User login
Painless penile papule
A 36-year-old man sought treatment at our outpatient dermatology clinic for an asymptomatic penile lesion that he’d had for a month. He’d been diagnosed with human immunodeficiency virus (HIV) infection 5 years earlier, and was taking highly active antiretroviral therapy of emtricitabine 200 mg/tenofovir 300 mg daily and nevirapine 200 mg twice a day. The patient’s CD4 T-cell count was 530 cells/mm3 (normal for a nonimmunocompromised adult is 500-1200 cells/mm3) and his viral load was undetectable. He wasn’t in a committed relationship and reported having no sexual partners for many years.
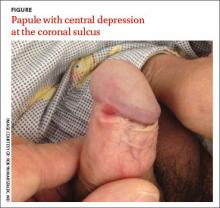
Physical examination revealed an indurated, 7 mm white to pink keratotic papule with a central depression near the coronal sulcus (FIGURE). No ulcers or erosions were seen. The patient denied having urethral discharge, pain, or pruritus. During the previous week, he said he’d applied triamcinolone cream 0.1% twice daily to the area with no improvement.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Syphilis
The asymptomatic nature and clinical presentation of the patient’s lesion prompted us to suspect syphilis. Skin biopsy of the lesion revealed features that were consistent with syphilis and a rapid plasma reagin (RPR) was positive with a titer of 1:32, confirming our suspicions. (His RPR was checked 3 years earlier and it was nonreactive.) Despite the diagnosis, the patient continued to deny having had any recent sexual encounters.
The “great mimicker”
Syphilis infection occurs after inoculation of Treponema pallidum through microscopic breaks in the mucosal surfaces followed by attachment and invasion of spirochete into host cells. Treponemes then multiply and circulate to the regional lymph nodes and internal organs, leading to a variety of clinical manifestations based on the stage of the infection (primary, secondary, and latent/late), the time that has elapsed since inoculation, and the host’s immune response.
Syphilis is often referred to as the “great mimicker” based on its propensity to present as one of a variety of phenotypes. Syphilitic chancres often mimic other genital ulcers, including those caused by different sexually transmitted diseases such as chancroid (as a result of infection with Haemophilus ducreyi) or granuloma inguinale (Klebsiella granulomatis). Syphilitic chancres may also appear clinically similar to genital aphthous ulcers or cutaneous manifestations of herpes simplex virus.
Chancroid. While the tender ulcer of chancroid has a ragged and undermined border with a dirty gray base, the classic, nontender, syphilitic chancre has a clean base with an indurated border reminiscent of the firm quality of cartilage.1
Granuloma inguinale presents as one or multiple nontender, friable, soft, red granulating papules that lack the firm border or clean base of the syphilitic chancre.1
Aphthous ulcers are often soft, shallow, and tender, appearing punched-out with surrounding rims of erythema and clean, white, even bases.2
Genital herpes simplex virus is characterized by tender eroded coalescing vesicles with scalloped, soft borders, contrasted by the indurated smooth rounded border of the syphilitic chancre.1
How syphilis affects HIV, and vice versa
HIV infection has been known to alter the natural history and presentation of syphilis, and syphilis may also impact the course and evaluation of HIV infection.3 Syphilis and other infections that lead to genital ulcers increase an individual’s propensity to acquire HIV due to the loss of the barrier function of the epithelial membrane and the production of cytokines stimulated by treponemal lipoproteins.4 This facilitates transmission of the virus.
In the typical clinical presentation of primary syphilis in an immunocompetent patient, an indolent papule develops 10 to 90 days after inoculation and subsequently ulcerates into an indurated chancre. Patients with HIV may develop multiple chancres that are larger, deeper, and more ulcerative.4-6 Approximately one-quarter of these patients present with lesions of both primary and secondary syphilis at the time of diagnosis.5 However, our patient presented with a solitary painless indurated papule after years of stable and well-controlled HIV infection; this suggests that cutaneous manifestations of syphilis may have atypical clinical presentations in patients who are also infected with HIV.5,6
What you’ll see in the secondary stage
In immunocompetent patients, secondary syphilis is characterized by fever, malaise, lymphadenopathy, moth-eaten alopecia, focal neurologic findings, condyloma lata, mucocutaneous aphthae, and a generalized papulosquamous eruption.7 After 3 to
12 weeks, the secondary infection spontaneously disappears and leads into the latency period, which may last years. Thirty percent of untreated patients progress from latent to tertiary syphilis.7 During this stage, treponemes invade the central nervous system, heart, bone, and skin, triggering vigorous host cellular immune responses and delayed-type hypersensitivity reactions.
When complicated by HIV, secondary syphilis may present along a more aggressive course, with early neurologic and ophthalmologic involvement.8 Patients coinfected with syphilis and HIV are also more prone to developing neurosyphilis—even after completing penicillin therapy—and a more intensive diagnostic evaluation should be considered for such patients.9 Higher protein levels and lower glucose levels in the cerebrospinal fluid are also reported in HIV-infected patients with syphilis,10 likely due to the weakened host immune response.
What you’ll see on the labwork
Like other acute infections, syphilis may cause transient increases in viral load with decreases in the CD4 count that resolve after treatment.11-14 Also worth noting:
- RPR at titers of >1:32 and CD4 counts <350 cells/mm3 may be associated with neurosyphilis in patients with HIV.10
- High RPR titers have been linked to elevated liver function enzymes in patients with syphilis and HIV, although the clinical significance of this is
unknown.15
Treat with penicillin
All stages of syphilis can be treated with penicillin G, a standard benzathine penicillin.16 Adult patients with primary and secondary syphilis should receive a single intramuscular dose of 2.4 million units of benzathine penicillin G.16
Our patient responded well to the recommended course of penicillin therapy and no other systemic signs of the infection were noted. He was also counseled on safe sexual practices and barrier protection.
CORRESPONDENCE
Katherine Masterpol, 955 Main Street Suite G6, Winchester, MA 01890; drkasia@gmail.com
1. Goldsmith, Lowell, Fischer B. Syphilis. Rochester, NY: VisualDx. Available at: http://www.visualdx.com/. Updated January 19, 2015. Accessed February 13, 2015.
2. Allen C, Woo SB. Aphthous Stomatitis. Rochester, NY: VisualDx. Available at: http://www.visualdx.com/. Updated August 21, 2013. Accessed February 13, 2015.
3. Zetola NM, Klausner JD. Syphilis and HIV Infection: an update. Clin Infect Dis. 2007:44:1222-1228.
4. Marra CM. Syphilis and human immunodeficiency virus infection. Semin Neurol. 1992;12:43-50.
5. Rompalo AM, Lawlor J, Seaman P, et al. Modification of syphilitic genital ulcer manifestations by coexistent HIV infection. Sex Transm Dis. 2001;28:448-454.
6. Schöfer H, Imhof M, Thoma-Greber E, et al. Active syphilis in HIV infection: a multicentre retrospective survey. The German AIDS Study Group (GASG). Genitourin Med. 1996;72:176-181.
7. James WD, Berger T, Elston D. Andrew’s Diseases of the Skin: Clinical Dermatology. 11th ed. Philadelphia, PA: Saunders; 2011.
8. Lynn WA, Lightman S. Syphilis and HIV: a dangerous combination. Lancet Infect Dis. 2004;4:456-466.
9. Musher DM. Syphilis, neurosyphilis, penicillin, and AIDS. J Infect Dis. 1991;163:1201-1206.
10. Marra CM, Maxwell CL, Smith SL, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis. 2004;189:369-376.
11. Sadiq ST, McSorley J, Copas AJ, et al. The effects of early syphilis on CD4 counts and HIV-1 RNA viral loads in blood and semen. Sex Transm Infect. 2005;81:380-385.
12. Kofoed K, Gerstoft J, Mathiesen LR, et al. Syphilis and human immunodeficiency virus (HIV)-1 coinfection: influence on CD4 T-cell count, HIV-1 viral load, and treatment response. Sex Transm Dis. 2006;33:143-148.
13. Dyer JR, Eron JJ, Hoffman IF, et al. Association of CD4 cell depletion and elevated blood and seminal plasma human immunodeficiency virus type 1 (HIV-1) RNA concentrations with genital ulcer disease in HIV-1-infected men in Malawi. J Infect Dis. 1998;177:224-227.
14. Buchacz K, Patel P, Taylor M, et al. Syphilis increases HIV viral load and decreases CD4 cell counts in HIV-infected patients with new syphilis infections. AIDS. 2004;18:2075-2079.
15. Palacios R, Navarro F, Narankiewicz D, et al. Liver involvement in HIV-infected patients with early syphilis. Int J STD AIDS. 2013;24:31-33.
16. Centers for Disease Control and Prevention. 2010 STD Treatment Guidelines. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/std/treatment/2010/genital-ulcers.htm#a5. Accessed February 4, 2015.
A 36-year-old man sought treatment at our outpatient dermatology clinic for an asymptomatic penile lesion that he’d had for a month. He’d been diagnosed with human immunodeficiency virus (HIV) infection 5 years earlier, and was taking highly active antiretroviral therapy of emtricitabine 200 mg/tenofovir 300 mg daily and nevirapine 200 mg twice a day. The patient’s CD4 T-cell count was 530 cells/mm3 (normal for a nonimmunocompromised adult is 500-1200 cells/mm3) and his viral load was undetectable. He wasn’t in a committed relationship and reported having no sexual partners for many years.
Physical examination revealed an indurated, 7 mm white to pink keratotic papule with a central depression near the coronal sulcus (FIGURE). No ulcers or erosions were seen. The patient denied having urethral discharge, pain, or pruritus. During the previous week, he said he’d applied triamcinolone cream 0.1% twice daily to the area with no improvement.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Syphilis
The asymptomatic nature and clinical presentation of the patient’s lesion prompted us to suspect syphilis. Skin biopsy of the lesion revealed features that were consistent with syphilis and a rapid plasma reagin (RPR) was positive with a titer of 1:32, confirming our suspicions. (His RPR was checked 3 years earlier and it was nonreactive.) Despite the diagnosis, the patient continued to deny having had any recent sexual encounters.
The “great mimicker”
Syphilis infection occurs after inoculation of Treponema pallidum through microscopic breaks in the mucosal surfaces followed by attachment and invasion of spirochete into host cells. Treponemes then multiply and circulate to the regional lymph nodes and internal organs, leading to a variety of clinical manifestations based on the stage of the infection (primary, secondary, and latent/late), the time that has elapsed since inoculation, and the host’s immune response.
Syphilis is often referred to as the “great mimicker” based on its propensity to present as one of a variety of phenotypes. Syphilitic chancres often mimic other genital ulcers, including those caused by different sexually transmitted diseases such as chancroid (as a result of infection with Haemophilus ducreyi) or granuloma inguinale (Klebsiella granulomatis). Syphilitic chancres may also appear clinically similar to genital aphthous ulcers or cutaneous manifestations of herpes simplex virus.
Chancroid. While the tender ulcer of chancroid has a ragged and undermined border with a dirty gray base, the classic, nontender, syphilitic chancre has a clean base with an indurated border reminiscent of the firm quality of cartilage.1
Granuloma inguinale presents as one or multiple nontender, friable, soft, red granulating papules that lack the firm border or clean base of the syphilitic chancre.1
Aphthous ulcers are often soft, shallow, and tender, appearing punched-out with surrounding rims of erythema and clean, white, even bases.2
Genital herpes simplex virus is characterized by tender eroded coalescing vesicles with scalloped, soft borders, contrasted by the indurated smooth rounded border of the syphilitic chancre.1
How syphilis affects HIV, and vice versa
HIV infection has been known to alter the natural history and presentation of syphilis, and syphilis may also impact the course and evaluation of HIV infection.3 Syphilis and other infections that lead to genital ulcers increase an individual’s propensity to acquire HIV due to the loss of the barrier function of the epithelial membrane and the production of cytokines stimulated by treponemal lipoproteins.4 This facilitates transmission of the virus.
In the typical clinical presentation of primary syphilis in an immunocompetent patient, an indolent papule develops 10 to 90 days after inoculation and subsequently ulcerates into an indurated chancre. Patients with HIV may develop multiple chancres that are larger, deeper, and more ulcerative.4-6 Approximately one-quarter of these patients present with lesions of both primary and secondary syphilis at the time of diagnosis.5 However, our patient presented with a solitary painless indurated papule after years of stable and well-controlled HIV infection; this suggests that cutaneous manifestations of syphilis may have atypical clinical presentations in patients who are also infected with HIV.5,6
What you’ll see in the secondary stage
In immunocompetent patients, secondary syphilis is characterized by fever, malaise, lymphadenopathy, moth-eaten alopecia, focal neurologic findings, condyloma lata, mucocutaneous aphthae, and a generalized papulosquamous eruption.7 After 3 to
12 weeks, the secondary infection spontaneously disappears and leads into the latency period, which may last years. Thirty percent of untreated patients progress from latent to tertiary syphilis.7 During this stage, treponemes invade the central nervous system, heart, bone, and skin, triggering vigorous host cellular immune responses and delayed-type hypersensitivity reactions.
When complicated by HIV, secondary syphilis may present along a more aggressive course, with early neurologic and ophthalmologic involvement.8 Patients coinfected with syphilis and HIV are also more prone to developing neurosyphilis—even after completing penicillin therapy—and a more intensive diagnostic evaluation should be considered for such patients.9 Higher protein levels and lower glucose levels in the cerebrospinal fluid are also reported in HIV-infected patients with syphilis,10 likely due to the weakened host immune response.
What you’ll see on the labwork
Like other acute infections, syphilis may cause transient increases in viral load with decreases in the CD4 count that resolve after treatment.11-14 Also worth noting:
- RPR at titers of >1:32 and CD4 counts <350 cells/mm3 may be associated with neurosyphilis in patients with HIV.10
- High RPR titers have been linked to elevated liver function enzymes in patients with syphilis and HIV, although the clinical significance of this is
unknown.15
Treat with penicillin
All stages of syphilis can be treated with penicillin G, a standard benzathine penicillin.16 Adult patients with primary and secondary syphilis should receive a single intramuscular dose of 2.4 million units of benzathine penicillin G.16
Our patient responded well to the recommended course of penicillin therapy and no other systemic signs of the infection were noted. He was also counseled on safe sexual practices and barrier protection.
CORRESPONDENCE
Katherine Masterpol, 955 Main Street Suite G6, Winchester, MA 01890; drkasia@gmail.com
A 36-year-old man sought treatment at our outpatient dermatology clinic for an asymptomatic penile lesion that he’d had for a month. He’d been diagnosed with human immunodeficiency virus (HIV) infection 5 years earlier, and was taking highly active antiretroviral therapy of emtricitabine 200 mg/tenofovir 300 mg daily and nevirapine 200 mg twice a day. The patient’s CD4 T-cell count was 530 cells/mm3 (normal for a nonimmunocompromised adult is 500-1200 cells/mm3) and his viral load was undetectable. He wasn’t in a committed relationship and reported having no sexual partners for many years.
Physical examination revealed an indurated, 7 mm white to pink keratotic papule with a central depression near the coronal sulcus (FIGURE). No ulcers or erosions were seen. The patient denied having urethral discharge, pain, or pruritus. During the previous week, he said he’d applied triamcinolone cream 0.1% twice daily to the area with no improvement.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Syphilis
The asymptomatic nature and clinical presentation of the patient’s lesion prompted us to suspect syphilis. Skin biopsy of the lesion revealed features that were consistent with syphilis and a rapid plasma reagin (RPR) was positive with a titer of 1:32, confirming our suspicions. (His RPR was checked 3 years earlier and it was nonreactive.) Despite the diagnosis, the patient continued to deny having had any recent sexual encounters.
The “great mimicker”
Syphilis infection occurs after inoculation of Treponema pallidum through microscopic breaks in the mucosal surfaces followed by attachment and invasion of spirochete into host cells. Treponemes then multiply and circulate to the regional lymph nodes and internal organs, leading to a variety of clinical manifestations based on the stage of the infection (primary, secondary, and latent/late), the time that has elapsed since inoculation, and the host’s immune response.
Syphilis is often referred to as the “great mimicker” based on its propensity to present as one of a variety of phenotypes. Syphilitic chancres often mimic other genital ulcers, including those caused by different sexually transmitted diseases such as chancroid (as a result of infection with Haemophilus ducreyi) or granuloma inguinale (Klebsiella granulomatis). Syphilitic chancres may also appear clinically similar to genital aphthous ulcers or cutaneous manifestations of herpes simplex virus.
Chancroid. While the tender ulcer of chancroid has a ragged and undermined border with a dirty gray base, the classic, nontender, syphilitic chancre has a clean base with an indurated border reminiscent of the firm quality of cartilage.1
Granuloma inguinale presents as one or multiple nontender, friable, soft, red granulating papules that lack the firm border or clean base of the syphilitic chancre.1
Aphthous ulcers are often soft, shallow, and tender, appearing punched-out with surrounding rims of erythema and clean, white, even bases.2
Genital herpes simplex virus is characterized by tender eroded coalescing vesicles with scalloped, soft borders, contrasted by the indurated smooth rounded border of the syphilitic chancre.1
How syphilis affects HIV, and vice versa
HIV infection has been known to alter the natural history and presentation of syphilis, and syphilis may also impact the course and evaluation of HIV infection.3 Syphilis and other infections that lead to genital ulcers increase an individual’s propensity to acquire HIV due to the loss of the barrier function of the epithelial membrane and the production of cytokines stimulated by treponemal lipoproteins.4 This facilitates transmission of the virus.
In the typical clinical presentation of primary syphilis in an immunocompetent patient, an indolent papule develops 10 to 90 days after inoculation and subsequently ulcerates into an indurated chancre. Patients with HIV may develop multiple chancres that are larger, deeper, and more ulcerative.4-6 Approximately one-quarter of these patients present with lesions of both primary and secondary syphilis at the time of diagnosis.5 However, our patient presented with a solitary painless indurated papule after years of stable and well-controlled HIV infection; this suggests that cutaneous manifestations of syphilis may have atypical clinical presentations in patients who are also infected with HIV.5,6
What you’ll see in the secondary stage
In immunocompetent patients, secondary syphilis is characterized by fever, malaise, lymphadenopathy, moth-eaten alopecia, focal neurologic findings, condyloma lata, mucocutaneous aphthae, and a generalized papulosquamous eruption.7 After 3 to
12 weeks, the secondary infection spontaneously disappears and leads into the latency period, which may last years. Thirty percent of untreated patients progress from latent to tertiary syphilis.7 During this stage, treponemes invade the central nervous system, heart, bone, and skin, triggering vigorous host cellular immune responses and delayed-type hypersensitivity reactions.
When complicated by HIV, secondary syphilis may present along a more aggressive course, with early neurologic and ophthalmologic involvement.8 Patients coinfected with syphilis and HIV are also more prone to developing neurosyphilis—even after completing penicillin therapy—and a more intensive diagnostic evaluation should be considered for such patients.9 Higher protein levels and lower glucose levels in the cerebrospinal fluid are also reported in HIV-infected patients with syphilis,10 likely due to the weakened host immune response.
What you’ll see on the labwork
Like other acute infections, syphilis may cause transient increases in viral load with decreases in the CD4 count that resolve after treatment.11-14 Also worth noting:
- RPR at titers of >1:32 and CD4 counts <350 cells/mm3 may be associated with neurosyphilis in patients with HIV.10
- High RPR titers have been linked to elevated liver function enzymes in patients with syphilis and HIV, although the clinical significance of this is
unknown.15
Treat with penicillin
All stages of syphilis can be treated with penicillin G, a standard benzathine penicillin.16 Adult patients with primary and secondary syphilis should receive a single intramuscular dose of 2.4 million units of benzathine penicillin G.16
Our patient responded well to the recommended course of penicillin therapy and no other systemic signs of the infection were noted. He was also counseled on safe sexual practices and barrier protection.
CORRESPONDENCE
Katherine Masterpol, 955 Main Street Suite G6, Winchester, MA 01890; drkasia@gmail.com
1. Goldsmith, Lowell, Fischer B. Syphilis. Rochester, NY: VisualDx. Available at: http://www.visualdx.com/. Updated January 19, 2015. Accessed February 13, 2015.
2. Allen C, Woo SB. Aphthous Stomatitis. Rochester, NY: VisualDx. Available at: http://www.visualdx.com/. Updated August 21, 2013. Accessed February 13, 2015.
3. Zetola NM, Klausner JD. Syphilis and HIV Infection: an update. Clin Infect Dis. 2007:44:1222-1228.
4. Marra CM. Syphilis and human immunodeficiency virus infection. Semin Neurol. 1992;12:43-50.
5. Rompalo AM, Lawlor J, Seaman P, et al. Modification of syphilitic genital ulcer manifestations by coexistent HIV infection. Sex Transm Dis. 2001;28:448-454.
6. Schöfer H, Imhof M, Thoma-Greber E, et al. Active syphilis in HIV infection: a multicentre retrospective survey. The German AIDS Study Group (GASG). Genitourin Med. 1996;72:176-181.
7. James WD, Berger T, Elston D. Andrew’s Diseases of the Skin: Clinical Dermatology. 11th ed. Philadelphia, PA: Saunders; 2011.
8. Lynn WA, Lightman S. Syphilis and HIV: a dangerous combination. Lancet Infect Dis. 2004;4:456-466.
9. Musher DM. Syphilis, neurosyphilis, penicillin, and AIDS. J Infect Dis. 1991;163:1201-1206.
10. Marra CM, Maxwell CL, Smith SL, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis. 2004;189:369-376.
11. Sadiq ST, McSorley J, Copas AJ, et al. The effects of early syphilis on CD4 counts and HIV-1 RNA viral loads in blood and semen. Sex Transm Infect. 2005;81:380-385.
12. Kofoed K, Gerstoft J, Mathiesen LR, et al. Syphilis and human immunodeficiency virus (HIV)-1 coinfection: influence on CD4 T-cell count, HIV-1 viral load, and treatment response. Sex Transm Dis. 2006;33:143-148.
13. Dyer JR, Eron JJ, Hoffman IF, et al. Association of CD4 cell depletion and elevated blood and seminal plasma human immunodeficiency virus type 1 (HIV-1) RNA concentrations with genital ulcer disease in HIV-1-infected men in Malawi. J Infect Dis. 1998;177:224-227.
14. Buchacz K, Patel P, Taylor M, et al. Syphilis increases HIV viral load and decreases CD4 cell counts in HIV-infected patients with new syphilis infections. AIDS. 2004;18:2075-2079.
15. Palacios R, Navarro F, Narankiewicz D, et al. Liver involvement in HIV-infected patients with early syphilis. Int J STD AIDS. 2013;24:31-33.
16. Centers for Disease Control and Prevention. 2010 STD Treatment Guidelines. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/std/treatment/2010/genital-ulcers.htm#a5. Accessed February 4, 2015.
1. Goldsmith, Lowell, Fischer B. Syphilis. Rochester, NY: VisualDx. Available at: http://www.visualdx.com/. Updated January 19, 2015. Accessed February 13, 2015.
2. Allen C, Woo SB. Aphthous Stomatitis. Rochester, NY: VisualDx. Available at: http://www.visualdx.com/. Updated August 21, 2013. Accessed February 13, 2015.
3. Zetola NM, Klausner JD. Syphilis and HIV Infection: an update. Clin Infect Dis. 2007:44:1222-1228.
4. Marra CM. Syphilis and human immunodeficiency virus infection. Semin Neurol. 1992;12:43-50.
5. Rompalo AM, Lawlor J, Seaman P, et al. Modification of syphilitic genital ulcer manifestations by coexistent HIV infection. Sex Transm Dis. 2001;28:448-454.
6. Schöfer H, Imhof M, Thoma-Greber E, et al. Active syphilis in HIV infection: a multicentre retrospective survey. The German AIDS Study Group (GASG). Genitourin Med. 1996;72:176-181.
7. James WD, Berger T, Elston D. Andrew’s Diseases of the Skin: Clinical Dermatology. 11th ed. Philadelphia, PA: Saunders; 2011.
8. Lynn WA, Lightman S. Syphilis and HIV: a dangerous combination. Lancet Infect Dis. 2004;4:456-466.
9. Musher DM. Syphilis, neurosyphilis, penicillin, and AIDS. J Infect Dis. 1991;163:1201-1206.
10. Marra CM, Maxwell CL, Smith SL, et al. Cerebrospinal fluid abnormalities in patients with syphilis: association with clinical and laboratory features. J Infect Dis. 2004;189:369-376.
11. Sadiq ST, McSorley J, Copas AJ, et al. The effects of early syphilis on CD4 counts and HIV-1 RNA viral loads in blood and semen. Sex Transm Infect. 2005;81:380-385.
12. Kofoed K, Gerstoft J, Mathiesen LR, et al. Syphilis and human immunodeficiency virus (HIV)-1 coinfection: influence on CD4 T-cell count, HIV-1 viral load, and treatment response. Sex Transm Dis. 2006;33:143-148.
13. Dyer JR, Eron JJ, Hoffman IF, et al. Association of CD4 cell depletion and elevated blood and seminal plasma human immunodeficiency virus type 1 (HIV-1) RNA concentrations with genital ulcer disease in HIV-1-infected men in Malawi. J Infect Dis. 1998;177:224-227.
14. Buchacz K, Patel P, Taylor M, et al. Syphilis increases HIV viral load and decreases CD4 cell counts in HIV-infected patients with new syphilis infections. AIDS. 2004;18:2075-2079.
15. Palacios R, Navarro F, Narankiewicz D, et al. Liver involvement in HIV-infected patients with early syphilis. Int J STD AIDS. 2013;24:31-33.
16. Centers for Disease Control and Prevention. 2010 STD Treatment Guidelines. Centers for Disease Control and Prevention Web site. Available at: http://www.cdc.gov/std/treatment/2010/genital-ulcers.htm#a5. Accessed February 4, 2015.