NATIONAL HARBOR – Measurements of aortic annular geometry, valve calcification, and final device position with two- and three-dimensional echocardiography are predictive of increased risk of leakage after transcatheter valve implantation, according to a retrospective study.
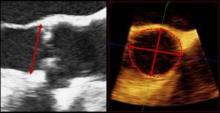
The study also showed that 3-D transesophageal echocardiography (3-D TEE) does a better job of measuring the aortic annulus, compared with 2-D TEE, according to a retrospective study.
The annular measurement is critical for optimal valve sizing and prevention of paravalvular aortic regurgitation in patients undergoing transcatheter aortic valve replacement (TAVR).
Paravalvular aortic regurgitation (PAR), is a known complication of TAVR, and according to 2-year analysis of the PARTNER trial, PAR after TAVR was associated with increased late mortality (N. Engl. J. Med. 2012;366:1686-95).
TAVR is in its infancy in the United States, compared with Europe, and experts are studying how and which imaging techniques could yield the best results before, during, and after TAVR (also called TAVI).
"Every center has their preference," said Dr. Praveen Mehrotra, a noninvasive cardiologist and the lead author of the study at Massachusetts General Hospital in Boston. "Some centers use CT and 2-D TEE. At Mass General, we integrate information obtained from 2-D and 3-D TEE."
Meanwhile, the role of 3-D TEE in TAVR hasn’t been adequately explored, added Dr. Mehrotra, who presented his poster at the annual meeting of the American Society of Echocardiography.
Dr. Mehrotra and his colleagues set out to retrospectively identify 2-D and 3-D TEE parameters that could predict significant PAR after TAVR.
They analyzed 2-D and 3-D TEE images from 94 patients undergoing TAVR between June 2008 and December 2011. The images were used to assess three parameters: annulus geometry, aortic valve apparatus calcification, and final device position.
Twenty one of the patients (22%) showed significant PAR after TAVR, but before postdilation.
In 2-D TEE, the annulus geometry was assessed by measuring the largest anteroposterior annulus dimension at the aortic valve hinge points in mid-systole, the authors wrote. Using 3-D TEE, researchers measured or calculated four parameters for the aortic annulus geometry: minor axis, major axis, eccentricity index, and annular area.
The annular dimension measured by 2-D TEE was similar in the PAR (22.8 mm) and No PAR (22.4 mm) groups. But, the 3-D TEE measurements were significantly larger in the PAR group than in the No PAR group, as measured by annular minor axis (23.8 mm vs. 22.7 mm), major axis (27.0 mm vs. 25.3 mm), eccentricity index (0.88 vs. 0.90), and annular area (5.19 cm2 vs. 4.52 cm2), the researchers reported.
The annular-prosthesis incongruence (API) index was also significantly higher in patients with PAR (1.07% vs. 0.93%), "indicating valve undersizing in this group," the authors wrote.
Using 3-D TEE, the researchers identified and graded significant areas of calcification in the aortic valve apparatus, which is also very important before TAVR, said Mehrotra.
The final device position was assessed using 2-D TEE images.
The results showed that higher API index, Aortic Valve Apparatus Calcification score, and final position of the device were predictors of significant PAR after TAVR, with odds ratios of 9.4, 3.6, and 1.2, respectively, the authors reported.
"Our study highlights the ability of 2-D and 3-D TEE for accurate annular sizing and optimal valve positioning during TAVR," they wrote.
The takeaway message, said Dr. Mehrotra in an interview, is that "the role of echo is essential before, during, and after TAVR.
He added that 3-D echocardiography has an emerging role in annular sizing. In particular, annular area by 3-D TEE may be more important than the anteroposterior dimension by 2-D TEE for accurate valve sizing, said Dr. Mehrotra. "Technologies like 3-D TEE and cardiac CT can help with preprocedural planning, but they should be used by people who understand how to use them."
While his study focused on 2-D and 3-D TEE, Dr. Mehrotra said he expected more studies begin comparing cardiac CT and 3-D TEE, which is more like, "comparing apples to apples."
In a discussion on TAVR imaging, Dr. Rebecca T. Hahn, director of interventional echocardiography at Columbia University, New York, said that cardiac CT and echocardiography are complementary. However, CT is less user-dependent, compared with 3-D TEE.
Dr. Mehrotra and Dr. Hahn had no relevant financial disclosures.