User login
Real-world data for immunotherapy-treated NSCLC found robust
Real-world outcome data from patients with advanced non–small cell lung cancer (NSCLC) treated with immunotherapy are robust enough to use for regulatory and payer decisions, suggests an analysis of six data sets and more than 13,000 patients.
“Study of routinely collected health care data is increasingly important for various stakeholders who are interested in better understanding particular patient populations, evaluating drug safety in the postmarketing setting, measuring health care use and clinical outcomes, performing comparative effectiveness research, and optimizing drug pricing models,” noted lead investigator Mark Stewart, PhD, Friends of Cancer Research, Washington, and coinvestigators. “However, before [real-world data] finds widespread use as an adjunct to – or in unique settings, an alternative for – [randomized clinical trials], the validity of readily extractable clinical outcomes measures – real-world endpoints – must be established.”
The investigators undertook a retrospective cohort study using administrative claims and electronic health records for patients with advanced NSCLC treated with inhibitors of programmed death 1 (PD-1) or programmed death ligand 1 (PD-L1) between January 2011 and October 2017 in real-world settings. They analyzed six data sets having 269 to 6,924 patients each (13,639 patients total).
Results reported in JCO Clinical Cancer Informatics showed that the real-world intermediate endpoints of time to treatment discontinuation and time to next treatment were moderately to highly correlated with real-world overall survival (Spearman’s rank correlation coefficient, 0.36 to 0.89, with most values 0.60 or higher).
In real-world settings, the 1-year rate of overall survival after starting immunotherapy ranged from 40% to 57%. Real-world data and trial data were similar with respect to median overall survival (8.6-13.5 months vs. 9.2-12.7 months).
The data sources used for the study have been extensively used for research and are curated on an ongoing basis to ensure the data are accurate and as complete as possible, Dr. Stewart and coinvestigators noted.
“These findings demonstrate that real-world endpoints are generally consistent with each other and with outcomes observed in randomized clinical trials, which substantiates the potential validity of real-world data to support regulatory and payer decision-making,” they maintained. “Differences observed likely reflect true differences between real-world and protocol-driven practices.
“Additional studies are needed to further support the use of [real-world evidence] and inform the development of regulatory guidance,” the investigators concluded. “Standardizing definitions for real-world endpoints and determining appropriate analytic methodologies for [real-world data] will be critical for broader adoption of real-world studies and will provide greater confidence in associated findings. As more refined and standardized approaches are developed that incorporate deep clinical and bioinformatics expertise, the greater the utility of [real-world data] will be for detecting even small, but important, differences in treatment effects.”
Dr. Stewart disclosed no conflicts of interest. The study was supported in part by the National Cancer Institute and the Patient Centered Outcomes Research Institute.
SOURCE: Stewart M et al. JCO Clin Cancer Inform. 2019 July 23. doi: 10.1200/CCI.18.00155.
Real-world outcome data from patients with advanced non–small cell lung cancer (NSCLC) treated with immunotherapy are robust enough to use for regulatory and payer decisions, suggests an analysis of six data sets and more than 13,000 patients.
“Study of routinely collected health care data is increasingly important for various stakeholders who are interested in better understanding particular patient populations, evaluating drug safety in the postmarketing setting, measuring health care use and clinical outcomes, performing comparative effectiveness research, and optimizing drug pricing models,” noted lead investigator Mark Stewart, PhD, Friends of Cancer Research, Washington, and coinvestigators. “However, before [real-world data] finds widespread use as an adjunct to – or in unique settings, an alternative for – [randomized clinical trials], the validity of readily extractable clinical outcomes measures – real-world endpoints – must be established.”
The investigators undertook a retrospective cohort study using administrative claims and electronic health records for patients with advanced NSCLC treated with inhibitors of programmed death 1 (PD-1) or programmed death ligand 1 (PD-L1) between January 2011 and October 2017 in real-world settings. They analyzed six data sets having 269 to 6,924 patients each (13,639 patients total).
Results reported in JCO Clinical Cancer Informatics showed that the real-world intermediate endpoints of time to treatment discontinuation and time to next treatment were moderately to highly correlated with real-world overall survival (Spearman’s rank correlation coefficient, 0.36 to 0.89, with most values 0.60 or higher).
In real-world settings, the 1-year rate of overall survival after starting immunotherapy ranged from 40% to 57%. Real-world data and trial data were similar with respect to median overall survival (8.6-13.5 months vs. 9.2-12.7 months).
The data sources used for the study have been extensively used for research and are curated on an ongoing basis to ensure the data are accurate and as complete as possible, Dr. Stewart and coinvestigators noted.
“These findings demonstrate that real-world endpoints are generally consistent with each other and with outcomes observed in randomized clinical trials, which substantiates the potential validity of real-world data to support regulatory and payer decision-making,” they maintained. “Differences observed likely reflect true differences between real-world and protocol-driven practices.
“Additional studies are needed to further support the use of [real-world evidence] and inform the development of regulatory guidance,” the investigators concluded. “Standardizing definitions for real-world endpoints and determining appropriate analytic methodologies for [real-world data] will be critical for broader adoption of real-world studies and will provide greater confidence in associated findings. As more refined and standardized approaches are developed that incorporate deep clinical and bioinformatics expertise, the greater the utility of [real-world data] will be for detecting even small, but important, differences in treatment effects.”
Dr. Stewart disclosed no conflicts of interest. The study was supported in part by the National Cancer Institute and the Patient Centered Outcomes Research Institute.
SOURCE: Stewart M et al. JCO Clin Cancer Inform. 2019 July 23. doi: 10.1200/CCI.18.00155.
Real-world outcome data from patients with advanced non–small cell lung cancer (NSCLC) treated with immunotherapy are robust enough to use for regulatory and payer decisions, suggests an analysis of six data sets and more than 13,000 patients.
“Study of routinely collected health care data is increasingly important for various stakeholders who are interested in better understanding particular patient populations, evaluating drug safety in the postmarketing setting, measuring health care use and clinical outcomes, performing comparative effectiveness research, and optimizing drug pricing models,” noted lead investigator Mark Stewart, PhD, Friends of Cancer Research, Washington, and coinvestigators. “However, before [real-world data] finds widespread use as an adjunct to – or in unique settings, an alternative for – [randomized clinical trials], the validity of readily extractable clinical outcomes measures – real-world endpoints – must be established.”
The investigators undertook a retrospective cohort study using administrative claims and electronic health records for patients with advanced NSCLC treated with inhibitors of programmed death 1 (PD-1) or programmed death ligand 1 (PD-L1) between January 2011 and October 2017 in real-world settings. They analyzed six data sets having 269 to 6,924 patients each (13,639 patients total).
Results reported in JCO Clinical Cancer Informatics showed that the real-world intermediate endpoints of time to treatment discontinuation and time to next treatment were moderately to highly correlated with real-world overall survival (Spearman’s rank correlation coefficient, 0.36 to 0.89, with most values 0.60 or higher).
In real-world settings, the 1-year rate of overall survival after starting immunotherapy ranged from 40% to 57%. Real-world data and trial data were similar with respect to median overall survival (8.6-13.5 months vs. 9.2-12.7 months).
The data sources used for the study have been extensively used for research and are curated on an ongoing basis to ensure the data are accurate and as complete as possible, Dr. Stewart and coinvestigators noted.
“These findings demonstrate that real-world endpoints are generally consistent with each other and with outcomes observed in randomized clinical trials, which substantiates the potential validity of real-world data to support regulatory and payer decision-making,” they maintained. “Differences observed likely reflect true differences between real-world and protocol-driven practices.
“Additional studies are needed to further support the use of [real-world evidence] and inform the development of regulatory guidance,” the investigators concluded. “Standardizing definitions for real-world endpoints and determining appropriate analytic methodologies for [real-world data] will be critical for broader adoption of real-world studies and will provide greater confidence in associated findings. As more refined and standardized approaches are developed that incorporate deep clinical and bioinformatics expertise, the greater the utility of [real-world data] will be for detecting even small, but important, differences in treatment effects.”
Dr. Stewart disclosed no conflicts of interest. The study was supported in part by the National Cancer Institute and the Patient Centered Outcomes Research Institute.
SOURCE: Stewart M et al. JCO Clin Cancer Inform. 2019 July 23. doi: 10.1200/CCI.18.00155.
FROM JCO CLINICAL CANCER INFORMATICS
Erdafitinib is efficacious in FGFR-altered urothelial carcinoma
Erdafitinib, an oral pan–fibroblast growth factor receptor (FGFR) tyrosine kinase inhibitor, is efficacious when used to treat urothelial cancer harboring FGFR genetic alterations, although dose adjustments are commonly needed, suggests a multicenter phase 2 trial.
“Mutations and fusions in FGFR2/3 are common in patients with urothelial carcinoma, particularly in the luminal I subtype, and can cause constitutive FGFR signaling that may contribute to carcinogenesis,” write Yohann Loriot, MD, of Gustave Roussy, Université Paris-Sud and Université Paris-Saclay, in Villejuif, France, and coinvestigators. Up to 20% of patients with advanced disease and fully 37% of those with upper-tract tumors have alterations in these genes. “ Thus, FGFR inhibition may be particularly appropriate in patients with luminal I subtype disease, in which immunotherapeutic approaches may be less effective,” they noted.
In the trial, 99 patients with pretreated locally advanced and unresectable or metastatic urothelial carcinoma having FGFR alterations were given single-agent, open-label erdafitinib (Balversa) for a median of five cycles. The drug was recently granted accelerated approval by the Food and Drug Administration for this indication.
The rate of confirmed response according to investigator assessment was 40% (3% of patients had a complete response and 37% had a partial response), based on trial results reported in the New England Journal of Medicine. The response rate was 59% among the subset who had previously received immunotherapy.
With a median follow-up of 11.0 months, the median duration of progression-free survival was 5.5 months, and the median duration of overall survival was 13.8 months.
Fully 46% of patients experienced a grade 3 or higher treatment-related adverse event, most commonly hyponatremia (11%), stomatitis (10%), and asthenia (7%). Nearly 56% of the trial population as a whole required a dose reduction. However, only 13% of patients stopped treatment because of an adverse event, and there were no treatment-related deaths.
“This study met its primary objective,” Dr. Loriot and coinvestigators concluded. “These findings showed that among patients with locally advanced and unresectable or metastatic urothelial carcinoma with certain FGFR alterations, erdafitinib had promising antitumor activity.”
“The response to erdafitinib was rapid and independent of the number of previous courses and types of therapy, the presence of visceral metastasis, or tumor location,” they wrote. In addition, the efficacy appears to be better than that achieved previously with chemotherapy, immune checkpoint inhibitors, and antibody-drug conjugates.
The trial was funded by Janssen Research and Development. Dr. Loriot reports grants and personal fees from Janssen, during the conduct of the study.
SOURCE: Loriot Y et al. N Engl J Med. 2019;381:338-348. doi: 10.1056/NEJMoa1817323.
Erdafitinib, an oral pan–fibroblast growth factor receptor (FGFR) tyrosine kinase inhibitor, is efficacious when used to treat urothelial cancer harboring FGFR genetic alterations, although dose adjustments are commonly needed, suggests a multicenter phase 2 trial.
“Mutations and fusions in FGFR2/3 are common in patients with urothelial carcinoma, particularly in the luminal I subtype, and can cause constitutive FGFR signaling that may contribute to carcinogenesis,” write Yohann Loriot, MD, of Gustave Roussy, Université Paris-Sud and Université Paris-Saclay, in Villejuif, France, and coinvestigators. Up to 20% of patients with advanced disease and fully 37% of those with upper-tract tumors have alterations in these genes. “ Thus, FGFR inhibition may be particularly appropriate in patients with luminal I subtype disease, in which immunotherapeutic approaches may be less effective,” they noted.
In the trial, 99 patients with pretreated locally advanced and unresectable or metastatic urothelial carcinoma having FGFR alterations were given single-agent, open-label erdafitinib (Balversa) for a median of five cycles. The drug was recently granted accelerated approval by the Food and Drug Administration for this indication.
The rate of confirmed response according to investigator assessment was 40% (3% of patients had a complete response and 37% had a partial response), based on trial results reported in the New England Journal of Medicine. The response rate was 59% among the subset who had previously received immunotherapy.
With a median follow-up of 11.0 months, the median duration of progression-free survival was 5.5 months, and the median duration of overall survival was 13.8 months.
Fully 46% of patients experienced a grade 3 or higher treatment-related adverse event, most commonly hyponatremia (11%), stomatitis (10%), and asthenia (7%). Nearly 56% of the trial population as a whole required a dose reduction. However, only 13% of patients stopped treatment because of an adverse event, and there were no treatment-related deaths.
“This study met its primary objective,” Dr. Loriot and coinvestigators concluded. “These findings showed that among patients with locally advanced and unresectable or metastatic urothelial carcinoma with certain FGFR alterations, erdafitinib had promising antitumor activity.”
“The response to erdafitinib was rapid and independent of the number of previous courses and types of therapy, the presence of visceral metastasis, or tumor location,” they wrote. In addition, the efficacy appears to be better than that achieved previously with chemotherapy, immune checkpoint inhibitors, and antibody-drug conjugates.
The trial was funded by Janssen Research and Development. Dr. Loriot reports grants and personal fees from Janssen, during the conduct of the study.
SOURCE: Loriot Y et al. N Engl J Med. 2019;381:338-348. doi: 10.1056/NEJMoa1817323.
Erdafitinib, an oral pan–fibroblast growth factor receptor (FGFR) tyrosine kinase inhibitor, is efficacious when used to treat urothelial cancer harboring FGFR genetic alterations, although dose adjustments are commonly needed, suggests a multicenter phase 2 trial.
“Mutations and fusions in FGFR2/3 are common in patients with urothelial carcinoma, particularly in the luminal I subtype, and can cause constitutive FGFR signaling that may contribute to carcinogenesis,” write Yohann Loriot, MD, of Gustave Roussy, Université Paris-Sud and Université Paris-Saclay, in Villejuif, France, and coinvestigators. Up to 20% of patients with advanced disease and fully 37% of those with upper-tract tumors have alterations in these genes. “ Thus, FGFR inhibition may be particularly appropriate in patients with luminal I subtype disease, in which immunotherapeutic approaches may be less effective,” they noted.
In the trial, 99 patients with pretreated locally advanced and unresectable or metastatic urothelial carcinoma having FGFR alterations were given single-agent, open-label erdafitinib (Balversa) for a median of five cycles. The drug was recently granted accelerated approval by the Food and Drug Administration for this indication.
The rate of confirmed response according to investigator assessment was 40% (3% of patients had a complete response and 37% had a partial response), based on trial results reported in the New England Journal of Medicine. The response rate was 59% among the subset who had previously received immunotherapy.
With a median follow-up of 11.0 months, the median duration of progression-free survival was 5.5 months, and the median duration of overall survival was 13.8 months.
Fully 46% of patients experienced a grade 3 or higher treatment-related adverse event, most commonly hyponatremia (11%), stomatitis (10%), and asthenia (7%). Nearly 56% of the trial population as a whole required a dose reduction. However, only 13% of patients stopped treatment because of an adverse event, and there were no treatment-related deaths.
“This study met its primary objective,” Dr. Loriot and coinvestigators concluded. “These findings showed that among patients with locally advanced and unresectable or metastatic urothelial carcinoma with certain FGFR alterations, erdafitinib had promising antitumor activity.”
“The response to erdafitinib was rapid and independent of the number of previous courses and types of therapy, the presence of visceral metastasis, or tumor location,” they wrote. In addition, the efficacy appears to be better than that achieved previously with chemotherapy, immune checkpoint inhibitors, and antibody-drug conjugates.
The trial was funded by Janssen Research and Development. Dr. Loriot reports grants and personal fees from Janssen, during the conduct of the study.
SOURCE: Loriot Y et al. N Engl J Med. 2019;381:338-348. doi: 10.1056/NEJMoa1817323.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Erdafitinib has good efficacy when used to treat advanced urothelial carcinoma harboring FGFR alterations.
Major finding: The confirmed response rate was 40% (3% of patients had a complete response, 37% of patients had a partial response). With a median follow-up of 11.0 months, the median duration of progression-free survival was 5.5 months, and the median duration of overall survival was 13.8 months.
Study details: A multicenter, open-label, single-arm phase 2 trial among 99 patients with pretreated locally advanced and unresectable or metastatic urothelial carcinoma having FGFR alterations.
Disclosures: The trial was funded by Janssen Research and Development. Dr. Loriot reports grants and personal fees from Janssen, during the conduct of the study.
Source: Loriot Y et al. N Engl J Med. 2019;381:338-48. doi: 10.1056/NEJMoa1817323.
Durvalumab fails to advance in pancreatic cancer
, according to results of a phase 2 randomized controlled trial.
“Immune checkpoint blockade in PDAC as a single-agent therapy was not currently indicated beyond the subgroup of patients with microsatellite instability or mismatch repair deficiency ... however, a precedent existed for evaluating a combination of 2 immune checkpoint antagonists in this setting,” noted the investigators, led by Eileen M. O’Reilly, MD, gastrointestinal medical oncology, David M. Rubenstein Center for Pancreatic Cancer, Memorial Sloan Kettering Cancer Center and Cornell University, New York. In particular, a combination of agents that inhibit programmed cell death-1 ligand 1 (PD-L1) and the human T-cell receptor protein cytotoxic T-lymphocyte-associated protein 4 (CTLA4), nonredundant mechanisms, has shown promise.
Dr. O’Reilly and coinvestigators treated 65 patients in the trial’s initial cohort who had received only a single first-line fluorouracil- or gemcitabine-based chemotherapy regimen for recurrent or metastatic PDAC. Patients were randomized to combination therapy with durvalumab (Imfinzi), an anti-PD-L1 antibody, and tremelimumab, an investigational anti-CTLA4 antibody, followed by durvalumab alone, or to durvalumab monotherapy.
The objective response rate was just 3.1% with combination therapy and 0% with monotherapy—values that fell far short of the predefined 10% rate needed to initiate a planned expansion cohort. Both groups had a median progression-free survival of 1.5 months, Dr. O’Reilly and associates wrote. Their report is in JAMA Oncology.
The rate of grade 3 or higher treatment-related adverse events was 22% in the combination therapy group and 6% in the monotherapy group. In both groups, the most common events were fatigue and diarrhea. Some 6% and 3% of patients, respectively, stopped treatment because of a treatment-related adverse event.
The small trial population precluded detailed analyses of associations between treatment response and PD-L1 expression or microsatellite instability status.
“The observed efficacy of durvalumab plus tremelimumab therapy and durvalumab monotherapy was reflective of a population of patients with [metastatic PDAC] who had poor prognoses and rapidly progressing disease; however, treatment was well tolerated,” Dr. O’Reilly and coinvestigators wrote.
“Future studies are needed to evaluate how to best combine immune checkpoint blockade with other agents, including cytotoxic and targeted therapies, with the intention of overcoming the unique immunosuppressive, hypoxic, and fibrotic tumor microenvironment of PDAC. Such studies should evaluate biomarker expression to identify patients most likely to benefit from immune checkpoint blockade,” they recommended.
Dr. O’Reilly disclosed holding a consulting or advisory role or receiving grants from numerous pharmaceutical companies, including AstraZeneca, which funded the study.
SOURCE: O’Reilly EM et al. JAMA Oncol. 2019 July 18. doi:10.1001/jamaoncol.2019.1588.
“This study clearly and soberly demonstrates that despite the observed clinical benefits of dual ICI [immune check-point inhibition] therapy appreciated in other tumor types, PDAC remains refractory to standalone dual ICI therapy,” Dan A. Laheru, MD, and colleagues wrote in an invited commentary. “The priming of antitumor T-cell responses in the draining lymph nodes by anti-CTLA-4 therapy, tremelimumab, appears to be insufficient in priming T cells in PDAC for the addition of PD-L1 therapy.”
Current evidence suggests two main challenges will have to be overcome to pave the way for effective ICI therapy in PDAC and similarly nonimmunogenic cancers, they proposed. One will be inducing high-quality effector T cells into the tumor microenvironment (TME); the other will be reprogramming this “extremely immunosuppressive” milieu.
“Although there remains a rationale for testing dual checkpoint blockade therapy in patients with PDAC, this strategy will likely need to include agents that will first trigger the trafficking of T cells into the otherwise T-cell-poor tumor so that T cells are available for activation by ICIs. Furthermore, other agents need to be further tested in combination that would effectively reprogram the otherwise immunosuppressive PDAC TME to optimize T-cell function by turning off inhibitory signals,” Dr. Laheru and colleagues noted. “This study also strongly suggests that we should no longer test stand-alone ICI monotherapy or dual ICI in patients with PDAC without a T-cell inducing agent, whether that is a personalized vaccine-based therapy, small-molecule/antibody immunomodulator, or another immunotherapy agent altogether.
“The road to developing improved immunotherapy for patients with PDAC remains challenging,” they concluded. “Through the results of such work presented by the authors along with a greater understanding of the immune microenvironment, it is our hope that subsequent trials will allow future patients with PDAC to realize the benefits of immunotherapy that have helped so many in other cancer types.”
Arsen Osipov, MD, Neeha Zaidi, MD, and Dan A. Laheru, MD, are with the Skip Viragh Center for Pancreatic Cancer Research and Clinical Care, Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University, Baltimore.
“This study clearly and soberly demonstrates that despite the observed clinical benefits of dual ICI [immune check-point inhibition] therapy appreciated in other tumor types, PDAC remains refractory to standalone dual ICI therapy,” Dan A. Laheru, MD, and colleagues wrote in an invited commentary. “The priming of antitumor T-cell responses in the draining lymph nodes by anti-CTLA-4 therapy, tremelimumab, appears to be insufficient in priming T cells in PDAC for the addition of PD-L1 therapy.”
Current evidence suggests two main challenges will have to be overcome to pave the way for effective ICI therapy in PDAC and similarly nonimmunogenic cancers, they proposed. One will be inducing high-quality effector T cells into the tumor microenvironment (TME); the other will be reprogramming this “extremely immunosuppressive” milieu.
“Although there remains a rationale for testing dual checkpoint blockade therapy in patients with PDAC, this strategy will likely need to include agents that will first trigger the trafficking of T cells into the otherwise T-cell-poor tumor so that T cells are available for activation by ICIs. Furthermore, other agents need to be further tested in combination that would effectively reprogram the otherwise immunosuppressive PDAC TME to optimize T-cell function by turning off inhibitory signals,” Dr. Laheru and colleagues noted. “This study also strongly suggests that we should no longer test stand-alone ICI monotherapy or dual ICI in patients with PDAC without a T-cell inducing agent, whether that is a personalized vaccine-based therapy, small-molecule/antibody immunomodulator, or another immunotherapy agent altogether.
“The road to developing improved immunotherapy for patients with PDAC remains challenging,” they concluded. “Through the results of such work presented by the authors along with a greater understanding of the immune microenvironment, it is our hope that subsequent trials will allow future patients with PDAC to realize the benefits of immunotherapy that have helped so many in other cancer types.”
Arsen Osipov, MD, Neeha Zaidi, MD, and Dan A. Laheru, MD, are with the Skip Viragh Center for Pancreatic Cancer Research and Clinical Care, Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University, Baltimore.
“This study clearly and soberly demonstrates that despite the observed clinical benefits of dual ICI [immune check-point inhibition] therapy appreciated in other tumor types, PDAC remains refractory to standalone dual ICI therapy,” Dan A. Laheru, MD, and colleagues wrote in an invited commentary. “The priming of antitumor T-cell responses in the draining lymph nodes by anti-CTLA-4 therapy, tremelimumab, appears to be insufficient in priming T cells in PDAC for the addition of PD-L1 therapy.”
Current evidence suggests two main challenges will have to be overcome to pave the way for effective ICI therapy in PDAC and similarly nonimmunogenic cancers, they proposed. One will be inducing high-quality effector T cells into the tumor microenvironment (TME); the other will be reprogramming this “extremely immunosuppressive” milieu.
“Although there remains a rationale for testing dual checkpoint blockade therapy in patients with PDAC, this strategy will likely need to include agents that will first trigger the trafficking of T cells into the otherwise T-cell-poor tumor so that T cells are available for activation by ICIs. Furthermore, other agents need to be further tested in combination that would effectively reprogram the otherwise immunosuppressive PDAC TME to optimize T-cell function by turning off inhibitory signals,” Dr. Laheru and colleagues noted. “This study also strongly suggests that we should no longer test stand-alone ICI monotherapy or dual ICI in patients with PDAC without a T-cell inducing agent, whether that is a personalized vaccine-based therapy, small-molecule/antibody immunomodulator, or another immunotherapy agent altogether.
“The road to developing improved immunotherapy for patients with PDAC remains challenging,” they concluded. “Through the results of such work presented by the authors along with a greater understanding of the immune microenvironment, it is our hope that subsequent trials will allow future patients with PDAC to realize the benefits of immunotherapy that have helped so many in other cancer types.”
Arsen Osipov, MD, Neeha Zaidi, MD, and Dan A. Laheru, MD, are with the Skip Viragh Center for Pancreatic Cancer Research and Clinical Care, Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins University, Baltimore.
, according to results of a phase 2 randomized controlled trial.
“Immune checkpoint blockade in PDAC as a single-agent therapy was not currently indicated beyond the subgroup of patients with microsatellite instability or mismatch repair deficiency ... however, a precedent existed for evaluating a combination of 2 immune checkpoint antagonists in this setting,” noted the investigators, led by Eileen M. O’Reilly, MD, gastrointestinal medical oncology, David M. Rubenstein Center for Pancreatic Cancer, Memorial Sloan Kettering Cancer Center and Cornell University, New York. In particular, a combination of agents that inhibit programmed cell death-1 ligand 1 (PD-L1) and the human T-cell receptor protein cytotoxic T-lymphocyte-associated protein 4 (CTLA4), nonredundant mechanisms, has shown promise.
Dr. O’Reilly and coinvestigators treated 65 patients in the trial’s initial cohort who had received only a single first-line fluorouracil- or gemcitabine-based chemotherapy regimen for recurrent or metastatic PDAC. Patients were randomized to combination therapy with durvalumab (Imfinzi), an anti-PD-L1 antibody, and tremelimumab, an investigational anti-CTLA4 antibody, followed by durvalumab alone, or to durvalumab monotherapy.
The objective response rate was just 3.1% with combination therapy and 0% with monotherapy—values that fell far short of the predefined 10% rate needed to initiate a planned expansion cohort. Both groups had a median progression-free survival of 1.5 months, Dr. O’Reilly and associates wrote. Their report is in JAMA Oncology.
The rate of grade 3 or higher treatment-related adverse events was 22% in the combination therapy group and 6% in the monotherapy group. In both groups, the most common events were fatigue and diarrhea. Some 6% and 3% of patients, respectively, stopped treatment because of a treatment-related adverse event.
The small trial population precluded detailed analyses of associations between treatment response and PD-L1 expression or microsatellite instability status.
“The observed efficacy of durvalumab plus tremelimumab therapy and durvalumab monotherapy was reflective of a population of patients with [metastatic PDAC] who had poor prognoses and rapidly progressing disease; however, treatment was well tolerated,” Dr. O’Reilly and coinvestigators wrote.
“Future studies are needed to evaluate how to best combine immune checkpoint blockade with other agents, including cytotoxic and targeted therapies, with the intention of overcoming the unique immunosuppressive, hypoxic, and fibrotic tumor microenvironment of PDAC. Such studies should evaluate biomarker expression to identify patients most likely to benefit from immune checkpoint blockade,” they recommended.
Dr. O’Reilly disclosed holding a consulting or advisory role or receiving grants from numerous pharmaceutical companies, including AstraZeneca, which funded the study.
SOURCE: O’Reilly EM et al. JAMA Oncol. 2019 July 18. doi:10.1001/jamaoncol.2019.1588.
, according to results of a phase 2 randomized controlled trial.
“Immune checkpoint blockade in PDAC as a single-agent therapy was not currently indicated beyond the subgroup of patients with microsatellite instability or mismatch repair deficiency ... however, a precedent existed for evaluating a combination of 2 immune checkpoint antagonists in this setting,” noted the investigators, led by Eileen M. O’Reilly, MD, gastrointestinal medical oncology, David M. Rubenstein Center for Pancreatic Cancer, Memorial Sloan Kettering Cancer Center and Cornell University, New York. In particular, a combination of agents that inhibit programmed cell death-1 ligand 1 (PD-L1) and the human T-cell receptor protein cytotoxic T-lymphocyte-associated protein 4 (CTLA4), nonredundant mechanisms, has shown promise.
Dr. O’Reilly and coinvestigators treated 65 patients in the trial’s initial cohort who had received only a single first-line fluorouracil- or gemcitabine-based chemotherapy regimen for recurrent or metastatic PDAC. Patients were randomized to combination therapy with durvalumab (Imfinzi), an anti-PD-L1 antibody, and tremelimumab, an investigational anti-CTLA4 antibody, followed by durvalumab alone, or to durvalumab monotherapy.
The objective response rate was just 3.1% with combination therapy and 0% with monotherapy—values that fell far short of the predefined 10% rate needed to initiate a planned expansion cohort. Both groups had a median progression-free survival of 1.5 months, Dr. O’Reilly and associates wrote. Their report is in JAMA Oncology.
The rate of grade 3 or higher treatment-related adverse events was 22% in the combination therapy group and 6% in the monotherapy group. In both groups, the most common events were fatigue and diarrhea. Some 6% and 3% of patients, respectively, stopped treatment because of a treatment-related adverse event.
The small trial population precluded detailed analyses of associations between treatment response and PD-L1 expression or microsatellite instability status.
“The observed efficacy of durvalumab plus tremelimumab therapy and durvalumab monotherapy was reflective of a population of patients with [metastatic PDAC] who had poor prognoses and rapidly progressing disease; however, treatment was well tolerated,” Dr. O’Reilly and coinvestigators wrote.
“Future studies are needed to evaluate how to best combine immune checkpoint blockade with other agents, including cytotoxic and targeted therapies, with the intention of overcoming the unique immunosuppressive, hypoxic, and fibrotic tumor microenvironment of PDAC. Such studies should evaluate biomarker expression to identify patients most likely to benefit from immune checkpoint blockade,” they recommended.
Dr. O’Reilly disclosed holding a consulting or advisory role or receiving grants from numerous pharmaceutical companies, including AstraZeneca, which funded the study.
SOURCE: O’Reilly EM et al. JAMA Oncol. 2019 July 18. doi:10.1001/jamaoncol.2019.1588.
FROM JAMA ONCOLOGY
Hurricanes delay RT, worsening survival of NSCLC
suggests a retrospective cohort study.
“Radiotherapy is particularly vulnerable because it requires dependable electrical power and daily treatment,” lead investigator Leticia M. Nogueira, PhD, Surveillance and Health Services Research Program, American Cancer Society, and colleagues noted. “Disruptions are especially concerning for patients undergoing treatment for locally advanced ... NSCLC because treatment delays as little as 2 days negatively affect survival.”
The investigators used the National Cancer Database to identify patients receiving definitive radiotherapy for nonoperative locally advanced NSCLC between 2004 and 2014 who had at least 1 year of follow-up for vital status.
Each patient undergoing radiotherapy when a hurricane disaster was declared for their facility’s area was matched through propensity scoring with a patient treated during a declaration-free period having similar start month, sex, age, stage, nodal status, and income. Analyses compared 1,734 exposed patients with 1,734 unexposed patients.
Study results reported in JAMA showed that 101 hurricane disaster declarations were made during the study period, and they lasted from 1 day to 69 days. The radiation treatment duration was about 21 days (45%) longer for patients exposed to these declarations than for unexposed counterparts (66.9 vs. 46.2 days; P less than .001).
Over a median follow-up of 15 months, exposed patients were more likely to die (adjusted hazard ratio, 1.19; P = .001). Moreover, risk generally rose with the duration of the declaration, peaking for patients exposed to those lasting 27 days (adjusted relative risk, 1.27).
“Because data on other potentially explanatory factors are lacking, the relative contribution of treatment delay to the observed association cannot be quantified. However, treatment delay is one of the few hurricane-related disruptions that can be prevented,” Dr. Nogueira and colleagues maintain.
“Because no recommended correction for radiotherapy delays exists ... strategies for identifying patients, arranging for transferring treatment, and eliminating patient out-of-network insurance charges should be considered in disaster mitigation planning,” they recommend.
Dr. Nogueira disclosed no relevant conflicts of interest. The investigators conducted the study as part of the in-tramural research program at the American Cancer Society or contributed their time.
SOURCE: Nogueira LM et al. JAMA. 2019 Jul 16;322(3):269-71.
suggests a retrospective cohort study.
“Radiotherapy is particularly vulnerable because it requires dependable electrical power and daily treatment,” lead investigator Leticia M. Nogueira, PhD, Surveillance and Health Services Research Program, American Cancer Society, and colleagues noted. “Disruptions are especially concerning for patients undergoing treatment for locally advanced ... NSCLC because treatment delays as little as 2 days negatively affect survival.”
The investigators used the National Cancer Database to identify patients receiving definitive radiotherapy for nonoperative locally advanced NSCLC between 2004 and 2014 who had at least 1 year of follow-up for vital status.
Each patient undergoing radiotherapy when a hurricane disaster was declared for their facility’s area was matched through propensity scoring with a patient treated during a declaration-free period having similar start month, sex, age, stage, nodal status, and income. Analyses compared 1,734 exposed patients with 1,734 unexposed patients.
Study results reported in JAMA showed that 101 hurricane disaster declarations were made during the study period, and they lasted from 1 day to 69 days. The radiation treatment duration was about 21 days (45%) longer for patients exposed to these declarations than for unexposed counterparts (66.9 vs. 46.2 days; P less than .001).
Over a median follow-up of 15 months, exposed patients were more likely to die (adjusted hazard ratio, 1.19; P = .001). Moreover, risk generally rose with the duration of the declaration, peaking for patients exposed to those lasting 27 days (adjusted relative risk, 1.27).
“Because data on other potentially explanatory factors are lacking, the relative contribution of treatment delay to the observed association cannot be quantified. However, treatment delay is one of the few hurricane-related disruptions that can be prevented,” Dr. Nogueira and colleagues maintain.
“Because no recommended correction for radiotherapy delays exists ... strategies for identifying patients, arranging for transferring treatment, and eliminating patient out-of-network insurance charges should be considered in disaster mitigation planning,” they recommend.
Dr. Nogueira disclosed no relevant conflicts of interest. The investigators conducted the study as part of the in-tramural research program at the American Cancer Society or contributed their time.
SOURCE: Nogueira LM et al. JAMA. 2019 Jul 16;322(3):269-71.
suggests a retrospective cohort study.
“Radiotherapy is particularly vulnerable because it requires dependable electrical power and daily treatment,” lead investigator Leticia M. Nogueira, PhD, Surveillance and Health Services Research Program, American Cancer Society, and colleagues noted. “Disruptions are especially concerning for patients undergoing treatment for locally advanced ... NSCLC because treatment delays as little as 2 days negatively affect survival.”
The investigators used the National Cancer Database to identify patients receiving definitive radiotherapy for nonoperative locally advanced NSCLC between 2004 and 2014 who had at least 1 year of follow-up for vital status.
Each patient undergoing radiotherapy when a hurricane disaster was declared for their facility’s area was matched through propensity scoring with a patient treated during a declaration-free period having similar start month, sex, age, stage, nodal status, and income. Analyses compared 1,734 exposed patients with 1,734 unexposed patients.
Study results reported in JAMA showed that 101 hurricane disaster declarations were made during the study period, and they lasted from 1 day to 69 days. The radiation treatment duration was about 21 days (45%) longer for patients exposed to these declarations than for unexposed counterparts (66.9 vs. 46.2 days; P less than .001).
Over a median follow-up of 15 months, exposed patients were more likely to die (adjusted hazard ratio, 1.19; P = .001). Moreover, risk generally rose with the duration of the declaration, peaking for patients exposed to those lasting 27 days (adjusted relative risk, 1.27).
“Because data on other potentially explanatory factors are lacking, the relative contribution of treatment delay to the observed association cannot be quantified. However, treatment delay is one of the few hurricane-related disruptions that can be prevented,” Dr. Nogueira and colleagues maintain.
“Because no recommended correction for radiotherapy delays exists ... strategies for identifying patients, arranging for transferring treatment, and eliminating patient out-of-network insurance charges should be considered in disaster mitigation planning,” they recommend.
Dr. Nogueira disclosed no relevant conflicts of interest. The investigators conducted the study as part of the in-tramural research program at the American Cancer Society or contributed their time.
SOURCE: Nogueira LM et al. JAMA. 2019 Jul 16;322(3):269-71.
FROM JAMA
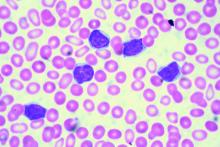
Ibrutinib-venetoclax found highly active in hard-to-treat CLL
The strategy of simultaneously inhibiting proliferation and reactivating apoptosis can eradicate chronic lymphocytic leukemia (CLL) in a large share of patients, suggest results from the phase 2 CLARITY trial.
“Both ibrutinib and venetoclax are active in CLL with improved survival; however, as monotherapies, both currently are given until disease progression,” wrote Peter Hillmen, MBChB, PhD, St. James’s University Hospital, Leeds, England, and his colleagues.
In the single-arm, open-label trial, the investigators treated 53 patients with relapsed or refractory CLL with combination ibrutinib (Imbruvica), a small-molecule inhibitor of Bruton’s tyrosine kinase, and venetoclax (Venclexta), a small molecule inhibitor of the anti-apoptotic protein Bcl-2. The primary endpoint was MRD negativity, defined as presence of fewer than one CLL cell in 10,000 leukocytes, after 12 months of combination therapy.
Results reported in the Journal of Clinical Oncology showed that the combination was highly active, with 53% of patients achieving MRD negativity in the blood and 36% achieving MRD negativity in the marrow.
Most patients, 89%, had a treatment response, and slightly more than half, 51%, achieved a complete remission. With a median 21.1-month follow-up, only a single patient experienced progression and all were still alive.
Adverse effects were generally manageable. Grade 3-4 adverse events of special interest included 34 cases of neutropenia and 1 case of biochemical tumor lysis syndrome that was managed by delaying venetoclax.
“We have demonstrated promising efficacy that indicates potent synergy between ibrutinib and venetoclax for inducing MRD-negative responses with manageable adverse effects,” the investigators wrote. “The observation that a significant proportion of patients experience MRD-negative remission indicates that this combination can be given for a limited period and then stopped after patients achieve a deep remission.”
Whether the combination leads to permanent disease eradication in certain patients is still unclear, the investigators added.
The trial was supported by Bloodwise under the Trials Acceleration Programme, by the National Institute for Health Research Leeds Clinical Research Facility, and by an unrestricted educational grant from Janssen-Cilag and AbbVie. Ibrutinib was provided free of charge by Janssen-Cilag, and venetoclax was provided free of charge by AbbVie. Dr. Hillman reported financial relationships with Janssen, AbbVie, Roche, Pharmacyclics, and Gilead Sciences.
SOURCE: Hillmen P et al. J Clin Oncol. 2019 Jul 11. doi: 10.1200/JCO.19.00894.
The strategy of simultaneously inhibiting proliferation and reactivating apoptosis can eradicate chronic lymphocytic leukemia (CLL) in a large share of patients, suggest results from the phase 2 CLARITY trial.
“Both ibrutinib and venetoclax are active in CLL with improved survival; however, as monotherapies, both currently are given until disease progression,” wrote Peter Hillmen, MBChB, PhD, St. James’s University Hospital, Leeds, England, and his colleagues.
In the single-arm, open-label trial, the investigators treated 53 patients with relapsed or refractory CLL with combination ibrutinib (Imbruvica), a small-molecule inhibitor of Bruton’s tyrosine kinase, and venetoclax (Venclexta), a small molecule inhibitor of the anti-apoptotic protein Bcl-2. The primary endpoint was MRD negativity, defined as presence of fewer than one CLL cell in 10,000 leukocytes, after 12 months of combination therapy.
Results reported in the Journal of Clinical Oncology showed that the combination was highly active, with 53% of patients achieving MRD negativity in the blood and 36% achieving MRD negativity in the marrow.
Most patients, 89%, had a treatment response, and slightly more than half, 51%, achieved a complete remission. With a median 21.1-month follow-up, only a single patient experienced progression and all were still alive.
Adverse effects were generally manageable. Grade 3-4 adverse events of special interest included 34 cases of neutropenia and 1 case of biochemical tumor lysis syndrome that was managed by delaying venetoclax.
“We have demonstrated promising efficacy that indicates potent synergy between ibrutinib and venetoclax for inducing MRD-negative responses with manageable adverse effects,” the investigators wrote. “The observation that a significant proportion of patients experience MRD-negative remission indicates that this combination can be given for a limited period and then stopped after patients achieve a deep remission.”
Whether the combination leads to permanent disease eradication in certain patients is still unclear, the investigators added.
The trial was supported by Bloodwise under the Trials Acceleration Programme, by the National Institute for Health Research Leeds Clinical Research Facility, and by an unrestricted educational grant from Janssen-Cilag and AbbVie. Ibrutinib was provided free of charge by Janssen-Cilag, and venetoclax was provided free of charge by AbbVie. Dr. Hillman reported financial relationships with Janssen, AbbVie, Roche, Pharmacyclics, and Gilead Sciences.
SOURCE: Hillmen P et al. J Clin Oncol. 2019 Jul 11. doi: 10.1200/JCO.19.00894.
The strategy of simultaneously inhibiting proliferation and reactivating apoptosis can eradicate chronic lymphocytic leukemia (CLL) in a large share of patients, suggest results from the phase 2 CLARITY trial.
“Both ibrutinib and venetoclax are active in CLL with improved survival; however, as monotherapies, both currently are given until disease progression,” wrote Peter Hillmen, MBChB, PhD, St. James’s University Hospital, Leeds, England, and his colleagues.
In the single-arm, open-label trial, the investigators treated 53 patients with relapsed or refractory CLL with combination ibrutinib (Imbruvica), a small-molecule inhibitor of Bruton’s tyrosine kinase, and venetoclax (Venclexta), a small molecule inhibitor of the anti-apoptotic protein Bcl-2. The primary endpoint was MRD negativity, defined as presence of fewer than one CLL cell in 10,000 leukocytes, after 12 months of combination therapy.
Results reported in the Journal of Clinical Oncology showed that the combination was highly active, with 53% of patients achieving MRD negativity in the blood and 36% achieving MRD negativity in the marrow.
Most patients, 89%, had a treatment response, and slightly more than half, 51%, achieved a complete remission. With a median 21.1-month follow-up, only a single patient experienced progression and all were still alive.
Adverse effects were generally manageable. Grade 3-4 adverse events of special interest included 34 cases of neutropenia and 1 case of biochemical tumor lysis syndrome that was managed by delaying venetoclax.
“We have demonstrated promising efficacy that indicates potent synergy between ibrutinib and venetoclax for inducing MRD-negative responses with manageable adverse effects,” the investigators wrote. “The observation that a significant proportion of patients experience MRD-negative remission indicates that this combination can be given for a limited period and then stopped after patients achieve a deep remission.”
Whether the combination leads to permanent disease eradication in certain patients is still unclear, the investigators added.
The trial was supported by Bloodwise under the Trials Acceleration Programme, by the National Institute for Health Research Leeds Clinical Research Facility, and by an unrestricted educational grant from Janssen-Cilag and AbbVie. Ibrutinib was provided free of charge by Janssen-Cilag, and venetoclax was provided free of charge by AbbVie. Dr. Hillman reported financial relationships with Janssen, AbbVie, Roche, Pharmacyclics, and Gilead Sciences.
SOURCE: Hillmen P et al. J Clin Oncol. 2019 Jul 11. doi: 10.1200/JCO.19.00894.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Atezolizumab combo in first-line NSCLC misses cost-effectiveness mark
Adding the immune checkpoint inhibitor atezolizumab (Tecentriq) to doublet or triplet regimens as first-line treatment for nonsquamous non–small cell lung cancer (NSCLC) is not cost effective, even by a long shot, concluded a Markov modeling study.
Positive results of the IMpower150 trial led the Food and Drug Administration to approve and the National Comprehensive Cancer Network to recommend the combination of atezolizumab, bevacizumab, carboplatin, and paclitaxel (ABCP) as an option for selected patients in this setting, noted the investigators, led by XiaoMin Wan, PhD, of the department of pharmacy at the Second Xiangya Hospital and the Institute of Clinical Pharmacy, both at Central South University, Changsha, China.
“Although adding atezolizumab to the combination of bevacizumab and chemotherapy results in significantly higher survival in patients with metastatic NSCLC, the question of whether its price reflects its potential benefit remains unclear from a value standpoint,” they wrote.
Dr. Wan and colleagues developed a Markov model to compare the lifetime cost and effectiveness of various combinations – the quadruplet ABCP regimen, the triplet BCP regimen (bevacizumab, carboplatin, and paclitaxel), and the doublet CP regimen (carboplatin and paclitaxel) – when used as first‐line treatment for metastatic nonsquamous NSCLC.
ABCP yielded an additional 0.413 quality-adjusted life-years (QALYs) and 0.460 life-years, compared with BCP, and an additional 0.738 QALYs and 0.956 life-years, compared with CP. Respective incremental costs were $234,998 and $381,116, the investigators reported in Cancer.
Ultimately, ABCP had an incremental cost‐effectiveness ratio (ICER) of $568,967 per QALY, compared with BCP, and $516,114 per QALY, compared with CP – both of which far exceeded the conventional $100,000 ICER per QALY willingness-to-pay threshold.
Although atezolizumab targets programmed death–ligand 1 (PD-L1), the ICER improved only modestly to $464,703 per QALY when treatment was given only to patients having PD‐L1 expression of at least 50% on tumor cells or at least 10% on immune cells. Findings were similar when the duration of atezolizumab therapy was restricted to 2 years.
However, steep reductions in the costs of the two targeted agents altered results. Specifically, ABCP had an ICER of $99,786 and $162,441 per QALY, compared with BCP and CP, respectively, when the costs of atezolizumab and bevacizumab were reduced by 70%, and ABCP fell below the $100,000 willingness-to-pay threshold, compared with both regimens, when those costs were reduced by 83%.
“To our knowledge, the current study is the first cost-effectiveness analysis of ABCP, compared with BCP, in the first-line setting for patients with metastatic NSCLC,” Dr. Wan and colleagues noted. “From the perspective of the U.S. payer, ABCP is estimated not to be cost effective, compared with BCP or CP, in the first-line setting for patients with metastatic, nonsquamous NSCLC at a [willingness-to-pay] threshold of $100,000 per QALY.”
“Although ABCP is not considered to be cost effective, this does not mean that patients should receive the less-effective treatment strategy of BCP,” they cautioned, noting that recent cost-effectiveness data appear to favor the first-line combination of another immune checkpoint inhibitor, pembrolizumab (Keytruda), with chemotherapy instead. “A price reduction is warranted to make ABCP cost effective and affordable.”
Dr. Wan did not report any relevant conflicts of interest. The study was supported by grants from the National Natural Science Foundation of China and the research project of the Health and Family Planning Commission of Hunan province.
SOURCE: Wan X et al. Cancer. 2019 Jul 9. doi: 10.1002/cncr.32368.
Adding the immune checkpoint inhibitor atezolizumab (Tecentriq) to doublet or triplet regimens as first-line treatment for nonsquamous non–small cell lung cancer (NSCLC) is not cost effective, even by a long shot, concluded a Markov modeling study.
Positive results of the IMpower150 trial led the Food and Drug Administration to approve and the National Comprehensive Cancer Network to recommend the combination of atezolizumab, bevacizumab, carboplatin, and paclitaxel (ABCP) as an option for selected patients in this setting, noted the investigators, led by XiaoMin Wan, PhD, of the department of pharmacy at the Second Xiangya Hospital and the Institute of Clinical Pharmacy, both at Central South University, Changsha, China.
“Although adding atezolizumab to the combination of bevacizumab and chemotherapy results in significantly higher survival in patients with metastatic NSCLC, the question of whether its price reflects its potential benefit remains unclear from a value standpoint,” they wrote.
Dr. Wan and colleagues developed a Markov model to compare the lifetime cost and effectiveness of various combinations – the quadruplet ABCP regimen, the triplet BCP regimen (bevacizumab, carboplatin, and paclitaxel), and the doublet CP regimen (carboplatin and paclitaxel) – when used as first‐line treatment for metastatic nonsquamous NSCLC.
ABCP yielded an additional 0.413 quality-adjusted life-years (QALYs) and 0.460 life-years, compared with BCP, and an additional 0.738 QALYs and 0.956 life-years, compared with CP. Respective incremental costs were $234,998 and $381,116, the investigators reported in Cancer.
Ultimately, ABCP had an incremental cost‐effectiveness ratio (ICER) of $568,967 per QALY, compared with BCP, and $516,114 per QALY, compared with CP – both of which far exceeded the conventional $100,000 ICER per QALY willingness-to-pay threshold.
Although atezolizumab targets programmed death–ligand 1 (PD-L1), the ICER improved only modestly to $464,703 per QALY when treatment was given only to patients having PD‐L1 expression of at least 50% on tumor cells or at least 10% on immune cells. Findings were similar when the duration of atezolizumab therapy was restricted to 2 years.
However, steep reductions in the costs of the two targeted agents altered results. Specifically, ABCP had an ICER of $99,786 and $162,441 per QALY, compared with BCP and CP, respectively, when the costs of atezolizumab and bevacizumab were reduced by 70%, and ABCP fell below the $100,000 willingness-to-pay threshold, compared with both regimens, when those costs were reduced by 83%.
“To our knowledge, the current study is the first cost-effectiveness analysis of ABCP, compared with BCP, in the first-line setting for patients with metastatic NSCLC,” Dr. Wan and colleagues noted. “From the perspective of the U.S. payer, ABCP is estimated not to be cost effective, compared with BCP or CP, in the first-line setting for patients with metastatic, nonsquamous NSCLC at a [willingness-to-pay] threshold of $100,000 per QALY.”
“Although ABCP is not considered to be cost effective, this does not mean that patients should receive the less-effective treatment strategy of BCP,” they cautioned, noting that recent cost-effectiveness data appear to favor the first-line combination of another immune checkpoint inhibitor, pembrolizumab (Keytruda), with chemotherapy instead. “A price reduction is warranted to make ABCP cost effective and affordable.”
Dr. Wan did not report any relevant conflicts of interest. The study was supported by grants from the National Natural Science Foundation of China and the research project of the Health and Family Planning Commission of Hunan province.
SOURCE: Wan X et al. Cancer. 2019 Jul 9. doi: 10.1002/cncr.32368.
Adding the immune checkpoint inhibitor atezolizumab (Tecentriq) to doublet or triplet regimens as first-line treatment for nonsquamous non–small cell lung cancer (NSCLC) is not cost effective, even by a long shot, concluded a Markov modeling study.
Positive results of the IMpower150 trial led the Food and Drug Administration to approve and the National Comprehensive Cancer Network to recommend the combination of atezolizumab, bevacizumab, carboplatin, and paclitaxel (ABCP) as an option for selected patients in this setting, noted the investigators, led by XiaoMin Wan, PhD, of the department of pharmacy at the Second Xiangya Hospital and the Institute of Clinical Pharmacy, both at Central South University, Changsha, China.
“Although adding atezolizumab to the combination of bevacizumab and chemotherapy results in significantly higher survival in patients with metastatic NSCLC, the question of whether its price reflects its potential benefit remains unclear from a value standpoint,” they wrote.
Dr. Wan and colleagues developed a Markov model to compare the lifetime cost and effectiveness of various combinations – the quadruplet ABCP regimen, the triplet BCP regimen (bevacizumab, carboplatin, and paclitaxel), and the doublet CP regimen (carboplatin and paclitaxel) – when used as first‐line treatment for metastatic nonsquamous NSCLC.
ABCP yielded an additional 0.413 quality-adjusted life-years (QALYs) and 0.460 life-years, compared with BCP, and an additional 0.738 QALYs and 0.956 life-years, compared with CP. Respective incremental costs were $234,998 and $381,116, the investigators reported in Cancer.
Ultimately, ABCP had an incremental cost‐effectiveness ratio (ICER) of $568,967 per QALY, compared with BCP, and $516,114 per QALY, compared with CP – both of which far exceeded the conventional $100,000 ICER per QALY willingness-to-pay threshold.
Although atezolizumab targets programmed death–ligand 1 (PD-L1), the ICER improved only modestly to $464,703 per QALY when treatment was given only to patients having PD‐L1 expression of at least 50% on tumor cells or at least 10% on immune cells. Findings were similar when the duration of atezolizumab therapy was restricted to 2 years.
However, steep reductions in the costs of the two targeted agents altered results. Specifically, ABCP had an ICER of $99,786 and $162,441 per QALY, compared with BCP and CP, respectively, when the costs of atezolizumab and bevacizumab were reduced by 70%, and ABCP fell below the $100,000 willingness-to-pay threshold, compared with both regimens, when those costs were reduced by 83%.
“To our knowledge, the current study is the first cost-effectiveness analysis of ABCP, compared with BCP, in the first-line setting for patients with metastatic NSCLC,” Dr. Wan and colleagues noted. “From the perspective of the U.S. payer, ABCP is estimated not to be cost effective, compared with BCP or CP, in the first-line setting for patients with metastatic, nonsquamous NSCLC at a [willingness-to-pay] threshold of $100,000 per QALY.”
“Although ABCP is not considered to be cost effective, this does not mean that patients should receive the less-effective treatment strategy of BCP,” they cautioned, noting that recent cost-effectiveness data appear to favor the first-line combination of another immune checkpoint inhibitor, pembrolizumab (Keytruda), with chemotherapy instead. “A price reduction is warranted to make ABCP cost effective and affordable.”
Dr. Wan did not report any relevant conflicts of interest. The study was supported by grants from the National Natural Science Foundation of China and the research project of the Health and Family Planning Commission of Hunan province.
SOURCE: Wan X et al. Cancer. 2019 Jul 9. doi: 10.1002/cncr.32368.
FROM CANCER
Gaps in patient-provider survivorship communication persist
There has been little to no recent improvement in the large share of cancer patients who are not receiving detailed information about survivorship care, suggests a nationally representative cross-sectional survey.
In 2006, the Institute of Medicine issued a seminal report recommending survivorship care planning to address the special needs of this patient population, noted the investigators, led by Ashish Rai, PhD, American Cancer Society, Framingham, Mass. Other organizations have since issued guidelines and policies in this area.
For the study, Dr. Rai and colleagues analyzed data from 2,266 survivors who completed the 2011 or 2016 Medical Expenditure Panel Survey – Experiences with Cancer questionnaire. Survivors were asked whether any clinician had ever discussed various aspects of survivorship care; responses were dichotomized as having had detailed discussion versus not (brief or no discussion, or not remembering).
Between 2011 and 2016, there was minimal change in the percentage of survivors who reported not receiving detailed information on follow-up care (from 35.1% to 35.4%), late or long-term adverse effects (from 54.2% to 55.5%), lifestyle recommendations (from 58.9% to 57.8%), and emotional or social needs (from 69.2% to 68.2%), the investigators wrote. Their report is in Journal of Oncology Practice.
When analyses were restricted to only those survivors who had received cancer-directed treatment within 3 years of the survey, findings were essentially the same.
About one-quarter of survivors reported having detailed discussions about all four topics in both 2011 (24.4%) and 2016 (21.9%).
In 2016, nearly half of survivors, 47.6%, reported not having detailed discussions with their providers about a summary of their cancer treatments. (This question was not asked in 2011.)
“Despite national efforts and organizations promoting survivorship care planning and highlighting the need for improved quality of survivorship care delivery, clear gaps in quality of communication between survivors of cancer and providers persist,” Dr. Rai and colleagues said.
“Continued efforts are needed to promote communication about survivorship issues, including implementation and evaluation of targeted interventions in key survivorship care areas,” they recommended. “These interventions may consist of furnishing guidance on optimal ways to identify and address survivors’ communication needs, streamlining the flow of information across provider types, ensuring better integration of primary care providers with the survivorship care paradigm, and augmenting the use of health information technology for collection and dissemination of information across the cancer control continuum.”
Dr. Rai did not disclose any relevant conflicts of interest. The study did not receive specific funding.
SOURCE: Rai A et al. J Oncol Pract. 2019 July 2. doi: 10.1200/JOP.19.00157.
There has been little to no recent improvement in the large share of cancer patients who are not receiving detailed information about survivorship care, suggests a nationally representative cross-sectional survey.
In 2006, the Institute of Medicine issued a seminal report recommending survivorship care planning to address the special needs of this patient population, noted the investigators, led by Ashish Rai, PhD, American Cancer Society, Framingham, Mass. Other organizations have since issued guidelines and policies in this area.
For the study, Dr. Rai and colleagues analyzed data from 2,266 survivors who completed the 2011 or 2016 Medical Expenditure Panel Survey – Experiences with Cancer questionnaire. Survivors were asked whether any clinician had ever discussed various aspects of survivorship care; responses were dichotomized as having had detailed discussion versus not (brief or no discussion, or not remembering).
Between 2011 and 2016, there was minimal change in the percentage of survivors who reported not receiving detailed information on follow-up care (from 35.1% to 35.4%), late or long-term adverse effects (from 54.2% to 55.5%), lifestyle recommendations (from 58.9% to 57.8%), and emotional or social needs (from 69.2% to 68.2%), the investigators wrote. Their report is in Journal of Oncology Practice.
When analyses were restricted to only those survivors who had received cancer-directed treatment within 3 years of the survey, findings were essentially the same.
About one-quarter of survivors reported having detailed discussions about all four topics in both 2011 (24.4%) and 2016 (21.9%).
In 2016, nearly half of survivors, 47.6%, reported not having detailed discussions with their providers about a summary of their cancer treatments. (This question was not asked in 2011.)
“Despite national efforts and organizations promoting survivorship care planning and highlighting the need for improved quality of survivorship care delivery, clear gaps in quality of communication between survivors of cancer and providers persist,” Dr. Rai and colleagues said.
“Continued efforts are needed to promote communication about survivorship issues, including implementation and evaluation of targeted interventions in key survivorship care areas,” they recommended. “These interventions may consist of furnishing guidance on optimal ways to identify and address survivors’ communication needs, streamlining the flow of information across provider types, ensuring better integration of primary care providers with the survivorship care paradigm, and augmenting the use of health information technology for collection and dissemination of information across the cancer control continuum.”
Dr. Rai did not disclose any relevant conflicts of interest. The study did not receive specific funding.
SOURCE: Rai A et al. J Oncol Pract. 2019 July 2. doi: 10.1200/JOP.19.00157.
There has been little to no recent improvement in the large share of cancer patients who are not receiving detailed information about survivorship care, suggests a nationally representative cross-sectional survey.
In 2006, the Institute of Medicine issued a seminal report recommending survivorship care planning to address the special needs of this patient population, noted the investigators, led by Ashish Rai, PhD, American Cancer Society, Framingham, Mass. Other organizations have since issued guidelines and policies in this area.
For the study, Dr. Rai and colleagues analyzed data from 2,266 survivors who completed the 2011 or 2016 Medical Expenditure Panel Survey – Experiences with Cancer questionnaire. Survivors were asked whether any clinician had ever discussed various aspects of survivorship care; responses were dichotomized as having had detailed discussion versus not (brief or no discussion, or not remembering).
Between 2011 and 2016, there was minimal change in the percentage of survivors who reported not receiving detailed information on follow-up care (from 35.1% to 35.4%), late or long-term adverse effects (from 54.2% to 55.5%), lifestyle recommendations (from 58.9% to 57.8%), and emotional or social needs (from 69.2% to 68.2%), the investigators wrote. Their report is in Journal of Oncology Practice.
When analyses were restricted to only those survivors who had received cancer-directed treatment within 3 years of the survey, findings were essentially the same.
About one-quarter of survivors reported having detailed discussions about all four topics in both 2011 (24.4%) and 2016 (21.9%).
In 2016, nearly half of survivors, 47.6%, reported not having detailed discussions with their providers about a summary of their cancer treatments. (This question was not asked in 2011.)
“Despite national efforts and organizations promoting survivorship care planning and highlighting the need for improved quality of survivorship care delivery, clear gaps in quality of communication between survivors of cancer and providers persist,” Dr. Rai and colleagues said.
“Continued efforts are needed to promote communication about survivorship issues, including implementation and evaluation of targeted interventions in key survivorship care areas,” they recommended. “These interventions may consist of furnishing guidance on optimal ways to identify and address survivors’ communication needs, streamlining the flow of information across provider types, ensuring better integration of primary care providers with the survivorship care paradigm, and augmenting the use of health information technology for collection and dissemination of information across the cancer control continuum.”
Dr. Rai did not disclose any relevant conflicts of interest. The study did not receive specific funding.
SOURCE: Rai A et al. J Oncol Pract. 2019 July 2. doi: 10.1200/JOP.19.00157.
FROM THE JOURNAL OF ONCOLOGY PRACTICE
Comorbidities drive excess mortality after breast cancer diagnosis in childhood cancer survivors
Among women with breast cancer, risk of death is more than twice as high for those who are childhood cancer survivors than for those in whom this cancer is their first, found a retrospective cohort study. However, the excess deaths are mainly from comorbidities related to previous therapies.
Breast cancer is among the leading subsequent malignancies in adult survivors of pediatric cancers, note the investigators, who were led by Chaya S. Moskowitz, PhD, of the department of epidemiology and biostatistics at Memorial Sloan Kettering Cancer Center in New York. But outcomes after this diagnosis are not well characterized.
The investigators used the Childhood Cancer Survivor Study to identify 274 female 5-year survivors of cancer diagnosed before age 21 years who received a subsequent breast cancer diagnosis at a median age of 38 years. They then used Surveillance, Epidemiology, and End Results data to identify a control group of 1,095 female patients with de novo breast cancer matched on age, race, stage, and year of breast cancer diagnosis.
The 10-year overall survival was 73% among the childhood cancer survivors, investigators reported in the Journal of Clinical Oncology.
Compared with the control women whose breast cancer was their first cancer, the women with breast cancer who were childhood cancer survivors had an elevated risk of death from any cause (hazard ratio, 2.2) that persisted after analyses were adjusted for receipt of chemotherapy and radiation therapy (HR, 2.4). In addition, findings were similar in analyses restricted to women with ductal carcinoma in situ and women with stage 1-3 breast cancer.
The childhood cancer survivors had a modestly elevated risk of dying from breast cancer (HR, 1.3) but a sharply elevated risk of dying from other health-related causes, including other subsequent malignancies and cardiovascular or pulmonary disease often related to previous therapies (HR, 5.5).
In addition, the childhood cancer survivors had a higher cumulative incidence of diagnosis of second asynchronous breast cancers a year or more later, relative to the women in whom breast cancer was their first cancer (P less than .001). The 5-year cumulative incidence was 8.0% among the childhood cancer survivors and just 2.7% among the control women.
“Although BC [breast cancer]-specific mortality was modestly higher in childhood cancer survivors, deaths attributable to health conditions other than BC seem to be the driving force in the elevated all-cause mortality,” Dr. Moskowitz and colleagues wrote.
“To change the dismal outcomes of these women, our results suggest that it is imperative that at the time of a secondary BC diagnosis, they have a comprehensive evaluation that extends beyond a singular focus of the BC,” they concluded. “This should include an assessment of existing cardiopulmonary disease and a plan for future cancer screening to optimize the management of comorbidities and cardiopulmonary disease and prolong the lifespan of these survivors.”
Dr. Moskowitz reported that she has a consulting or advisory role with Bioclinica. The study was supported by the National Cancer Institute, a Memorial Sloan Kettering Cancer Center Core grant, the Meg Berté Owen Foundation, and the American Lebanese Syrian Associated Charities.
SOURCE: Moskowitz CS et al. J Clin Oncol. 2019 Jul 1. doi: 10.1200/JCO.18.02219.
Among women with breast cancer, risk of death is more than twice as high for those who are childhood cancer survivors than for those in whom this cancer is their first, found a retrospective cohort study. However, the excess deaths are mainly from comorbidities related to previous therapies.
Breast cancer is among the leading subsequent malignancies in adult survivors of pediatric cancers, note the investigators, who were led by Chaya S. Moskowitz, PhD, of the department of epidemiology and biostatistics at Memorial Sloan Kettering Cancer Center in New York. But outcomes after this diagnosis are not well characterized.
The investigators used the Childhood Cancer Survivor Study to identify 274 female 5-year survivors of cancer diagnosed before age 21 years who received a subsequent breast cancer diagnosis at a median age of 38 years. They then used Surveillance, Epidemiology, and End Results data to identify a control group of 1,095 female patients with de novo breast cancer matched on age, race, stage, and year of breast cancer diagnosis.
The 10-year overall survival was 73% among the childhood cancer survivors, investigators reported in the Journal of Clinical Oncology.
Compared with the control women whose breast cancer was their first cancer, the women with breast cancer who were childhood cancer survivors had an elevated risk of death from any cause (hazard ratio, 2.2) that persisted after analyses were adjusted for receipt of chemotherapy and radiation therapy (HR, 2.4). In addition, findings were similar in analyses restricted to women with ductal carcinoma in situ and women with stage 1-3 breast cancer.
The childhood cancer survivors had a modestly elevated risk of dying from breast cancer (HR, 1.3) but a sharply elevated risk of dying from other health-related causes, including other subsequent malignancies and cardiovascular or pulmonary disease often related to previous therapies (HR, 5.5).
In addition, the childhood cancer survivors had a higher cumulative incidence of diagnosis of second asynchronous breast cancers a year or more later, relative to the women in whom breast cancer was their first cancer (P less than .001). The 5-year cumulative incidence was 8.0% among the childhood cancer survivors and just 2.7% among the control women.
“Although BC [breast cancer]-specific mortality was modestly higher in childhood cancer survivors, deaths attributable to health conditions other than BC seem to be the driving force in the elevated all-cause mortality,” Dr. Moskowitz and colleagues wrote.
“To change the dismal outcomes of these women, our results suggest that it is imperative that at the time of a secondary BC diagnosis, they have a comprehensive evaluation that extends beyond a singular focus of the BC,” they concluded. “This should include an assessment of existing cardiopulmonary disease and a plan for future cancer screening to optimize the management of comorbidities and cardiopulmonary disease and prolong the lifespan of these survivors.”
Dr. Moskowitz reported that she has a consulting or advisory role with Bioclinica. The study was supported by the National Cancer Institute, a Memorial Sloan Kettering Cancer Center Core grant, the Meg Berté Owen Foundation, and the American Lebanese Syrian Associated Charities.
SOURCE: Moskowitz CS et al. J Clin Oncol. 2019 Jul 1. doi: 10.1200/JCO.18.02219.
Among women with breast cancer, risk of death is more than twice as high for those who are childhood cancer survivors than for those in whom this cancer is their first, found a retrospective cohort study. However, the excess deaths are mainly from comorbidities related to previous therapies.
Breast cancer is among the leading subsequent malignancies in adult survivors of pediatric cancers, note the investigators, who were led by Chaya S. Moskowitz, PhD, of the department of epidemiology and biostatistics at Memorial Sloan Kettering Cancer Center in New York. But outcomes after this diagnosis are not well characterized.
The investigators used the Childhood Cancer Survivor Study to identify 274 female 5-year survivors of cancer diagnosed before age 21 years who received a subsequent breast cancer diagnosis at a median age of 38 years. They then used Surveillance, Epidemiology, and End Results data to identify a control group of 1,095 female patients with de novo breast cancer matched on age, race, stage, and year of breast cancer diagnosis.
The 10-year overall survival was 73% among the childhood cancer survivors, investigators reported in the Journal of Clinical Oncology.
Compared with the control women whose breast cancer was their first cancer, the women with breast cancer who were childhood cancer survivors had an elevated risk of death from any cause (hazard ratio, 2.2) that persisted after analyses were adjusted for receipt of chemotherapy and radiation therapy (HR, 2.4). In addition, findings were similar in analyses restricted to women with ductal carcinoma in situ and women with stage 1-3 breast cancer.
The childhood cancer survivors had a modestly elevated risk of dying from breast cancer (HR, 1.3) but a sharply elevated risk of dying from other health-related causes, including other subsequent malignancies and cardiovascular or pulmonary disease often related to previous therapies (HR, 5.5).
In addition, the childhood cancer survivors had a higher cumulative incidence of diagnosis of second asynchronous breast cancers a year or more later, relative to the women in whom breast cancer was their first cancer (P less than .001). The 5-year cumulative incidence was 8.0% among the childhood cancer survivors and just 2.7% among the control women.
“Although BC [breast cancer]-specific mortality was modestly higher in childhood cancer survivors, deaths attributable to health conditions other than BC seem to be the driving force in the elevated all-cause mortality,” Dr. Moskowitz and colleagues wrote.
“To change the dismal outcomes of these women, our results suggest that it is imperative that at the time of a secondary BC diagnosis, they have a comprehensive evaluation that extends beyond a singular focus of the BC,” they concluded. “This should include an assessment of existing cardiopulmonary disease and a plan for future cancer screening to optimize the management of comorbidities and cardiopulmonary disease and prolong the lifespan of these survivors.”
Dr. Moskowitz reported that she has a consulting or advisory role with Bioclinica. The study was supported by the National Cancer Institute, a Memorial Sloan Kettering Cancer Center Core grant, the Meg Berté Owen Foundation, and the American Lebanese Syrian Associated Charities.
SOURCE: Moskowitz CS et al. J Clin Oncol. 2019 Jul 1. doi: 10.1200/JCO.18.02219.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Racial, age disparities confirmed in triple-negative breast cancer
Odds of triple-negative breast cancer (TNBC) are elevated for minority women and younger women, results of a nationwide cross-sectional cohort study of more than a million breast cancer cases confirm.
Previous studies have suggested certain sociodemographic groups are disproportionately affected by TNBC, but have been limited by the population studied, size, and characteristics assessed, note the investigators, who were led by Lia C. Scott, PhD, MPH, of the division of epidemiology and biostatistics at the School of Public Health, Georgia State University, Atlanta. “It is imperative that cancer research identify factors that drive disparities and focus on prevention,” they wrote in Cancer.
Dr. Scott and coinvestigators used the United States Cancer Statistics database to identify 1,151,724 cases of breast cancer diagnosed during 2010-2014 in 39 states having the necessary data. TNBC accounted for roughly 8.4% of all cases.
In unadjusted analyses using non-Hispanic white women as the comparator, odds of TNBC were significantly higher for non-Hispanic black women (odds ratio, 2.27), Hispanic women (OR, 1.22), and American Indian/Alaska Native women (OR, 1.26). On the other hand, odds were lower for Asian women (OR, 0.92).
By age group, compared with women 50-64 years old, women younger than 40 years were most likely to have the TNBC phenotype (OR, 1.95), while women aged 75 or older were least likely (OR, 0.75). Odds of TNBC were also significantly elevated for women whose cancer was diagnosed at stage III or higher (OR, 1.69) or at stage IV (OR, 1.47).
Findings were essentially the same in analyses simultaneously adjusted for age, race, and stage.
“The results of the current study demonstrated that there is a significant burden of disease in TNBC diagnosed among women of color, specifically non-Hispanic black women, and younger women,” Dr. Scott and coinvestigators write. “Given the large sample size and geospatial coverage of the data, these results are somewhat different from and also more generalizable, compared with data from previous studies.”
“With the advent and availability of more comprehensive cancer data, such as the United States Cancer Statistics database, it is important that we continue to explore disparities in order to better inform practice and policy around screenable cancers like breast cancer,” she further commented in a statement. “We hope that this update on the epidemiology of triple-negative breast cancer can provide a basis to further explore contributing factors in future research.”
Dr. Scott disclosed that she received a Dissertation Training Grant (F31-Diversity) from the National Institutes of Health. The study was funded by the National Institute on Minority Health and Health Disparities of the National Institutes of Health; the Centers for Disease Control and Prevention’s National Program of Cancer Registries contributed funds to cover the standard research data center fees for researchers conducting analyses under approved research projects.
SOURCE: Scott LC et al. Cancer. 2019 Jul 8. doi: 10.1002/cncr.32207.
Odds of triple-negative breast cancer (TNBC) are elevated for minority women and younger women, results of a nationwide cross-sectional cohort study of more than a million breast cancer cases confirm.
Previous studies have suggested certain sociodemographic groups are disproportionately affected by TNBC, but have been limited by the population studied, size, and characteristics assessed, note the investigators, who were led by Lia C. Scott, PhD, MPH, of the division of epidemiology and biostatistics at the School of Public Health, Georgia State University, Atlanta. “It is imperative that cancer research identify factors that drive disparities and focus on prevention,” they wrote in Cancer.
Dr. Scott and coinvestigators used the United States Cancer Statistics database to identify 1,151,724 cases of breast cancer diagnosed during 2010-2014 in 39 states having the necessary data. TNBC accounted for roughly 8.4% of all cases.
In unadjusted analyses using non-Hispanic white women as the comparator, odds of TNBC were significantly higher for non-Hispanic black women (odds ratio, 2.27), Hispanic women (OR, 1.22), and American Indian/Alaska Native women (OR, 1.26). On the other hand, odds were lower for Asian women (OR, 0.92).
By age group, compared with women 50-64 years old, women younger than 40 years were most likely to have the TNBC phenotype (OR, 1.95), while women aged 75 or older were least likely (OR, 0.75). Odds of TNBC were also significantly elevated for women whose cancer was diagnosed at stage III or higher (OR, 1.69) or at stage IV (OR, 1.47).
Findings were essentially the same in analyses simultaneously adjusted for age, race, and stage.
“The results of the current study demonstrated that there is a significant burden of disease in TNBC diagnosed among women of color, specifically non-Hispanic black women, and younger women,” Dr. Scott and coinvestigators write. “Given the large sample size and geospatial coverage of the data, these results are somewhat different from and also more generalizable, compared with data from previous studies.”
“With the advent and availability of more comprehensive cancer data, such as the United States Cancer Statistics database, it is important that we continue to explore disparities in order to better inform practice and policy around screenable cancers like breast cancer,” she further commented in a statement. “We hope that this update on the epidemiology of triple-negative breast cancer can provide a basis to further explore contributing factors in future research.”
Dr. Scott disclosed that she received a Dissertation Training Grant (F31-Diversity) from the National Institutes of Health. The study was funded by the National Institute on Minority Health and Health Disparities of the National Institutes of Health; the Centers for Disease Control and Prevention’s National Program of Cancer Registries contributed funds to cover the standard research data center fees for researchers conducting analyses under approved research projects.
SOURCE: Scott LC et al. Cancer. 2019 Jul 8. doi: 10.1002/cncr.32207.
Odds of triple-negative breast cancer (TNBC) are elevated for minority women and younger women, results of a nationwide cross-sectional cohort study of more than a million breast cancer cases confirm.
Previous studies have suggested certain sociodemographic groups are disproportionately affected by TNBC, but have been limited by the population studied, size, and characteristics assessed, note the investigators, who were led by Lia C. Scott, PhD, MPH, of the division of epidemiology and biostatistics at the School of Public Health, Georgia State University, Atlanta. “It is imperative that cancer research identify factors that drive disparities and focus on prevention,” they wrote in Cancer.
Dr. Scott and coinvestigators used the United States Cancer Statistics database to identify 1,151,724 cases of breast cancer diagnosed during 2010-2014 in 39 states having the necessary data. TNBC accounted for roughly 8.4% of all cases.
In unadjusted analyses using non-Hispanic white women as the comparator, odds of TNBC were significantly higher for non-Hispanic black women (odds ratio, 2.27), Hispanic women (OR, 1.22), and American Indian/Alaska Native women (OR, 1.26). On the other hand, odds were lower for Asian women (OR, 0.92).
By age group, compared with women 50-64 years old, women younger than 40 years were most likely to have the TNBC phenotype (OR, 1.95), while women aged 75 or older were least likely (OR, 0.75). Odds of TNBC were also significantly elevated for women whose cancer was diagnosed at stage III or higher (OR, 1.69) or at stage IV (OR, 1.47).
Findings were essentially the same in analyses simultaneously adjusted for age, race, and stage.
“The results of the current study demonstrated that there is a significant burden of disease in TNBC diagnosed among women of color, specifically non-Hispanic black women, and younger women,” Dr. Scott and coinvestigators write. “Given the large sample size and geospatial coverage of the data, these results are somewhat different from and also more generalizable, compared with data from previous studies.”
“With the advent and availability of more comprehensive cancer data, such as the United States Cancer Statistics database, it is important that we continue to explore disparities in order to better inform practice and policy around screenable cancers like breast cancer,” she further commented in a statement. “We hope that this update on the epidemiology of triple-negative breast cancer can provide a basis to further explore contributing factors in future research.”
Dr. Scott disclosed that she received a Dissertation Training Grant (F31-Diversity) from the National Institutes of Health. The study was funded by the National Institute on Minority Health and Health Disparities of the National Institutes of Health; the Centers for Disease Control and Prevention’s National Program of Cancer Registries contributed funds to cover the standard research data center fees for researchers conducting analyses under approved research projects.
SOURCE: Scott LC et al. Cancer. 2019 Jul 8. doi: 10.1002/cncr.32207.
FROM CANCER
Vemurafenib has durable activity in NSCLC harboring BRAF V600 mutations
The oral BRAF(V600E) kinase inhibitor vemurafenib (Zelboraf) has durable activity in non–small cell lung cancer (NSCLC) harboring BRAF V600 mutations and possibly provides greater benefit for treatment-naive patients, found the phase 2, open-label, single-arm VE-BASKET trial.
“Targetable oncogenic drivers in NSCLC with robust clinical validation include EGFR mutations and ALK and ROS1 fusions, but identifying other targetable, clinically important subgroups of NSCLC is a high priority,” wrote the investigators, who were led by Vivek Subbiah, MD, of the University of Texas MD Anderson Cancer Center, Houston. Roughly 1%-4% of NSCLC patients have tumors harboring a BRAF V600 mutation, they noted.
Analyses were based on 62 patients with BRAF V600–mutant NSCLC enrolled in the trial’s NSCLC cohort or all-comers cohort. All received vemurafenib (960 mg twice daily) until disease progression or unacceptable toxicity.
Thirteen percent of the patients had not received any previous systemic therapy. Among those previously treated, the median number of systemic regimens received was two.
Results reported in JCO Precicion Oncology showed that the median treatment duration was 6.0 months for all patients (12.0 months for previously untreated patients and 5.7 months for previously treated patients).
The objective response rate, the trial’s primary endpoint, was 37.1% overall; it was similar in the previously untreated group and the previously treated group (37.5% and 37.0%, respectively). The clinical benefit rate was 48.4% overall, with a larger differential according to previous treatment at 62.5% and 46.3%.
Median progression-free survival was 6.5 months in all patients (12.9 months in those previously untreated and 6.1 months in those previously treated), and median overall survival was 15.4 months in all patients (not estimable in those previously untreated, but 15.4 months in those previously treated).
The most common adverse events of any grade were nausea (seen in 40% of patients), hyperkeratosis (34%), and decreased appetite (32%). The most common grade 3 or worse adverse event was anemia (10%). The safety profile generally resembled that previously observed among patients with melanoma, with no new signals.
“Vemurafenib showed promising activity in patients with NSCLC harboring BRAF V600 mutations,” Dr. Subbiah and colleagues concluded. “The prolonged [overall survival] … in the NSCLC population represents promising durability of effect with single-agent BRAF inhibition.”
“The apparent increase in median [progression-free survival] in previously untreated patients compared with previously treated patients warrants additional investigation of earlier treatment in this patient population,” they maintained.
Dr. Subbiah disclosed having a consulting or advisory role with or receiving research funding from numerous pharmaceutical companies. The study was sponsored by Hoffmann-La Roche.
SOURCE: Subbiah V et al. JCO Precis Oncol. 2019 June 27. doi: 10.1200/PO.18.00266.
The oral BRAF(V600E) kinase inhibitor vemurafenib (Zelboraf) has durable activity in non–small cell lung cancer (NSCLC) harboring BRAF V600 mutations and possibly provides greater benefit for treatment-naive patients, found the phase 2, open-label, single-arm VE-BASKET trial.
“Targetable oncogenic drivers in NSCLC with robust clinical validation include EGFR mutations and ALK and ROS1 fusions, but identifying other targetable, clinically important subgroups of NSCLC is a high priority,” wrote the investigators, who were led by Vivek Subbiah, MD, of the University of Texas MD Anderson Cancer Center, Houston. Roughly 1%-4% of NSCLC patients have tumors harboring a BRAF V600 mutation, they noted.
Analyses were based on 62 patients with BRAF V600–mutant NSCLC enrolled in the trial’s NSCLC cohort or all-comers cohort. All received vemurafenib (960 mg twice daily) until disease progression or unacceptable toxicity.
Thirteen percent of the patients had not received any previous systemic therapy. Among those previously treated, the median number of systemic regimens received was two.
Results reported in JCO Precicion Oncology showed that the median treatment duration was 6.0 months for all patients (12.0 months for previously untreated patients and 5.7 months for previously treated patients).
The objective response rate, the trial’s primary endpoint, was 37.1% overall; it was similar in the previously untreated group and the previously treated group (37.5% and 37.0%, respectively). The clinical benefit rate was 48.4% overall, with a larger differential according to previous treatment at 62.5% and 46.3%.
Median progression-free survival was 6.5 months in all patients (12.9 months in those previously untreated and 6.1 months in those previously treated), and median overall survival was 15.4 months in all patients (not estimable in those previously untreated, but 15.4 months in those previously treated).
The most common adverse events of any grade were nausea (seen in 40% of patients), hyperkeratosis (34%), and decreased appetite (32%). The most common grade 3 or worse adverse event was anemia (10%). The safety profile generally resembled that previously observed among patients with melanoma, with no new signals.
“Vemurafenib showed promising activity in patients with NSCLC harboring BRAF V600 mutations,” Dr. Subbiah and colleagues concluded. “The prolonged [overall survival] … in the NSCLC population represents promising durability of effect with single-agent BRAF inhibition.”
“The apparent increase in median [progression-free survival] in previously untreated patients compared with previously treated patients warrants additional investigation of earlier treatment in this patient population,” they maintained.
Dr. Subbiah disclosed having a consulting or advisory role with or receiving research funding from numerous pharmaceutical companies. The study was sponsored by Hoffmann-La Roche.
SOURCE: Subbiah V et al. JCO Precis Oncol. 2019 June 27. doi: 10.1200/PO.18.00266.
The oral BRAF(V600E) kinase inhibitor vemurafenib (Zelboraf) has durable activity in non–small cell lung cancer (NSCLC) harboring BRAF V600 mutations and possibly provides greater benefit for treatment-naive patients, found the phase 2, open-label, single-arm VE-BASKET trial.
“Targetable oncogenic drivers in NSCLC with robust clinical validation include EGFR mutations and ALK and ROS1 fusions, but identifying other targetable, clinically important subgroups of NSCLC is a high priority,” wrote the investigators, who were led by Vivek Subbiah, MD, of the University of Texas MD Anderson Cancer Center, Houston. Roughly 1%-4% of NSCLC patients have tumors harboring a BRAF V600 mutation, they noted.
Analyses were based on 62 patients with BRAF V600–mutant NSCLC enrolled in the trial’s NSCLC cohort or all-comers cohort. All received vemurafenib (960 mg twice daily) until disease progression or unacceptable toxicity.
Thirteen percent of the patients had not received any previous systemic therapy. Among those previously treated, the median number of systemic regimens received was two.
Results reported in JCO Precicion Oncology showed that the median treatment duration was 6.0 months for all patients (12.0 months for previously untreated patients and 5.7 months for previously treated patients).
The objective response rate, the trial’s primary endpoint, was 37.1% overall; it was similar in the previously untreated group and the previously treated group (37.5% and 37.0%, respectively). The clinical benefit rate was 48.4% overall, with a larger differential according to previous treatment at 62.5% and 46.3%.
Median progression-free survival was 6.5 months in all patients (12.9 months in those previously untreated and 6.1 months in those previously treated), and median overall survival was 15.4 months in all patients (not estimable in those previously untreated, but 15.4 months in those previously treated).
The most common adverse events of any grade were nausea (seen in 40% of patients), hyperkeratosis (34%), and decreased appetite (32%). The most common grade 3 or worse adverse event was anemia (10%). The safety profile generally resembled that previously observed among patients with melanoma, with no new signals.
“Vemurafenib showed promising activity in patients with NSCLC harboring BRAF V600 mutations,” Dr. Subbiah and colleagues concluded. “The prolonged [overall survival] … in the NSCLC population represents promising durability of effect with single-agent BRAF inhibition.”
“The apparent increase in median [progression-free survival] in previously untreated patients compared with previously treated patients warrants additional investigation of earlier treatment in this patient population,” they maintained.
Dr. Subbiah disclosed having a consulting or advisory role with or receiving research funding from numerous pharmaceutical companies. The study was sponsored by Hoffmann-La Roche.
SOURCE: Subbiah V et al. JCO Precis Oncol. 2019 June 27. doi: 10.1200/PO.18.00266.
FROM JCO PRECISION ONCOLOGY