The idea of performing a tricuspid valve repair during a mitral valve procedure has fueled considerable debate among cardiovascular surgeons largely because the grading of tricuspid regurgitation (TR) has been an unreliable marker, so now may be the time to use a new parameter, Dr. Robert Dion of Genk, Belgium, argues in an expert opinion in the Journal of Thoracic and Cardiovascular Surgery (2015 Nov 20;150:1040-3).
“Therefore, we need a parameter hardly depending on preload,” Dr. Dion said. He noted that many authors have validated the use of annual dilatation of 40 mm or 21mm/m2.
Further, preoperative functional New York Heart Association (NYHA) class plays a major role, Dr. Dion said. TR is progressive in nature and the existence of concomitant mitral valve disease can aggravate annular dilation. The earlier surgeons operate on the mitral valve, the less frequently patients will require tricuspid valve repair at the same time, he said.
The controversy was aired in a report at the 2015 American Association for Thoracic Surgery meeting when Dr. Joanna Chikwe of Mount Sinai Hospital in New York discussed an approach that led to tricuspid valve repair at the time of mitral valve surgery in almost two-thirds of patients. Dr. Chikwe and her coauthors opted for concomitant surgery when patients had moderate TR or tricuspid annular dilatation of 40 mm or greater – a strategy that Dr. Dion said was validated because they reported comparable outcomes in terms of death, morbidity, or pacemaker need. The concomitant repair cured TR and prevented progression at seven years of follow-up; and it induced right ventricle recovery and reduced pulmonary hypertension.
In this opinion piece, Dr. Dion took issue with comments made by Dr. Tirone E. David of the University of Toronto during Dr. Chikwe’s AATS presentation. Dr. David, for whom the David reimplantation technique for aortic root replacement is named, called the technique “overkill,” according to Dr. Dion.
Specifically, Dr. Dion questioned Dr. David’s assertions that the use of rigid rings in mitral valve repair causes TR and that no evidence validates the 40-mm diameter minimum in patients with degenerative mitral valve disease. On the first point, Dr. Dion said no evidence has linked the rigidity of the mitral valve ring and progression of tricuspid regurgitation. On the second, Dr. Dion cited eight studies of progressive tricuspid annular dilation with mitral regurgitation, most of which proposed the 40-mm threshold for concomitant tricuspid valve repair. Since then, the 40-mm threshold has been adopted for both European and American guidelines and validated by five reports from 2011 to 2014.
Dr. Dion said the rationale for using annular dilation rather than TR grade rests on “three poles”: annular dilation does not depend on preload whereas the right ventricle does; documented discrepancies between clinical and hemodynamic data (J Cardiol Surg. 1994 Mar;9(2 suppl):237-41; J Am Coll Cardiol. 2004 Feb. 4;43:405-9); and the idea that TR is “bad” for the patient. He also cited disparities in the number of concomitant repairs performed at leading centers: 7%-10% at the Mayo Clinic and Dr. David’s Toronto center, 25% in Leipzig, 40%-45% in his own clinic and two others, and 65% in Dr. Chikwe’s facility.
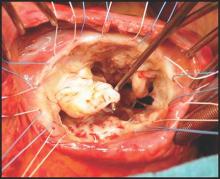
But early intervention for mitral valve dysfunction is a key indicator of the need for concomitant tricuspid valve repair, Dr. Dion said. “The earlier we operate on the MV, the less frequently patients will require tricuspid valve repair,” he said. In his own approach, Dr. Dion uses a transseptal approach of the mitral valve. For TR greater than grade 2, he performs tricuspid repair using a semirigid ring sized on the area of the anterior leaflet tissue; and if the tenting distance is 8 mm or greater, he includes anterior leaflet augmentation. When TR grade is 2 or less, he also performs concomitant tricuspid repair when the tricuspid annulus is 40 mm or greater or when the tricuspid annulus is 3.5-4 mm in the setting of a host of other cardiac problems, from atrial fibrillation to left valve dysfunction. “Otherwise: abstention,” he said.
“The major issue here is to do everything possible to avoid the risk and outcomes of reoperative tricuspid valve surgery,” Dr. Dion said, citing in-hospital death rates of 13.2% that Dr. David reported (Ann Thorac Surg. 2013 Jan;95:119-24.) and 14.6% the Leipzig group reported (J Thorac Cardiovasc Surg. 2013 Oct; 146:841-7).While he acknowledged calls for a prospective, randomized clinical trial, Dr. Dion said the contraindications for concomitant tricuspid valve repair with mitral valve repair have already been well documented.