instruct parents to explain to their children that all feelings are okay and normal, and to let children talk about their feelings and help put them into perspective.1 Children may need help in expressing these feelings, so be patient. If an incident happened at the child’s school, teachers and administrators may conduct group sessions to help children express their concerns about being back in school.
6. Seek creativity or spirituality. Encourage parents and other adults to provide a creative outlet for children, such as making get well cards or sending letters to the survivors and their families. Writing thank you letters to doctors, nurses, fire-fighters, and police officers also may be comforting.1,2 Suggest that parents encourage their children to pray or think hopeful thoughts for the victims and their families.
2 tips for interacting with adults
7. Recommend they take care of themselves. Explain to adult caregivers that because children learn by observing, they shouldn’t ignore their own feelings of anxiety, grief, and anger. By expressing their emotions in a productive manner, adults will be better able to support their children. Encourage adults to talk to friends, family, religious leaders, or mental health counselors.
8. Advise adults to be alert for children who may need professional help. Tell them to be vigilant when monitoring a child’s emotional state. Children who may benefit from mental health counseling after a tragedy may exhibit warning signs, such as changes in behavior, appetite, and sleep patterns, which may indicate the child is experiencing grief, anxiety, or discomfort.
Remind adults to be aware of children who are at greater risk for mental health issues, including those who are already struggling with other recent traumatic experiences—past traumatic experiences, personal loss, depression, or other mental illness.1 Be particularly observant for children who may be at risk of suicide.1,2 Professional counseling may be needed for a child who is experiencing an emotional reaction that lasts >1 month and is impacting his or her daily functioning.1
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. American Psychological Association. Helping your children manage distress in the aftermath of a shooting. http://www.apa.org/helpcenter/aftermath.aspx. Updated April 2011. Accessed February 15, 2013.
2. National Association of School Psychologists resources. A national tragedy: helping children cope. http://www.nasponline.org/resources/crisis_safety/terror_general.aspx. Published September 2001. Accessed February 15, 2013.
1. American Psychological Association. Helping your children manage distress in the aftermath of a shooting. http://www.apa.org/helpcenter/aftermath.aspx. Updated April 2011. Accessed February 15, 2013.
2. National Association of School Psychologists resources. A national tragedy: helping children cope. http://www.nasponline.org/resources/crisis_safety/terror_general.aspx. Published September 2001. Accessed February 15, 2013.
Stiff person syndrome: What psychiatrists need to know
Stiff person syndrome (SPS) is a rare autoimmune condition characterized by stiffness and rigidity in the lower limb muscles. Because SPS often is misdiagnosed as a psychiatric illness and psychiatric comorbidities are common in patients with this disorder,1 awareness and recognition of this unique condition is essential.
An insidious presentation
Patients with SPS present with:2
- axial muscle stiffness slowly progressing to proximal muscles
- unremarkable motor, sensory, and cranial nerve examinations with normal intellectual functioning
- normal muscle strength, although electromyography shows continuous motor activity
- spasms evoked by sudden movements, jarring noise, and emotional distress
- slow and cautious gait to avoid triggering spasms and falls.
Symptoms start slowly and insidiously. Axial muscle stiffness can result in spinal deformity. Involvement is asymmetrical, with a predilection for proximal lower limb and lumbar paraspinal muscles. Affected muscles reveal tight, hard, board-like rigidity. In later stages of SPS, mild atrophy and muscle weakness are likely.
Frequent misdiagnosis
Because facial muscle spasticity is prominent, SPS patients may be misdiagnosed with Parkinson’s disease, primary lateral sclerosis, or multiple sclerosis. Spasms affecting respiratory and thoracic paraspinal muscles (status spasticus) may be misdiagnosed as an anxiety-related condition. These spasms can be life-threatening and require IV diazepam and supportive measures.
More than 60% of SPS patients have a comorbid psychiatric disorder.3 Anxiety disorders—generalized anxiety disorder, agoraphobia, and panic disorder—major depression, and alcohol abuse are the most frequent psychiatric comorbidities seen in SPS patients.3
SPS patients who panic when in public may be misdiagnosed with agoraphobia.3 Emotional stimuli may cause muscle spasms leading to falls. Treating muscle spasticity with γ-aminobutyric acid (GABA) agonists and narcotics can lead to drug abuse and dependence. Muscle spasticity can fluctuate from hour to hour, abate with sleep, and get worse with emotional distress. These findings are why approximately 70% of SPS patients are initially misdiagnosed; conversion disorder is a frequent misdiagnosis.4 Mood disorder in SPS patients may be resistant to antidepressants until these patients are treated with immunotherapy.4
Treating SPS patients
Although early intervention can reduce long-term disability, approximately 50% of SPS patients eventually have to use a wheelchair as a result of pain and immobility.5
Antibodies to glutamic acid decarboxylase, which is the rate-limiting enzyme for GABA synthesis, are present in 85% of SPS patients.5 Therefore, treatment usually includes GABA-enhancing drugs, including sedative anxiolytics (clonazepam and diazepam), antiepileptics (gabapentin, levetiracetam, tiagabine, and vigabatrin), antispasticity drugs (baclofen, dantrolene, and tizanidine), and immunotherapy (corticosteroids, IV immunoglobulins, and rituximab).5 Antidepressants, biofeedback, and relaxation training also can offer relief. Psychotherapy and substance dependency interventions may be needed.
To achieve optimum outcomes in SPS patients, a close collaborative relationship among all treating clinicians—including primary care physicians, neurologists, anesthesiologists, and psychiatrists—is necessary.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Tinsley JA, Barth EM, Black JL, et al. Psychiatric consultations in stiff-man syndrome. J Clin Psychiatry. 1997;58(10):444-449.
2. Egwuonwu S, Chedebeau F. Stiff-person syndrome: a case report and review of the literature. J Natl Med Assoc. 2010;102(12):1261-1263.
3. Black JL, Barth EM, Williams DE, et al. Stiff-man syndrome. Results of interviews and psychologic testing. Psychosomatics. 1998;39(1):38-44.
4. Culav-Sumić J, Bosnjak I, Pastar Z, et al. Anxious depression and the stiff-person plus syndrome. Cogn Behav Neurol. 2008;21(4):242-245.
5. Hadavi S, Noyce AJ, Leslie RD, et al. Stiff person syndrome. Pract Neurol. 2011;11(5):272-282.
Stiff person syndrome (SPS) is a rare autoimmune condition characterized by stiffness and rigidity in the lower limb muscles. Because SPS often is misdiagnosed as a psychiatric illness and psychiatric comorbidities are common in patients with this disorder,1 awareness and recognition of this unique condition is essential.
An insidious presentation
Patients with SPS present with:2
- axial muscle stiffness slowly progressing to proximal muscles
- unremarkable motor, sensory, and cranial nerve examinations with normal intellectual functioning
- normal muscle strength, although electromyography shows continuous motor activity
- spasms evoked by sudden movements, jarring noise, and emotional distress
- slow and cautious gait to avoid triggering spasms and falls.
Symptoms start slowly and insidiously. Axial muscle stiffness can result in spinal deformity. Involvement is asymmetrical, with a predilection for proximal lower limb and lumbar paraspinal muscles. Affected muscles reveal tight, hard, board-like rigidity. In later stages of SPS, mild atrophy and muscle weakness are likely.
Frequent misdiagnosis
Because facial muscle spasticity is prominent, SPS patients may be misdiagnosed with Parkinson’s disease, primary lateral sclerosis, or multiple sclerosis. Spasms affecting respiratory and thoracic paraspinal muscles (status spasticus) may be misdiagnosed as an anxiety-related condition. These spasms can be life-threatening and require IV diazepam and supportive measures.
More than 60% of SPS patients have a comorbid psychiatric disorder.3 Anxiety disorders—generalized anxiety disorder, agoraphobia, and panic disorder—major depression, and alcohol abuse are the most frequent psychiatric comorbidities seen in SPS patients.3
SPS patients who panic when in public may be misdiagnosed with agoraphobia.3 Emotional stimuli may cause muscle spasms leading to falls. Treating muscle spasticity with γ-aminobutyric acid (GABA) agonists and narcotics can lead to drug abuse and dependence. Muscle spasticity can fluctuate from hour to hour, abate with sleep, and get worse with emotional distress. These findings are why approximately 70% of SPS patients are initially misdiagnosed; conversion disorder is a frequent misdiagnosis.4 Mood disorder in SPS patients may be resistant to antidepressants until these patients are treated with immunotherapy.4
Treating SPS patients
Although early intervention can reduce long-term disability, approximately 50% of SPS patients eventually have to use a wheelchair as a result of pain and immobility.5
Antibodies to glutamic acid decarboxylase, which is the rate-limiting enzyme for GABA synthesis, are present in 85% of SPS patients.5 Therefore, treatment usually includes GABA-enhancing drugs, including sedative anxiolytics (clonazepam and diazepam), antiepileptics (gabapentin, levetiracetam, tiagabine, and vigabatrin), antispasticity drugs (baclofen, dantrolene, and tizanidine), and immunotherapy (corticosteroids, IV immunoglobulins, and rituximab).5 Antidepressants, biofeedback, and relaxation training also can offer relief. Psychotherapy and substance dependency interventions may be needed.
To achieve optimum outcomes in SPS patients, a close collaborative relationship among all treating clinicians—including primary care physicians, neurologists, anesthesiologists, and psychiatrists—is necessary.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Stiff person syndrome (SPS) is a rare autoimmune condition characterized by stiffness and rigidity in the lower limb muscles. Because SPS often is misdiagnosed as a psychiatric illness and psychiatric comorbidities are common in patients with this disorder,1 awareness and recognition of this unique condition is essential.
An insidious presentation
Patients with SPS present with:2
- axial muscle stiffness slowly progressing to proximal muscles
- unremarkable motor, sensory, and cranial nerve examinations with normal intellectual functioning
- normal muscle strength, although electromyography shows continuous motor activity
- spasms evoked by sudden movements, jarring noise, and emotional distress
- slow and cautious gait to avoid triggering spasms and falls.
Symptoms start slowly and insidiously. Axial muscle stiffness can result in spinal deformity. Involvement is asymmetrical, with a predilection for proximal lower limb and lumbar paraspinal muscles. Affected muscles reveal tight, hard, board-like rigidity. In later stages of SPS, mild atrophy and muscle weakness are likely.
Frequent misdiagnosis
Because facial muscle spasticity is prominent, SPS patients may be misdiagnosed with Parkinson’s disease, primary lateral sclerosis, or multiple sclerosis. Spasms affecting respiratory and thoracic paraspinal muscles (status spasticus) may be misdiagnosed as an anxiety-related condition. These spasms can be life-threatening and require IV diazepam and supportive measures.
More than 60% of SPS patients have a comorbid psychiatric disorder.3 Anxiety disorders—generalized anxiety disorder, agoraphobia, and panic disorder—major depression, and alcohol abuse are the most frequent psychiatric comorbidities seen in SPS patients.3
SPS patients who panic when in public may be misdiagnosed with agoraphobia.3 Emotional stimuli may cause muscle spasms leading to falls. Treating muscle spasticity with γ-aminobutyric acid (GABA) agonists and narcotics can lead to drug abuse and dependence. Muscle spasticity can fluctuate from hour to hour, abate with sleep, and get worse with emotional distress. These findings are why approximately 70% of SPS patients are initially misdiagnosed; conversion disorder is a frequent misdiagnosis.4 Mood disorder in SPS patients may be resistant to antidepressants until these patients are treated with immunotherapy.4
Treating SPS patients
Although early intervention can reduce long-term disability, approximately 50% of SPS patients eventually have to use a wheelchair as a result of pain and immobility.5
Antibodies to glutamic acid decarboxylase, which is the rate-limiting enzyme for GABA synthesis, are present in 85% of SPS patients.5 Therefore, treatment usually includes GABA-enhancing drugs, including sedative anxiolytics (clonazepam and diazepam), antiepileptics (gabapentin, levetiracetam, tiagabine, and vigabatrin), antispasticity drugs (baclofen, dantrolene, and tizanidine), and immunotherapy (corticosteroids, IV immunoglobulins, and rituximab).5 Antidepressants, biofeedback, and relaxation training also can offer relief. Psychotherapy and substance dependency interventions may be needed.
To achieve optimum outcomes in SPS patients, a close collaborative relationship among all treating clinicians—including primary care physicians, neurologists, anesthesiologists, and psychiatrists—is necessary.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Tinsley JA, Barth EM, Black JL, et al. Psychiatric consultations in stiff-man syndrome. J Clin Psychiatry. 1997;58(10):444-449.
2. Egwuonwu S, Chedebeau F. Stiff-person syndrome: a case report and review of the literature. J Natl Med Assoc. 2010;102(12):1261-1263.
3. Black JL, Barth EM, Williams DE, et al. Stiff-man syndrome. Results of interviews and psychologic testing. Psychosomatics. 1998;39(1):38-44.
4. Culav-Sumić J, Bosnjak I, Pastar Z, et al. Anxious depression and the stiff-person plus syndrome. Cogn Behav Neurol. 2008;21(4):242-245.
5. Hadavi S, Noyce AJ, Leslie RD, et al. Stiff person syndrome. Pract Neurol. 2011;11(5):272-282.
1. Tinsley JA, Barth EM, Black JL, et al. Psychiatric consultations in stiff-man syndrome. J Clin Psychiatry. 1997;58(10):444-449.
2. Egwuonwu S, Chedebeau F. Stiff-person syndrome: a case report and review of the literature. J Natl Med Assoc. 2010;102(12):1261-1263.
3. Black JL, Barth EM, Williams DE, et al. Stiff-man syndrome. Results of interviews and psychologic testing. Psychosomatics. 1998;39(1):38-44.
4. Culav-Sumić J, Bosnjak I, Pastar Z, et al. Anxious depression and the stiff-person plus syndrome. Cogn Behav Neurol. 2008;21(4):242-245.
5. Hadavi S, Noyce AJ, Leslie RD, et al. Stiff person syndrome. Pract Neurol. 2011;11(5):272-282.
Teens, social media, and ‘sexting’: What to tell parents
Discuss this article at www.facebook.com/CurrentPsychiatry
Children and adolescents who have unrestricted use of the internet and cell phones are at increased risk for being exposed to sexually explicit material. One study found almost 1 in 5 high school students have “sexted”—sending a text message with sexually explicit pictures—and almost twice as many reported that they had received a sexually explicit picture via cell phone.1 More than 25% of students acknowledged forwarding a sexually explicit picture to others; >33% did so despite knowing the legal consequences, including being arrested and facing pornography charges.1
Concerned parents may seek advice on how to prevent their child from receiving or sending sexually inappropriate material on the internet or on their cell phones. You can help parents keep their children safe by sharing the following tips from The American Academy of Pediatrics (AAP)2:
Keep up with technology. Advise parents to become familiar with popular social networking websites such as Facebook. Creating their own Facebook page and “friending” their child may help them facilitate a conversation about their individual online experiences.
Enable privacy features. Instruct parents to install parental controls on their child’s computer. Explain to parents that these monitoring systems can help them check their child’s e-mail, chat records, and instant messages. Many social networking sites have privacy features that can help block unwanted users from contacting a child.
Check up on your children. Parents should let children know they are aware of their online presence and will be keeping an eye on them. They should periodically check a child’s chat logs, messages, e-mails, and social networking profiles for inappropriate content, friends, messages, and images. Instruct parents to teach their children that nothing is private once it’s posted on the internet. Suggest keeping the child’s computer in a public location such as the family room or kitchen.
Limit time spent online. Explain to parents that they should limit their child’s internet and cell phone access.
Combating ‘sexting’
Suggest to parents that they explain to their child in an age-appropriate manner what sexting is before giving their child a cell phone. The AAP2 recommends that parents make sure their children understand the legal ramifications of sexting. A child who is caught sexting could be arrested, which may hurt his or her chances of being accepted into college or getting a job. A simple way to reduce a child’s opportunities for sexting is to restrict his or her access to a cell phone during social situations where peer pressure could influence behavior.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Strassberg DS, McKinnon RK, Sustaíta MA. Sexting by high school students: an exploratory and descriptive study [published online June 7, 2012]. Arch Sex Behav. doi: 10.1007/s10508-012-9969-8.
2. American Academy of Pediatrics. Talking to kids and teens about social media and sexting. http://www.aap.org/en-us/about-the-aap/aap-press-room/news-features-and-safety-tips/pages/Talking-to-Kids-and-Teens-About-Social-Media-and-Sexting.aspx?. Published June 2009. Updated March 2, 2011. Accessed August 14, 2012.
Discuss this article at www.facebook.com/CurrentPsychiatry
Children and adolescents who have unrestricted use of the internet and cell phones are at increased risk for being exposed to sexually explicit material. One study found almost 1 in 5 high school students have “sexted”—sending a text message with sexually explicit pictures—and almost twice as many reported that they had received a sexually explicit picture via cell phone.1 More than 25% of students acknowledged forwarding a sexually explicit picture to others; >33% did so despite knowing the legal consequences, including being arrested and facing pornography charges.1
Concerned parents may seek advice on how to prevent their child from receiving or sending sexually inappropriate material on the internet or on their cell phones. You can help parents keep their children safe by sharing the following tips from The American Academy of Pediatrics (AAP)2:
Keep up with technology. Advise parents to become familiar with popular social networking websites such as Facebook. Creating their own Facebook page and “friending” their child may help them facilitate a conversation about their individual online experiences.
Enable privacy features. Instruct parents to install parental controls on their child’s computer. Explain to parents that these monitoring systems can help them check their child’s e-mail, chat records, and instant messages. Many social networking sites have privacy features that can help block unwanted users from contacting a child.
Check up on your children. Parents should let children know they are aware of their online presence and will be keeping an eye on them. They should periodically check a child’s chat logs, messages, e-mails, and social networking profiles for inappropriate content, friends, messages, and images. Instruct parents to teach their children that nothing is private once it’s posted on the internet. Suggest keeping the child’s computer in a public location such as the family room or kitchen.
Limit time spent online. Explain to parents that they should limit their child’s internet and cell phone access.
Combating ‘sexting’
Suggest to parents that they explain to their child in an age-appropriate manner what sexting is before giving their child a cell phone. The AAP2 recommends that parents make sure their children understand the legal ramifications of sexting. A child who is caught sexting could be arrested, which may hurt his or her chances of being accepted into college or getting a job. A simple way to reduce a child’s opportunities for sexting is to restrict his or her access to a cell phone during social situations where peer pressure could influence behavior.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Children and adolescents who have unrestricted use of the internet and cell phones are at increased risk for being exposed to sexually explicit material. One study found almost 1 in 5 high school students have “sexted”—sending a text message with sexually explicit pictures—and almost twice as many reported that they had received a sexually explicit picture via cell phone.1 More than 25% of students acknowledged forwarding a sexually explicit picture to others; >33% did so despite knowing the legal consequences, including being arrested and facing pornography charges.1
Concerned parents may seek advice on how to prevent their child from receiving or sending sexually inappropriate material on the internet or on their cell phones. You can help parents keep their children safe by sharing the following tips from The American Academy of Pediatrics (AAP)2:
Keep up with technology. Advise parents to become familiar with popular social networking websites such as Facebook. Creating their own Facebook page and “friending” their child may help them facilitate a conversation about their individual online experiences.
Enable privacy features. Instruct parents to install parental controls on their child’s computer. Explain to parents that these monitoring systems can help them check their child’s e-mail, chat records, and instant messages. Many social networking sites have privacy features that can help block unwanted users from contacting a child.
Check up on your children. Parents should let children know they are aware of their online presence and will be keeping an eye on them. They should periodically check a child’s chat logs, messages, e-mails, and social networking profiles for inappropriate content, friends, messages, and images. Instruct parents to teach their children that nothing is private once it’s posted on the internet. Suggest keeping the child’s computer in a public location such as the family room or kitchen.
Limit time spent online. Explain to parents that they should limit their child’s internet and cell phone access.
Combating ‘sexting’
Suggest to parents that they explain to their child in an age-appropriate manner what sexting is before giving their child a cell phone. The AAP2 recommends that parents make sure their children understand the legal ramifications of sexting. A child who is caught sexting could be arrested, which may hurt his or her chances of being accepted into college or getting a job. A simple way to reduce a child’s opportunities for sexting is to restrict his or her access to a cell phone during social situations where peer pressure could influence behavior.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Strassberg DS, McKinnon RK, Sustaíta MA. Sexting by high school students: an exploratory and descriptive study [published online June 7, 2012]. Arch Sex Behav. doi: 10.1007/s10508-012-9969-8.
2. American Academy of Pediatrics. Talking to kids and teens about social media and sexting. http://www.aap.org/en-us/about-the-aap/aap-press-room/news-features-and-safety-tips/pages/Talking-to-Kids-and-Teens-About-Social-Media-and-Sexting.aspx?. Published June 2009. Updated March 2, 2011. Accessed August 14, 2012.
1. Strassberg DS, McKinnon RK, Sustaíta MA. Sexting by high school students: an exploratory and descriptive study [published online June 7, 2012]. Arch Sex Behav. doi: 10.1007/s10508-012-9969-8.
2. American Academy of Pediatrics. Talking to kids and teens about social media and sexting. http://www.aap.org/en-us/about-the-aap/aap-press-room/news-features-and-safety-tips/pages/Talking-to-Kids-and-Teens-About-Social-Media-and-Sexting.aspx?. Published June 2009. Updated March 2, 2011. Accessed August 14, 2012.
Sleep terrors in adults: How to help control this potentially dangerous condition
Sleep terrors (STs)—also known as night terrors—are characterized by sudden arousal accompanied by a piercing scream or cry in the first few hours after falling asleep. These parasomnias arise out of slow-wave sleep (stages 3 and 4 of nonrapid eye movement [non-REM] sleep) and affect approximately 5% of adults.1 The condition is twice as common in men than women, and usually affects children but may not develop until adulthood.1
During STs, a patient may act scared, afraid, agitated, anxious, or panicky without being fully aware of his or her surroundings. The episode may last 30 seconds to 5 minutes; most patients don’t remember the event the next morning. STs may leave individuals feeling exhausted and perplexed the next day. Verbalization during the episode is incoherent and a patient’s perception of the environment seems altered. Tachycardia, tachypnea, sweating, flushed skin, or mydriasis are prominent. When ST patients walk, they may do so violently and can cause harm to themselves or others.
The differential diagnosis of STs includes posttraumatic stress disorder; nocturnal seizures characterized by excessive motor activity and organic CNS lesions; REM sleep behavior disorder; sleep choking syndrome; and nocturnal panic attacks. Patients with STs report high rates of stressful events—eg, divorce or bereavement—in the previous year. They are more likely to have a history of mood and anxiety disorders and high levels of depression, anxiety, and obsessive-compulsive and phobic traits. One study found patients with STs were 4.3 times more likely to have had a car accident in the past year.2
Evaluating and treating STs
Rule out comorbid conditions such as obstructive sleep apnea and periodic limb movement disorder. Encourage your patient to improve his or her sleep hygiene by maintaining a regular sleep/wake cycle, exercising, and limiting caffeine and alcohol and exposure to bright light before bedtime.
Self-help techniques. To avoid injury, encourage your patient to remove dangerous objects from their sleeping area. Suggest locking the doors to the room or home, and putting medications in a secure place. Patients also may consider keeping their mattress close to the floor to limit the risk of injury.
Pharmacotherapy and psychotherapy. Along with counseling and support, your patient may benefit from cognitive-behavioral therapy, relaxation therapy, or hypnosis.3 Anticipatory arousal therapy may help by interrupting the altered underlying electrophysiology of partial arousal.
If your patient is concerned about physical injury during STs, consider prescribing clonazepam, temazepam, or diazepam.4 Trazodone and selective serotonin reuptake inhibitors such as paroxetine5 also have been used to treat STs.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Crisp AH. The sleepwalking/night terrors syndrome in adults. Postgrad Med J. 1996;72(852):599-604.
2. Oudiette D, Leu S, Pottier M, et al. Dreamlike mentations during sleepwalking and sleep terrors in adults. Sleep. 2009;32(12):1621-1627.
3. Lowe P, Humphreys C, Williams SJ. Night terrors: women’s experiences of (not) sleeping where there is domestic violence. Violence Against Women. 2007;13(6):549-561.
4. Schenck CH, Mahowald MW. Long-term nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med. 1996;100(3):333-337.
5. Lillywhite AR, Wilson SJ, Nutt DJ. Successful treatment of night terrors and somnambulism with paroxetine. Br J Psychiatry. 1994;164(4):551-554.
Sleep terrors (STs)—also known as night terrors—are characterized by sudden arousal accompanied by a piercing scream or cry in the first few hours after falling asleep. These parasomnias arise out of slow-wave sleep (stages 3 and 4 of nonrapid eye movement [non-REM] sleep) and affect approximately 5% of adults.1 The condition is twice as common in men than women, and usually affects children but may not develop until adulthood.1
During STs, a patient may act scared, afraid, agitated, anxious, or panicky without being fully aware of his or her surroundings. The episode may last 30 seconds to 5 minutes; most patients don’t remember the event the next morning. STs may leave individuals feeling exhausted and perplexed the next day. Verbalization during the episode is incoherent and a patient’s perception of the environment seems altered. Tachycardia, tachypnea, sweating, flushed skin, or mydriasis are prominent. When ST patients walk, they may do so violently and can cause harm to themselves or others.
The differential diagnosis of STs includes posttraumatic stress disorder; nocturnal seizures characterized by excessive motor activity and organic CNS lesions; REM sleep behavior disorder; sleep choking syndrome; and nocturnal panic attacks. Patients with STs report high rates of stressful events—eg, divorce or bereavement—in the previous year. They are more likely to have a history of mood and anxiety disorders and high levels of depression, anxiety, and obsessive-compulsive and phobic traits. One study found patients with STs were 4.3 times more likely to have had a car accident in the past year.2
Evaluating and treating STs
Rule out comorbid conditions such as obstructive sleep apnea and periodic limb movement disorder. Encourage your patient to improve his or her sleep hygiene by maintaining a regular sleep/wake cycle, exercising, and limiting caffeine and alcohol and exposure to bright light before bedtime.
Self-help techniques. To avoid injury, encourage your patient to remove dangerous objects from their sleeping area. Suggest locking the doors to the room or home, and putting medications in a secure place. Patients also may consider keeping their mattress close to the floor to limit the risk of injury.
Pharmacotherapy and psychotherapy. Along with counseling and support, your patient may benefit from cognitive-behavioral therapy, relaxation therapy, or hypnosis.3 Anticipatory arousal therapy may help by interrupting the altered underlying electrophysiology of partial arousal.
If your patient is concerned about physical injury during STs, consider prescribing clonazepam, temazepam, or diazepam.4 Trazodone and selective serotonin reuptake inhibitors such as paroxetine5 also have been used to treat STs.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Sleep terrors (STs)—also known as night terrors—are characterized by sudden arousal accompanied by a piercing scream or cry in the first few hours after falling asleep. These parasomnias arise out of slow-wave sleep (stages 3 and 4 of nonrapid eye movement [non-REM] sleep) and affect approximately 5% of adults.1 The condition is twice as common in men than women, and usually affects children but may not develop until adulthood.1
During STs, a patient may act scared, afraid, agitated, anxious, or panicky without being fully aware of his or her surroundings. The episode may last 30 seconds to 5 minutes; most patients don’t remember the event the next morning. STs may leave individuals feeling exhausted and perplexed the next day. Verbalization during the episode is incoherent and a patient’s perception of the environment seems altered. Tachycardia, tachypnea, sweating, flushed skin, or mydriasis are prominent. When ST patients walk, they may do so violently and can cause harm to themselves or others.
The differential diagnosis of STs includes posttraumatic stress disorder; nocturnal seizures characterized by excessive motor activity and organic CNS lesions; REM sleep behavior disorder; sleep choking syndrome; and nocturnal panic attacks. Patients with STs report high rates of stressful events—eg, divorce or bereavement—in the previous year. They are more likely to have a history of mood and anxiety disorders and high levels of depression, anxiety, and obsessive-compulsive and phobic traits. One study found patients with STs were 4.3 times more likely to have had a car accident in the past year.2
Evaluating and treating STs
Rule out comorbid conditions such as obstructive sleep apnea and periodic limb movement disorder. Encourage your patient to improve his or her sleep hygiene by maintaining a regular sleep/wake cycle, exercising, and limiting caffeine and alcohol and exposure to bright light before bedtime.
Self-help techniques. To avoid injury, encourage your patient to remove dangerous objects from their sleeping area. Suggest locking the doors to the room or home, and putting medications in a secure place. Patients also may consider keeping their mattress close to the floor to limit the risk of injury.
Pharmacotherapy and psychotherapy. Along with counseling and support, your patient may benefit from cognitive-behavioral therapy, relaxation therapy, or hypnosis.3 Anticipatory arousal therapy may help by interrupting the altered underlying electrophysiology of partial arousal.
If your patient is concerned about physical injury during STs, consider prescribing clonazepam, temazepam, or diazepam.4 Trazodone and selective serotonin reuptake inhibitors such as paroxetine5 also have been used to treat STs.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Crisp AH. The sleepwalking/night terrors syndrome in adults. Postgrad Med J. 1996;72(852):599-604.
2. Oudiette D, Leu S, Pottier M, et al. Dreamlike mentations during sleepwalking and sleep terrors in adults. Sleep. 2009;32(12):1621-1627.
3. Lowe P, Humphreys C, Williams SJ. Night terrors: women’s experiences of (not) sleeping where there is domestic violence. Violence Against Women. 2007;13(6):549-561.
4. Schenck CH, Mahowald MW. Long-term nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med. 1996;100(3):333-337.
5. Lillywhite AR, Wilson SJ, Nutt DJ. Successful treatment of night terrors and somnambulism with paroxetine. Br J Psychiatry. 1994;164(4):551-554.
1. Crisp AH. The sleepwalking/night terrors syndrome in adults. Postgrad Med J. 1996;72(852):599-604.
2. Oudiette D, Leu S, Pottier M, et al. Dreamlike mentations during sleepwalking and sleep terrors in adults. Sleep. 2009;32(12):1621-1627.
3. Lowe P, Humphreys C, Williams SJ. Night terrors: women’s experiences of (not) sleeping where there is domestic violence. Violence Against Women. 2007;13(6):549-561.
4. Schenck CH, Mahowald MW. Long-term nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med. 1996;100(3):333-337.
5. Lillywhite AR, Wilson SJ, Nutt DJ. Successful treatment of night terrors and somnambulism with paroxetine. Br J Psychiatry. 1994;164(4):551-554.
‘Bugs in my skin’: What you should know about delusional infestation
Patients with delusional infestation (DI) falsely believe that they are infested with tiny infectious agents—typically vermin, insects, or small animals—that crawl on, in, or under their skin, leaving marks and building nests.1 Patients often describe the pathogens on the skin of hands, arms, feet, lower legs, scalp, or genital areas. They state the pathogen is difficult to diagnose and usually is contracted by human contact. Most patients with DI engage in intensive, repetitive, and often dangerous self-cleansing to get rid of the pathogens, which results in skin lesions.1 Less often, patients believe they are infested with bacteria or viruses.1
The typical DI patient is a middle age or older female with few social contacts, no psychiatric history, and normal cognitive and social function.1 Geriatric patients with dementia and vision or hearing impairment who live in a nursing home may develop DI; it also may be seen in geriatric patients with vascular encephalopathy.
What to consider
First rule out a genuine infestation by referring your patient for dermatologic and microbiologic testing. Order basic laboratory tests to assess inflammation markers—complete blood cell count, erythrocyte sedimentation rate, C-reactive protein, electrolytes, liver function, thyroid-stimulating hormone, and fasting glucose.1 Suggest a cranial MRI to rule out a brain disorder. Also, perform a urinalysis for cocaine, amphetamines, or cannabinoids, which can cause DI.1 Rule out medical conditions that are associated with pruritus and psychiatric symptoms, including endocrine, renal, hepatic, rheumatoid, and nutritional conditions.
Treating DI patients
Collaborate with a dermatologist, microbiologist, and primary care physician because these clinicians can deliver medical interventions, such as treating skin lesions and prescribing non-sedating antihistamines to alleviate pruritus. The Table1 offers other suggestions for managing DI patients.
Pharmacotherapy. Although high-quality evidence supporting antipsychotics for treating DI is lacking, olanzapine and risperidone are considered first-line agents; haloperidol and perphenazine also are recommended.1 Response and remission rates are similar with typical and atypical antipsychotics and the median onset of efficacy with antipsychotics is approximately 1.5 weeks.1,2 Antidepressants—including escitalopram, sertraline, mirtazapine, and venlafaxine—have been shown to effectively treat DI.3 In treatment-resistant cases, pimozide and electroconvulsive therapy have been used.1
Psychotherapy is effective for only 10% of DI patients.4
Table
Treating patients with DI: What to do and what to avoid
| Do’s | Don’t |
|---|---|
| Do acknowledge and empathize with your patient’s concerns | Don’t try to convince your patient he or she is wrong about the self-diagnosis |
| Do perform a thorough physical exam and diagnostic investigation | Don’t use words such as “delusional” or “psychotic” |
| Do paraphrase symptoms as “sensations” or “crawling” instead of reinforcing or questioning them | Don’t start psychopharmacology until you establish rapport with your patient |
| Do indicate that symptoms could be secondary to overactivity of the nervous system or “unexplained dermopathy” | |
| Do suggest that antipsychotics may help reduce your patient’s distress and itching | |
| DI: delusional infestation Source: Adapted from reference 1 | |
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690-732.
2. Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28(5):500-508.
3. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746-758.
4. Wykoff RF. Delusions of parasitosis: a review. Rev Infect Dis. 1987;9(3):433-437.
Patients with delusional infestation (DI) falsely believe that they are infested with tiny infectious agents—typically vermin, insects, or small animals—that crawl on, in, or under their skin, leaving marks and building nests.1 Patients often describe the pathogens on the skin of hands, arms, feet, lower legs, scalp, or genital areas. They state the pathogen is difficult to diagnose and usually is contracted by human contact. Most patients with DI engage in intensive, repetitive, and often dangerous self-cleansing to get rid of the pathogens, which results in skin lesions.1 Less often, patients believe they are infested with bacteria or viruses.1
The typical DI patient is a middle age or older female with few social contacts, no psychiatric history, and normal cognitive and social function.1 Geriatric patients with dementia and vision or hearing impairment who live in a nursing home may develop DI; it also may be seen in geriatric patients with vascular encephalopathy.
What to consider
First rule out a genuine infestation by referring your patient for dermatologic and microbiologic testing. Order basic laboratory tests to assess inflammation markers—complete blood cell count, erythrocyte sedimentation rate, C-reactive protein, electrolytes, liver function, thyroid-stimulating hormone, and fasting glucose.1 Suggest a cranial MRI to rule out a brain disorder. Also, perform a urinalysis for cocaine, amphetamines, or cannabinoids, which can cause DI.1 Rule out medical conditions that are associated with pruritus and psychiatric symptoms, including endocrine, renal, hepatic, rheumatoid, and nutritional conditions.
Treating DI patients
Collaborate with a dermatologist, microbiologist, and primary care physician because these clinicians can deliver medical interventions, such as treating skin lesions and prescribing non-sedating antihistamines to alleviate pruritus. The Table1 offers other suggestions for managing DI patients.
Pharmacotherapy. Although high-quality evidence supporting antipsychotics for treating DI is lacking, olanzapine and risperidone are considered first-line agents; haloperidol and perphenazine also are recommended.1 Response and remission rates are similar with typical and atypical antipsychotics and the median onset of efficacy with antipsychotics is approximately 1.5 weeks.1,2 Antidepressants—including escitalopram, sertraline, mirtazapine, and venlafaxine—have been shown to effectively treat DI.3 In treatment-resistant cases, pimozide and electroconvulsive therapy have been used.1
Psychotherapy is effective for only 10% of DI patients.4
Table
Treating patients with DI: What to do and what to avoid
| Do’s | Don’t |
|---|---|
| Do acknowledge and empathize with your patient’s concerns | Don’t try to convince your patient he or she is wrong about the self-diagnosis |
| Do perform a thorough physical exam and diagnostic investigation | Don’t use words such as “delusional” or “psychotic” |
| Do paraphrase symptoms as “sensations” or “crawling” instead of reinforcing or questioning them | Don’t start psychopharmacology until you establish rapport with your patient |
| Do indicate that symptoms could be secondary to overactivity of the nervous system or “unexplained dermopathy” | |
| Do suggest that antipsychotics may help reduce your patient’s distress and itching | |
| DI: delusional infestation Source: Adapted from reference 1 | |
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Patients with delusional infestation (DI) falsely believe that they are infested with tiny infectious agents—typically vermin, insects, or small animals—that crawl on, in, or under their skin, leaving marks and building nests.1 Patients often describe the pathogens on the skin of hands, arms, feet, lower legs, scalp, or genital areas. They state the pathogen is difficult to diagnose and usually is contracted by human contact. Most patients with DI engage in intensive, repetitive, and often dangerous self-cleansing to get rid of the pathogens, which results in skin lesions.1 Less often, patients believe they are infested with bacteria or viruses.1
The typical DI patient is a middle age or older female with few social contacts, no psychiatric history, and normal cognitive and social function.1 Geriatric patients with dementia and vision or hearing impairment who live in a nursing home may develop DI; it also may be seen in geriatric patients with vascular encephalopathy.
What to consider
First rule out a genuine infestation by referring your patient for dermatologic and microbiologic testing. Order basic laboratory tests to assess inflammation markers—complete blood cell count, erythrocyte sedimentation rate, C-reactive protein, electrolytes, liver function, thyroid-stimulating hormone, and fasting glucose.1 Suggest a cranial MRI to rule out a brain disorder. Also, perform a urinalysis for cocaine, amphetamines, or cannabinoids, which can cause DI.1 Rule out medical conditions that are associated with pruritus and psychiatric symptoms, including endocrine, renal, hepatic, rheumatoid, and nutritional conditions.
Treating DI patients
Collaborate with a dermatologist, microbiologist, and primary care physician because these clinicians can deliver medical interventions, such as treating skin lesions and prescribing non-sedating antihistamines to alleviate pruritus. The Table1 offers other suggestions for managing DI patients.
Pharmacotherapy. Although high-quality evidence supporting antipsychotics for treating DI is lacking, olanzapine and risperidone are considered first-line agents; haloperidol and perphenazine also are recommended.1 Response and remission rates are similar with typical and atypical antipsychotics and the median onset of efficacy with antipsychotics is approximately 1.5 weeks.1,2 Antidepressants—including escitalopram, sertraline, mirtazapine, and venlafaxine—have been shown to effectively treat DI.3 In treatment-resistant cases, pimozide and electroconvulsive therapy have been used.1
Psychotherapy is effective for only 10% of DI patients.4
Table
Treating patients with DI: What to do and what to avoid
| Do’s | Don’t |
|---|---|
| Do acknowledge and empathize with your patient’s concerns | Don’t try to convince your patient he or she is wrong about the self-diagnosis |
| Do perform a thorough physical exam and diagnostic investigation | Don’t use words such as “delusional” or “psychotic” |
| Do paraphrase symptoms as “sensations” or “crawling” instead of reinforcing or questioning them | Don’t start psychopharmacology until you establish rapport with your patient |
| Do indicate that symptoms could be secondary to overactivity of the nervous system or “unexplained dermopathy” | |
| Do suggest that antipsychotics may help reduce your patient’s distress and itching | |
| DI: delusional infestation Source: Adapted from reference 1 | |
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690-732.
2. Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28(5):500-508.
3. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746-758.
4. Wykoff RF. Delusions of parasitosis: a review. Rev Infect Dis. 1987;9(3):433-437.
1. Freudenmann RW, Lepping P. Delusional infestation. Clin Microbiol Rev. 2009;22(4):690-732.
2. Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28(5):500-508.
3. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet. 2009;373(9665):746-758.
4. Wykoff RF. Delusions of parasitosis: a review. Rev Infect Dis. 1987;9(3):433-437.
How to lower suicide risk in depressed children and adolescents
Discuss this article at www.facebook.com/CurrentPsychiatry
Although depression affects nearly 2% of children (age ≤12) and up to 10% of adolescents (age 13 to 18),1 the disorder often is underdiagnosed and undertreated in pediatric patients.2 Treating depression in young patients is challenging. Only 30% to 40% of depressed children and adolescents who receive evidence-based treatment achieve remission.3 In addition, 50% to 70% of those who initially achieve remission will experience recurrence within 5 years.4 Suicide is the third leading cause of death among children and adolescents, and depression greatly increases the likelihood of suicide.5,6
This article reviews assessing and treating depression in children and adolescents, and how to lower suicide risk in pediatric patients.
Symptoms vary with age
Depressive symptoms vary as a function of the child’s cognitive development and social functioning. Hopelessness and vegetative and motivational symptoms may be more frequent in adolescents than in children.7
In preschool-age children, depression manifests indirectly through somatic symptoms and behavioral disturbances. In this age group, sadness or irritability are sensitive and predominant symptoms of depression.8 In older children, sadness and loss of interest in social activities may indicate depression. In adolescents, feelings of mental and physical weariness, aloneness, disconnectedness, uncertainty, vulnerability, anger, irritability, and ambivalence toward friends suggest a depressive disorder.9
Genetic predisposition to depression, poor family support, dysfunctional parenting, and individual vulnerabilities such as poor self-esteem or emotional dysregulation may increase young patients’ risk for depression.10 Peer and family support may protect against depression. Personal competence stemming from social acceptance and body image satisfaction also may be protective factors. A sense of religious and existential well-being (finding meaning and purpose in life) are significantly associated with lower rates of depression among adolescents.11
A persistent illness
The mean duration of a depressive episode in children and adolescents is 7 to 8 months.12 However, subsyndromal depressive symptoms—as well as relapse and recurrence—are common. Long-term studies indicate that many depressed adolescents experience depressive episodes into adulthood.12 Factors that may predict recurrence in adulthood include:
- severity of depressive episodes
- concurrent psychotic symptoms
- suicidal thoughts
- history of recurrent depressive episodes
- threshold residual symptoms
- recent stressful life events
- adverse family environment
- family history of depression.12
Early symptom onset, greater depression severity, suicidality, presence of comorbid anxiety, disruptive disorders, and an adverse family environment also predict longer recovery time.12 A study of depressed adolescents found that a history of recurrent depression, family history of recurrent depression, personality disorder traits, and (for girls only) conflict with parents predicted recurrence of depression in young adulthood.4Table 1 summarizes factors that affect depression outcomes in children and adolescents.
Table 1
What affects depression outcomes in children and adolescents?
| Factor | Outcomes |
|---|---|
| Age | Pharmacotherapy and CBT are equally effective in younger and older adolescents.a Although age does not affect long-term treatment outcomes, older adolescents (age 18 to 19) with treatment-resistant depression may respond better to a combination of CBT and medicationb |
| Sex | Females are more likely to experience relapse.c However, sex does not influence response to initial treatmentc |
| Socioeconomic status | Adolescents with high socioeconomic status are more likely to respond to CBT |
| Illness characteristics | Severity of depression is the strongest predictor of poor outcome.d-f Patients with moderate depression are more likely to benefit from CBT added to medication.g However, adding CBT to medication did not affect outcomes in adolescents with self-injurious behavior.b,f Suicidal behaviors during treatment are less frequent when CBT is combined with medicationh,i |
| Substance abuse | Patients with substance use disorders are less likely to respond to depression treatmentf and those who continued to abuse substances during treatment are less likely to achieve remission than those who abstainb |
| Cognitive measures | Higher levels of hopelessness are associated with poor outcomes. For adolescents with treatment-resistant depression who experience hopelessness, adding CBT to pharmacotherapy did not provide additional benefit. Some studies have noted that adolescents with cognitive distortions are more likely to benefit from CBT plus pharmacotherapyb |
| Family characteristics/environment | High family stress is associated with poor treatment outcomes.f Experiencing loss and physically dangerous events does not affect depression outcomes. Trauma and history of abuse adversely effect depression treatment outcomes |
CBT: cognitive-behavioral therapy
| |
Assessment strategies
Semi-structured interviews such as the Child and Adolescent Psychiatric Assessment, the Diagnostic Interview for Children and Adolescents, and the Kiddie Schedule for Affective Disorder and Schizophrenia are useful for assessing depression in pediatric patients (Table 2).13-16 These tools can be used to assess depression criteria based on information gathered from several sources. Many instruments can be used to assess and monitor pediatric depression, including the Children’s Depression Inventory, the Reynolds Child Depression Scales and Adolescent Depression Scales, and the Child Depression Rating Scale.
To assess suicide risk in depressed younger patients:
- ask about emotional difficulties
- identify lack of developmental progress
- estimate their level of distress
- detect impairment in functioning
- estimate the level of danger to themselves and others.17
The best way to assess for suicidal ideation is to ask about it directly while interviewing the patient and his or her parents. Simple questions such as “Have you ever thought about killing yourself or wish you were dead?” and “Have you ever done anything on purpose to hurt or kill yourself?” can be effective.10 These questions are best placed in the middle or toward the end of a list of questions about depressive symptoms.
Adolescents may be more likely than adults to disclose information about suicidality on self-reports.6 However, self-assessment suicide scales are not a substitute for clinical assessment because they tend to be oversensitive and non-specific and lack predictive value. A positive response to either of these questions should prompt a more detailed clinical investigation. There is no evidence that asking about suicide risk increases suicidal behavior, even in high-risk youths.
Table 2
Assessing children and adolescents: 3 semi-structured interviews
| Interview | Features |
|---|---|
| Child and Adolescent Psychiatric Assessment13 | For patients age 9 to 17. Assesses symptoms from the past 3 months. Administration time: 1 to 2 hours. Requires minimal interviewer experience. Assesses impairment in multiple areas (family, peers, school, leisure activities) |
| Diagnostic Interview for Children and Adolescents14 | Separate versions for children (age 6 to 12) and adolescents (age 13 to 17). Assesses lifetime psychopathology. Administration time: 1 to 2 hours. Interrater reliability varies (poor to good) |
| Kiddie Schedule for Affective Disorders and Schizophrenia15 | Assesses lifetime and current psychopathology. Administration time: 35 minutes to 2.5 hours. Interrater reliability: fair to excellent16 |
Treatment options
Psychotherapy. Several controlled studies and meta-analyses support the efficacy of cognitive-behavioral therapy (CBT) for mild depression in pediatric patients.18-20 Two recent meta-analyses of CBT studies in depressed adolescents found the mean effect size of CBT was 0.34 to 0.35.19,21 However, a separate analysis found CBT did not have long-term benefits for depressed adolescents, particularly patients with a history of abuse.22
Interpersonal therapy also can be effective in adolescent outpatients with mild to moderate depression. One study found the effect size of psychotherapy was modest (0.36).19
Pharmacotherapy. Two meta-analyses support selective serotonin reuptake inhibitors (SSRIs) for treating mild to moderate depression in children and adolescents. One found 61% of depressed patients age <19 who received an SSRI were “much improved” or “very much improved.”23 Another meta-analysis that compared SSRIs and placebo found fluoxetine was more effective than sertraline or citalopram for depressed adolescents.24 Other studies have shown that for severe depression, the effect size of antidepressants (0.69) is higher than that of placebo (0.39).25 Antidepressants are more effective in adolescents than in children.25
Fluoxetine is the only FDA-approved medication for treating depression in children age ≥8. In 2007 the FDA extended to all antidepressants its “black-box” warning about increased risk of suicidality in patients up to age 24. The results of studies that analyzed data about the safety of antidepressants in children and adolescents have been mixed—some found evidence of increased suicidality with antidepressant use,26,27 whereas others showed no increased risk.28,29Table 3 summarizes steps to minimize the risk of antidepressant-induced suicidality.17
Psychotherapy plus pharmacotherapy. Researchers who compared fluoxetine to CBT and to a combination of the 2 in adolescents with moderate to severe depression found that fluoxetine was most effective in the first 12 weeks of treatment.30 Surprisingly, CBT’s effectiveness was not different from placebo.30 However, studies have shown that combining psychotherapy and medication results in greater symptom improvement,30 faster clinical response,31 improvement of global functioning and quality of life,32 and reduced suicidality.33 At 6 months, the difference in response between medication and psychotherapy was small.25 The Treatment of Resistant Depression in Adolescents study found that for chronic adolescent depression, pharmacotherapy (fluoxetine and venlafaxine) combined with CBT produced a higher response rate than pharmacotherapy alone (54% vs 41%).34
Table 3
Protecting against antidepressant-induced suicidality
| Before initiating antidepressant treatment |
|---|
| Review the patient’s psychiatric history |
| Assess for past suicidal behavior |
| Assess for a family history of mental illness or mood disorders and suicide attempts |
| Screen for unrecognized bipolar spectrum disorders |
| Educate patients and their families to watch for signs of worsening depression or suicidality, and to report such symptoms immediately |
| During antidepressant treatment |
| Pay attention to abrupt changes in symptoms, particularly symptoms that were not part of the patient’s initial presentation |
| Watch for deterioration of symptoms |
| Monitor for emergence of ‘activating’ symptoms (ie, irritability, impulsivity, anxiety, insomnia, agitation, hostility, akathisia, hypomania, or mania) |
| Evaluate the patient’s suicide risk factors, including having a specific plan and/or access to lethal means |
| Consider hospitalization if the patient is at high risk for suicide |
| Source: Reference 17 |
Lowering suicide risk
Up to 60% of adolescents who commit suicide had a depressive disorder. Risk factors for child and adolescent suicide attempts include:
- self-harm behaviors
- psychiatric disorders
- family disturbances
- substance abuse
- physical/sexual abuse.17
How to best manage suicidal youths depends on an adequate assessment of the severity of the patient’s current problems and conflicts and the degree of suicidal intent. Assessment of coping resources, access to support systems, and the attitude of the patient and family toward intervention and follow-up also is important.
Children and adolescents at high risk for suicide—those with a plan or recent suicide attempt with high probability of lethality, stated current intent to kill themselves, or recent suicidal ideation or behavior—may need inpatient psychiatric admission. Although no studies have shown that admitting high-risk suicidal patients prevents suicide, hospitalization often is the safest course of action. Develop ing a comprehensive outpatient treatment plan before discharge is essential. Patients with fewer risk factors, especially those who want help and have social support, hope for the future, and a desire to resolve conflicts, may require only a brief crisis-oriented intervention.
The following recommendations for managing suicidality in children and adolescents are based on clinical experience and have not been empirically validated.
Develop a safety plan to direct the patient’s behavior under various situations. For example, the patient would agree in writing that “If I feel depressed, I will do X, Y, and Z to address it,” or “If I find myself having suicidal thoughts, I will contact ABC.” Having a safety plan lowers the risk of a suicide attempt more than having a suicide contract, which does not give the patient any tools.35
Create a ‘hope box.’ This is a box in which the patient collects mementos and other objects that remind him or her of hope and reasons to live. The patient should be able to access it at all times, so he or she can tap into it during crisis periods to avert suicidal acts.35
Counteract alienation. A sense of social isolation and burdensomeness may be “tipping factors” for suicidal acts when adolescents feel depressed.35 Clinicians should try to help connect patients to meaningful social activities, even in small doses.
Manage overarousal. Overarousal in depressed children and adolescents is manifested as agitation. Insomnia is a clinically modifiable risk factor. Insomnia initially responds well to behavioral interventions such as sleep hygiene, sleep restriction, and stimulus control techniques.35
Related Resources
- National Suicide Prevention Lifeline. 800-273-TALK (8255). www.suicidepreventionlifeline.org.
- Suicide Prevention Resource Center. www.sprc.org.
Drug Brand Names
- Citalopram • Celexa
- Fluoxetine • Prozac
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosures
Drs. Shailesh Jain and Islam report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rakesh Jain is a consultant to or has received research/grant support from Eli Lilly and Company, Merck, Pfizer Inc., Shionogi Pharmaceuticals, and Shire.
1. Birmaher B, Brent D. AACAP Work Group on Quality Issues, et al. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503-1526.
2. Lewinsohn PM, Clarke GN, Seeley JR, et al. Major depression in community adolescents: age at onset, episode duration, and time to recurrence. J Am Acad Child Adolesc Psychiatry. 1994;33(6):809-818.
3. Emslie GJ, Kennard BD, Mayes TL. Predictors of treatment response in adolescent depression. Pediatr Ann. 2011;40(6):300-306.
4. Lewinsohn PM, Rohde P, Seeley JR, et al. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry. 2000;157(10):1584-1591.
5. Foley DL, Goldston DB, Costello EJ, et al. Proximal psychiatric risk factors for suicidality in youth: the Great Smoky Mountains Study. Arch Gen Psychiatry. 2006;63(9):1017-1024.
6. Gould MS, Greenberg T, Velting DM, et al. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386-405.
7. Weiss B, Garber J. Developmental differences in the phenomenology of depression. Dev Psychopathol. 2003;15(2):403-430.
8. Calles JL, Jr. Depression in children and adolescents. Prim Care. 2007;34(2):243-258abstract vi.
9. Farmer TJ. The experience of major depression: adolescents’ perspectives. Issues Ment Health Nurs. 2002;23(6):567-585.
10. Zalsman G, Brent DA, Weersing VR. Depressive disorders in childhood and adolescence: an overview: epidemiology clinical manifestation and risk factors. Child Adolesc Psychiatr Clin N Am. 2006;15(4):827-841, vii.
11. Cotton S, Larkin E, Hoopes A, et al. The impact of adolescent spirituality on depressive symptoms and health risk behaviors. J Adolesc Health. 2005;36(6):529.-
12. Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child Adolesc Psychiatr Clin N Am. 2002;11(3):619-637, x.
13. Angold A, Costello EJ. A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C). Psychol Med. 1995;25(4):755-762.
14. Reich W. Diagnostic interview for children and adolescents (DICA). J Am Acad Child Adolesc Psychiatry. 2000;39(1):59-66.
15. Puig-Antich J, Lukens E, Brent D. Psychosocial schedule for school age children - revised. Pittsburgh PA: Western Psychiatric Institute and Clinic; 1986.
16. Ambrosini PJ. Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS). J Am Acad Child Adolesc Psychiatry. 2000;39(1):49-58.
17. Dodig-Curković K, Curković M, Radić J, et al. Suicidal behavior and suicide among children and adolescents-risk factors and epidemiological characteristics. Coll Antropol. 2010;34(2):771-777.
18. Harrington R, Whittaker J, Shoebridge P, et al. Systematic review of efficacy of cognitive behaviour therapies in childhood and adolescent depressive disorder. BMJ. 1998;316(7144):1559-1563.
19. Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychol Bull. 2006;132(1):132-149.
20. Mufson L, Dorta KP, Wickramaratne P, et al. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry. 2004;61(6):577-584.
21. Klein JB, Jacobs RH, Reinecke MA. Cognitive-behavioral therapy for adolescent depression: a meta-analytic investigation of changes in effect-size estimates. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1403-1413.
22. Vitiello B, Emslie G, Clarke G, et al. Long-term outcome of adolescent depression initially resistant to selective serotonin reuptake inhibitor treatment: a follow-up study of the TORDIA sample. J Clin Psychiatry. 2011;72(3):388-396.
23. Bridge JA, Iyengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297(15):1683-1696.
24. Usala T, Clavenna A, Zuddas A, et al. Randomised controlled trials of selective serotonin reuptake inhibitors in treating depression in children and adolescents: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2008;18(1):62-73.
25. March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64(10):1132-1143.
26. Bridge JA, Iyengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297(15):1683-1696.
27. Stone M, Laughren T, Jones ML, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009;339:b2880.-
28. Khan A, Khan S, Kolts R, et al. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry. 2003;160(4):790-792.
29. Simon GE, Savarino J. Suicide attempts among patients starting depression treatment with medications or psychotherapy. Am J Psychiatry. 2007;164(7):1029-1034.
30. March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292(7):807-820.
31. Kratochvil C, Emslie G, Silva S, et al. Acute time to response in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1412-1418.
32. Vitiello B, Rohde P, Silva S, et al. Functioning and quality of life in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1419-1426.
33. Emslie G, Kratochvil C, Vitiello B, et al. Treatment for Adolescents with Depression Study (TADS): safety results. J Am Acad Child Adolesc Psychiatry. 2006;45(12):1440-1455.
34. Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008;299(8):901-913.
35. Joiner TE, Ribeiro JD. Assessment and management of suicidal behavior in teens. Psychiatr Ann. 2011;41(4):220-225.
Discuss this article at www.facebook.com/CurrentPsychiatry
Although depression affects nearly 2% of children (age ≤12) and up to 10% of adolescents (age 13 to 18),1 the disorder often is underdiagnosed and undertreated in pediatric patients.2 Treating depression in young patients is challenging. Only 30% to 40% of depressed children and adolescents who receive evidence-based treatment achieve remission.3 In addition, 50% to 70% of those who initially achieve remission will experience recurrence within 5 years.4 Suicide is the third leading cause of death among children and adolescents, and depression greatly increases the likelihood of suicide.5,6
This article reviews assessing and treating depression in children and adolescents, and how to lower suicide risk in pediatric patients.
Symptoms vary with age
Depressive symptoms vary as a function of the child’s cognitive development and social functioning. Hopelessness and vegetative and motivational symptoms may be more frequent in adolescents than in children.7
In preschool-age children, depression manifests indirectly through somatic symptoms and behavioral disturbances. In this age group, sadness or irritability are sensitive and predominant symptoms of depression.8 In older children, sadness and loss of interest in social activities may indicate depression. In adolescents, feelings of mental and physical weariness, aloneness, disconnectedness, uncertainty, vulnerability, anger, irritability, and ambivalence toward friends suggest a depressive disorder.9
Genetic predisposition to depression, poor family support, dysfunctional parenting, and individual vulnerabilities such as poor self-esteem or emotional dysregulation may increase young patients’ risk for depression.10 Peer and family support may protect against depression. Personal competence stemming from social acceptance and body image satisfaction also may be protective factors. A sense of religious and existential well-being (finding meaning and purpose in life) are significantly associated with lower rates of depression among adolescents.11
A persistent illness
The mean duration of a depressive episode in children and adolescents is 7 to 8 months.12 However, subsyndromal depressive symptoms—as well as relapse and recurrence—are common. Long-term studies indicate that many depressed adolescents experience depressive episodes into adulthood.12 Factors that may predict recurrence in adulthood include:
- severity of depressive episodes
- concurrent psychotic symptoms
- suicidal thoughts
- history of recurrent depressive episodes
- threshold residual symptoms
- recent stressful life events
- adverse family environment
- family history of depression.12
Early symptom onset, greater depression severity, suicidality, presence of comorbid anxiety, disruptive disorders, and an adverse family environment also predict longer recovery time.12 A study of depressed adolescents found that a history of recurrent depression, family history of recurrent depression, personality disorder traits, and (for girls only) conflict with parents predicted recurrence of depression in young adulthood.4Table 1 summarizes factors that affect depression outcomes in children and adolescents.
Table 1
What affects depression outcomes in children and adolescents?
| Factor | Outcomes |
|---|---|
| Age | Pharmacotherapy and CBT are equally effective in younger and older adolescents.a Although age does not affect long-term treatment outcomes, older adolescents (age 18 to 19) with treatment-resistant depression may respond better to a combination of CBT and medicationb |
| Sex | Females are more likely to experience relapse.c However, sex does not influence response to initial treatmentc |
| Socioeconomic status | Adolescents with high socioeconomic status are more likely to respond to CBT |
| Illness characteristics | Severity of depression is the strongest predictor of poor outcome.d-f Patients with moderate depression are more likely to benefit from CBT added to medication.g However, adding CBT to medication did not affect outcomes in adolescents with self-injurious behavior.b,f Suicidal behaviors during treatment are less frequent when CBT is combined with medicationh,i |
| Substance abuse | Patients with substance use disorders are less likely to respond to depression treatmentf and those who continued to abuse substances during treatment are less likely to achieve remission than those who abstainb |
| Cognitive measures | Higher levels of hopelessness are associated with poor outcomes. For adolescents with treatment-resistant depression who experience hopelessness, adding CBT to pharmacotherapy did not provide additional benefit. Some studies have noted that adolescents with cognitive distortions are more likely to benefit from CBT plus pharmacotherapyb |
| Family characteristics/environment | High family stress is associated with poor treatment outcomes.f Experiencing loss and physically dangerous events does not affect depression outcomes. Trauma and history of abuse adversely effect depression treatment outcomes |
CBT: cognitive-behavioral therapy
| |
Assessment strategies
Semi-structured interviews such as the Child and Adolescent Psychiatric Assessment, the Diagnostic Interview for Children and Adolescents, and the Kiddie Schedule for Affective Disorder and Schizophrenia are useful for assessing depression in pediatric patients (Table 2).13-16 These tools can be used to assess depression criteria based on information gathered from several sources. Many instruments can be used to assess and monitor pediatric depression, including the Children’s Depression Inventory, the Reynolds Child Depression Scales and Adolescent Depression Scales, and the Child Depression Rating Scale.
To assess suicide risk in depressed younger patients:
- ask about emotional difficulties
- identify lack of developmental progress
- estimate their level of distress
- detect impairment in functioning
- estimate the level of danger to themselves and others.17
The best way to assess for suicidal ideation is to ask about it directly while interviewing the patient and his or her parents. Simple questions such as “Have you ever thought about killing yourself or wish you were dead?” and “Have you ever done anything on purpose to hurt or kill yourself?” can be effective.10 These questions are best placed in the middle or toward the end of a list of questions about depressive symptoms.
Adolescents may be more likely than adults to disclose information about suicidality on self-reports.6 However, self-assessment suicide scales are not a substitute for clinical assessment because they tend to be oversensitive and non-specific and lack predictive value. A positive response to either of these questions should prompt a more detailed clinical investigation. There is no evidence that asking about suicide risk increases suicidal behavior, even in high-risk youths.
Table 2
Assessing children and adolescents: 3 semi-structured interviews
| Interview | Features |
|---|---|
| Child and Adolescent Psychiatric Assessment13 | For patients age 9 to 17. Assesses symptoms from the past 3 months. Administration time: 1 to 2 hours. Requires minimal interviewer experience. Assesses impairment in multiple areas (family, peers, school, leisure activities) |
| Diagnostic Interview for Children and Adolescents14 | Separate versions for children (age 6 to 12) and adolescents (age 13 to 17). Assesses lifetime psychopathology. Administration time: 1 to 2 hours. Interrater reliability varies (poor to good) |
| Kiddie Schedule for Affective Disorders and Schizophrenia15 | Assesses lifetime and current psychopathology. Administration time: 35 minutes to 2.5 hours. Interrater reliability: fair to excellent16 |
Treatment options
Psychotherapy. Several controlled studies and meta-analyses support the efficacy of cognitive-behavioral therapy (CBT) for mild depression in pediatric patients.18-20 Two recent meta-analyses of CBT studies in depressed adolescents found the mean effect size of CBT was 0.34 to 0.35.19,21 However, a separate analysis found CBT did not have long-term benefits for depressed adolescents, particularly patients with a history of abuse.22
Interpersonal therapy also can be effective in adolescent outpatients with mild to moderate depression. One study found the effect size of psychotherapy was modest (0.36).19
Pharmacotherapy. Two meta-analyses support selective serotonin reuptake inhibitors (SSRIs) for treating mild to moderate depression in children and adolescents. One found 61% of depressed patients age <19 who received an SSRI were “much improved” or “very much improved.”23 Another meta-analysis that compared SSRIs and placebo found fluoxetine was more effective than sertraline or citalopram for depressed adolescents.24 Other studies have shown that for severe depression, the effect size of antidepressants (0.69) is higher than that of placebo (0.39).25 Antidepressants are more effective in adolescents than in children.25
Fluoxetine is the only FDA-approved medication for treating depression in children age ≥8. In 2007 the FDA extended to all antidepressants its “black-box” warning about increased risk of suicidality in patients up to age 24. The results of studies that analyzed data about the safety of antidepressants in children and adolescents have been mixed—some found evidence of increased suicidality with antidepressant use,26,27 whereas others showed no increased risk.28,29Table 3 summarizes steps to minimize the risk of antidepressant-induced suicidality.17
Psychotherapy plus pharmacotherapy. Researchers who compared fluoxetine to CBT and to a combination of the 2 in adolescents with moderate to severe depression found that fluoxetine was most effective in the first 12 weeks of treatment.30 Surprisingly, CBT’s effectiveness was not different from placebo.30 However, studies have shown that combining psychotherapy and medication results in greater symptom improvement,30 faster clinical response,31 improvement of global functioning and quality of life,32 and reduced suicidality.33 At 6 months, the difference in response between medication and psychotherapy was small.25 The Treatment of Resistant Depression in Adolescents study found that for chronic adolescent depression, pharmacotherapy (fluoxetine and venlafaxine) combined with CBT produced a higher response rate than pharmacotherapy alone (54% vs 41%).34
Table 3
Protecting against antidepressant-induced suicidality
| Before initiating antidepressant treatment |
|---|
| Review the patient’s psychiatric history |
| Assess for past suicidal behavior |
| Assess for a family history of mental illness or mood disorders and suicide attempts |
| Screen for unrecognized bipolar spectrum disorders |
| Educate patients and their families to watch for signs of worsening depression or suicidality, and to report such symptoms immediately |
| During antidepressant treatment |
| Pay attention to abrupt changes in symptoms, particularly symptoms that were not part of the patient’s initial presentation |
| Watch for deterioration of symptoms |
| Monitor for emergence of ‘activating’ symptoms (ie, irritability, impulsivity, anxiety, insomnia, agitation, hostility, akathisia, hypomania, or mania) |
| Evaluate the patient’s suicide risk factors, including having a specific plan and/or access to lethal means |
| Consider hospitalization if the patient is at high risk for suicide |
| Source: Reference 17 |
Lowering suicide risk
Up to 60% of adolescents who commit suicide had a depressive disorder. Risk factors for child and adolescent suicide attempts include:
- self-harm behaviors
- psychiatric disorders
- family disturbances
- substance abuse
- physical/sexual abuse.17
How to best manage suicidal youths depends on an adequate assessment of the severity of the patient’s current problems and conflicts and the degree of suicidal intent. Assessment of coping resources, access to support systems, and the attitude of the patient and family toward intervention and follow-up also is important.
Children and adolescents at high risk for suicide—those with a plan or recent suicide attempt with high probability of lethality, stated current intent to kill themselves, or recent suicidal ideation or behavior—may need inpatient psychiatric admission. Although no studies have shown that admitting high-risk suicidal patients prevents suicide, hospitalization often is the safest course of action. Develop ing a comprehensive outpatient treatment plan before discharge is essential. Patients with fewer risk factors, especially those who want help and have social support, hope for the future, and a desire to resolve conflicts, may require only a brief crisis-oriented intervention.
The following recommendations for managing suicidality in children and adolescents are based on clinical experience and have not been empirically validated.
Develop a safety plan to direct the patient’s behavior under various situations. For example, the patient would agree in writing that “If I feel depressed, I will do X, Y, and Z to address it,” or “If I find myself having suicidal thoughts, I will contact ABC.” Having a safety plan lowers the risk of a suicide attempt more than having a suicide contract, which does not give the patient any tools.35
Create a ‘hope box.’ This is a box in which the patient collects mementos and other objects that remind him or her of hope and reasons to live. The patient should be able to access it at all times, so he or she can tap into it during crisis periods to avert suicidal acts.35
Counteract alienation. A sense of social isolation and burdensomeness may be “tipping factors” for suicidal acts when adolescents feel depressed.35 Clinicians should try to help connect patients to meaningful social activities, even in small doses.
Manage overarousal. Overarousal in depressed children and adolescents is manifested as agitation. Insomnia is a clinically modifiable risk factor. Insomnia initially responds well to behavioral interventions such as sleep hygiene, sleep restriction, and stimulus control techniques.35
Related Resources
- National Suicide Prevention Lifeline. 800-273-TALK (8255). www.suicidepreventionlifeline.org.
- Suicide Prevention Resource Center. www.sprc.org.
Drug Brand Names
- Citalopram • Celexa
- Fluoxetine • Prozac
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosures
Drs. Shailesh Jain and Islam report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rakesh Jain is a consultant to or has received research/grant support from Eli Lilly and Company, Merck, Pfizer Inc., Shionogi Pharmaceuticals, and Shire.
Discuss this article at www.facebook.com/CurrentPsychiatry
Although depression affects nearly 2% of children (age ≤12) and up to 10% of adolescents (age 13 to 18),1 the disorder often is underdiagnosed and undertreated in pediatric patients.2 Treating depression in young patients is challenging. Only 30% to 40% of depressed children and adolescents who receive evidence-based treatment achieve remission.3 In addition, 50% to 70% of those who initially achieve remission will experience recurrence within 5 years.4 Suicide is the third leading cause of death among children and adolescents, and depression greatly increases the likelihood of suicide.5,6
This article reviews assessing and treating depression in children and adolescents, and how to lower suicide risk in pediatric patients.
Symptoms vary with age
Depressive symptoms vary as a function of the child’s cognitive development and social functioning. Hopelessness and vegetative and motivational symptoms may be more frequent in adolescents than in children.7
In preschool-age children, depression manifests indirectly through somatic symptoms and behavioral disturbances. In this age group, sadness or irritability are sensitive and predominant symptoms of depression.8 In older children, sadness and loss of interest in social activities may indicate depression. In adolescents, feelings of mental and physical weariness, aloneness, disconnectedness, uncertainty, vulnerability, anger, irritability, and ambivalence toward friends suggest a depressive disorder.9
Genetic predisposition to depression, poor family support, dysfunctional parenting, and individual vulnerabilities such as poor self-esteem or emotional dysregulation may increase young patients’ risk for depression.10 Peer and family support may protect against depression. Personal competence stemming from social acceptance and body image satisfaction also may be protective factors. A sense of religious and existential well-being (finding meaning and purpose in life) are significantly associated with lower rates of depression among adolescents.11
A persistent illness
The mean duration of a depressive episode in children and adolescents is 7 to 8 months.12 However, subsyndromal depressive symptoms—as well as relapse and recurrence—are common. Long-term studies indicate that many depressed adolescents experience depressive episodes into adulthood.12 Factors that may predict recurrence in adulthood include:
- severity of depressive episodes
- concurrent psychotic symptoms
- suicidal thoughts
- history of recurrent depressive episodes
- threshold residual symptoms
- recent stressful life events
- adverse family environment
- family history of depression.12
Early symptom onset, greater depression severity, suicidality, presence of comorbid anxiety, disruptive disorders, and an adverse family environment also predict longer recovery time.12 A study of depressed adolescents found that a history of recurrent depression, family history of recurrent depression, personality disorder traits, and (for girls only) conflict with parents predicted recurrence of depression in young adulthood.4Table 1 summarizes factors that affect depression outcomes in children and adolescents.
Table 1
What affects depression outcomes in children and adolescents?
| Factor | Outcomes |
|---|---|
| Age | Pharmacotherapy and CBT are equally effective in younger and older adolescents.a Although age does not affect long-term treatment outcomes, older adolescents (age 18 to 19) with treatment-resistant depression may respond better to a combination of CBT and medicationb |
| Sex | Females are more likely to experience relapse.c However, sex does not influence response to initial treatmentc |
| Socioeconomic status | Adolescents with high socioeconomic status are more likely to respond to CBT |
| Illness characteristics | Severity of depression is the strongest predictor of poor outcome.d-f Patients with moderate depression are more likely to benefit from CBT added to medication.g However, adding CBT to medication did not affect outcomes in adolescents with self-injurious behavior.b,f Suicidal behaviors during treatment are less frequent when CBT is combined with medicationh,i |
| Substance abuse | Patients with substance use disorders are less likely to respond to depression treatmentf and those who continued to abuse substances during treatment are less likely to achieve remission than those who abstainb |
| Cognitive measures | Higher levels of hopelessness are associated with poor outcomes. For adolescents with treatment-resistant depression who experience hopelessness, adding CBT to pharmacotherapy did not provide additional benefit. Some studies have noted that adolescents with cognitive distortions are more likely to benefit from CBT plus pharmacotherapyb |
| Family characteristics/environment | High family stress is associated with poor treatment outcomes.f Experiencing loss and physically dangerous events does not affect depression outcomes. Trauma and history of abuse adversely effect depression treatment outcomes |
CBT: cognitive-behavioral therapy
| |
Assessment strategies
Semi-structured interviews such as the Child and Adolescent Psychiatric Assessment, the Diagnostic Interview for Children and Adolescents, and the Kiddie Schedule for Affective Disorder and Schizophrenia are useful for assessing depression in pediatric patients (Table 2).13-16 These tools can be used to assess depression criteria based on information gathered from several sources. Many instruments can be used to assess and monitor pediatric depression, including the Children’s Depression Inventory, the Reynolds Child Depression Scales and Adolescent Depression Scales, and the Child Depression Rating Scale.
To assess suicide risk in depressed younger patients:
- ask about emotional difficulties
- identify lack of developmental progress
- estimate their level of distress
- detect impairment in functioning
- estimate the level of danger to themselves and others.17
The best way to assess for suicidal ideation is to ask about it directly while interviewing the patient and his or her parents. Simple questions such as “Have you ever thought about killing yourself or wish you were dead?” and “Have you ever done anything on purpose to hurt or kill yourself?” can be effective.10 These questions are best placed in the middle or toward the end of a list of questions about depressive symptoms.
Adolescents may be more likely than adults to disclose information about suicidality on self-reports.6 However, self-assessment suicide scales are not a substitute for clinical assessment because they tend to be oversensitive and non-specific and lack predictive value. A positive response to either of these questions should prompt a more detailed clinical investigation. There is no evidence that asking about suicide risk increases suicidal behavior, even in high-risk youths.
Table 2
Assessing children and adolescents: 3 semi-structured interviews
| Interview | Features |
|---|---|
| Child and Adolescent Psychiatric Assessment13 | For patients age 9 to 17. Assesses symptoms from the past 3 months. Administration time: 1 to 2 hours. Requires minimal interviewer experience. Assesses impairment in multiple areas (family, peers, school, leisure activities) |
| Diagnostic Interview for Children and Adolescents14 | Separate versions for children (age 6 to 12) and adolescents (age 13 to 17). Assesses lifetime psychopathology. Administration time: 1 to 2 hours. Interrater reliability varies (poor to good) |
| Kiddie Schedule for Affective Disorders and Schizophrenia15 | Assesses lifetime and current psychopathology. Administration time: 35 minutes to 2.5 hours. Interrater reliability: fair to excellent16 |
Treatment options
Psychotherapy. Several controlled studies and meta-analyses support the efficacy of cognitive-behavioral therapy (CBT) for mild depression in pediatric patients.18-20 Two recent meta-analyses of CBT studies in depressed adolescents found the mean effect size of CBT was 0.34 to 0.35.19,21 However, a separate analysis found CBT did not have long-term benefits for depressed adolescents, particularly patients with a history of abuse.22
Interpersonal therapy also can be effective in adolescent outpatients with mild to moderate depression. One study found the effect size of psychotherapy was modest (0.36).19
Pharmacotherapy. Two meta-analyses support selective serotonin reuptake inhibitors (SSRIs) for treating mild to moderate depression in children and adolescents. One found 61% of depressed patients age <19 who received an SSRI were “much improved” or “very much improved.”23 Another meta-analysis that compared SSRIs and placebo found fluoxetine was more effective than sertraline or citalopram for depressed adolescents.24 Other studies have shown that for severe depression, the effect size of antidepressants (0.69) is higher than that of placebo (0.39).25 Antidepressants are more effective in adolescents than in children.25
Fluoxetine is the only FDA-approved medication for treating depression in children age ≥8. In 2007 the FDA extended to all antidepressants its “black-box” warning about increased risk of suicidality in patients up to age 24. The results of studies that analyzed data about the safety of antidepressants in children and adolescents have been mixed—some found evidence of increased suicidality with antidepressant use,26,27 whereas others showed no increased risk.28,29Table 3 summarizes steps to minimize the risk of antidepressant-induced suicidality.17
Psychotherapy plus pharmacotherapy. Researchers who compared fluoxetine to CBT and to a combination of the 2 in adolescents with moderate to severe depression found that fluoxetine was most effective in the first 12 weeks of treatment.30 Surprisingly, CBT’s effectiveness was not different from placebo.30 However, studies have shown that combining psychotherapy and medication results in greater symptom improvement,30 faster clinical response,31 improvement of global functioning and quality of life,32 and reduced suicidality.33 At 6 months, the difference in response between medication and psychotherapy was small.25 The Treatment of Resistant Depression in Adolescents study found that for chronic adolescent depression, pharmacotherapy (fluoxetine and venlafaxine) combined with CBT produced a higher response rate than pharmacotherapy alone (54% vs 41%).34
Table 3
Protecting against antidepressant-induced suicidality
| Before initiating antidepressant treatment |
|---|
| Review the patient’s psychiatric history |
| Assess for past suicidal behavior |
| Assess for a family history of mental illness or mood disorders and suicide attempts |
| Screen for unrecognized bipolar spectrum disorders |
| Educate patients and their families to watch for signs of worsening depression or suicidality, and to report such symptoms immediately |
| During antidepressant treatment |
| Pay attention to abrupt changes in symptoms, particularly symptoms that were not part of the patient’s initial presentation |
| Watch for deterioration of symptoms |
| Monitor for emergence of ‘activating’ symptoms (ie, irritability, impulsivity, anxiety, insomnia, agitation, hostility, akathisia, hypomania, or mania) |
| Evaluate the patient’s suicide risk factors, including having a specific plan and/or access to lethal means |
| Consider hospitalization if the patient is at high risk for suicide |
| Source: Reference 17 |
Lowering suicide risk
Up to 60% of adolescents who commit suicide had a depressive disorder. Risk factors for child and adolescent suicide attempts include:
- self-harm behaviors
- psychiatric disorders
- family disturbances
- substance abuse
- physical/sexual abuse.17
How to best manage suicidal youths depends on an adequate assessment of the severity of the patient’s current problems and conflicts and the degree of suicidal intent. Assessment of coping resources, access to support systems, and the attitude of the patient and family toward intervention and follow-up also is important.
Children and adolescents at high risk for suicide—those with a plan or recent suicide attempt with high probability of lethality, stated current intent to kill themselves, or recent suicidal ideation or behavior—may need inpatient psychiatric admission. Although no studies have shown that admitting high-risk suicidal patients prevents suicide, hospitalization often is the safest course of action. Develop ing a comprehensive outpatient treatment plan before discharge is essential. Patients with fewer risk factors, especially those who want help and have social support, hope for the future, and a desire to resolve conflicts, may require only a brief crisis-oriented intervention.
The following recommendations for managing suicidality in children and adolescents are based on clinical experience and have not been empirically validated.
Develop a safety plan to direct the patient’s behavior under various situations. For example, the patient would agree in writing that “If I feel depressed, I will do X, Y, and Z to address it,” or “If I find myself having suicidal thoughts, I will contact ABC.” Having a safety plan lowers the risk of a suicide attempt more than having a suicide contract, which does not give the patient any tools.35
Create a ‘hope box.’ This is a box in which the patient collects mementos and other objects that remind him or her of hope and reasons to live. The patient should be able to access it at all times, so he or she can tap into it during crisis periods to avert suicidal acts.35
Counteract alienation. A sense of social isolation and burdensomeness may be “tipping factors” for suicidal acts when adolescents feel depressed.35 Clinicians should try to help connect patients to meaningful social activities, even in small doses.
Manage overarousal. Overarousal in depressed children and adolescents is manifested as agitation. Insomnia is a clinically modifiable risk factor. Insomnia initially responds well to behavioral interventions such as sleep hygiene, sleep restriction, and stimulus control techniques.35
Related Resources
- National Suicide Prevention Lifeline. 800-273-TALK (8255). www.suicidepreventionlifeline.org.
- Suicide Prevention Resource Center. www.sprc.org.
Drug Brand Names
- Citalopram • Celexa
- Fluoxetine • Prozac
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosures
Drs. Shailesh Jain and Islam report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rakesh Jain is a consultant to or has received research/grant support from Eli Lilly and Company, Merck, Pfizer Inc., Shionogi Pharmaceuticals, and Shire.
1. Birmaher B, Brent D. AACAP Work Group on Quality Issues, et al. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503-1526.
2. Lewinsohn PM, Clarke GN, Seeley JR, et al. Major depression in community adolescents: age at onset, episode duration, and time to recurrence. J Am Acad Child Adolesc Psychiatry. 1994;33(6):809-818.
3. Emslie GJ, Kennard BD, Mayes TL. Predictors of treatment response in adolescent depression. Pediatr Ann. 2011;40(6):300-306.
4. Lewinsohn PM, Rohde P, Seeley JR, et al. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry. 2000;157(10):1584-1591.
5. Foley DL, Goldston DB, Costello EJ, et al. Proximal psychiatric risk factors for suicidality in youth: the Great Smoky Mountains Study. Arch Gen Psychiatry. 2006;63(9):1017-1024.
6. Gould MS, Greenberg T, Velting DM, et al. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386-405.
7. Weiss B, Garber J. Developmental differences in the phenomenology of depression. Dev Psychopathol. 2003;15(2):403-430.
8. Calles JL, Jr. Depression in children and adolescents. Prim Care. 2007;34(2):243-258abstract vi.
9. Farmer TJ. The experience of major depression: adolescents’ perspectives. Issues Ment Health Nurs. 2002;23(6):567-585.
10. Zalsman G, Brent DA, Weersing VR. Depressive disorders in childhood and adolescence: an overview: epidemiology clinical manifestation and risk factors. Child Adolesc Psychiatr Clin N Am. 2006;15(4):827-841, vii.
11. Cotton S, Larkin E, Hoopes A, et al. The impact of adolescent spirituality on depressive symptoms and health risk behaviors. J Adolesc Health. 2005;36(6):529.-
12. Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child Adolesc Psychiatr Clin N Am. 2002;11(3):619-637, x.
13. Angold A, Costello EJ. A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C). Psychol Med. 1995;25(4):755-762.
14. Reich W. Diagnostic interview for children and adolescents (DICA). J Am Acad Child Adolesc Psychiatry. 2000;39(1):59-66.
15. Puig-Antich J, Lukens E, Brent D. Psychosocial schedule for school age children - revised. Pittsburgh PA: Western Psychiatric Institute and Clinic; 1986.
16. Ambrosini PJ. Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS). J Am Acad Child Adolesc Psychiatry. 2000;39(1):49-58.
17. Dodig-Curković K, Curković M, Radić J, et al. Suicidal behavior and suicide among children and adolescents-risk factors and epidemiological characteristics. Coll Antropol. 2010;34(2):771-777.
18. Harrington R, Whittaker J, Shoebridge P, et al. Systematic review of efficacy of cognitive behaviour therapies in childhood and adolescent depressive disorder. BMJ. 1998;316(7144):1559-1563.
19. Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychol Bull. 2006;132(1):132-149.
20. Mufson L, Dorta KP, Wickramaratne P, et al. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry. 2004;61(6):577-584.
21. Klein JB, Jacobs RH, Reinecke MA. Cognitive-behavioral therapy for adolescent depression: a meta-analytic investigation of changes in effect-size estimates. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1403-1413.
22. Vitiello B, Emslie G, Clarke G, et al. Long-term outcome of adolescent depression initially resistant to selective serotonin reuptake inhibitor treatment: a follow-up study of the TORDIA sample. J Clin Psychiatry. 2011;72(3):388-396.
23. Bridge JA, Iyengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297(15):1683-1696.
24. Usala T, Clavenna A, Zuddas A, et al. Randomised controlled trials of selective serotonin reuptake inhibitors in treating depression in children and adolescents: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2008;18(1):62-73.
25. March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64(10):1132-1143.
26. Bridge JA, Iyengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297(15):1683-1696.
27. Stone M, Laughren T, Jones ML, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009;339:b2880.-
28. Khan A, Khan S, Kolts R, et al. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry. 2003;160(4):790-792.
29. Simon GE, Savarino J. Suicide attempts among patients starting depression treatment with medications or psychotherapy. Am J Psychiatry. 2007;164(7):1029-1034.
30. March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292(7):807-820.
31. Kratochvil C, Emslie G, Silva S, et al. Acute time to response in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1412-1418.
32. Vitiello B, Rohde P, Silva S, et al. Functioning and quality of life in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1419-1426.
33. Emslie G, Kratochvil C, Vitiello B, et al. Treatment for Adolescents with Depression Study (TADS): safety results. J Am Acad Child Adolesc Psychiatry. 2006;45(12):1440-1455.
34. Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008;299(8):901-913.
35. Joiner TE, Ribeiro JD. Assessment and management of suicidal behavior in teens. Psychiatr Ann. 2011;41(4):220-225.
1. Birmaher B, Brent D. AACAP Work Group on Quality Issues, et al. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1503-1526.
2. Lewinsohn PM, Clarke GN, Seeley JR, et al. Major depression in community adolescents: age at onset, episode duration, and time to recurrence. J Am Acad Child Adolesc Psychiatry. 1994;33(6):809-818.
3. Emslie GJ, Kennard BD, Mayes TL. Predictors of treatment response in adolescent depression. Pediatr Ann. 2011;40(6):300-306.
4. Lewinsohn PM, Rohde P, Seeley JR, et al. Natural course of adolescent major depressive disorder in a community sample: predictors of recurrence in young adults. Am J Psychiatry. 2000;157(10):1584-1591.
5. Foley DL, Goldston DB, Costello EJ, et al. Proximal psychiatric risk factors for suicidality in youth: the Great Smoky Mountains Study. Arch Gen Psychiatry. 2006;63(9):1017-1024.
6. Gould MS, Greenberg T, Velting DM, et al. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386-405.
7. Weiss B, Garber J. Developmental differences in the phenomenology of depression. Dev Psychopathol. 2003;15(2):403-430.
8. Calles JL, Jr. Depression in children and adolescents. Prim Care. 2007;34(2):243-258abstract vi.
9. Farmer TJ. The experience of major depression: adolescents’ perspectives. Issues Ment Health Nurs. 2002;23(6):567-585.
10. Zalsman G, Brent DA, Weersing VR. Depressive disorders in childhood and adolescence: an overview: epidemiology clinical manifestation and risk factors. Child Adolesc Psychiatr Clin N Am. 2006;15(4):827-841, vii.
11. Cotton S, Larkin E, Hoopes A, et al. The impact of adolescent spirituality on depressive symptoms and health risk behaviors. J Adolesc Health. 2005;36(6):529.-
12. Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child Adolesc Psychiatr Clin N Am. 2002;11(3):619-637, x.
13. Angold A, Costello EJ. A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C). Psychol Med. 1995;25(4):755-762.
14. Reich W. Diagnostic interview for children and adolescents (DICA). J Am Acad Child Adolesc Psychiatry. 2000;39(1):59-66.
15. Puig-Antich J, Lukens E, Brent D. Psychosocial schedule for school age children - revised. Pittsburgh PA: Western Psychiatric Institute and Clinic; 1986.
16. Ambrosini PJ. Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS). J Am Acad Child Adolesc Psychiatry. 2000;39(1):49-58.
17. Dodig-Curković K, Curković M, Radić J, et al. Suicidal behavior and suicide among children and adolescents-risk factors and epidemiological characteristics. Coll Antropol. 2010;34(2):771-777.
18. Harrington R, Whittaker J, Shoebridge P, et al. Systematic review of efficacy of cognitive behaviour therapies in childhood and adolescent depressive disorder. BMJ. 1998;316(7144):1559-1563.
19. Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychol Bull. 2006;132(1):132-149.
20. Mufson L, Dorta KP, Wickramaratne P, et al. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry. 2004;61(6):577-584.
21. Klein JB, Jacobs RH, Reinecke MA. Cognitive-behavioral therapy for adolescent depression: a meta-analytic investigation of changes in effect-size estimates. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1403-1413.
22. Vitiello B, Emslie G, Clarke G, et al. Long-term outcome of adolescent depression initially resistant to selective serotonin reuptake inhibitor treatment: a follow-up study of the TORDIA sample. J Clin Psychiatry. 2011;72(3):388-396.
23. Bridge JA, Iyengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297(15):1683-1696.
24. Usala T, Clavenna A, Zuddas A, et al. Randomised controlled trials of selective serotonin reuptake inhibitors in treating depression in children and adolescents: a systematic review and meta-analysis. Eur Neuropsychopharmacol. 2008;18(1):62-73.
25. March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64(10):1132-1143.
26. Bridge JA, Iyengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007;297(15):1683-1696.
27. Stone M, Laughren T, Jones ML, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ. 2009;339:b2880.-
28. Khan A, Khan S, Kolts R, et al. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry. 2003;160(4):790-792.
29. Simon GE, Savarino J. Suicide attempts among patients starting depression treatment with medications or psychotherapy. Am J Psychiatry. 2007;164(7):1029-1034.
30. March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292(7):807-820.
31. Kratochvil C, Emslie G, Silva S, et al. Acute time to response in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1412-1418.
32. Vitiello B, Rohde P, Silva S, et al. Functioning and quality of life in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1419-1426.
33. Emslie G, Kratochvil C, Vitiello B, et al. Treatment for Adolescents with Depression Study (TADS): safety results. J Am Acad Child Adolesc Psychiatry. 2006;45(12):1440-1455.
34. Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008;299(8):901-913.
35. Joiner TE, Ribeiro JD. Assessment and management of suicidal behavior in teens. Psychiatr Ann. 2011;41(4):220-225.
Psychostimulants and college students: 7 steps to prevent misuse
Discuss this article at www.facebook.com/CurrentPsychiatry
In a survey of 115 college students taking medication for attention-deficit/hyperactivity disorder (ADHD), 31% reported having taken their drugs more frequently or at a higher dose than prescribed, or used someone else’s medication since beginning college.1 Fifty-six percent reported being asked to give or sell their medication in the past 6 months; 26% of those solicited gave or sold their medication to a peer.1 The 3 most frequently reported reasons for misusing ADHD medications centered on studying: to improve concentration, to lengthen study time, and to feel less restless while studying.1
Although treating ADHD with first-line stimulants may reduce the incidence of substance use disorders,2,3 monitor patients closely to ensure therapeutic drugs are not being misused or abused.
- Use screening tools such as the CRAFFT test4 for adolescents and the 5-question RAFFT test for adults.5 Also, consider toxicology screenings.
- Consider extended-release formulations, which can reduce recreational stimulant use because subjective likeability is more strongly influenced by the drug delivery rate than by plasma concentration.
- Consider other medications/formulas such as a transdermal patch delivery of methylphenidate or prodrug formulations such as lisdexamfetamine, which is gut enzyme-dependent to hydrolyze into lysine and d-amphetamine. Also, consider nonstimulants such as atomoxetine, bupropion, or tricyclic antidepressants.
- Rule out mood disorders, especially depression, which may be driving the urge to get “high.”
- Involve family members or other forms of supervision, who may be able to better monitor medications.
- Improve physician/patient communication because active physician involvement and better patient communication about treatment-related issues is better for all involved.
- Provide triplicate prescriptions in person to avoid “prescriptions lost in the mail,” and keep a log of all prescriptions you dispense.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
2. Biederman J, Monuteaux MC, Spencer T, et al. Stimulant therapy and risk for subsequent substance use disorders in male adults with ADHD: a naturalistic controlled 10-year follow-up study. Am J Psychiatry. 2008;165(5):597-603.
3. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179-185.
4. The Center for Adolescent Substance Abuse Research. For teens. http://www.ceasar-boston.org/teens/test.php. Accessed January 19 2012.
5. Bastiaens L, Riccardi K, Sakhrani D. The RAFFT as a screening tool for adult substance use disorders. Am J Drug Alcohol Abuse. 2002;28(4):681-691.
Discuss this article at www.facebook.com/CurrentPsychiatry
In a survey of 115 college students taking medication for attention-deficit/hyperactivity disorder (ADHD), 31% reported having taken their drugs more frequently or at a higher dose than prescribed, or used someone else’s medication since beginning college.1 Fifty-six percent reported being asked to give or sell their medication in the past 6 months; 26% of those solicited gave or sold their medication to a peer.1 The 3 most frequently reported reasons for misusing ADHD medications centered on studying: to improve concentration, to lengthen study time, and to feel less restless while studying.1
Although treating ADHD with first-line stimulants may reduce the incidence of substance use disorders,2,3 monitor patients closely to ensure therapeutic drugs are not being misused or abused.
- Use screening tools such as the CRAFFT test4 for adolescents and the 5-question RAFFT test for adults.5 Also, consider toxicology screenings.
- Consider extended-release formulations, which can reduce recreational stimulant use because subjective likeability is more strongly influenced by the drug delivery rate than by plasma concentration.
- Consider other medications/formulas such as a transdermal patch delivery of methylphenidate or prodrug formulations such as lisdexamfetamine, which is gut enzyme-dependent to hydrolyze into lysine and d-amphetamine. Also, consider nonstimulants such as atomoxetine, bupropion, or tricyclic antidepressants.
- Rule out mood disorders, especially depression, which may be driving the urge to get “high.”
- Involve family members or other forms of supervision, who may be able to better monitor medications.
- Improve physician/patient communication because active physician involvement and better patient communication about treatment-related issues is better for all involved.
- Provide triplicate prescriptions in person to avoid “prescriptions lost in the mail,” and keep a log of all prescriptions you dispense.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
In a survey of 115 college students taking medication for attention-deficit/hyperactivity disorder (ADHD), 31% reported having taken their drugs more frequently or at a higher dose than prescribed, or used someone else’s medication since beginning college.1 Fifty-six percent reported being asked to give or sell their medication in the past 6 months; 26% of those solicited gave or sold their medication to a peer.1 The 3 most frequently reported reasons for misusing ADHD medications centered on studying: to improve concentration, to lengthen study time, and to feel less restless while studying.1
Although treating ADHD with first-line stimulants may reduce the incidence of substance use disorders,2,3 monitor patients closely to ensure therapeutic drugs are not being misused or abused.
- Use screening tools such as the CRAFFT test4 for adolescents and the 5-question RAFFT test for adults.5 Also, consider toxicology screenings.
- Consider extended-release formulations, which can reduce recreational stimulant use because subjective likeability is more strongly influenced by the drug delivery rate than by plasma concentration.
- Consider other medications/formulas such as a transdermal patch delivery of methylphenidate or prodrug formulations such as lisdexamfetamine, which is gut enzyme-dependent to hydrolyze into lysine and d-amphetamine. Also, consider nonstimulants such as atomoxetine, bupropion, or tricyclic antidepressants.
- Rule out mood disorders, especially depression, which may be driving the urge to get “high.”
- Involve family members or other forms of supervision, who may be able to better monitor medications.
- Improve physician/patient communication because active physician involvement and better patient communication about treatment-related issues is better for all involved.
- Provide triplicate prescriptions in person to avoid “prescriptions lost in the mail,” and keep a log of all prescriptions you dispense.
Disclosure
Dr. Jain reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
2. Biederman J, Monuteaux MC, Spencer T, et al. Stimulant therapy and risk for subsequent substance use disorders in male adults with ADHD: a naturalistic controlled 10-year follow-up study. Am J Psychiatry. 2008;165(5):597-603.
3. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179-185.
4. The Center for Adolescent Substance Abuse Research. For teens. http://www.ceasar-boston.org/teens/test.php. Accessed January 19 2012.
5. Bastiaens L, Riccardi K, Sakhrani D. The RAFFT as a screening tool for adult substance use disorders. Am J Drug Alcohol Abuse. 2002;28(4):681-691.
1. Rabiner DL, Anastopoulos AD, Costello EJ, et al. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144-153.
2. Biederman J, Monuteaux MC, Spencer T, et al. Stimulant therapy and risk for subsequent substance use disorders in male adults with ADHD: a naturalistic controlled 10-year follow-up study. Am J Psychiatry. 2008;165(5):597-603.
3. Wilens TE, Faraone SV, Biederman J, et al. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179-185.
4. The Center for Adolescent Substance Abuse Research. For teens. http://www.ceasar-boston.org/teens/test.php. Accessed January 19 2012.
5. Bastiaens L, Riccardi K, Sakhrani D. The RAFFT as a screening tool for adult substance use disorders. Am J Drug Alcohol Abuse. 2002;28(4):681-691.