User login
Spontaneous Pneumomediastinum
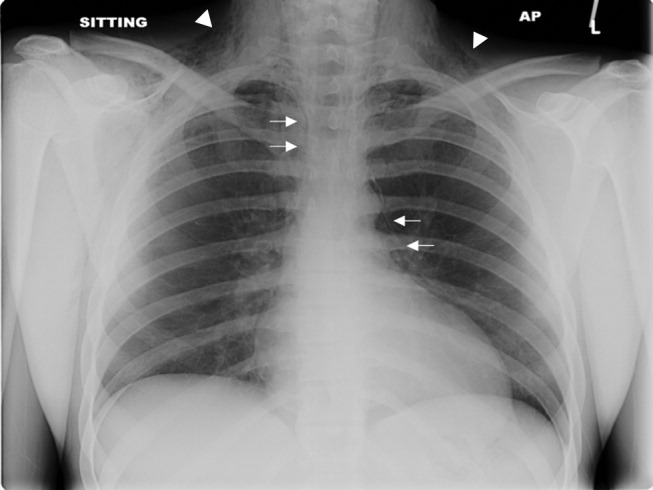
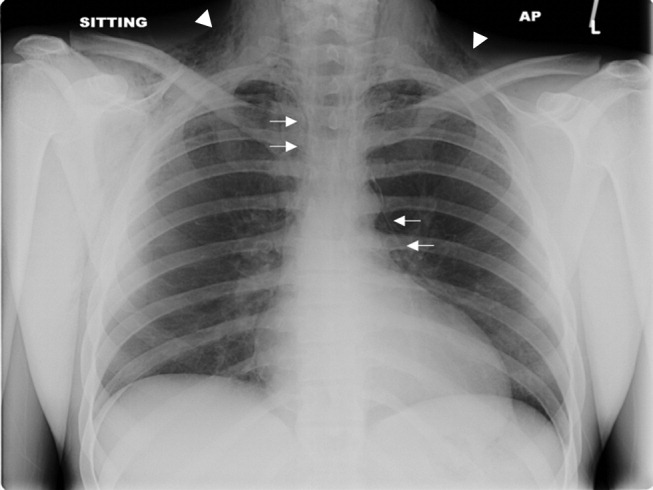
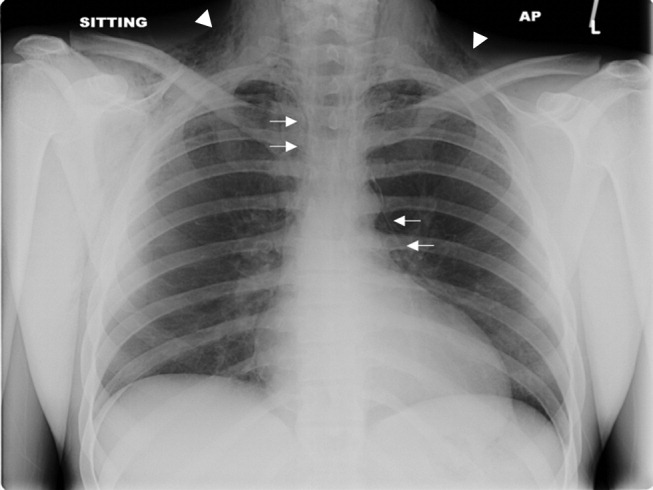
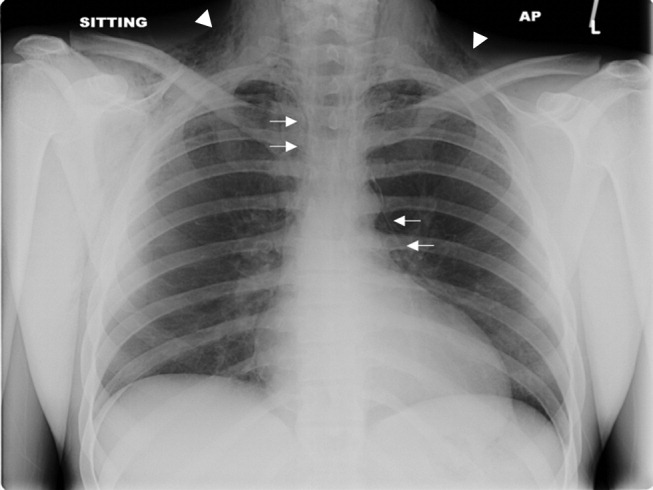
A previously healthy 22‐year‐old white man presented with acute psychosis after an 11‐day binge of smoking and injecting methamphetamine. The physical exam revealed crepitus over the anterior neck and Hamman's crunch (a crunching sound synchronous with the cardiac cycle and best heard with patient positioned in the left lateral decubitus position). Chest film (Fig. 1) and computerized tomography (Fig. 2) showed pneumomediastinum with extensive subcutaneous emphysema and pneumorrhachis (air in the epidural space).1 An esophogram was normal. Following 48 hours of inpatient observation and oxygen therapy, the neumomediastinum and psychosis resolved.

Spontaneous pneumomediastinum is rare, accounting for 1 in 30,000 emergency department referrals. It is more common among users of illicit substances (ie, amphetamine and methylenedioxymethamphetamine [MDMA/ecstasy]).2 Patients present with chest pain, dyspnea, and the typical physical findings described above.3 Chest imaging confirms the diagnosis.4 Vigorous inhalation during a Valsalva maneuver is thought to rupture terminal alveoli. Gas then enters the lung interstitium and dissects along fascial planes into the hilum and mediastinum and occasionally into the epidural space.5 Thorough investigation rules out other sources of air from the neck, abdomen, or ruptured esophagus (Boerhaave syndrome). Treatment is generally supportive and includes oxygen therapy, reassurance, analgesics, and close monitoring for complications (eg, pneumothorax). Surgical intervention is only necessary if a pneumothorax develops.6 Prognosis is excellent.
- .Spontaneous mediastinal emphysema.Bull Johns Hopkins Hosp.1939;64:1–21.
- ,.Spontaneous pneumomediastinum: a benign curiosity or a significant problem?Chest.2005;3298–3302128.
- ,.Spontaneous pneumomediastinum, pneumothorax and ecstasy abuse.Emerg Med.:2001;13:121–123.
- ,,,,.“Spontaneous Pneumomediastinum.Ann Thorac Surg.2004;78:711–713.
- ,,.Pneumorrhachis secondary to traumatic pneumomediastinum in a child.Pediatr Radiol.2006;36:711–713.
- ,,.Spontaneous pneumomediastinum.Curr Surg.2006;63:351–353.
A previously healthy 22‐year‐old white man presented with acute psychosis after an 11‐day binge of smoking and injecting methamphetamine. The physical exam revealed crepitus over the anterior neck and Hamman's crunch (a crunching sound synchronous with the cardiac cycle and best heard with patient positioned in the left lateral decubitus position). Chest film (Fig. 1) and computerized tomography (Fig. 2) showed pneumomediastinum with extensive subcutaneous emphysema and pneumorrhachis (air in the epidural space).1 An esophogram was normal. Following 48 hours of inpatient observation and oxygen therapy, the neumomediastinum and psychosis resolved.

Spontaneous pneumomediastinum is rare, accounting for 1 in 30,000 emergency department referrals. It is more common among users of illicit substances (ie, amphetamine and methylenedioxymethamphetamine [MDMA/ecstasy]).2 Patients present with chest pain, dyspnea, and the typical physical findings described above.3 Chest imaging confirms the diagnosis.4 Vigorous inhalation during a Valsalva maneuver is thought to rupture terminal alveoli. Gas then enters the lung interstitium and dissects along fascial planes into the hilum and mediastinum and occasionally into the epidural space.5 Thorough investigation rules out other sources of air from the neck, abdomen, or ruptured esophagus (Boerhaave syndrome). Treatment is generally supportive and includes oxygen therapy, reassurance, analgesics, and close monitoring for complications (eg, pneumothorax). Surgical intervention is only necessary if a pneumothorax develops.6 Prognosis is excellent.
A previously healthy 22‐year‐old white man presented with acute psychosis after an 11‐day binge of smoking and injecting methamphetamine. The physical exam revealed crepitus over the anterior neck and Hamman's crunch (a crunching sound synchronous with the cardiac cycle and best heard with patient positioned in the left lateral decubitus position). Chest film (Fig. 1) and computerized tomography (Fig. 2) showed pneumomediastinum with extensive subcutaneous emphysema and pneumorrhachis (air in the epidural space).1 An esophogram was normal. Following 48 hours of inpatient observation and oxygen therapy, the neumomediastinum and psychosis resolved.

Spontaneous pneumomediastinum is rare, accounting for 1 in 30,000 emergency department referrals. It is more common among users of illicit substances (ie, amphetamine and methylenedioxymethamphetamine [MDMA/ecstasy]).2 Patients present with chest pain, dyspnea, and the typical physical findings described above.3 Chest imaging confirms the diagnosis.4 Vigorous inhalation during a Valsalva maneuver is thought to rupture terminal alveoli. Gas then enters the lung interstitium and dissects along fascial planes into the hilum and mediastinum and occasionally into the epidural space.5 Thorough investigation rules out other sources of air from the neck, abdomen, or ruptured esophagus (Boerhaave syndrome). Treatment is generally supportive and includes oxygen therapy, reassurance, analgesics, and close monitoring for complications (eg, pneumothorax). Surgical intervention is only necessary if a pneumothorax develops.6 Prognosis is excellent.
- .Spontaneous mediastinal emphysema.Bull Johns Hopkins Hosp.1939;64:1–21.
- ,.Spontaneous pneumomediastinum: a benign curiosity or a significant problem?Chest.2005;3298–3302128.
- ,.Spontaneous pneumomediastinum, pneumothorax and ecstasy abuse.Emerg Med.:2001;13:121–123.
- ,,,,.“Spontaneous Pneumomediastinum.Ann Thorac Surg.2004;78:711–713.
- ,,.Pneumorrhachis secondary to traumatic pneumomediastinum in a child.Pediatr Radiol.2006;36:711–713.
- ,,.Spontaneous pneumomediastinum.Curr Surg.2006;63:351–353.
- .Spontaneous mediastinal emphysema.Bull Johns Hopkins Hosp.1939;64:1–21.
- ,.Spontaneous pneumomediastinum: a benign curiosity or a significant problem?Chest.2005;3298–3302128.
- ,.Spontaneous pneumomediastinum, pneumothorax and ecstasy abuse.Emerg Med.:2001;13:121–123.
- ,,,,.“Spontaneous Pneumomediastinum.Ann Thorac Surg.2004;78:711–713.
- ,,.Pneumorrhachis secondary to traumatic pneumomediastinum in a child.Pediatr Radiol.2006;36:711–713.
- ,,.Spontaneous pneumomediastinum.Curr Surg.2006;63:351–353.