A dental infection was the cause of a patient’s persistent sinus infection.
A 55-year-old man who had experienced discolored nasal drainage and mucus plugs in the right side of his nose for 5 years was referred to the ear, nose, and throat clinic. A computerized tomography (CT) scan showed opacification of the right ethmoid and maxillary sinuses and periapical radiolucency in the first and second right maxillary molars (Figure 1).
On physical examination, extensive decay was noted in the teeth corresponding to the periapical lesions. Endoscopic evaluation of the nose revealed mucosal swelling in the right middle meatus and pus draining from the right maxillary sinus ostium.
The patient was treated with antibiotics (amoxicillin and clavulanate; moxifloxacin) and nasal rinses but failed to improve.
As a result, the patient underwent endoscopic sinus surgery. Postoperatively, the patient’s symptoms recurred, and the maxillary sinus was filled with pus. A repeat CT scan showed swelling of the maxillary sinus mucosa (Figure 2, arrow B).
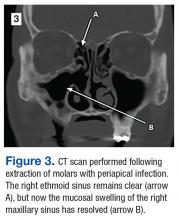
The maxillary molars were considered the source of the persistent sinus infection, and the patient was referred to oral surgery for extraction. Three months after oral surgery, the extraction sites were completely healed, and the right maxillary sinus appeared free of disease endoscopically (Figure 3).
Dental infections should be considered a source of maxillary sinus disease especially in cases of rhinosinusitis that do not resolve with standard medical and surgical management.1,2
Author and Disclosure Information
Dr. Brown is a physician in the department of surgery, division of ear, nose, and throat, at Carl T. Hayden VA Medical Center in Phoenix, Arizona.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Issue
Federal Practitioner - 34(3)
Author and Disclosure Information
Dr. Brown is a physician in the department of surgery, division of ear, nose, and throat, at Carl T. Hayden VA Medical Center in Phoenix, Arizona.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Author and Disclosure Information
Dr. Brown is a physician in the department of surgery, division of ear, nose, and throat, at Carl T. Hayden VA Medical Center in Phoenix, Arizona.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
A dental infection was the cause of a patient’s persistent sinus infection.
A dental infection was the cause of a patient’s persistent sinus infection.
A 55-year-old man who had experienced discolored nasal drainage and mucus plugs in the right side of his nose for 5 years was referred to the ear, nose, and throat clinic. A computerized tomography (CT) scan showed opacification of the right ethmoid and maxillary sinuses and periapical radiolucency in the first and second right maxillary molars (Figure 1).
On physical examination, extensive decay was noted in the teeth corresponding to the periapical lesions. Endoscopic evaluation of the nose revealed mucosal swelling in the right middle meatus and pus draining from the right maxillary sinus ostium.
The patient was treated with antibiotics (amoxicillin and clavulanate; moxifloxacin) and nasal rinses but failed to improve.
As a result, the patient underwent endoscopic sinus surgery. Postoperatively, the patient’s symptoms recurred, and the maxillary sinus was filled with pus. A repeat CT scan showed swelling of the maxillary sinus mucosa (Figure 2, arrow B).
The maxillary molars were considered the source of the persistent sinus infection, and the patient was referred to oral surgery for extraction. Three months after oral surgery, the extraction sites were completely healed, and the right maxillary sinus appeared free of disease endoscopically (Figure 3).
Dental infections should be considered a source of maxillary sinus disease especially in cases of rhinosinusitis that do not resolve with standard medical and surgical management.1,2
A 55-year-old man who had experienced discolored nasal drainage and mucus plugs in the right side of his nose for 5 years was referred to the ear, nose, and throat clinic. A computerized tomography (CT) scan showed opacification of the right ethmoid and maxillary sinuses and periapical radiolucency in the first and second right maxillary molars (Figure 1).
On physical examination, extensive decay was noted in the teeth corresponding to the periapical lesions. Endoscopic evaluation of the nose revealed mucosal swelling in the right middle meatus and pus draining from the right maxillary sinus ostium.
The patient was treated with antibiotics (amoxicillin and clavulanate; moxifloxacin) and nasal rinses but failed to improve.
As a result, the patient underwent endoscopic sinus surgery. Postoperatively, the patient’s symptoms recurred, and the maxillary sinus was filled with pus. A repeat CT scan showed swelling of the maxillary sinus mucosa (Figure 2, arrow B).
The maxillary molars were considered the source of the persistent sinus infection, and the patient was referred to oral surgery for extraction. Three months after oral surgery, the extraction sites were completely healed, and the right maxillary sinus appeared free of disease endoscopically (Figure 3).
Dental infections should be considered a source of maxillary sinus disease especially in cases of rhinosinusitis that do not resolve with standard medical and surgical management.1,2
Issue
Federal Practitioner - 34(3)
Issue
Federal Practitioner - 34(3)
Content Gating
No Gating (article Unlocked/Free)
Consolidated Pubs: Do Not Show Source Publication Logo