User login
Outcomes Following Implementation of a Hospital-Wide, Multicomponent Delirium Care Pathway
Delirium is an acute disturbance in mental status characterized by fluctuations in cognition and attention that affects more than 2.6 million hospitalized older adults in the United States annually, a rate that is expected to increase as the population ages.1-4 Hospital-acquired delirium is associated with poor outcomes, including prolonged hospital length of stay (LOS), loss of independence, cognitive impairment, and even death.5-10 Individuals who develop delirium do poorly after hospital discharge and are more likely to be readmitted within 30 days.11 Approximately 30% to 40% of hospital-acquired delirium cases are preventable.10,12 However, programs designed to prevent delirium and associated complications, such as increased LOS, have demonstrated variable success.12-14 Many studies are limited by small sample sizes, lack of generalizability to different hospitalized patient populations, poor adherence, or reliance on outside funding.12,13,15-18
Delirium prevention programs face several challenges because delirium could be caused by a variety of risk factors and precipitants.19,20 Some risk factors that occur frequently among hospitalized patients can be mitigated, such as sensory impairment, immobility from physical restraints or urinary catheters, and polypharmacy.20,21 Effective delirium care pathways targeting these risk factors must be multifaceted, interdisciplinary, and interprofessional. Accurate risk assessment is critical to allocate resources to high-risk patients. Delirium affects patients in all medical and surgical disciplines, and often is underdiagnosed.19,22 Comprehensive screening is necessary to identify cases early and track outcomes, and educational efforts must reach all providers in the hospital. These challenges require a systematic, pragmatic approach to change.
The purpose of this study was to evaluate the association between a delirium care pathway and clinical outcomes for hospitalized patients. We hypothesized that this program would be associated with reduced hospital LOS, with secondary benefits to hospitalization costs, odds of 30-day readmission, and delirium rates.
METHODS
Study Design
In this retrospective cohort study, we compared clinical outcomes the year before and after implementation of a delirium care pathway across seven hospital units. The study period spanned October 1, 2015, through February 28, 2019. The study was approved by the University of California, San Francisco Institutional Review Board (#13-12500).
Multicomponent Delirium Care Pathway
The delirium care pathway was developed collaboratively among geriatrics, hospital medicine, neurology, anesthesiology, surgery, and psychiatry services, with an interprofessional team of physicians, nurses, pharmacists, and physical and occupational therapists. This pathway was implemented in units consecutively, approximately every 4 months in the following order: neurosciences, medicine, cardiology, general surgery, specialty surgery, hematology-oncology, and transplant. The same implementation education protocols were performed in each unit. The pathway consisted of several components targeting delirium prevention and management (Appendix Figure 1 and Appendix Figure 2). Systematic screening for delirium was introduced as part of the multicomponent intervention. Nursing staff assessed each patient’s risk of developing delirium at admission using the AWOL score, a validated delirium prediction tool.23 AWOL consists of: patient Age, spelling “World” backwards correctly, Orientation, and assessment of iLlness severity by the nurse. For patients who spoke a language other than English, spelling of “world” backwards was translated to his or her primary language, or if this was not possible, the task was modified to serial 7s (subtracting 7 from 100 in a serial fashion). This modification has been validated for use in other languages.24 Patients at high risk for delirium based on an AWOL score ≥2 received a multidisciplinary intervention with four components: (1) notifying the primary team by pager and electronic medical record (EMR), (2) a nurse-led, evidence-based, nonpharmacologic multicomponent intervention,25 (3) placement of a delirium order set by the physician, and (4) review of medications by the unit pharmacist who adjusted administration timing to occur during waking hours and placed a note in the EMR notifying the primary team of potentially deliriogenic medications. The delirium order set reinforced the nonpharmacologic multicomponent intervention through a nursing order, placed an automatic consult to occupational therapy, and included options to order physical therapy, order speech/language therapy, obtain vital signs three times daily with minimal night interruptions, remove an indwelling bladder catheter, and prescribe melatonin as a sleep aid.
The bedside nurse screened all patients for active delirium every 12-hour shift using the Nursing Delirium Screening Scale (NuDESC) and entered the results into the EMR.23,26 Capturing NuDESC results in the EMR allowed communication across medical providers as well as monitoring of screening adherence. Each nurse received two in-person trainings in staff meetings and one-to-one instruction during the first week of implementation. All nurses were required to complete a 15-minute training module and had the option of completing an additional 1-hour continuing medical education module. If a patient was transferred to the intensive care unit (ICU), delirium was identified through use of the ICU-specific Confusion Assessment Method (CAM-ICU) assessments, which the bedside nurse performed each shift throughout the intervention period.27 Nurses were instructed to call the primary team physician after every positive screen. Before each unit’s implementation start date, physicians with patients on that unit received education through a combination of grand rounds, resident lectures and seminars, and a pocket card on delirium evaluation and management.
Participants and Eligibility Criteria
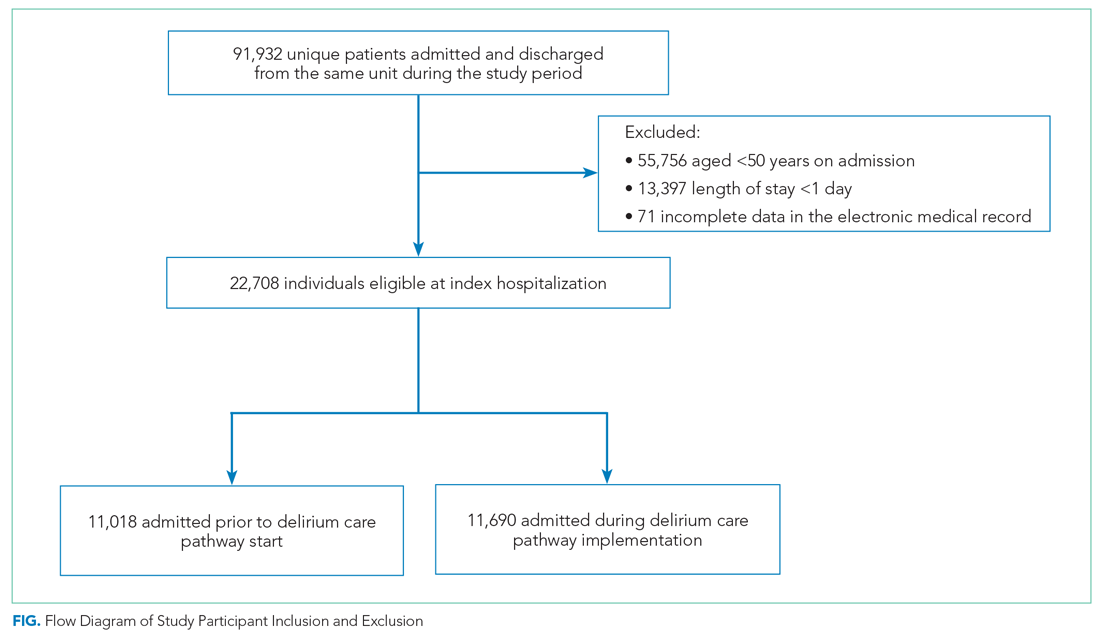
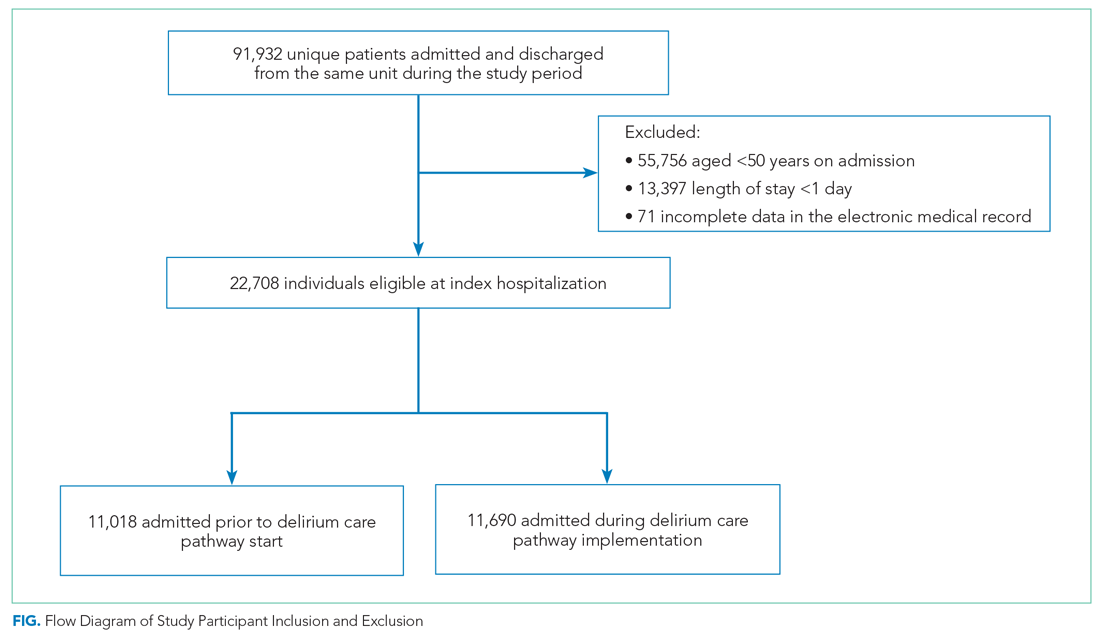
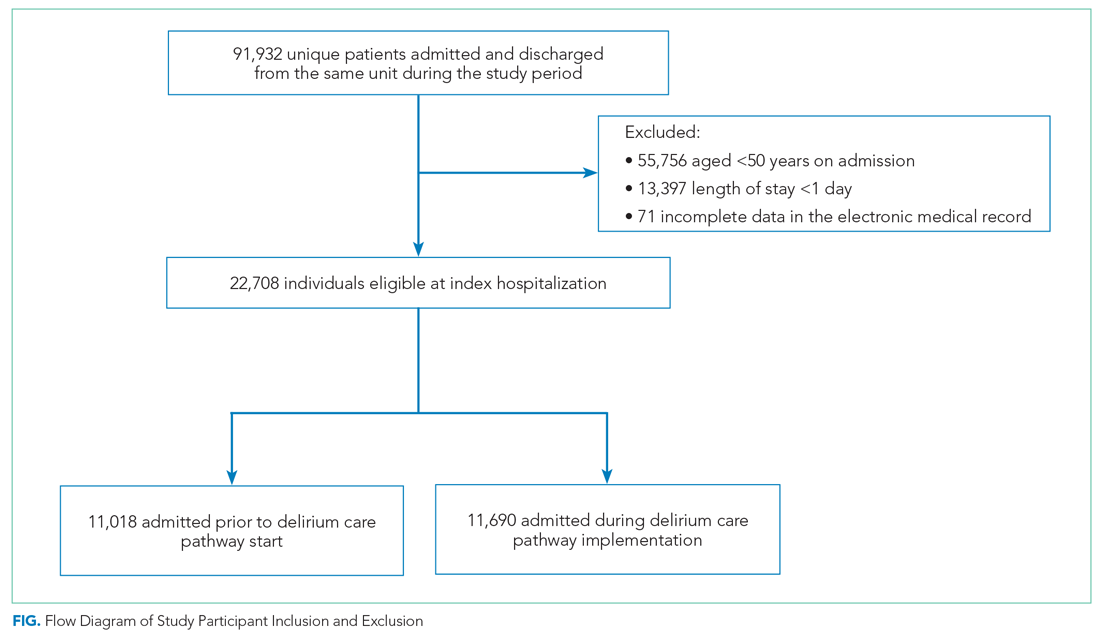
We included all patients aged ≥50 years hospitalized for >1 day on each hospital unit (Figure). We included adults aged ≥50 years to maximize the number of participants for this study while also capturing a population at risk for delirium. Because the delirium care pathway was unit-based and the pathway was rolled out sequentially across units, only patients who were admitted to and discharged from the same unit were included to better isolate the effect of the pathway. Patients who were transferred to the ICU were only included if they were discharged from the original unit of admission. Only the first hospitalization was included for patients with multiple hospitalizations during the study period.
Patient Characteristics
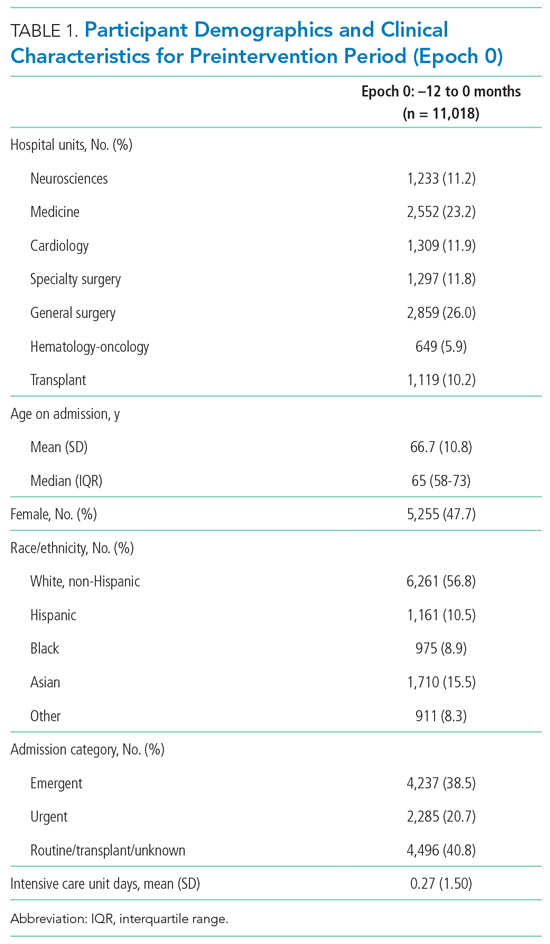
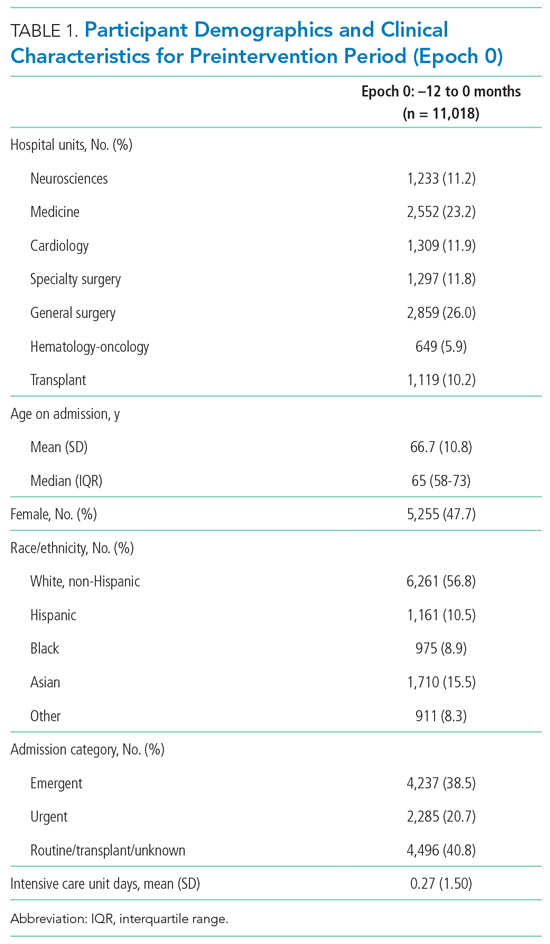
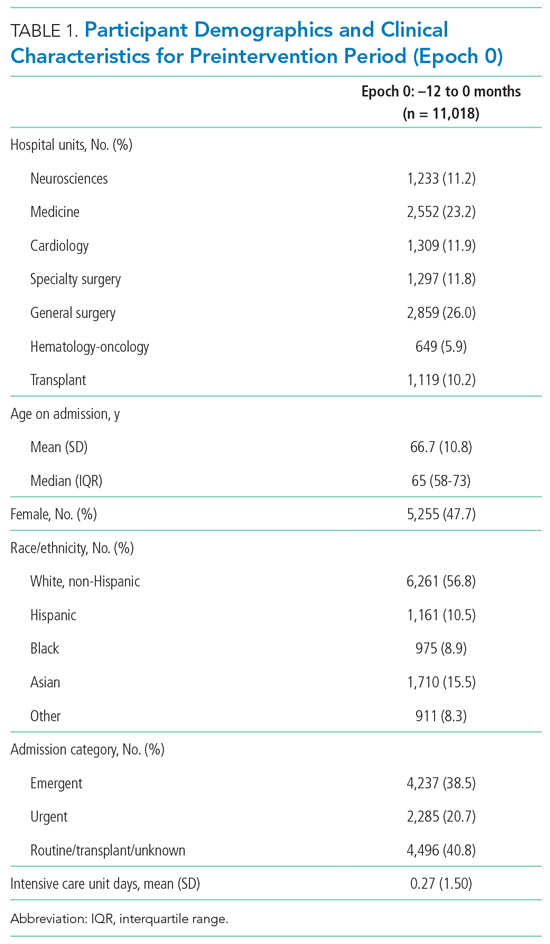
Patient demographics and clinical data were collected after discharge through Clarity and Vizient electronic databases (Table 1 and Table 2). All Elixhauser comorbidities were included except for the following International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10) codes that overlapped with a delirium diagnosis: G31.2, G93.89, G93.9, G94, R41.0, and R41.82 (Appendix Table 1). Severity of illness was obtained from Vizient, which calculates illness severity based on clinical and claims data (Appendix Table 1).
Delirium Metrics
Delirium screening was introduced as part of the multicomponent intervention, and therefore delirium rates before the intervention could not be determined. Trends in delirium prevalence and incidence after the intervention are reported. Prevalent delirium was defined as a single score of ≥2 on the nurse-administered NuDESC or a positive CAM-ICU at any point during the hospital stay. Incident delirium was identified if the first NuDESC score was negative and any subsequent NuDESC or CAM-ICU score was positive.

Outcomes
The primary study outcome was hospital LOS across all participants. Secondary outcomes included total direct cost and odds of 30-day hospital readmission. Readmissions tracked as part of hospital quality reporting were obtained from Vizient and were not captured if they occurred at another hospital. We also examined rates of safety attendant and restraint use during the study period, defined as the number of safety attendant days or restraint days per 1,000 patient days.
Because previous studies have demonstrated the effectiveness of multicomponent delirium interventions among elderly general medical patients,12 we also investigated these same outcomes in the medicine unit alone.
Statistical Analysis
The date of intervention implementation was determined for each hospital unit, which was defined as time(0) [t(0)]. The 12-month postintervention period was divided into four 3-month epochs to assess for trends. Data were aggregated across the seven units using t(0) as the start date, agnostic to the calendar month. Demographic and clinical characteristics were collected for the 12-months before t(0) and the four 3-month epochs after t(0). Univariate analysis of outcome variables comparing trends across the same epochs were conducted in the same manner, except for the rate of delirium, which was measured after t(0) and therefore could not be compared with the preintervention period.
Multivariable models were adjusted for age, sex, race/ethnicity, admission category, Elixhauser comorbidities, severity of illness quartile, and number days spent in the ICU. Admission category referred to whether the admission was emergent, urgent, or elective/unknown. Because it took 3 months after t(0) for each unit to reach a delirium screening compliance rate of 90%, the intervention was only considered fully implemented after this period. A ramp-up variable was set to 0 for admissions occurring prior to the intervention to t(0), 1/3 for admissions occurring 1 month post intervention, 2/3 for 2 months post intervention, and 1 for admissions occurring 3 to 12 months post intervention. In this way, the coefficient for the ramp-up variable estimated the postintervention versus preintervention effect. Numerical outcomes (LOS, cost) were log transformed to reduce skewness and analyzed using linear models. Coefficients were back-transformed to provide interpretations as proportional change in the median outcomes.
For LOS and readmission, we assessed secular trends by including admission date and admission date squared, in case the trend was nonlinear, as possible predictors; admission date was the specific date—not time from t(0)—to account for secular trends and allow contemporaneous controls in the analysis. To be conservative, we retained secular terms (first considering the quadratic and then the linear) if P <.10. The categorical outcome (30-day readmission) was analyzed using a logistic model. Count variables (delirium, safety attendants, restraints) were analyzed using Poisson regression models with a log link, and coefficients were back-transformed to provide rate ratio interpretations. Because delirium was not measured before t(0), and because the intervention was considered to take 3 months to become fully effective, baseline delirium rates were defined as those in the first 3 months adjusted by the ramp-up variable. For each outcome we included hospital unit, a ramp-up variable (measuring the pre- vs postintervention effect), and their interaction. If there was no statistically significant interaction, we presented the outcome for all units combined. If the interaction was statistically significant, we looked for consistency across units and reported results for all units combined when consistent, along with site-specific results. If the results were not consistent across the units, we provided site-specific results only. All statistical analyses were performed using SAS software, version 9.4 (SAS Institute Inc).
RESULTS
Participant Demographics and Clinical Characteristics
A total of 22,708 individuals were included in this study, with 11,018 in the preintervention period (Table 1 and Table 2). Most patients were cared for on the general surgery unit (n = 5,899), followed by the medicine unit (n = 4,923). The smallest number of patients were cared for on the hematology-oncology unit (n = 1,709). Across the five epochs, patients were of similar age and sex, and spent a similar number of days in the ICU. The population was diverse with regard to race and ethnicity; there were minor differences in admission category. There were also minor differences in severity of illness and some comorbidities between timepoints (Appendix Table 1).
Delirium Metrics
Delirium prevalence was 13.0% during the first epoch post intervention, followed by 12.0%, 11.7%, and 13.0% in the subsequent epochs (P = .91). Incident delirium occurred in 6.1% of patients during the first epoch post intervention, followed by 5.3%, 5.3%, and 5.8% in the subsequent epochs (P = .63).
Primary Outcome
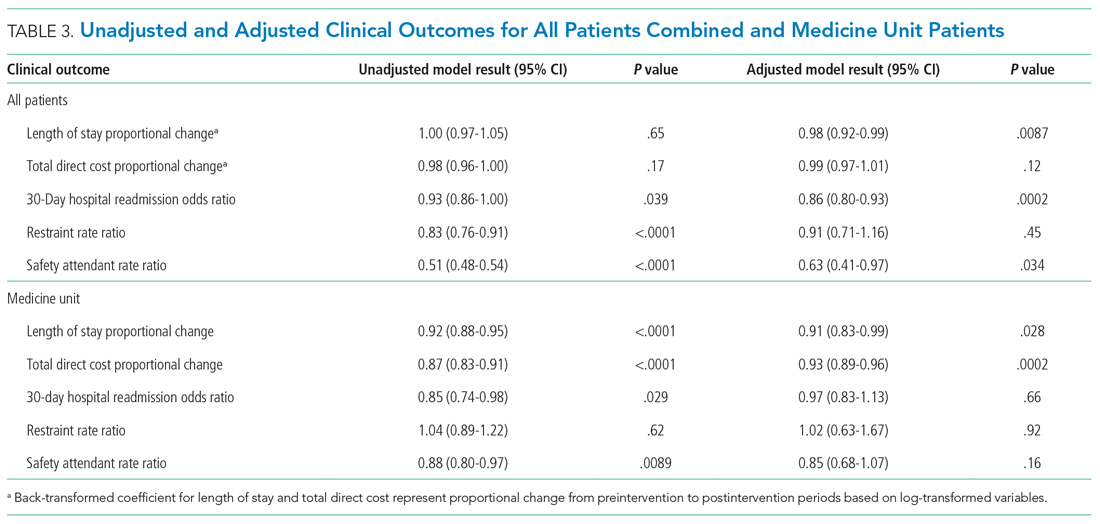
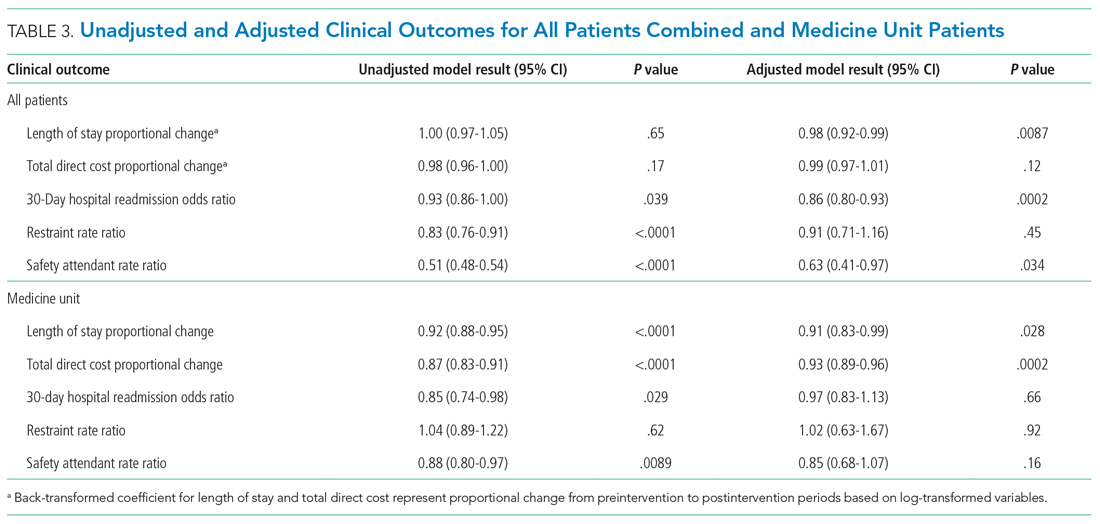
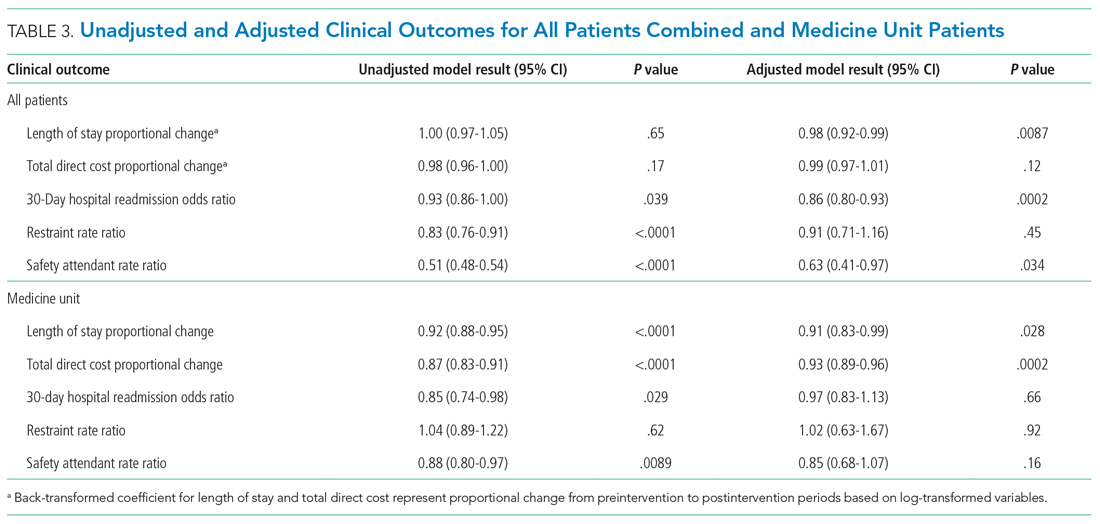
Epoch-level data for LOS before and after the intervention is shown in Appendix Table 2. The mean unadjusted LOS for all units combined did not decrease after the intervention, but in the adjusted model, the mean LOS decreased by 2% after the intervention (P = .0087; Table 3).
Secondary Outcomes
The odds of 30-day readmission decreased by 14% (P = .0002) in the adjusted models for all units combined (Table 3). There was no statistically significant reduction in adjusted total direct hospitalization cost or rate of restraint use. The safety attendant results showed strong effect modification across sites; the site-specific estimates are provided in Appendix Table 3. However, the estimated values all showed reductions, and a number were large and statistically significant.
Medicine Unit Outcomes
On the medicine unit alone, we observed a statistically significant reduction in LOS of 9% after implementation of the delirium care pathway (P = .028) in the adjusted model (Table 3). There was an associated 7% proportional decrease in total direct cost (P = .0002). Reductions in 30-day readmission and safety attendant use did not remain statistically significant in the adjusted models.
DISCUSSION
Implementation of a hospital-wide multicomponent delirium care pathway was associated with reduced hospital LOS and 30-day hospital readmission in a study of 22,708 hospitalized adults at a tertiary care, university hospital in Northern California, encompassing both medical and surgical acute care patients. When evaluating general medicine patients alone, pathway implementation was associated with reductions in LOS and total direct cost. The cost savings of 7% among medical patients translates to median savings of $1,237 per hospitalization. This study—one of the largest to date examining implementation of a hospital-wide delirium care pathway—supports use of a multicomponent delirium care pathway for older adults hospitalized for a range of conditions.
Multicomponent pathways for delirium prevention and management are increasingly being used in hospital settings. The United Kingdom National Institute for Health and Care Excellence guidelines recommend delirium assessment and intervention by a multidisciplinary team within 24 hours of hospital admission for those at risk.25 These guidelines are based on evidence accumulated in clinical studies over the past 30 years suggesting that multicomponent interventions reduce incident delirium by 30% to 40% among medical and surgical patients.12,13,25,28
Although multicomponent delirium care pathways are associated with improved patient outcomes, the specific clinical benefits might vary across patient populations. Here, we found larger reductions in LOS and total direct cost among medicine patients. Medical patients might respond more robustly to nonpharmacologic multicomponent delirium interventions because of differing delirium etiologies (eg, constipation and sleep deprivation in a medical patient vs seizures or encephalitis in a neurosciences patient). Another explanation for the difference observed in total direct cost might be the inclusion of surgical units in the total study population. For example, not all hospital days are equivalent in cost for patients on a surgical unit.29 For patients requiring surgical care, most of the hospitalization cost might be incurred during the initial days of hospitalization, when there are perioperative costs; therefore, reduced LOS might have a lower economic impact.29 Multicomponent, nonpharmacologic delirium interventions encourage discontinuing restraints. As a result, one might expect a need for more frequent safety attendant use and an associated cost increase. However, we found that the estimated unit-specific values for safety attendant use showed reductions, which were large and highly statistically significant. For all units combined and the medicine unit alone, we found that the rate of restraint use decreased, although the change was not statistically significant. It is possible that some of the interventions taught to nurses and physicians as part of care pathway implementation, such as the use of family support for at-risk and delirious patients, led to a reduction in both safety attendants and restraints.
Our study had several strengths. This is one of the largest hospital-based delirium interventions studied, both in terms of its scope across seven diverse medical and surgical hospital units and the number of hospitalized patients studied. This intervention did not require additional staff or creating a specialized ward. Adherence to the pathway, as measured by risk assessment and delirium screening, was high (>90%) 3 months after implementation. This allowed for robust outcome ascertainment. The patient population’s characteristics and rates of delirium were stable over time. Because different hospital units incorporated the multicomponent delirium care pathway at different times, limiting enrollment to patients admitted and discharged from the same unit isolated the analysis to patients exposed to the pathway on each unit. This design also limited potential influence of other hospital quality improvement projects that might have occurred at the same time.
The primary limitation of this study is that screening for delirium was introduced as part of the multicomponent intervention. This decision was made to maximize buy-in from bedside nurses performing delirium screening because this addition to their workflow was explicitly linked to delirium prevention and management measures. Delirium could not be ascertained preintervention from the EMR because it is a clinical diagnosis and is coded inadequately.30 We could only measure the change in delirium metrics after implementation of the delirium care pathway. Because baseline delirium rates before the intervention were not measured systematically, conclusions about the intervention’s association with delirium metrics are limited. All other outcomes were measured before and after the intervention.
Although the comprehensive delirium screening program and high rate of adherence are a methodologic strength of this study, a second limitation is the use of the NuDESC. Our previous research demonstrated that the NuDESC has low sensitivity but high specificity and positive predictive value,26 which might underestimate delirium rates in this study. However, any underestimation should be stable over time and temporal trends should remain meaningful. This could allow more widespread study of delirium among hospitalized individuals. Because this care pathway was hospital-wide, it was important to ensure both consistency of screening and longevity of the initiative, and it was necessary to select a delirium assessment tool that was efficient and validated for nursing implementation. For these reasons, the NuDESC was an appropriate choice.
It is possible that our results could be influenced by unmeasured confounders. For example, although we incorporated Elixhauser medical comorbidities and illness severity into our model, we were unable to adjust for baseline functional status or frailty. Baseline functional status and frailty were not reliably recorded in the EMR, although these are potential confounders when investigating clinical outcomes including hospital readmission.
CONCLUSION
Implementation of a systematic, hospital-wide multicomponent delirium care pathway is associated with reductions in hospital LOS and 30-day readmission. In general medicine units, the reduction in LOS and associated cost savings were robust. These results demonstrate the feasibility and effectiveness of implementing an interprofessional, multidisciplinary multicomponent delirium care pathway through medical center funding to benefit patients and the hospital system.
Acknowledgments
The authors thank the many hospital staff members, especially the nurses, pharmacists, therapists, and patient care assistants, who helped implement the multicomponent delirium care pathway. All persons who have contributed significantly to this work are listed as authors of this work.
1. Bidwell J. Interventions for preventing delirium in hospitalized non-ICU patients: A Cochrane review summary. Int J Nurs Stud. 2017;70:142-143. https://doi.org/ 10.1016/j.ijnurstu.2016.11.010
2. Maldonado JR. Delirium in the acute care setting: characteristics, diagnosis and treatment. Crit Care Clin. 2008;24(4):657-722, vii. https://doi.org/10.1016/j.ccc.2008.05.008
3. Field RR, Wall MH. Delirium: past, present, and future. Semin Cardiothorac Vasc Anesth. 2013;17(3):170-179. https://doi.org/10.1177/1089253213476957
4. Oh ST, Park JY. Postoperative delirium. Korean J Anesthesiol. 2019;72(1):4-12. https://doi.org/10.4097/kja.d.18.00073.1
5. Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990;263(8):1097-1101.
6. Salluh JI, Soares M, Teles JM, et al. Delirium epidemiology in critical care (DECCA): an international study. Crit Care. 2010;14(6):R210. https://doi.org/10.1186/cc9333
7. Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753-1762. https://doi.org/
8. McCusker J, Cole MG, Dendukuri N, Belzile E. Does delirium increase hospital stay? J Am Geriatr Soc. 2003;51(11):1539-1546. https://doi.org/10.1001/jama.291.14.1753
9. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242. https://doi.org/10.1046/j.1525-1497.1998.00073.x
10. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364. https://doi.org/10.1093/ageing/afl005
11. LaHue SC, Douglas VC, Kuo T, et al. Association between inpatient delirium and hospital readmission in patients >/= 65 years of age: a retrospective cohort study. J Hosp Med. 2019;14(4):201-206. https://doi.org/10.12788/jhm.3130
12. Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512-520. https://doi.org/10.1001/jamainternmed.2014.7779
13. Inouye SK, Bogardus ST, Jr., Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669-676. https://doi.org/10.1056/NEJM199903043400901
14. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516-522. https://doi.org/
15. Alhaidari AA, Allen-Narker RA. An evolving approach to delirium: A mixed-methods process evaluation of a hospital-wide delirium program in New Zealand. Australas J Ageing. 2017. https://doi.org/10.1046/j.1532-5415.2001.49108.x
16. Holroyd-Leduc JM, Khandwala F, Sink KM. How can delirium best be prevented and managed in older patients in hospital? CMAJ. 2010;182(5):465-470. https://doi.org/10.1503/cmaj.080519
17. Siddiqi N, Stockdale R, Britton AM, Holmes J. Interventions for preventing delirium in hospitalised patients. Cochrane Database Syst Rev. 2007(2):CD005563. https://doi.org/ 10.1002/14651858.CD005563.pub2
18. Siddiqi N, Harrison JK, Clegg A, et al. Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2016;3:CD005563. https://doi.org/10.1002/14651858.CD005563.pub3
19. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922. https://doi.org/10.1016/S0140-6736(13)60688-1
20. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857.
21. LaHue SC, Liu VX. Loud and clear: sensory impairment, delirium, and functional recovery in critical illness. Am J Respir Crit Care Med. 2016;194(3):252-253. https://doi.org/10.1164/rccm.201602-0372ED
22. Ritter SRF, Cardoso AF, Lins MMP, Zoccoli TLV, Freitas MPD, Camargos EF. Underdiagnosis of delirium in the elderly in acute care hospital settings: lessons not learned. Psychogeriatrics. 2018;18(4):268-275. https://doi.org/10.1111/psyg.12324
23. Douglas VC, Hessler CS, Dhaliwal G, et al. The AWOL tool: derivation and validation of a delirium prediction rule. J Hosp Med. 2013;8(9):493-499. https://doi.org/10.1002/jhm.2062
24. Tombaugh TN, McDowell I, Kristjansson B, Hubley AM. Mini-Mental State Examination (MMSE) and the modified MMSE (3MS): A psychometric comparison and normative data. Psychol Assessment. 1996;8(1):48-59. https://doi.org/10.1037/1040-3590.8.1.48
25. Young J, Murthy L, Westby M, Akunne A, O’Mahony R, Guideline Development Group. Diagnosis, prevention, and management of delirium: summary of NICE guidance. BMJ. 2010;341:c3704. https://doi.org/10.1136/bmj.c3704
26. Hargrave A, Bastiaens J, Bourgeois JA, et al. Validation of a nurse-based delirium-screening tool for hospitalized patients. Psychosomatics. 2017;58(6):594-603. https://doi.org/10.1016/j.psym.2017.05.005
27. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703-2710. https://doi.org/10.1001/jama.286.21.2703
28. Strijbos MJ, Steunenberg B, van der Mast RC, Inouye SK, Schuurmans MJ. Design and methods of the Hospital Elder Life Program (HELP), a multicomponent targeted intervention to prevent delirium in hospitalized older patients: efficacy and cost-effectiveness in Dutch health care. BMC Geriatr. 2013;13:78. https://doi.org/10.1186/1471-2318-13-78
29. Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg. 2000;191(2):123-130. https://doi.org/10.1016/s1072-7515(00)00352-5
30. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210-220. https://doi.org/10.1038/nrneurol.2009.24
Delirium is an acute disturbance in mental status characterized by fluctuations in cognition and attention that affects more than 2.6 million hospitalized older adults in the United States annually, a rate that is expected to increase as the population ages.1-4 Hospital-acquired delirium is associated with poor outcomes, including prolonged hospital length of stay (LOS), loss of independence, cognitive impairment, and even death.5-10 Individuals who develop delirium do poorly after hospital discharge and are more likely to be readmitted within 30 days.11 Approximately 30% to 40% of hospital-acquired delirium cases are preventable.10,12 However, programs designed to prevent delirium and associated complications, such as increased LOS, have demonstrated variable success.12-14 Many studies are limited by small sample sizes, lack of generalizability to different hospitalized patient populations, poor adherence, or reliance on outside funding.12,13,15-18
Delirium prevention programs face several challenges because delirium could be caused by a variety of risk factors and precipitants.19,20 Some risk factors that occur frequently among hospitalized patients can be mitigated, such as sensory impairment, immobility from physical restraints or urinary catheters, and polypharmacy.20,21 Effective delirium care pathways targeting these risk factors must be multifaceted, interdisciplinary, and interprofessional. Accurate risk assessment is critical to allocate resources to high-risk patients. Delirium affects patients in all medical and surgical disciplines, and often is underdiagnosed.19,22 Comprehensive screening is necessary to identify cases early and track outcomes, and educational efforts must reach all providers in the hospital. These challenges require a systematic, pragmatic approach to change.
The purpose of this study was to evaluate the association between a delirium care pathway and clinical outcomes for hospitalized patients. We hypothesized that this program would be associated with reduced hospital LOS, with secondary benefits to hospitalization costs, odds of 30-day readmission, and delirium rates.
METHODS
Study Design
In this retrospective cohort study, we compared clinical outcomes the year before and after implementation of a delirium care pathway across seven hospital units. The study period spanned October 1, 2015, through February 28, 2019. The study was approved by the University of California, San Francisco Institutional Review Board (#13-12500).
Multicomponent Delirium Care Pathway
The delirium care pathway was developed collaboratively among geriatrics, hospital medicine, neurology, anesthesiology, surgery, and psychiatry services, with an interprofessional team of physicians, nurses, pharmacists, and physical and occupational therapists. This pathway was implemented in units consecutively, approximately every 4 months in the following order: neurosciences, medicine, cardiology, general surgery, specialty surgery, hematology-oncology, and transplant. The same implementation education protocols were performed in each unit. The pathway consisted of several components targeting delirium prevention and management (Appendix Figure 1 and Appendix Figure 2). Systematic screening for delirium was introduced as part of the multicomponent intervention. Nursing staff assessed each patient’s risk of developing delirium at admission using the AWOL score, a validated delirium prediction tool.23 AWOL consists of: patient Age, spelling “World” backwards correctly, Orientation, and assessment of iLlness severity by the nurse. For patients who spoke a language other than English, spelling of “world” backwards was translated to his or her primary language, or if this was not possible, the task was modified to serial 7s (subtracting 7 from 100 in a serial fashion). This modification has been validated for use in other languages.24 Patients at high risk for delirium based on an AWOL score ≥2 received a multidisciplinary intervention with four components: (1) notifying the primary team by pager and electronic medical record (EMR), (2) a nurse-led, evidence-based, nonpharmacologic multicomponent intervention,25 (3) placement of a delirium order set by the physician, and (4) review of medications by the unit pharmacist who adjusted administration timing to occur during waking hours and placed a note in the EMR notifying the primary team of potentially deliriogenic medications. The delirium order set reinforced the nonpharmacologic multicomponent intervention through a nursing order, placed an automatic consult to occupational therapy, and included options to order physical therapy, order speech/language therapy, obtain vital signs three times daily with minimal night interruptions, remove an indwelling bladder catheter, and prescribe melatonin as a sleep aid.
The bedside nurse screened all patients for active delirium every 12-hour shift using the Nursing Delirium Screening Scale (NuDESC) and entered the results into the EMR.23,26 Capturing NuDESC results in the EMR allowed communication across medical providers as well as monitoring of screening adherence. Each nurse received two in-person trainings in staff meetings and one-to-one instruction during the first week of implementation. All nurses were required to complete a 15-minute training module and had the option of completing an additional 1-hour continuing medical education module. If a patient was transferred to the intensive care unit (ICU), delirium was identified through use of the ICU-specific Confusion Assessment Method (CAM-ICU) assessments, which the bedside nurse performed each shift throughout the intervention period.27 Nurses were instructed to call the primary team physician after every positive screen. Before each unit’s implementation start date, physicians with patients on that unit received education through a combination of grand rounds, resident lectures and seminars, and a pocket card on delirium evaluation and management.
Participants and Eligibility Criteria
We included all patients aged ≥50 years hospitalized for >1 day on each hospital unit (Figure). We included adults aged ≥50 years to maximize the number of participants for this study while also capturing a population at risk for delirium. Because the delirium care pathway was unit-based and the pathway was rolled out sequentially across units, only patients who were admitted to and discharged from the same unit were included to better isolate the effect of the pathway. Patients who were transferred to the ICU were only included if they were discharged from the original unit of admission. Only the first hospitalization was included for patients with multiple hospitalizations during the study period.
Patient Characteristics
Patient demographics and clinical data were collected after discharge through Clarity and Vizient electronic databases (Table 1 and Table 2). All Elixhauser comorbidities were included except for the following International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10) codes that overlapped with a delirium diagnosis: G31.2, G93.89, G93.9, G94, R41.0, and R41.82 (Appendix Table 1). Severity of illness was obtained from Vizient, which calculates illness severity based on clinical and claims data (Appendix Table 1).
Delirium Metrics
Delirium screening was introduced as part of the multicomponent intervention, and therefore delirium rates before the intervention could not be determined. Trends in delirium prevalence and incidence after the intervention are reported. Prevalent delirium was defined as a single score of ≥2 on the nurse-administered NuDESC or a positive CAM-ICU at any point during the hospital stay. Incident delirium was identified if the first NuDESC score was negative and any subsequent NuDESC or CAM-ICU score was positive.

Outcomes
The primary study outcome was hospital LOS across all participants. Secondary outcomes included total direct cost and odds of 30-day hospital readmission. Readmissions tracked as part of hospital quality reporting were obtained from Vizient and were not captured if they occurred at another hospital. We also examined rates of safety attendant and restraint use during the study period, defined as the number of safety attendant days or restraint days per 1,000 patient days.
Because previous studies have demonstrated the effectiveness of multicomponent delirium interventions among elderly general medical patients,12 we also investigated these same outcomes in the medicine unit alone.
Statistical Analysis
The date of intervention implementation was determined for each hospital unit, which was defined as time(0) [t(0)]. The 12-month postintervention period was divided into four 3-month epochs to assess for trends. Data were aggregated across the seven units using t(0) as the start date, agnostic to the calendar month. Demographic and clinical characteristics were collected for the 12-months before t(0) and the four 3-month epochs after t(0). Univariate analysis of outcome variables comparing trends across the same epochs were conducted in the same manner, except for the rate of delirium, which was measured after t(0) and therefore could not be compared with the preintervention period.
Multivariable models were adjusted for age, sex, race/ethnicity, admission category, Elixhauser comorbidities, severity of illness quartile, and number days spent in the ICU. Admission category referred to whether the admission was emergent, urgent, or elective/unknown. Because it took 3 months after t(0) for each unit to reach a delirium screening compliance rate of 90%, the intervention was only considered fully implemented after this period. A ramp-up variable was set to 0 for admissions occurring prior to the intervention to t(0), 1/3 for admissions occurring 1 month post intervention, 2/3 for 2 months post intervention, and 1 for admissions occurring 3 to 12 months post intervention. In this way, the coefficient for the ramp-up variable estimated the postintervention versus preintervention effect. Numerical outcomes (LOS, cost) were log transformed to reduce skewness and analyzed using linear models. Coefficients were back-transformed to provide interpretations as proportional change in the median outcomes.
For LOS and readmission, we assessed secular trends by including admission date and admission date squared, in case the trend was nonlinear, as possible predictors; admission date was the specific date—not time from t(0)—to account for secular trends and allow contemporaneous controls in the analysis. To be conservative, we retained secular terms (first considering the quadratic and then the linear) if P <.10. The categorical outcome (30-day readmission) was analyzed using a logistic model. Count variables (delirium, safety attendants, restraints) were analyzed using Poisson regression models with a log link, and coefficients were back-transformed to provide rate ratio interpretations. Because delirium was not measured before t(0), and because the intervention was considered to take 3 months to become fully effective, baseline delirium rates were defined as those in the first 3 months adjusted by the ramp-up variable. For each outcome we included hospital unit, a ramp-up variable (measuring the pre- vs postintervention effect), and their interaction. If there was no statistically significant interaction, we presented the outcome for all units combined. If the interaction was statistically significant, we looked for consistency across units and reported results for all units combined when consistent, along with site-specific results. If the results were not consistent across the units, we provided site-specific results only. All statistical analyses were performed using SAS software, version 9.4 (SAS Institute Inc).
RESULTS
Participant Demographics and Clinical Characteristics
A total of 22,708 individuals were included in this study, with 11,018 in the preintervention period (Table 1 and Table 2). Most patients were cared for on the general surgery unit (n = 5,899), followed by the medicine unit (n = 4,923). The smallest number of patients were cared for on the hematology-oncology unit (n = 1,709). Across the five epochs, patients were of similar age and sex, and spent a similar number of days in the ICU. The population was diverse with regard to race and ethnicity; there were minor differences in admission category. There were also minor differences in severity of illness and some comorbidities between timepoints (Appendix Table 1).
Delirium Metrics
Delirium prevalence was 13.0% during the first epoch post intervention, followed by 12.0%, 11.7%, and 13.0% in the subsequent epochs (P = .91). Incident delirium occurred in 6.1% of patients during the first epoch post intervention, followed by 5.3%, 5.3%, and 5.8% in the subsequent epochs (P = .63).
Primary Outcome
Epoch-level data for LOS before and after the intervention is shown in Appendix Table 2. The mean unadjusted LOS for all units combined did not decrease after the intervention, but in the adjusted model, the mean LOS decreased by 2% after the intervention (P = .0087; Table 3).
Secondary Outcomes
The odds of 30-day readmission decreased by 14% (P = .0002) in the adjusted models for all units combined (Table 3). There was no statistically significant reduction in adjusted total direct hospitalization cost or rate of restraint use. The safety attendant results showed strong effect modification across sites; the site-specific estimates are provided in Appendix Table 3. However, the estimated values all showed reductions, and a number were large and statistically significant.
Medicine Unit Outcomes
On the medicine unit alone, we observed a statistically significant reduction in LOS of 9% after implementation of the delirium care pathway (P = .028) in the adjusted model (Table 3). There was an associated 7% proportional decrease in total direct cost (P = .0002). Reductions in 30-day readmission and safety attendant use did not remain statistically significant in the adjusted models.
DISCUSSION
Implementation of a hospital-wide multicomponent delirium care pathway was associated with reduced hospital LOS and 30-day hospital readmission in a study of 22,708 hospitalized adults at a tertiary care, university hospital in Northern California, encompassing both medical and surgical acute care patients. When evaluating general medicine patients alone, pathway implementation was associated with reductions in LOS and total direct cost. The cost savings of 7% among medical patients translates to median savings of $1,237 per hospitalization. This study—one of the largest to date examining implementation of a hospital-wide delirium care pathway—supports use of a multicomponent delirium care pathway for older adults hospitalized for a range of conditions.
Multicomponent pathways for delirium prevention and management are increasingly being used in hospital settings. The United Kingdom National Institute for Health and Care Excellence guidelines recommend delirium assessment and intervention by a multidisciplinary team within 24 hours of hospital admission for those at risk.25 These guidelines are based on evidence accumulated in clinical studies over the past 30 years suggesting that multicomponent interventions reduce incident delirium by 30% to 40% among medical and surgical patients.12,13,25,28
Although multicomponent delirium care pathways are associated with improved patient outcomes, the specific clinical benefits might vary across patient populations. Here, we found larger reductions in LOS and total direct cost among medicine patients. Medical patients might respond more robustly to nonpharmacologic multicomponent delirium interventions because of differing delirium etiologies (eg, constipation and sleep deprivation in a medical patient vs seizures or encephalitis in a neurosciences patient). Another explanation for the difference observed in total direct cost might be the inclusion of surgical units in the total study population. For example, not all hospital days are equivalent in cost for patients on a surgical unit.29 For patients requiring surgical care, most of the hospitalization cost might be incurred during the initial days of hospitalization, when there are perioperative costs; therefore, reduced LOS might have a lower economic impact.29 Multicomponent, nonpharmacologic delirium interventions encourage discontinuing restraints. As a result, one might expect a need for more frequent safety attendant use and an associated cost increase. However, we found that the estimated unit-specific values for safety attendant use showed reductions, which were large and highly statistically significant. For all units combined and the medicine unit alone, we found that the rate of restraint use decreased, although the change was not statistically significant. It is possible that some of the interventions taught to nurses and physicians as part of care pathway implementation, such as the use of family support for at-risk and delirious patients, led to a reduction in both safety attendants and restraints.
Our study had several strengths. This is one of the largest hospital-based delirium interventions studied, both in terms of its scope across seven diverse medical and surgical hospital units and the number of hospitalized patients studied. This intervention did not require additional staff or creating a specialized ward. Adherence to the pathway, as measured by risk assessment and delirium screening, was high (>90%) 3 months after implementation. This allowed for robust outcome ascertainment. The patient population’s characteristics and rates of delirium were stable over time. Because different hospital units incorporated the multicomponent delirium care pathway at different times, limiting enrollment to patients admitted and discharged from the same unit isolated the analysis to patients exposed to the pathway on each unit. This design also limited potential influence of other hospital quality improvement projects that might have occurred at the same time.
The primary limitation of this study is that screening for delirium was introduced as part of the multicomponent intervention. This decision was made to maximize buy-in from bedside nurses performing delirium screening because this addition to their workflow was explicitly linked to delirium prevention and management measures. Delirium could not be ascertained preintervention from the EMR because it is a clinical diagnosis and is coded inadequately.30 We could only measure the change in delirium metrics after implementation of the delirium care pathway. Because baseline delirium rates before the intervention were not measured systematically, conclusions about the intervention’s association with delirium metrics are limited. All other outcomes were measured before and after the intervention.
Although the comprehensive delirium screening program and high rate of adherence are a methodologic strength of this study, a second limitation is the use of the NuDESC. Our previous research demonstrated that the NuDESC has low sensitivity but high specificity and positive predictive value,26 which might underestimate delirium rates in this study. However, any underestimation should be stable over time and temporal trends should remain meaningful. This could allow more widespread study of delirium among hospitalized individuals. Because this care pathway was hospital-wide, it was important to ensure both consistency of screening and longevity of the initiative, and it was necessary to select a delirium assessment tool that was efficient and validated for nursing implementation. For these reasons, the NuDESC was an appropriate choice.
It is possible that our results could be influenced by unmeasured confounders. For example, although we incorporated Elixhauser medical comorbidities and illness severity into our model, we were unable to adjust for baseline functional status or frailty. Baseline functional status and frailty were not reliably recorded in the EMR, although these are potential confounders when investigating clinical outcomes including hospital readmission.
CONCLUSION
Implementation of a systematic, hospital-wide multicomponent delirium care pathway is associated with reductions in hospital LOS and 30-day readmission. In general medicine units, the reduction in LOS and associated cost savings were robust. These results demonstrate the feasibility and effectiveness of implementing an interprofessional, multidisciplinary multicomponent delirium care pathway through medical center funding to benefit patients and the hospital system.
Acknowledgments
The authors thank the many hospital staff members, especially the nurses, pharmacists, therapists, and patient care assistants, who helped implement the multicomponent delirium care pathway. All persons who have contributed significantly to this work are listed as authors of this work.
Delirium is an acute disturbance in mental status characterized by fluctuations in cognition and attention that affects more than 2.6 million hospitalized older adults in the United States annually, a rate that is expected to increase as the population ages.1-4 Hospital-acquired delirium is associated with poor outcomes, including prolonged hospital length of stay (LOS), loss of independence, cognitive impairment, and even death.5-10 Individuals who develop delirium do poorly after hospital discharge and are more likely to be readmitted within 30 days.11 Approximately 30% to 40% of hospital-acquired delirium cases are preventable.10,12 However, programs designed to prevent delirium and associated complications, such as increased LOS, have demonstrated variable success.12-14 Many studies are limited by small sample sizes, lack of generalizability to different hospitalized patient populations, poor adherence, or reliance on outside funding.12,13,15-18
Delirium prevention programs face several challenges because delirium could be caused by a variety of risk factors and precipitants.19,20 Some risk factors that occur frequently among hospitalized patients can be mitigated, such as sensory impairment, immobility from physical restraints or urinary catheters, and polypharmacy.20,21 Effective delirium care pathways targeting these risk factors must be multifaceted, interdisciplinary, and interprofessional. Accurate risk assessment is critical to allocate resources to high-risk patients. Delirium affects patients in all medical and surgical disciplines, and often is underdiagnosed.19,22 Comprehensive screening is necessary to identify cases early and track outcomes, and educational efforts must reach all providers in the hospital. These challenges require a systematic, pragmatic approach to change.
The purpose of this study was to evaluate the association between a delirium care pathway and clinical outcomes for hospitalized patients. We hypothesized that this program would be associated with reduced hospital LOS, with secondary benefits to hospitalization costs, odds of 30-day readmission, and delirium rates.
METHODS
Study Design
In this retrospective cohort study, we compared clinical outcomes the year before and after implementation of a delirium care pathway across seven hospital units. The study period spanned October 1, 2015, through February 28, 2019. The study was approved by the University of California, San Francisco Institutional Review Board (#13-12500).
Multicomponent Delirium Care Pathway
The delirium care pathway was developed collaboratively among geriatrics, hospital medicine, neurology, anesthesiology, surgery, and psychiatry services, with an interprofessional team of physicians, nurses, pharmacists, and physical and occupational therapists. This pathway was implemented in units consecutively, approximately every 4 months in the following order: neurosciences, medicine, cardiology, general surgery, specialty surgery, hematology-oncology, and transplant. The same implementation education protocols were performed in each unit. The pathway consisted of several components targeting delirium prevention and management (Appendix Figure 1 and Appendix Figure 2). Systematic screening for delirium was introduced as part of the multicomponent intervention. Nursing staff assessed each patient’s risk of developing delirium at admission using the AWOL score, a validated delirium prediction tool.23 AWOL consists of: patient Age, spelling “World” backwards correctly, Orientation, and assessment of iLlness severity by the nurse. For patients who spoke a language other than English, spelling of “world” backwards was translated to his or her primary language, or if this was not possible, the task was modified to serial 7s (subtracting 7 from 100 in a serial fashion). This modification has been validated for use in other languages.24 Patients at high risk for delirium based on an AWOL score ≥2 received a multidisciplinary intervention with four components: (1) notifying the primary team by pager and electronic medical record (EMR), (2) a nurse-led, evidence-based, nonpharmacologic multicomponent intervention,25 (3) placement of a delirium order set by the physician, and (4) review of medications by the unit pharmacist who adjusted administration timing to occur during waking hours and placed a note in the EMR notifying the primary team of potentially deliriogenic medications. The delirium order set reinforced the nonpharmacologic multicomponent intervention through a nursing order, placed an automatic consult to occupational therapy, and included options to order physical therapy, order speech/language therapy, obtain vital signs three times daily with minimal night interruptions, remove an indwelling bladder catheter, and prescribe melatonin as a sleep aid.
The bedside nurse screened all patients for active delirium every 12-hour shift using the Nursing Delirium Screening Scale (NuDESC) and entered the results into the EMR.23,26 Capturing NuDESC results in the EMR allowed communication across medical providers as well as monitoring of screening adherence. Each nurse received two in-person trainings in staff meetings and one-to-one instruction during the first week of implementation. All nurses were required to complete a 15-minute training module and had the option of completing an additional 1-hour continuing medical education module. If a patient was transferred to the intensive care unit (ICU), delirium was identified through use of the ICU-specific Confusion Assessment Method (CAM-ICU) assessments, which the bedside nurse performed each shift throughout the intervention period.27 Nurses were instructed to call the primary team physician after every positive screen. Before each unit’s implementation start date, physicians with patients on that unit received education through a combination of grand rounds, resident lectures and seminars, and a pocket card on delirium evaluation and management.
Participants and Eligibility Criteria
We included all patients aged ≥50 years hospitalized for >1 day on each hospital unit (Figure). We included adults aged ≥50 years to maximize the number of participants for this study while also capturing a population at risk for delirium. Because the delirium care pathway was unit-based and the pathway was rolled out sequentially across units, only patients who were admitted to and discharged from the same unit were included to better isolate the effect of the pathway. Patients who were transferred to the ICU were only included if they were discharged from the original unit of admission. Only the first hospitalization was included for patients with multiple hospitalizations during the study period.
Patient Characteristics
Patient demographics and clinical data were collected after discharge through Clarity and Vizient electronic databases (Table 1 and Table 2). All Elixhauser comorbidities were included except for the following International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10) codes that overlapped with a delirium diagnosis: G31.2, G93.89, G93.9, G94, R41.0, and R41.82 (Appendix Table 1). Severity of illness was obtained from Vizient, which calculates illness severity based on clinical and claims data (Appendix Table 1).
Delirium Metrics
Delirium screening was introduced as part of the multicomponent intervention, and therefore delirium rates before the intervention could not be determined. Trends in delirium prevalence and incidence after the intervention are reported. Prevalent delirium was defined as a single score of ≥2 on the nurse-administered NuDESC or a positive CAM-ICU at any point during the hospital stay. Incident delirium was identified if the first NuDESC score was negative and any subsequent NuDESC or CAM-ICU score was positive.

Outcomes
The primary study outcome was hospital LOS across all participants. Secondary outcomes included total direct cost and odds of 30-day hospital readmission. Readmissions tracked as part of hospital quality reporting were obtained from Vizient and were not captured if they occurred at another hospital. We also examined rates of safety attendant and restraint use during the study period, defined as the number of safety attendant days or restraint days per 1,000 patient days.
Because previous studies have demonstrated the effectiveness of multicomponent delirium interventions among elderly general medical patients,12 we also investigated these same outcomes in the medicine unit alone.
Statistical Analysis
The date of intervention implementation was determined for each hospital unit, which was defined as time(0) [t(0)]. The 12-month postintervention period was divided into four 3-month epochs to assess for trends. Data were aggregated across the seven units using t(0) as the start date, agnostic to the calendar month. Demographic and clinical characteristics were collected for the 12-months before t(0) and the four 3-month epochs after t(0). Univariate analysis of outcome variables comparing trends across the same epochs were conducted in the same manner, except for the rate of delirium, which was measured after t(0) and therefore could not be compared with the preintervention period.
Multivariable models were adjusted for age, sex, race/ethnicity, admission category, Elixhauser comorbidities, severity of illness quartile, and number days spent in the ICU. Admission category referred to whether the admission was emergent, urgent, or elective/unknown. Because it took 3 months after t(0) for each unit to reach a delirium screening compliance rate of 90%, the intervention was only considered fully implemented after this period. A ramp-up variable was set to 0 for admissions occurring prior to the intervention to t(0), 1/3 for admissions occurring 1 month post intervention, 2/3 for 2 months post intervention, and 1 for admissions occurring 3 to 12 months post intervention. In this way, the coefficient for the ramp-up variable estimated the postintervention versus preintervention effect. Numerical outcomes (LOS, cost) were log transformed to reduce skewness and analyzed using linear models. Coefficients were back-transformed to provide interpretations as proportional change in the median outcomes.
For LOS and readmission, we assessed secular trends by including admission date and admission date squared, in case the trend was nonlinear, as possible predictors; admission date was the specific date—not time from t(0)—to account for secular trends and allow contemporaneous controls in the analysis. To be conservative, we retained secular terms (first considering the quadratic and then the linear) if P <.10. The categorical outcome (30-day readmission) was analyzed using a logistic model. Count variables (delirium, safety attendants, restraints) were analyzed using Poisson regression models with a log link, and coefficients were back-transformed to provide rate ratio interpretations. Because delirium was not measured before t(0), and because the intervention was considered to take 3 months to become fully effective, baseline delirium rates were defined as those in the first 3 months adjusted by the ramp-up variable. For each outcome we included hospital unit, a ramp-up variable (measuring the pre- vs postintervention effect), and their interaction. If there was no statistically significant interaction, we presented the outcome for all units combined. If the interaction was statistically significant, we looked for consistency across units and reported results for all units combined when consistent, along with site-specific results. If the results were not consistent across the units, we provided site-specific results only. All statistical analyses were performed using SAS software, version 9.4 (SAS Institute Inc).
RESULTS
Participant Demographics and Clinical Characteristics
A total of 22,708 individuals were included in this study, with 11,018 in the preintervention period (Table 1 and Table 2). Most patients were cared for on the general surgery unit (n = 5,899), followed by the medicine unit (n = 4,923). The smallest number of patients were cared for on the hematology-oncology unit (n = 1,709). Across the five epochs, patients were of similar age and sex, and spent a similar number of days in the ICU. The population was diverse with regard to race and ethnicity; there were minor differences in admission category. There were also minor differences in severity of illness and some comorbidities between timepoints (Appendix Table 1).
Delirium Metrics
Delirium prevalence was 13.0% during the first epoch post intervention, followed by 12.0%, 11.7%, and 13.0% in the subsequent epochs (P = .91). Incident delirium occurred in 6.1% of patients during the first epoch post intervention, followed by 5.3%, 5.3%, and 5.8% in the subsequent epochs (P = .63).
Primary Outcome
Epoch-level data for LOS before and after the intervention is shown in Appendix Table 2. The mean unadjusted LOS for all units combined did not decrease after the intervention, but in the adjusted model, the mean LOS decreased by 2% after the intervention (P = .0087; Table 3).
Secondary Outcomes
The odds of 30-day readmission decreased by 14% (P = .0002) in the adjusted models for all units combined (Table 3). There was no statistically significant reduction in adjusted total direct hospitalization cost or rate of restraint use. The safety attendant results showed strong effect modification across sites; the site-specific estimates are provided in Appendix Table 3. However, the estimated values all showed reductions, and a number were large and statistically significant.
Medicine Unit Outcomes
On the medicine unit alone, we observed a statistically significant reduction in LOS of 9% after implementation of the delirium care pathway (P = .028) in the adjusted model (Table 3). There was an associated 7% proportional decrease in total direct cost (P = .0002). Reductions in 30-day readmission and safety attendant use did not remain statistically significant in the adjusted models.
DISCUSSION
Implementation of a hospital-wide multicomponent delirium care pathway was associated with reduced hospital LOS and 30-day hospital readmission in a study of 22,708 hospitalized adults at a tertiary care, university hospital in Northern California, encompassing both medical and surgical acute care patients. When evaluating general medicine patients alone, pathway implementation was associated with reductions in LOS and total direct cost. The cost savings of 7% among medical patients translates to median savings of $1,237 per hospitalization. This study—one of the largest to date examining implementation of a hospital-wide delirium care pathway—supports use of a multicomponent delirium care pathway for older adults hospitalized for a range of conditions.
Multicomponent pathways for delirium prevention and management are increasingly being used in hospital settings. The United Kingdom National Institute for Health and Care Excellence guidelines recommend delirium assessment and intervention by a multidisciplinary team within 24 hours of hospital admission for those at risk.25 These guidelines are based on evidence accumulated in clinical studies over the past 30 years suggesting that multicomponent interventions reduce incident delirium by 30% to 40% among medical and surgical patients.12,13,25,28
Although multicomponent delirium care pathways are associated with improved patient outcomes, the specific clinical benefits might vary across patient populations. Here, we found larger reductions in LOS and total direct cost among medicine patients. Medical patients might respond more robustly to nonpharmacologic multicomponent delirium interventions because of differing delirium etiologies (eg, constipation and sleep deprivation in a medical patient vs seizures or encephalitis in a neurosciences patient). Another explanation for the difference observed in total direct cost might be the inclusion of surgical units in the total study population. For example, not all hospital days are equivalent in cost for patients on a surgical unit.29 For patients requiring surgical care, most of the hospitalization cost might be incurred during the initial days of hospitalization, when there are perioperative costs; therefore, reduced LOS might have a lower economic impact.29 Multicomponent, nonpharmacologic delirium interventions encourage discontinuing restraints. As a result, one might expect a need for more frequent safety attendant use and an associated cost increase. However, we found that the estimated unit-specific values for safety attendant use showed reductions, which were large and highly statistically significant. For all units combined and the medicine unit alone, we found that the rate of restraint use decreased, although the change was not statistically significant. It is possible that some of the interventions taught to nurses and physicians as part of care pathway implementation, such as the use of family support for at-risk and delirious patients, led to a reduction in both safety attendants and restraints.
Our study had several strengths. This is one of the largest hospital-based delirium interventions studied, both in terms of its scope across seven diverse medical and surgical hospital units and the number of hospitalized patients studied. This intervention did not require additional staff or creating a specialized ward. Adherence to the pathway, as measured by risk assessment and delirium screening, was high (>90%) 3 months after implementation. This allowed for robust outcome ascertainment. The patient population’s characteristics and rates of delirium were stable over time. Because different hospital units incorporated the multicomponent delirium care pathway at different times, limiting enrollment to patients admitted and discharged from the same unit isolated the analysis to patients exposed to the pathway on each unit. This design also limited potential influence of other hospital quality improvement projects that might have occurred at the same time.
The primary limitation of this study is that screening for delirium was introduced as part of the multicomponent intervention. This decision was made to maximize buy-in from bedside nurses performing delirium screening because this addition to their workflow was explicitly linked to delirium prevention and management measures. Delirium could not be ascertained preintervention from the EMR because it is a clinical diagnosis and is coded inadequately.30 We could only measure the change in delirium metrics after implementation of the delirium care pathway. Because baseline delirium rates before the intervention were not measured systematically, conclusions about the intervention’s association with delirium metrics are limited. All other outcomes were measured before and after the intervention.
Although the comprehensive delirium screening program and high rate of adherence are a methodologic strength of this study, a second limitation is the use of the NuDESC. Our previous research demonstrated that the NuDESC has low sensitivity but high specificity and positive predictive value,26 which might underestimate delirium rates in this study. However, any underestimation should be stable over time and temporal trends should remain meaningful. This could allow more widespread study of delirium among hospitalized individuals. Because this care pathway was hospital-wide, it was important to ensure both consistency of screening and longevity of the initiative, and it was necessary to select a delirium assessment tool that was efficient and validated for nursing implementation. For these reasons, the NuDESC was an appropriate choice.
It is possible that our results could be influenced by unmeasured confounders. For example, although we incorporated Elixhauser medical comorbidities and illness severity into our model, we were unable to adjust for baseline functional status or frailty. Baseline functional status and frailty were not reliably recorded in the EMR, although these are potential confounders when investigating clinical outcomes including hospital readmission.
CONCLUSION
Implementation of a systematic, hospital-wide multicomponent delirium care pathway is associated with reductions in hospital LOS and 30-day readmission. In general medicine units, the reduction in LOS and associated cost savings were robust. These results demonstrate the feasibility and effectiveness of implementing an interprofessional, multidisciplinary multicomponent delirium care pathway through medical center funding to benefit patients and the hospital system.
Acknowledgments
The authors thank the many hospital staff members, especially the nurses, pharmacists, therapists, and patient care assistants, who helped implement the multicomponent delirium care pathway. All persons who have contributed significantly to this work are listed as authors of this work.
1. Bidwell J. Interventions for preventing delirium in hospitalized non-ICU patients: A Cochrane review summary. Int J Nurs Stud. 2017;70:142-143. https://doi.org/ 10.1016/j.ijnurstu.2016.11.010
2. Maldonado JR. Delirium in the acute care setting: characteristics, diagnosis and treatment. Crit Care Clin. 2008;24(4):657-722, vii. https://doi.org/10.1016/j.ccc.2008.05.008
3. Field RR, Wall MH. Delirium: past, present, and future. Semin Cardiothorac Vasc Anesth. 2013;17(3):170-179. https://doi.org/10.1177/1089253213476957
4. Oh ST, Park JY. Postoperative delirium. Korean J Anesthesiol. 2019;72(1):4-12. https://doi.org/10.4097/kja.d.18.00073.1
5. Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990;263(8):1097-1101.
6. Salluh JI, Soares M, Teles JM, et al. Delirium epidemiology in critical care (DECCA): an international study. Crit Care. 2010;14(6):R210. https://doi.org/10.1186/cc9333
7. Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753-1762. https://doi.org/
8. McCusker J, Cole MG, Dendukuri N, Belzile E. Does delirium increase hospital stay? J Am Geriatr Soc. 2003;51(11):1539-1546. https://doi.org/10.1001/jama.291.14.1753
9. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242. https://doi.org/10.1046/j.1525-1497.1998.00073.x
10. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364. https://doi.org/10.1093/ageing/afl005
11. LaHue SC, Douglas VC, Kuo T, et al. Association between inpatient delirium and hospital readmission in patients >/= 65 years of age: a retrospective cohort study. J Hosp Med. 2019;14(4):201-206. https://doi.org/10.12788/jhm.3130
12. Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512-520. https://doi.org/10.1001/jamainternmed.2014.7779
13. Inouye SK, Bogardus ST, Jr., Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669-676. https://doi.org/10.1056/NEJM199903043400901
14. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516-522. https://doi.org/
15. Alhaidari AA, Allen-Narker RA. An evolving approach to delirium: A mixed-methods process evaluation of a hospital-wide delirium program in New Zealand. Australas J Ageing. 2017. https://doi.org/10.1046/j.1532-5415.2001.49108.x
16. Holroyd-Leduc JM, Khandwala F, Sink KM. How can delirium best be prevented and managed in older patients in hospital? CMAJ. 2010;182(5):465-470. https://doi.org/10.1503/cmaj.080519
17. Siddiqi N, Stockdale R, Britton AM, Holmes J. Interventions for preventing delirium in hospitalised patients. Cochrane Database Syst Rev. 2007(2):CD005563. https://doi.org/ 10.1002/14651858.CD005563.pub2
18. Siddiqi N, Harrison JK, Clegg A, et al. Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2016;3:CD005563. https://doi.org/10.1002/14651858.CD005563.pub3
19. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922. https://doi.org/10.1016/S0140-6736(13)60688-1
20. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857.
21. LaHue SC, Liu VX. Loud and clear: sensory impairment, delirium, and functional recovery in critical illness. Am J Respir Crit Care Med. 2016;194(3):252-253. https://doi.org/10.1164/rccm.201602-0372ED
22. Ritter SRF, Cardoso AF, Lins MMP, Zoccoli TLV, Freitas MPD, Camargos EF. Underdiagnosis of delirium in the elderly in acute care hospital settings: lessons not learned. Psychogeriatrics. 2018;18(4):268-275. https://doi.org/10.1111/psyg.12324
23. Douglas VC, Hessler CS, Dhaliwal G, et al. The AWOL tool: derivation and validation of a delirium prediction rule. J Hosp Med. 2013;8(9):493-499. https://doi.org/10.1002/jhm.2062
24. Tombaugh TN, McDowell I, Kristjansson B, Hubley AM. Mini-Mental State Examination (MMSE) and the modified MMSE (3MS): A psychometric comparison and normative data. Psychol Assessment. 1996;8(1):48-59. https://doi.org/10.1037/1040-3590.8.1.48
25. Young J, Murthy L, Westby M, Akunne A, O’Mahony R, Guideline Development Group. Diagnosis, prevention, and management of delirium: summary of NICE guidance. BMJ. 2010;341:c3704. https://doi.org/10.1136/bmj.c3704
26. Hargrave A, Bastiaens J, Bourgeois JA, et al. Validation of a nurse-based delirium-screening tool for hospitalized patients. Psychosomatics. 2017;58(6):594-603. https://doi.org/10.1016/j.psym.2017.05.005
27. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703-2710. https://doi.org/10.1001/jama.286.21.2703
28. Strijbos MJ, Steunenberg B, van der Mast RC, Inouye SK, Schuurmans MJ. Design and methods of the Hospital Elder Life Program (HELP), a multicomponent targeted intervention to prevent delirium in hospitalized older patients: efficacy and cost-effectiveness in Dutch health care. BMC Geriatr. 2013;13:78. https://doi.org/10.1186/1471-2318-13-78
29. Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg. 2000;191(2):123-130. https://doi.org/10.1016/s1072-7515(00)00352-5
30. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210-220. https://doi.org/10.1038/nrneurol.2009.24
1. Bidwell J. Interventions for preventing delirium in hospitalized non-ICU patients: A Cochrane review summary. Int J Nurs Stud. 2017;70:142-143. https://doi.org/ 10.1016/j.ijnurstu.2016.11.010
2. Maldonado JR. Delirium in the acute care setting: characteristics, diagnosis and treatment. Crit Care Clin. 2008;24(4):657-722, vii. https://doi.org/10.1016/j.ccc.2008.05.008
3. Field RR, Wall MH. Delirium: past, present, and future. Semin Cardiothorac Vasc Anesth. 2013;17(3):170-179. https://doi.org/10.1177/1089253213476957
4. Oh ST, Park JY. Postoperative delirium. Korean J Anesthesiol. 2019;72(1):4-12. https://doi.org/10.4097/kja.d.18.00073.1
5. Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990;263(8):1097-1101.
6. Salluh JI, Soares M, Teles JM, et al. Delirium epidemiology in critical care (DECCA): an international study. Crit Care. 2010;14(6):R210. https://doi.org/10.1186/cc9333
7. Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753-1762. https://doi.org/
8. McCusker J, Cole MG, Dendukuri N, Belzile E. Does delirium increase hospital stay? J Am Geriatr Soc. 2003;51(11):1539-1546. https://doi.org/10.1001/jama.291.14.1753
9. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242. https://doi.org/10.1046/j.1525-1497.1998.00073.x
10. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364. https://doi.org/10.1093/ageing/afl005
11. LaHue SC, Douglas VC, Kuo T, et al. Association between inpatient delirium and hospital readmission in patients >/= 65 years of age: a retrospective cohort study. J Hosp Med. 2019;14(4):201-206. https://doi.org/10.12788/jhm.3130
12. Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175(4):512-520. https://doi.org/10.1001/jamainternmed.2014.7779
13. Inouye SK, Bogardus ST, Jr., Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669-676. https://doi.org/10.1056/NEJM199903043400901
14. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516-522. https://doi.org/
15. Alhaidari AA, Allen-Narker RA. An evolving approach to delirium: A mixed-methods process evaluation of a hospital-wide delirium program in New Zealand. Australas J Ageing. 2017. https://doi.org/10.1046/j.1532-5415.2001.49108.x
16. Holroyd-Leduc JM, Khandwala F, Sink KM. How can delirium best be prevented and managed in older patients in hospital? CMAJ. 2010;182(5):465-470. https://doi.org/10.1503/cmaj.080519
17. Siddiqi N, Stockdale R, Britton AM, Holmes J. Interventions for preventing delirium in hospitalised patients. Cochrane Database Syst Rev. 2007(2):CD005563. https://doi.org/ 10.1002/14651858.CD005563.pub2
18. Siddiqi N, Harrison JK, Clegg A, et al. Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2016;3:CD005563. https://doi.org/10.1002/14651858.CD005563.pub3
19. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922. https://doi.org/10.1016/S0140-6736(13)60688-1
20. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857.
21. LaHue SC, Liu VX. Loud and clear: sensory impairment, delirium, and functional recovery in critical illness. Am J Respir Crit Care Med. 2016;194(3):252-253. https://doi.org/10.1164/rccm.201602-0372ED
22. Ritter SRF, Cardoso AF, Lins MMP, Zoccoli TLV, Freitas MPD, Camargos EF. Underdiagnosis of delirium in the elderly in acute care hospital settings: lessons not learned. Psychogeriatrics. 2018;18(4):268-275. https://doi.org/10.1111/psyg.12324
23. Douglas VC, Hessler CS, Dhaliwal G, et al. The AWOL tool: derivation and validation of a delirium prediction rule. J Hosp Med. 2013;8(9):493-499. https://doi.org/10.1002/jhm.2062
24. Tombaugh TN, McDowell I, Kristjansson B, Hubley AM. Mini-Mental State Examination (MMSE) and the modified MMSE (3MS): A psychometric comparison and normative data. Psychol Assessment. 1996;8(1):48-59. https://doi.org/10.1037/1040-3590.8.1.48
25. Young J, Murthy L, Westby M, Akunne A, O’Mahony R, Guideline Development Group. Diagnosis, prevention, and management of delirium: summary of NICE guidance. BMJ. 2010;341:c3704. https://doi.org/10.1136/bmj.c3704
26. Hargrave A, Bastiaens J, Bourgeois JA, et al. Validation of a nurse-based delirium-screening tool for hospitalized patients. Psychosomatics. 2017;58(6):594-603. https://doi.org/10.1016/j.psym.2017.05.005
27. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703-2710. https://doi.org/10.1001/jama.286.21.2703
28. Strijbos MJ, Steunenberg B, van der Mast RC, Inouye SK, Schuurmans MJ. Design and methods of the Hospital Elder Life Program (HELP), a multicomponent targeted intervention to prevent delirium in hospitalized older patients: efficacy and cost-effectiveness in Dutch health care. BMC Geriatr. 2013;13:78. https://doi.org/10.1186/1471-2318-13-78
29. Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg. 2000;191(2):123-130. https://doi.org/10.1016/s1072-7515(00)00352-5
30. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210-220. https://doi.org/10.1038/nrneurol.2009.24
© 2021 Society of Hospital Medicine
Association between Inpatient Delirium and Hospital Readmission in Patients ≥ 65 Years of Age: A Retrospective Cohort Study
Delirium is an acute change in mental status, affecting more than seven million hospitalized patients in the United States annually.1 Several factors increase the risk of developing delirium, including advanced age,2 cognitive dysfunction,3 hearing and vision impairment,4-6 and severe illness or major surgery.7 Delirium may be precipitated during hospitalization by common inpatient interventions, such as the use of physical restraints, polypharmacy, or bladder catheters.4,8 In-hospital delirium impacts an estimated 10%-15% of the general medical admissions and as many as 81% of patients in the intensive care unit (ICU).9-11 Despite the relative frequency with which delirium is encountered in the hospital, subsequent emergency department (ED) presentations or hospital readmissions for these patients are poorly characterized.
The development of delirium is associated with several negative outcomes during the hospital stay. Delirium is an independent predictor of prolonged hospital stay,7,9,12,13 prolonged mechanical ventilation,14 and mortality during admission.14,15 Inpatient delirium is associated with functional decline at discharge, leading to a new nursing home placement.16-19 Preexisting dementia is exacerbated by inpatient delirium, and a new diagnosis of cognitive impairment20 or dementia becomes more common after an episode of delirium.21
These data suggest that people diagnosed with delirium may be particularly vulnerable in the posthospitalization period. Hospitals with high rates of unplanned readmissions face penalties from the Centers for Medicare and Medicaid Services.22,23 However, few investigations have focused on postdischarge healthcare utilization, such as readmission rates and ED visits. Studies that address this topic are limited to postoperative patient populations.24
Using a cohort of hospitalized patients, we examined whether those diagnosed with delirium experienced worse outcomes compared with patients with no such condition. We hypothesized that the patients diagnosed with delirium during hospitalization would experience more readmissions and ED visits within 30 days of discharge compared with those without delirium.
METHODS
Study Design
This single-center retrospective cohort study took place at the Kaiser Permanente San Rafael Medical Center (KP-SRF), a 116-bed general community medical and surgical hospital located in Northern California, from September 6, 2010 to March 31, 2015. The Kaiser Permanente Northern California institutional review board, in accordance with the provisions of the Declaration of the Helsinki and International Conference on Harmonization Guidelines for Good Clinical Practice (CN-15-2491-H), approved this study.
Participants and Eligibility Criteria
This study included Kaiser Permanente members at least 65 years old who were hospitalized at KP-SRF from September 2010 to March 2015. Patient data were obtained from the electronic medical records. Patients with delirium were identified from a delirium registry; all other patients served as controls.
Starting on September 6, 2010, a hospital-wide program was initiated to screen hospitalized medical and surgical patients using the Confusion Assessment Method (CAM).25 As part of this program, nurses completed a four-hour training on delirium; the program included delirium identification and CAM administration. Patients deemed at risk for delirium by their nurse or displaying symptoms of delirium (fluctuation in attention or awareness, disorientation, restlessness, agitation, and psychomotor slowing) were screened by nurses one to two times within a 24-hour period. Physicians were notified by the nurse if their patient screened positive. Nurses were prohibited from performing CAMs in languages that they were not fluent in, thus resulting in screening of primarily English-speaking patients. Psychiatry was consulted at the discretion of the primary team physician to assist with diagnosis and management of delirium. As psychiatry consultation was left up to the discretion of the primary team physician, not all CAM-positive patients were evaluated. The psychiatrists conducted no routine evaluation on the CAM-negative patients unless requested by the primary team physician. The psychiatrist confirmed the delirium diagnosis with a clinical interview and assessment. The patients confirmed with delirium at any point during their hospitalization were prospectively added to a delirium registry. The patients assessed by the psychiatrist as not delirious were excluded from the registry. Only those patients added to the delirium registry during the study period were classified as delirious for this study. All other patients were included as controls. The presence of the nursing screening program using the CAM enriched the cohort, but a positive CAM was unnecessary nor was it sufficient for inclusion in the delirium group (Table 1).
To eliminate the influence of previous delirium episodes on readmission, the subjects were excluded if they reported a prior diagnosis of delirium in 2006 or later, which was the year the electronic medical record was initiated. This diagnosis was determined retrospectively using the following ICD-9 codes: 290.11, 290.3, 290.41, 292.0, 292.81, 292.89, 293.0, 293.0E, 293.0F, 293.1, 293.89, 294.10, 294.21, 304.00, 304.90, 305.50, 331.0, 437.0, 780.09, V11.8, and V15.89.26 Subjects were also excluded if they were ever diagnosed with alcohol-related delirium, as defined by ICD-9 codes 291, 303.9, and 305. Subjects were excluded from the primary analysis if Kaiser Permanente membership lapsed to any degree within 30 days of discharge. Patients who died in the hospital were not excluded; however, the analyses of postdischarge outcomes were conducted on the subpopulation of study subjects who were discharged alive.
For subjects with multiple entries in the delirium registry, the earliest hospitalization during the study period in which a delirium diagnosis was recorded was selected. For eligible patients without a diagnosis of delirium, a single hospitalization was selected randomly from the individual patients during the time period. The analysis database included only one hospitalization for each subject. The flowchart of patient selection is outlined in the Figure.
Patient Characteristics
Patient demographics and clinical data were obtained from the electronic medical records. We used several scores to characterize illness severity, including the Charlson comorbidity index,27 Laboratory-Based Acute Physiology, version 2 (LAPS2) score28—an externally validated score for acute severity of illness—and disease categories as defined by the Healthcare Cost and Utilization Project (HCUP).29
Outcomes
The primary outcome was the rate of readmission to the hospital within 30 days of discharge from the hospitalization in which delirium was first diagnosed. Readmissions and ED visits to any Kaiser Permanente hospital and to hospitals outside of the Kaiser Permanente network with Kaiser Permanente insurance were captured. To avoid incorrectly coding patients transferred from the index hospital to another hospital as readmissions, we excluded readmissions that occurred on the day of discharge or the following calendar day. This action was expected to lower the absolute number of readmissions but restrict the analysis to true readmissions. The models of postdischarge outcomes are based on the subset of patients discharged alive. The secondary outcome measures included discharge from the index hospitalization to a skilled nursing facility or hospice rather than to home and emergency room visits within 30 days of discharge. We also quantified rates of mortality during hospitalization and at 30 days postdischarge.
Statistical Analysis
Comparisons between patients with delirium and those without were performed using Pearson’s X2 test for categorical variables and student t-test for continuous variables. The estimated odds of our outcome measures for delirious and nondelirious subjects were calculated from multivariable logistic regression models, which controlled for predictors of delirium and additional information obtained during the hospitalization. For inpatient outcomes (in-hospital mortality and discharge to skilled nursing facility or hospice), we adjusted only for admission characteristics: age, race/ethnicity, admission to ICU, Charlson comorbidity index, HCUP category, and admission category. To limit the number of variables in our model, we consolidated the initial 30 HCUP categories (Appendix Table 1) by illness type into 13 categories (Appendix Table 2). For postdischarge outcomes, we adjusted for all the variables, including disposition (Table 2). The average estimated odds were calculated based on the observed marginal distribution of the control variables. The P value indicates how likely the odds on each outcome for delirious subjects differed significantly from those for other subjects. All statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, North Carolina).
RESULTS
Demographics and Clinical Characteristics
A total of 718 patients with delirium and 7,927 patients without delirium were included in this study. The related demographic information is outlined in Table 2. On average, the patients with delirium were older (83 ± 8 years versus 77 ± 8 years, P < .0001) but no difference in gender distribution was observed between groups. A similar racial breakdown was noted between groups, with white patients accounting for 87% of both patients with delirium and those without. The majority of admissions were unplanned medical admissions. The delirium cohort included more emergent surgical admissions compared with patients who did not develop delirium. Patients who developed delirium exhibited higher levels of illness severity on admission, as measured by the Charlson and LAPS2 scores, and were more often admitted to the ICU. Significant differences were also observed between admission illness categories between patients with delirium and those without.
Primary Outcome
Delirium during admission was significantly associated with hospital readmission within 30 days of discharge (adjusted odds ratio [aOR] = 2.60, 95% CI: 1.96–3.44; P < .0001; Table 3).
Secondary Outcomes
Delirium during admission was significantly (P < .0001; Table 3) associated with an ED visit within 30 days of discharge (OR: 2.18; 95% CI: 1.77–2.69) and discharge to a skilled nursing facility or hospice rather than home (OR: 2.52; 95% CI: 2.09–3.01). Delirium was not associated (P > .1) with death during hospitalization nor death 30 days following discharge.
As the delirious patients were much more likely to be discharged to a skilled nursing facility than nondelirious patients, we tested whether discharge disposition influenced readmission rates and ED visits between delirious and nondelirious patients in an unadjusted univariate analysis. The association between delirium and readmission and ED utilization was present regardless of disposition. Among patients discharged to skilled nursing, readmission rates were 4.76% and 13.38% (P < .001), and ED visit rates were 12.29% and 23.24% (P < .001) for nondelirious and delirious patients, respectively. Among patients discharged home, readmission rates were 4.96% and 14.37% (P < .001), and ED visit rates were 11.93% and 29.04% (P < .001) for nondelirious and delirious patients, respectively.
DISCUSSION
In this study of patients in a community hospital in Northern California, we observed a significant association between inpatient delirium and risk of hospital readmission within 30 days of discharge. We also demonstrated increased skilled nursing facility placement and ED utilization after discharge among hospitalized patients with delirium compared with those without. Patients with delirium in this study were diagnosed by a psychiatrist—a gold standard30—and the study was conducted in a health system database with near comprehensive ascertainment of readmissions. These results suggest that patients with delirium are particularly vulnerable in the posthospitalization period and are a key group to focusing on reducing readmission rates and postdischarge healthcare utilization.
Identifying the risk factors for hospital readmission is important for the benefit of both the patient and the hospital. In an analysis of Medicare claims data from 2003 to 2004, 19.6% of beneficiaries were readmitted within 30 days of discharge.31 There is a national effort to reduce unplanned hospital readmissions for both patient safety as hospitals with high readmission rates face penalties from the Centers for Medicare and Medicaid Services.22,23 Why delirium is associated with readmission remains unclear. Delirium may precipitate aspiration events, reduce oral intake which complicates medication administration and nutrition, or reduced mobility, leading to pulmonary emboli and skin breakdown, any of which could lead to readmission.32 Delirium may also accelerate the progression of cognitive decline and overall loss of functional independence.20 Delirious patients can be difficult to care for at home, and persistent delirium may lead to returns to the ED and readmission. Strategies to reduce readmissions associated with delirium may need to focus on both prevention of hospital-acquired delirium and targeted caregiver and patient support after discharge.
Hospital readmission and ED visits are not mutually exclusive experiences. In the United States, the majority of patients admitted to the hospital are admitted through the ED.33 Thus, most of the readmissions in this cohort were also likely counted as 30-day ED visits. However, as ED utilization occurs regardless of whether a patient is discharged or admitted from the ED, we reported all ED visits in this analysis, similar to other studies.34 More delirium patients returned to the ED 30 days postdischarge than were ultimately readmitted to the hospital, and delirious patients were more likely to visit the ED or be readmitted than nondelirious patients. These observations point toward the first 30 days after discharge as a crucial period for these patients.
Our study features several strengths. To our knowledge, this study is one of the largest investigations of inpatients with delirium. One distinguishing feature was that all cases of delirium in this study were diagnosed by a psychiatrist, which is considered a gold standard. Many studies rely solely on brief nursing-administered surveys for delirium diagnosis. Using Kaiser Permanente data allowed for more complete follow-up of patients, including vital status. Kaiser Permanente is both a medical system and an insurer, resulting in acquisition of detailed health information from all hospitalizations where Kaiser Permanente insurance was used for each patient. Therefore, patients were only lost to follow-up following discharge in the event of a membership lapse; these patients were excluded from analysis. The obtained data are also more generalizable than those of other studies examining readmission rates in delirious patients as the hospital where these data were collected is a 116-bed general community medical and surgical hospital. Thus, the patients enrolled in this study covered multiple hospital services with a variety of admission diagnoses. This condition contrasts with much of the existing literature on inpatient delirium; these studies mostly center on specific medical conditions or surgeries and are often conducted at academic medical centers. At the same time, Kaiser Permanente is a unique health maintenance organization focused on preventive care, and readmission rates are possibly lower than elsewhere given the universal access to primary care for Kaiser Permanente members. Our results may not generalize to patients hospitalized in other health systems.
The diagnosis of delirium is a clinical diagnosis without biomarkers or radiographic markers and is also underdiagnosed and poorly coded.32 For these reasons, delirium can be challenging to study in large administrative databases or data derived from electronic medical records. We addressed this limitation by classifying the delirium patients only when they had been diagnosed by a staff psychiatrist. However, not all patients who screened positive with the CAM were evaluated by the staff psychiatrist during the study period. Thus, several CAM-positive patients who were not evaluated by psychiatry were included in the control population. This situation may cause bias toward identification of more severe cases of delirium. Although the physicians were encouraged to consult the psychiatry department for any patients who screened positive for delirium with the CAM, the psychiatrist may not have been involved if patients were managed without consultation. These patients may have exhibited less severe delirium or hypoactive delirium. In addition, the CAM fails to detect all delirious patients; interrater variability may occur with CAM administration, and non-English speaking patients are more likely to be excluded.35 These situations are another possible way for our control population to include some delirious patients and those patients with less severe or hypoactive subtypes. While this might bias toward the null hypothesis, it is also possible our results only indicate an association between more clinically apparent delirium and readmission. A major limitation of this study is that we were unable to quantify the number of cohort patients screened with the CAM or the results of screening, thus limiting our ability to quantify the impact of potential biases introduced by the screening program.
This study may have underestimated readmission rates. We defined readmissions as all hospitalizations at any Kaiser Permanente facility, or to an alternate facility where Kaiser Permanente insurance was used, within 30 days of discharge. We excluded the day of discharge or the following calendar day to avoid mischaracterizing transfers from the index hospital to another Kaiser Permanente facility as readmissions. This step was conducted to avoid biasing our comparison, as delirious patients are less frequently discharged home than nondelirious patients. Therefore, while the relative odds of readmission between delirious and nondelirious patients reported in this study should be generalizable to other community hospitals, the absolute readmission rates reported here may not be comparable to those reported in other studies.
Delirium may represent a marker of more severe illness or medical complications accrued during the hospitalization, which could lead to the associations observed in this study due to confounding.32 Patients with delirium are more likely to be admitted emergently, admitted to the ICU, and feature higher acuity conditions than patients without delirium. We attempted to mitigate this possibility by using a multivariable model to control for variables related to illness severity, including the Charlson comorbidity index, HCUP diagnostic categories, and ICU admission. Despite including HCUP diagnostic categories in our model, we were unable to capture the contribution of certain diseases with finer granularity, such as preexistent dementia, which may also affect clinical outcomes.36 Similarly, although we incorporated markers of illness severity into our model, we were unable to adjust for baseline functional status or frailty, which were not reliably recorded in the electronic medical record but are potential confounders when investigating clinical outcomes including hospital readmission.
We also lacked information regarding the duration of delirium in our cohort. Therefore, we were unable to test whether longer episodes of delirium were more predictive of readmission than shorter episodes.
CONCLUSION
In-hospital delirium is associated with several negative patient outcomes. Our study demonstrates that delirium predicts 30-day readmission and emergency department utilization after hospital discharge. Bearing in mind that a third of hospital-acquired delirium cases may be preventable,32 hospitals should prioritize interventions to reduce postdischarge healthcare utilization and complications in this particularly vulnerable group.
Acknowledgments
The authors would like to acknowledge Dr. Andrew L. Avins for his guidance with the initial development of this project and Julie Fourie for contributing data to the overall study.
Disclosures
Dr. Liu receives funding from NIH K23GM112018 and
Funding
This study was funded by Kaiser Permanente Graduate Medical Education, who approved the design, conduct, and reporting of this study.
1. Bidwell J. Interventions for preventing delirium in hospitalized non-ICU patients: A Cochrane review summary. Int J Nurs Stud. 2017;70:142-143. PubMed
2. Ryan DJ, O’Regan NA, Caoimh RÓ, et al. Delirium in an adult acute hospital population: predictors, prevalence and detection. BMJ Open. 2013;3(1):e001772. PubMed
3. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-598. PubMed
4. Inouye SK. Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord. 1999;10(5):393-400. PubMed
5. Inouye SK, Zhang Y, Jones RN, et al. Risk factors for delirium at discharge: development and validation of a predictive model. Arch Intern Med. 2007;167(13):1406-1413. PubMed
6. LaHue SC, Liu VX. Loud and clear: sensory impairment, delirium, and functional recovery in critical illness. Am J Respir Crit Care Med. 2016;194(3):252-253. PubMed
7. Salluh JI, Soares M, Teles JM, et al. Delirium epidemiology in critical care (DECCA): an international study. Crit Care. 2010;14(6):R210. PubMed
8. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857. PubMed
9. Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753-1762. PubMed
10. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922. PubMed
11. Brown EG, Douglas VC. Moving beyond metabolic encephalopathy: an update on delirium prevention, workup, and management. Semin Neurol. 2015;35(6):646-655. PubMed
12. Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990;263(8):1097-1101. PubMed
13. McCusker J, Cole MG, Dendukuri N, Belzile E. Does delirium increase hospital stay? J Am Geriatr Soc. 2003;51(11):1539-1546. PubMed
14. Salluh JI, Wang H, Schneider EB, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350:h2538. PubMed
15. Abelha FJ, Luís C, Veiga D, et al. Outcome and quality of life in patients with postoperative delirium during an ICU stay following major surgery. Crit Care. 2013;17(5):R257. PubMed
16. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364. PubMed
17. Witlox J, Eurelings LS, de Jonghe JF, et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304(4):443-451. PubMed
18. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242. PubMed
19. Freter S, Koller K, Dunbar M, MacKnight C, Rockwood K. Translating delirium prevention strategies for elderly adults with hip fracture into routine clinical care: A pragmatic clinical trial. J Am Geriatr Soc. 2017;65(3):567-573. PubMed
20. Fong TG, Jones RN, Shi P, et al. Delirium accelerates cognitive decline in Alzheimer disease. Neurology. 2009;72(18):1570-1575. PubMed
21. Girard TD, Jackson JC, Pandharipande PP, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010;38(7):1513-1520. PubMed
22. Berenson RA, Paulus RA, Kalman NS. Medicare’s readmissions-reduction program—a positive alternative. N Engl J Med. 2012;366(15):1364-1366. PubMed
23. Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the hospital readmission reduction program and readmission rates for target and nontarget conditions. JAMA. 2016;316(24):2647-2656. PubMed
24. Elsamadicy AA, Wang TY, Back AG, et al. Post-operative delirium is an independent predictor of 30-day hospital readmission after spine surgery in the elderly (≥65years old): a study of 453 consecutive elderly spine surgery patients. J Clin Neurosci. 2017;41:128-131. PubMed
25. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948. PubMed
26. Inouye SK, Leo-Summers L, Zhang Y, et al. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005;53(2):312-318. PubMed
27. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245-1251. PubMed
28. Escobar GJ, Gardner MN, Greene JD, Draper D, Kipnis P. Risk-adjusting hospital mortality using a comprehensive electronic record in an integrated health care delivery system. Med Care. 2013;51(5):446-453. PubMed
29. Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract. 2002;5(3):143-151. PubMed
30. Lawlor PG, Bush SH. Delirium diagnosis, screening and management. Curr Opin Support Palliat Care. 2014;8(3):286-295. PubMed
31. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. PubMed
32. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210-220. PubMed
33. Leyenaar JK, Lagu T, Lindenauer PK. Direct admission to the hospital: an alternative approach to hospitalization. J Hosp Med. 2016;11(4):303-305. PubMed
34. Wang CL, Ding ST, Hsieh MJ, et al. Factors associated with emergency department visit within 30 days after discharge. BMC Health Serv Res. 2016;16:190. PubMed
35. Shi Q, Warren L, Saposnik G, Macdermid JC. Confusion assessment method: a systematic review and meta-analysis of diagnostic accuracy. Neuropsychiatr Dis Treat. 2013;9:1359-1370. PubMed
36. Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002;50(10):1723-1732. PubMed
Delirium is an acute change in mental status, affecting more than seven million hospitalized patients in the United States annually.1 Several factors increase the risk of developing delirium, including advanced age,2 cognitive dysfunction,3 hearing and vision impairment,4-6 and severe illness or major surgery.7 Delirium may be precipitated during hospitalization by common inpatient interventions, such as the use of physical restraints, polypharmacy, or bladder catheters.4,8 In-hospital delirium impacts an estimated 10%-15% of the general medical admissions and as many as 81% of patients in the intensive care unit (ICU).9-11 Despite the relative frequency with which delirium is encountered in the hospital, subsequent emergency department (ED) presentations or hospital readmissions for these patients are poorly characterized.
The development of delirium is associated with several negative outcomes during the hospital stay. Delirium is an independent predictor of prolonged hospital stay,7,9,12,13 prolonged mechanical ventilation,14 and mortality during admission.14,15 Inpatient delirium is associated with functional decline at discharge, leading to a new nursing home placement.16-19 Preexisting dementia is exacerbated by inpatient delirium, and a new diagnosis of cognitive impairment20 or dementia becomes more common after an episode of delirium.21
These data suggest that people diagnosed with delirium may be particularly vulnerable in the posthospitalization period. Hospitals with high rates of unplanned readmissions face penalties from the Centers for Medicare and Medicaid Services.22,23 However, few investigations have focused on postdischarge healthcare utilization, such as readmission rates and ED visits. Studies that address this topic are limited to postoperative patient populations.24
Using a cohort of hospitalized patients, we examined whether those diagnosed with delirium experienced worse outcomes compared with patients with no such condition. We hypothesized that the patients diagnosed with delirium during hospitalization would experience more readmissions and ED visits within 30 days of discharge compared with those without delirium.
METHODS
Study Design
This single-center retrospective cohort study took place at the Kaiser Permanente San Rafael Medical Center (KP-SRF), a 116-bed general community medical and surgical hospital located in Northern California, from September 6, 2010 to March 31, 2015. The Kaiser Permanente Northern California institutional review board, in accordance with the provisions of the Declaration of the Helsinki and International Conference on Harmonization Guidelines for Good Clinical Practice (CN-15-2491-H), approved this study.
Participants and Eligibility Criteria
This study included Kaiser Permanente members at least 65 years old who were hospitalized at KP-SRF from September 2010 to March 2015. Patient data were obtained from the electronic medical records. Patients with delirium were identified from a delirium registry; all other patients served as controls.
Starting on September 6, 2010, a hospital-wide program was initiated to screen hospitalized medical and surgical patients using the Confusion Assessment Method (CAM).25 As part of this program, nurses completed a four-hour training on delirium; the program included delirium identification and CAM administration. Patients deemed at risk for delirium by their nurse or displaying symptoms of delirium (fluctuation in attention or awareness, disorientation, restlessness, agitation, and psychomotor slowing) were screened by nurses one to two times within a 24-hour period. Physicians were notified by the nurse if their patient screened positive. Nurses were prohibited from performing CAMs in languages that they were not fluent in, thus resulting in screening of primarily English-speaking patients. Psychiatry was consulted at the discretion of the primary team physician to assist with diagnosis and management of delirium. As psychiatry consultation was left up to the discretion of the primary team physician, not all CAM-positive patients were evaluated. The psychiatrists conducted no routine evaluation on the CAM-negative patients unless requested by the primary team physician. The psychiatrist confirmed the delirium diagnosis with a clinical interview and assessment. The patients confirmed with delirium at any point during their hospitalization were prospectively added to a delirium registry. The patients assessed by the psychiatrist as not delirious were excluded from the registry. Only those patients added to the delirium registry during the study period were classified as delirious for this study. All other patients were included as controls. The presence of the nursing screening program using the CAM enriched the cohort, but a positive CAM was unnecessary nor was it sufficient for inclusion in the delirium group (Table 1).
To eliminate the influence of previous delirium episodes on readmission, the subjects were excluded if they reported a prior diagnosis of delirium in 2006 or later, which was the year the electronic medical record was initiated. This diagnosis was determined retrospectively using the following ICD-9 codes: 290.11, 290.3, 290.41, 292.0, 292.81, 292.89, 293.0, 293.0E, 293.0F, 293.1, 293.89, 294.10, 294.21, 304.00, 304.90, 305.50, 331.0, 437.0, 780.09, V11.8, and V15.89.26 Subjects were also excluded if they were ever diagnosed with alcohol-related delirium, as defined by ICD-9 codes 291, 303.9, and 305. Subjects were excluded from the primary analysis if Kaiser Permanente membership lapsed to any degree within 30 days of discharge. Patients who died in the hospital were not excluded; however, the analyses of postdischarge outcomes were conducted on the subpopulation of study subjects who were discharged alive.
For subjects with multiple entries in the delirium registry, the earliest hospitalization during the study period in which a delirium diagnosis was recorded was selected. For eligible patients without a diagnosis of delirium, a single hospitalization was selected randomly from the individual patients during the time period. The analysis database included only one hospitalization for each subject. The flowchart of patient selection is outlined in the Figure.
Patient Characteristics
Patient demographics and clinical data were obtained from the electronic medical records. We used several scores to characterize illness severity, including the Charlson comorbidity index,27 Laboratory-Based Acute Physiology, version 2 (LAPS2) score28—an externally validated score for acute severity of illness—and disease categories as defined by the Healthcare Cost and Utilization Project (HCUP).29
Outcomes
The primary outcome was the rate of readmission to the hospital within 30 days of discharge from the hospitalization in which delirium was first diagnosed. Readmissions and ED visits to any Kaiser Permanente hospital and to hospitals outside of the Kaiser Permanente network with Kaiser Permanente insurance were captured. To avoid incorrectly coding patients transferred from the index hospital to another hospital as readmissions, we excluded readmissions that occurred on the day of discharge or the following calendar day. This action was expected to lower the absolute number of readmissions but restrict the analysis to true readmissions. The models of postdischarge outcomes are based on the subset of patients discharged alive. The secondary outcome measures included discharge from the index hospitalization to a skilled nursing facility or hospice rather than to home and emergency room visits within 30 days of discharge. We also quantified rates of mortality during hospitalization and at 30 days postdischarge.
Statistical Analysis
Comparisons between patients with delirium and those without were performed using Pearson’s X2 test for categorical variables and student t-test for continuous variables. The estimated odds of our outcome measures for delirious and nondelirious subjects were calculated from multivariable logistic regression models, which controlled for predictors of delirium and additional information obtained during the hospitalization. For inpatient outcomes (in-hospital mortality and discharge to skilled nursing facility or hospice), we adjusted only for admission characteristics: age, race/ethnicity, admission to ICU, Charlson comorbidity index, HCUP category, and admission category. To limit the number of variables in our model, we consolidated the initial 30 HCUP categories (Appendix Table 1) by illness type into 13 categories (Appendix Table 2). For postdischarge outcomes, we adjusted for all the variables, including disposition (Table 2). The average estimated odds were calculated based on the observed marginal distribution of the control variables. The P value indicates how likely the odds on each outcome for delirious subjects differed significantly from those for other subjects. All statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, North Carolina).
RESULTS
Demographics and Clinical Characteristics
A total of 718 patients with delirium and 7,927 patients without delirium were included in this study. The related demographic information is outlined in Table 2. On average, the patients with delirium were older (83 ± 8 years versus 77 ± 8 years, P < .0001) but no difference in gender distribution was observed between groups. A similar racial breakdown was noted between groups, with white patients accounting for 87% of both patients with delirium and those without. The majority of admissions were unplanned medical admissions. The delirium cohort included more emergent surgical admissions compared with patients who did not develop delirium. Patients who developed delirium exhibited higher levels of illness severity on admission, as measured by the Charlson and LAPS2 scores, and were more often admitted to the ICU. Significant differences were also observed between admission illness categories between patients with delirium and those without.
Primary Outcome
Delirium during admission was significantly associated with hospital readmission within 30 days of discharge (adjusted odds ratio [aOR] = 2.60, 95% CI: 1.96–3.44; P < .0001; Table 3).
Secondary Outcomes
Delirium during admission was significantly (P < .0001; Table 3) associated with an ED visit within 30 days of discharge (OR: 2.18; 95% CI: 1.77–2.69) and discharge to a skilled nursing facility or hospice rather than home (OR: 2.52; 95% CI: 2.09–3.01). Delirium was not associated (P > .1) with death during hospitalization nor death 30 days following discharge.
As the delirious patients were much more likely to be discharged to a skilled nursing facility than nondelirious patients, we tested whether discharge disposition influenced readmission rates and ED visits between delirious and nondelirious patients in an unadjusted univariate analysis. The association between delirium and readmission and ED utilization was present regardless of disposition. Among patients discharged to skilled nursing, readmission rates were 4.76% and 13.38% (P < .001), and ED visit rates were 12.29% and 23.24% (P < .001) for nondelirious and delirious patients, respectively. Among patients discharged home, readmission rates were 4.96% and 14.37% (P < .001), and ED visit rates were 11.93% and 29.04% (P < .001) for nondelirious and delirious patients, respectively.
DISCUSSION
In this study of patients in a community hospital in Northern California, we observed a significant association between inpatient delirium and risk of hospital readmission within 30 days of discharge. We also demonstrated increased skilled nursing facility placement and ED utilization after discharge among hospitalized patients with delirium compared with those without. Patients with delirium in this study were diagnosed by a psychiatrist—a gold standard30—and the study was conducted in a health system database with near comprehensive ascertainment of readmissions. These results suggest that patients with delirium are particularly vulnerable in the posthospitalization period and are a key group to focusing on reducing readmission rates and postdischarge healthcare utilization.
Identifying the risk factors for hospital readmission is important for the benefit of both the patient and the hospital. In an analysis of Medicare claims data from 2003 to 2004, 19.6% of beneficiaries were readmitted within 30 days of discharge.31 There is a national effort to reduce unplanned hospital readmissions for both patient safety as hospitals with high readmission rates face penalties from the Centers for Medicare and Medicaid Services.22,23 Why delirium is associated with readmission remains unclear. Delirium may precipitate aspiration events, reduce oral intake which complicates medication administration and nutrition, or reduced mobility, leading to pulmonary emboli and skin breakdown, any of which could lead to readmission.32 Delirium may also accelerate the progression of cognitive decline and overall loss of functional independence.20 Delirious patients can be difficult to care for at home, and persistent delirium may lead to returns to the ED and readmission. Strategies to reduce readmissions associated with delirium may need to focus on both prevention of hospital-acquired delirium and targeted caregiver and patient support after discharge.
Hospital readmission and ED visits are not mutually exclusive experiences. In the United States, the majority of patients admitted to the hospital are admitted through the ED.33 Thus, most of the readmissions in this cohort were also likely counted as 30-day ED visits. However, as ED utilization occurs regardless of whether a patient is discharged or admitted from the ED, we reported all ED visits in this analysis, similar to other studies.34 More delirium patients returned to the ED 30 days postdischarge than were ultimately readmitted to the hospital, and delirious patients were more likely to visit the ED or be readmitted than nondelirious patients. These observations point toward the first 30 days after discharge as a crucial period for these patients.
Our study features several strengths. To our knowledge, this study is one of the largest investigations of inpatients with delirium. One distinguishing feature was that all cases of delirium in this study were diagnosed by a psychiatrist, which is considered a gold standard. Many studies rely solely on brief nursing-administered surveys for delirium diagnosis. Using Kaiser Permanente data allowed for more complete follow-up of patients, including vital status. Kaiser Permanente is both a medical system and an insurer, resulting in acquisition of detailed health information from all hospitalizations where Kaiser Permanente insurance was used for each patient. Therefore, patients were only lost to follow-up following discharge in the event of a membership lapse; these patients were excluded from analysis. The obtained data are also more generalizable than those of other studies examining readmission rates in delirious patients as the hospital where these data were collected is a 116-bed general community medical and surgical hospital. Thus, the patients enrolled in this study covered multiple hospital services with a variety of admission diagnoses. This condition contrasts with much of the existing literature on inpatient delirium; these studies mostly center on specific medical conditions or surgeries and are often conducted at academic medical centers. At the same time, Kaiser Permanente is a unique health maintenance organization focused on preventive care, and readmission rates are possibly lower than elsewhere given the universal access to primary care for Kaiser Permanente members. Our results may not generalize to patients hospitalized in other health systems.
The diagnosis of delirium is a clinical diagnosis without biomarkers or radiographic markers and is also underdiagnosed and poorly coded.32 For these reasons, delirium can be challenging to study in large administrative databases or data derived from electronic medical records. We addressed this limitation by classifying the delirium patients only when they had been diagnosed by a staff psychiatrist. However, not all patients who screened positive with the CAM were evaluated by the staff psychiatrist during the study period. Thus, several CAM-positive patients who were not evaluated by psychiatry were included in the control population. This situation may cause bias toward identification of more severe cases of delirium. Although the physicians were encouraged to consult the psychiatry department for any patients who screened positive for delirium with the CAM, the psychiatrist may not have been involved if patients were managed without consultation. These patients may have exhibited less severe delirium or hypoactive delirium. In addition, the CAM fails to detect all delirious patients; interrater variability may occur with CAM administration, and non-English speaking patients are more likely to be excluded.35 These situations are another possible way for our control population to include some delirious patients and those patients with less severe or hypoactive subtypes. While this might bias toward the null hypothesis, it is also possible our results only indicate an association between more clinically apparent delirium and readmission. A major limitation of this study is that we were unable to quantify the number of cohort patients screened with the CAM or the results of screening, thus limiting our ability to quantify the impact of potential biases introduced by the screening program.
This study may have underestimated readmission rates. We defined readmissions as all hospitalizations at any Kaiser Permanente facility, or to an alternate facility where Kaiser Permanente insurance was used, within 30 days of discharge. We excluded the day of discharge or the following calendar day to avoid mischaracterizing transfers from the index hospital to another Kaiser Permanente facility as readmissions. This step was conducted to avoid biasing our comparison, as delirious patients are less frequently discharged home than nondelirious patients. Therefore, while the relative odds of readmission between delirious and nondelirious patients reported in this study should be generalizable to other community hospitals, the absolute readmission rates reported here may not be comparable to those reported in other studies.
Delirium may represent a marker of more severe illness or medical complications accrued during the hospitalization, which could lead to the associations observed in this study due to confounding.32 Patients with delirium are more likely to be admitted emergently, admitted to the ICU, and feature higher acuity conditions than patients without delirium. We attempted to mitigate this possibility by using a multivariable model to control for variables related to illness severity, including the Charlson comorbidity index, HCUP diagnostic categories, and ICU admission. Despite including HCUP diagnostic categories in our model, we were unable to capture the contribution of certain diseases with finer granularity, such as preexistent dementia, which may also affect clinical outcomes.36 Similarly, although we incorporated markers of illness severity into our model, we were unable to adjust for baseline functional status or frailty, which were not reliably recorded in the electronic medical record but are potential confounders when investigating clinical outcomes including hospital readmission.
We also lacked information regarding the duration of delirium in our cohort. Therefore, we were unable to test whether longer episodes of delirium were more predictive of readmission than shorter episodes.
CONCLUSION
In-hospital delirium is associated with several negative patient outcomes. Our study demonstrates that delirium predicts 30-day readmission and emergency department utilization after hospital discharge. Bearing in mind that a third of hospital-acquired delirium cases may be preventable,32 hospitals should prioritize interventions to reduce postdischarge healthcare utilization and complications in this particularly vulnerable group.
Acknowledgments
The authors would like to acknowledge Dr. Andrew L. Avins for his guidance with the initial development of this project and Julie Fourie for contributing data to the overall study.
Disclosures
Dr. Liu receives funding from NIH K23GM112018 and
Funding
This study was funded by Kaiser Permanente Graduate Medical Education, who approved the design, conduct, and reporting of this study.
Delirium is an acute change in mental status, affecting more than seven million hospitalized patients in the United States annually.1 Several factors increase the risk of developing delirium, including advanced age,2 cognitive dysfunction,3 hearing and vision impairment,4-6 and severe illness or major surgery.7 Delirium may be precipitated during hospitalization by common inpatient interventions, such as the use of physical restraints, polypharmacy, or bladder catheters.4,8 In-hospital delirium impacts an estimated 10%-15% of the general medical admissions and as many as 81% of patients in the intensive care unit (ICU).9-11 Despite the relative frequency with which delirium is encountered in the hospital, subsequent emergency department (ED) presentations or hospital readmissions for these patients are poorly characterized.
The development of delirium is associated with several negative outcomes during the hospital stay. Delirium is an independent predictor of prolonged hospital stay,7,9,12,13 prolonged mechanical ventilation,14 and mortality during admission.14,15 Inpatient delirium is associated with functional decline at discharge, leading to a new nursing home placement.16-19 Preexisting dementia is exacerbated by inpatient delirium, and a new diagnosis of cognitive impairment20 or dementia becomes more common after an episode of delirium.21
These data suggest that people diagnosed with delirium may be particularly vulnerable in the posthospitalization period. Hospitals with high rates of unplanned readmissions face penalties from the Centers for Medicare and Medicaid Services.22,23 However, few investigations have focused on postdischarge healthcare utilization, such as readmission rates and ED visits. Studies that address this topic are limited to postoperative patient populations.24
Using a cohort of hospitalized patients, we examined whether those diagnosed with delirium experienced worse outcomes compared with patients with no such condition. We hypothesized that the patients diagnosed with delirium during hospitalization would experience more readmissions and ED visits within 30 days of discharge compared with those without delirium.
METHODS
Study Design
This single-center retrospective cohort study took place at the Kaiser Permanente San Rafael Medical Center (KP-SRF), a 116-bed general community medical and surgical hospital located in Northern California, from September 6, 2010 to March 31, 2015. The Kaiser Permanente Northern California institutional review board, in accordance with the provisions of the Declaration of the Helsinki and International Conference on Harmonization Guidelines for Good Clinical Practice (CN-15-2491-H), approved this study.
Participants and Eligibility Criteria
This study included Kaiser Permanente members at least 65 years old who were hospitalized at KP-SRF from September 2010 to March 2015. Patient data were obtained from the electronic medical records. Patients with delirium were identified from a delirium registry; all other patients served as controls.
Starting on September 6, 2010, a hospital-wide program was initiated to screen hospitalized medical and surgical patients using the Confusion Assessment Method (CAM).25 As part of this program, nurses completed a four-hour training on delirium; the program included delirium identification and CAM administration. Patients deemed at risk for delirium by their nurse or displaying symptoms of delirium (fluctuation in attention or awareness, disorientation, restlessness, agitation, and psychomotor slowing) were screened by nurses one to two times within a 24-hour period. Physicians were notified by the nurse if their patient screened positive. Nurses were prohibited from performing CAMs in languages that they were not fluent in, thus resulting in screening of primarily English-speaking patients. Psychiatry was consulted at the discretion of the primary team physician to assist with diagnosis and management of delirium. As psychiatry consultation was left up to the discretion of the primary team physician, not all CAM-positive patients were evaluated. The psychiatrists conducted no routine evaluation on the CAM-negative patients unless requested by the primary team physician. The psychiatrist confirmed the delirium diagnosis with a clinical interview and assessment. The patients confirmed with delirium at any point during their hospitalization were prospectively added to a delirium registry. The patients assessed by the psychiatrist as not delirious were excluded from the registry. Only those patients added to the delirium registry during the study period were classified as delirious for this study. All other patients were included as controls. The presence of the nursing screening program using the CAM enriched the cohort, but a positive CAM was unnecessary nor was it sufficient for inclusion in the delirium group (Table 1).
To eliminate the influence of previous delirium episodes on readmission, the subjects were excluded if they reported a prior diagnosis of delirium in 2006 or later, which was the year the electronic medical record was initiated. This diagnosis was determined retrospectively using the following ICD-9 codes: 290.11, 290.3, 290.41, 292.0, 292.81, 292.89, 293.0, 293.0E, 293.0F, 293.1, 293.89, 294.10, 294.21, 304.00, 304.90, 305.50, 331.0, 437.0, 780.09, V11.8, and V15.89.26 Subjects were also excluded if they were ever diagnosed with alcohol-related delirium, as defined by ICD-9 codes 291, 303.9, and 305. Subjects were excluded from the primary analysis if Kaiser Permanente membership lapsed to any degree within 30 days of discharge. Patients who died in the hospital were not excluded; however, the analyses of postdischarge outcomes were conducted on the subpopulation of study subjects who were discharged alive.
For subjects with multiple entries in the delirium registry, the earliest hospitalization during the study period in which a delirium diagnosis was recorded was selected. For eligible patients without a diagnosis of delirium, a single hospitalization was selected randomly from the individual patients during the time period. The analysis database included only one hospitalization for each subject. The flowchart of patient selection is outlined in the Figure.
Patient Characteristics
Patient demographics and clinical data were obtained from the electronic medical records. We used several scores to characterize illness severity, including the Charlson comorbidity index,27 Laboratory-Based Acute Physiology, version 2 (LAPS2) score28—an externally validated score for acute severity of illness—and disease categories as defined by the Healthcare Cost and Utilization Project (HCUP).29
Outcomes
The primary outcome was the rate of readmission to the hospital within 30 days of discharge from the hospitalization in which delirium was first diagnosed. Readmissions and ED visits to any Kaiser Permanente hospital and to hospitals outside of the Kaiser Permanente network with Kaiser Permanente insurance were captured. To avoid incorrectly coding patients transferred from the index hospital to another hospital as readmissions, we excluded readmissions that occurred on the day of discharge or the following calendar day. This action was expected to lower the absolute number of readmissions but restrict the analysis to true readmissions. The models of postdischarge outcomes are based on the subset of patients discharged alive. The secondary outcome measures included discharge from the index hospitalization to a skilled nursing facility or hospice rather than to home and emergency room visits within 30 days of discharge. We also quantified rates of mortality during hospitalization and at 30 days postdischarge.
Statistical Analysis
Comparisons between patients with delirium and those without were performed using Pearson’s X2 test for categorical variables and student t-test for continuous variables. The estimated odds of our outcome measures for delirious and nondelirious subjects were calculated from multivariable logistic regression models, which controlled for predictors of delirium and additional information obtained during the hospitalization. For inpatient outcomes (in-hospital mortality and discharge to skilled nursing facility or hospice), we adjusted only for admission characteristics: age, race/ethnicity, admission to ICU, Charlson comorbidity index, HCUP category, and admission category. To limit the number of variables in our model, we consolidated the initial 30 HCUP categories (Appendix Table 1) by illness type into 13 categories (Appendix Table 2). For postdischarge outcomes, we adjusted for all the variables, including disposition (Table 2). The average estimated odds were calculated based on the observed marginal distribution of the control variables. The P value indicates how likely the odds on each outcome for delirious subjects differed significantly from those for other subjects. All statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, North Carolina).
RESULTS
Demographics and Clinical Characteristics
A total of 718 patients with delirium and 7,927 patients without delirium were included in this study. The related demographic information is outlined in Table 2. On average, the patients with delirium were older (83 ± 8 years versus 77 ± 8 years, P < .0001) but no difference in gender distribution was observed between groups. A similar racial breakdown was noted between groups, with white patients accounting for 87% of both patients with delirium and those without. The majority of admissions were unplanned medical admissions. The delirium cohort included more emergent surgical admissions compared with patients who did not develop delirium. Patients who developed delirium exhibited higher levels of illness severity on admission, as measured by the Charlson and LAPS2 scores, and were more often admitted to the ICU. Significant differences were also observed between admission illness categories between patients with delirium and those without.
Primary Outcome
Delirium during admission was significantly associated with hospital readmission within 30 days of discharge (adjusted odds ratio [aOR] = 2.60, 95% CI: 1.96–3.44; P < .0001; Table 3).
Secondary Outcomes
Delirium during admission was significantly (P < .0001; Table 3) associated with an ED visit within 30 days of discharge (OR: 2.18; 95% CI: 1.77–2.69) and discharge to a skilled nursing facility or hospice rather than home (OR: 2.52; 95% CI: 2.09–3.01). Delirium was not associated (P > .1) with death during hospitalization nor death 30 days following discharge.
As the delirious patients were much more likely to be discharged to a skilled nursing facility than nondelirious patients, we tested whether discharge disposition influenced readmission rates and ED visits between delirious and nondelirious patients in an unadjusted univariate analysis. The association between delirium and readmission and ED utilization was present regardless of disposition. Among patients discharged to skilled nursing, readmission rates were 4.76% and 13.38% (P < .001), and ED visit rates were 12.29% and 23.24% (P < .001) for nondelirious and delirious patients, respectively. Among patients discharged home, readmission rates were 4.96% and 14.37% (P < .001), and ED visit rates were 11.93% and 29.04% (P < .001) for nondelirious and delirious patients, respectively.
DISCUSSION
In this study of patients in a community hospital in Northern California, we observed a significant association between inpatient delirium and risk of hospital readmission within 30 days of discharge. We also demonstrated increased skilled nursing facility placement and ED utilization after discharge among hospitalized patients with delirium compared with those without. Patients with delirium in this study were diagnosed by a psychiatrist—a gold standard30—and the study was conducted in a health system database with near comprehensive ascertainment of readmissions. These results suggest that patients with delirium are particularly vulnerable in the posthospitalization period and are a key group to focusing on reducing readmission rates and postdischarge healthcare utilization.
Identifying the risk factors for hospital readmission is important for the benefit of both the patient and the hospital. In an analysis of Medicare claims data from 2003 to 2004, 19.6% of beneficiaries were readmitted within 30 days of discharge.31 There is a national effort to reduce unplanned hospital readmissions for both patient safety as hospitals with high readmission rates face penalties from the Centers for Medicare and Medicaid Services.22,23 Why delirium is associated with readmission remains unclear. Delirium may precipitate aspiration events, reduce oral intake which complicates medication administration and nutrition, or reduced mobility, leading to pulmonary emboli and skin breakdown, any of which could lead to readmission.32 Delirium may also accelerate the progression of cognitive decline and overall loss of functional independence.20 Delirious patients can be difficult to care for at home, and persistent delirium may lead to returns to the ED and readmission. Strategies to reduce readmissions associated with delirium may need to focus on both prevention of hospital-acquired delirium and targeted caregiver and patient support after discharge.
Hospital readmission and ED visits are not mutually exclusive experiences. In the United States, the majority of patients admitted to the hospital are admitted through the ED.33 Thus, most of the readmissions in this cohort were also likely counted as 30-day ED visits. However, as ED utilization occurs regardless of whether a patient is discharged or admitted from the ED, we reported all ED visits in this analysis, similar to other studies.34 More delirium patients returned to the ED 30 days postdischarge than were ultimately readmitted to the hospital, and delirious patients were more likely to visit the ED or be readmitted than nondelirious patients. These observations point toward the first 30 days after discharge as a crucial period for these patients.
Our study features several strengths. To our knowledge, this study is one of the largest investigations of inpatients with delirium. One distinguishing feature was that all cases of delirium in this study were diagnosed by a psychiatrist, which is considered a gold standard. Many studies rely solely on brief nursing-administered surveys for delirium diagnosis. Using Kaiser Permanente data allowed for more complete follow-up of patients, including vital status. Kaiser Permanente is both a medical system and an insurer, resulting in acquisition of detailed health information from all hospitalizations where Kaiser Permanente insurance was used for each patient. Therefore, patients were only lost to follow-up following discharge in the event of a membership lapse; these patients were excluded from analysis. The obtained data are also more generalizable than those of other studies examining readmission rates in delirious patients as the hospital where these data were collected is a 116-bed general community medical and surgical hospital. Thus, the patients enrolled in this study covered multiple hospital services with a variety of admission diagnoses. This condition contrasts with much of the existing literature on inpatient delirium; these studies mostly center on specific medical conditions or surgeries and are often conducted at academic medical centers. At the same time, Kaiser Permanente is a unique health maintenance organization focused on preventive care, and readmission rates are possibly lower than elsewhere given the universal access to primary care for Kaiser Permanente members. Our results may not generalize to patients hospitalized in other health systems.
The diagnosis of delirium is a clinical diagnosis without biomarkers or radiographic markers and is also underdiagnosed and poorly coded.32 For these reasons, delirium can be challenging to study in large administrative databases or data derived from electronic medical records. We addressed this limitation by classifying the delirium patients only when they had been diagnosed by a staff psychiatrist. However, not all patients who screened positive with the CAM were evaluated by the staff psychiatrist during the study period. Thus, several CAM-positive patients who were not evaluated by psychiatry were included in the control population. This situation may cause bias toward identification of more severe cases of delirium. Although the physicians were encouraged to consult the psychiatry department for any patients who screened positive for delirium with the CAM, the psychiatrist may not have been involved if patients were managed without consultation. These patients may have exhibited less severe delirium or hypoactive delirium. In addition, the CAM fails to detect all delirious patients; interrater variability may occur with CAM administration, and non-English speaking patients are more likely to be excluded.35 These situations are another possible way for our control population to include some delirious patients and those patients with less severe or hypoactive subtypes. While this might bias toward the null hypothesis, it is also possible our results only indicate an association between more clinically apparent delirium and readmission. A major limitation of this study is that we were unable to quantify the number of cohort patients screened with the CAM or the results of screening, thus limiting our ability to quantify the impact of potential biases introduced by the screening program.
This study may have underestimated readmission rates. We defined readmissions as all hospitalizations at any Kaiser Permanente facility, or to an alternate facility where Kaiser Permanente insurance was used, within 30 days of discharge. We excluded the day of discharge or the following calendar day to avoid mischaracterizing transfers from the index hospital to another Kaiser Permanente facility as readmissions. This step was conducted to avoid biasing our comparison, as delirious patients are less frequently discharged home than nondelirious patients. Therefore, while the relative odds of readmission between delirious and nondelirious patients reported in this study should be generalizable to other community hospitals, the absolute readmission rates reported here may not be comparable to those reported in other studies.
Delirium may represent a marker of more severe illness or medical complications accrued during the hospitalization, which could lead to the associations observed in this study due to confounding.32 Patients with delirium are more likely to be admitted emergently, admitted to the ICU, and feature higher acuity conditions than patients without delirium. We attempted to mitigate this possibility by using a multivariable model to control for variables related to illness severity, including the Charlson comorbidity index, HCUP diagnostic categories, and ICU admission. Despite including HCUP diagnostic categories in our model, we were unable to capture the contribution of certain diseases with finer granularity, such as preexistent dementia, which may also affect clinical outcomes.36 Similarly, although we incorporated markers of illness severity into our model, we were unable to adjust for baseline functional status or frailty, which were not reliably recorded in the electronic medical record but are potential confounders when investigating clinical outcomes including hospital readmission.
We also lacked information regarding the duration of delirium in our cohort. Therefore, we were unable to test whether longer episodes of delirium were more predictive of readmission than shorter episodes.
CONCLUSION
In-hospital delirium is associated with several negative patient outcomes. Our study demonstrates that delirium predicts 30-day readmission and emergency department utilization after hospital discharge. Bearing in mind that a third of hospital-acquired delirium cases may be preventable,32 hospitals should prioritize interventions to reduce postdischarge healthcare utilization and complications in this particularly vulnerable group.
Acknowledgments
The authors would like to acknowledge Dr. Andrew L. Avins for his guidance with the initial development of this project and Julie Fourie for contributing data to the overall study.
Disclosures
Dr. Liu receives funding from NIH K23GM112018 and
Funding
This study was funded by Kaiser Permanente Graduate Medical Education, who approved the design, conduct, and reporting of this study.
1. Bidwell J. Interventions for preventing delirium in hospitalized non-ICU patients: A Cochrane review summary. Int J Nurs Stud. 2017;70:142-143. PubMed
2. Ryan DJ, O’Regan NA, Caoimh RÓ, et al. Delirium in an adult acute hospital population: predictors, prevalence and detection. BMJ Open. 2013;3(1):e001772. PubMed
3. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-598. PubMed
4. Inouye SK. Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord. 1999;10(5):393-400. PubMed
5. Inouye SK, Zhang Y, Jones RN, et al. Risk factors for delirium at discharge: development and validation of a predictive model. Arch Intern Med. 2007;167(13):1406-1413. PubMed
6. LaHue SC, Liu VX. Loud and clear: sensory impairment, delirium, and functional recovery in critical illness. Am J Respir Crit Care Med. 2016;194(3):252-253. PubMed
7. Salluh JI, Soares M, Teles JM, et al. Delirium epidemiology in critical care (DECCA): an international study. Crit Care. 2010;14(6):R210. PubMed
8. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857. PubMed
9. Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753-1762. PubMed
10. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922. PubMed
11. Brown EG, Douglas VC. Moving beyond metabolic encephalopathy: an update on delirium prevention, workup, and management. Semin Neurol. 2015;35(6):646-655. PubMed
12. Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990;263(8):1097-1101. PubMed
13. McCusker J, Cole MG, Dendukuri N, Belzile E. Does delirium increase hospital stay? J Am Geriatr Soc. 2003;51(11):1539-1546. PubMed
14. Salluh JI, Wang H, Schneider EB, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350:h2538. PubMed
15. Abelha FJ, Luís C, Veiga D, et al. Outcome and quality of life in patients with postoperative delirium during an ICU stay following major surgery. Crit Care. 2013;17(5):R257. PubMed
16. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364. PubMed
17. Witlox J, Eurelings LS, de Jonghe JF, et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304(4):443-451. PubMed
18. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242. PubMed
19. Freter S, Koller K, Dunbar M, MacKnight C, Rockwood K. Translating delirium prevention strategies for elderly adults with hip fracture into routine clinical care: A pragmatic clinical trial. J Am Geriatr Soc. 2017;65(3):567-573. PubMed
20. Fong TG, Jones RN, Shi P, et al. Delirium accelerates cognitive decline in Alzheimer disease. Neurology. 2009;72(18):1570-1575. PubMed
21. Girard TD, Jackson JC, Pandharipande PP, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010;38(7):1513-1520. PubMed
22. Berenson RA, Paulus RA, Kalman NS. Medicare’s readmissions-reduction program—a positive alternative. N Engl J Med. 2012;366(15):1364-1366. PubMed
23. Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the hospital readmission reduction program and readmission rates for target and nontarget conditions. JAMA. 2016;316(24):2647-2656. PubMed
24. Elsamadicy AA, Wang TY, Back AG, et al. Post-operative delirium is an independent predictor of 30-day hospital readmission after spine surgery in the elderly (≥65years old): a study of 453 consecutive elderly spine surgery patients. J Clin Neurosci. 2017;41:128-131. PubMed
25. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948. PubMed
26. Inouye SK, Leo-Summers L, Zhang Y, et al. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005;53(2):312-318. PubMed
27. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245-1251. PubMed
28. Escobar GJ, Gardner MN, Greene JD, Draper D, Kipnis P. Risk-adjusting hospital mortality using a comprehensive electronic record in an integrated health care delivery system. Med Care. 2013;51(5):446-453. PubMed
29. Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract. 2002;5(3):143-151. PubMed
30. Lawlor PG, Bush SH. Delirium diagnosis, screening and management. Curr Opin Support Palliat Care. 2014;8(3):286-295. PubMed
31. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. PubMed
32. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210-220. PubMed
33. Leyenaar JK, Lagu T, Lindenauer PK. Direct admission to the hospital: an alternative approach to hospitalization. J Hosp Med. 2016;11(4):303-305. PubMed
34. Wang CL, Ding ST, Hsieh MJ, et al. Factors associated with emergency department visit within 30 days after discharge. BMC Health Serv Res. 2016;16:190. PubMed
35. Shi Q, Warren L, Saposnik G, Macdermid JC. Confusion assessment method: a systematic review and meta-analysis of diagnostic accuracy. Neuropsychiatr Dis Treat. 2013;9:1359-1370. PubMed
36. Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002;50(10):1723-1732. PubMed
1. Bidwell J. Interventions for preventing delirium in hospitalized non-ICU patients: A Cochrane review summary. Int J Nurs Stud. 2017;70:142-143. PubMed
2. Ryan DJ, O’Regan NA, Caoimh RÓ, et al. Delirium in an adult acute hospital population: predictors, prevalence and detection. BMJ Open. 2013;3(1):e001772. PubMed
3. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-598. PubMed
4. Inouye SK. Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord. 1999;10(5):393-400. PubMed
5. Inouye SK, Zhang Y, Jones RN, et al. Risk factors for delirium at discharge: development and validation of a predictive model. Arch Intern Med. 2007;167(13):1406-1413. PubMed
6. LaHue SC, Liu VX. Loud and clear: sensory impairment, delirium, and functional recovery in critical illness. Am J Respir Crit Care Med. 2016;194(3):252-253. PubMed
7. Salluh JI, Soares M, Teles JM, et al. Delirium epidemiology in critical care (DECCA): an international study. Crit Care. 2010;14(6):R210. PubMed
8. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857. PubMed
9. Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753-1762. PubMed
10. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922. PubMed
11. Brown EG, Douglas VC. Moving beyond metabolic encephalopathy: an update on delirium prevention, workup, and management. Semin Neurol. 2015;35(6):646-655. PubMed
12. Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990;263(8):1097-1101. PubMed
13. McCusker J, Cole MG, Dendukuri N, Belzile E. Does delirium increase hospital stay? J Am Geriatr Soc. 2003;51(11):1539-1546. PubMed
14. Salluh JI, Wang H, Schneider EB, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350:h2538. PubMed
15. Abelha FJ, Luís C, Veiga D, et al. Outcome and quality of life in patients with postoperative delirium during an ICU stay following major surgery. Crit Care. 2013;17(5):R257. PubMed
16. Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350-364. PubMed
17. Witlox J, Eurelings LS, de Jonghe JF, et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304(4):443-451. PubMed
18. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234-242. PubMed
19. Freter S, Koller K, Dunbar M, MacKnight C, Rockwood K. Translating delirium prevention strategies for elderly adults with hip fracture into routine clinical care: A pragmatic clinical trial. J Am Geriatr Soc. 2017;65(3):567-573. PubMed
20. Fong TG, Jones RN, Shi P, et al. Delirium accelerates cognitive decline in Alzheimer disease. Neurology. 2009;72(18):1570-1575. PubMed
21. Girard TD, Jackson JC, Pandharipande PP, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010;38(7):1513-1520. PubMed
22. Berenson RA, Paulus RA, Kalman NS. Medicare’s readmissions-reduction program—a positive alternative. N Engl J Med. 2012;366(15):1364-1366. PubMed
23. Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the hospital readmission reduction program and readmission rates for target and nontarget conditions. JAMA. 2016;316(24):2647-2656. PubMed
24. Elsamadicy AA, Wang TY, Back AG, et al. Post-operative delirium is an independent predictor of 30-day hospital readmission after spine surgery in the elderly (≥65years old): a study of 453 consecutive elderly spine surgery patients. J Clin Neurosci. 2017;41:128-131. PubMed
25. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948. PubMed
26. Inouye SK, Leo-Summers L, Zhang Y, et al. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005;53(2):312-318. PubMed
27. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245-1251. PubMed
28. Escobar GJ, Gardner MN, Greene JD, Draper D, Kipnis P. Risk-adjusting hospital mortality using a comprehensive electronic record in an integrated health care delivery system. Med Care. 2013;51(5):446-453. PubMed
29. Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract. 2002;5(3):143-151. PubMed
30. Lawlor PG, Bush SH. Delirium diagnosis, screening and management. Curr Opin Support Palliat Care. 2014;8(3):286-295. PubMed
31. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. PubMed
32. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5(4):210-220. PubMed
33. Leyenaar JK, Lagu T, Lindenauer PK. Direct admission to the hospital: an alternative approach to hospitalization. J Hosp Med. 2016;11(4):303-305. PubMed
34. Wang CL, Ding ST, Hsieh MJ, et al. Factors associated with emergency department visit within 30 days after discharge. BMC Health Serv Res. 2016;16:190. PubMed
35. Shi Q, Warren L, Saposnik G, Macdermid JC. Confusion assessment method: a systematic review and meta-analysis of diagnostic accuracy. Neuropsychiatr Dis Treat. 2013;9:1359-1370. PubMed
36. Fick DM, Agostini JV, Inouye SK. Delirium superimposed on dementia: a systematic review. J Am Geriatr Soc. 2002;50(10):1723-1732. PubMed
© 2019 Society of Hospital Medicine