Lateral epicondylitis, also commonly referred to as tennis elbow, is a cumulative trauma disorder (CTD) that affects the extensor tendons of the forearm. Its causative mechanism is repetitive tension and movement of the extensor tendons of the wrist. Characteristic associated movements include supination and pronation of the forearm; these occur frequently during the performance of tasks that require repeated gripping and twisting.1
Among the extensor tendons affected by lateral epicondylitis, the extensor carpi radialis brevis is most commonly identified as the injured tendon.2 While the term epicondylitis implies inflammation as the pathological phenomenon behind this disorder, histologic evidence supports a degenerative process in which a noninflammatory angiofibroblastic tendinosis develops, one that is characterized by degenerative processes, including neovascularization and a disordered collagen matrix.3 In this discussion, therefore, while the disorder will be referred to as lateral epicondylitis (the more common nomenclature), lateral epicondylosis may be a more accurate term.
Pain symptoms described by patients with lateral epicondylitis are thought to be attributable to increasing numbers of free nerve endings in the newly developed granulomatous tissue, in addition to associated synovitis.4 The presence of microvascular damage, a histologic finding in lateral epicondylitis, has also led investigators to suggest several contributing risk factors for tennis elbow, including diabetes and smoking.5
More obscure contributing factors, including psychosocial and socioeconomic concerns, have also been suggested.6
EPIDEMIOLOGY
Though not uncommon in the general population, lateral epicondylitis has a peak incidence in the occupational setting, where its prevalence ranges from 4% to 30%.7 Lateral epicondylitis and other upper-extremity CTD account for 56% of all occupational injuries,8 making them a paramount source of concern for employers and employees alike. In a study of workers’ compensation claims in the United States, van Tulder et al6 found that the mean cost per repetitive strain injury ranged from $5,000 to $8,000. The medical costs and lost work time associated with lateral and medial epicondylitis have been estimated to total more than $22 billion per year in the US alone.7
DIAGNOSIS
Making a diagnosis of lateral epicondylitis is usually straightforward, requiring very little in the way of ancillary testing, such as x-rays or MRI.9
Patient History
A thorough patient history will typically reveal complaints of occupation- or activity-related pain in the lateral elbow, possibly affecting the muscle mass of the forearm.9 Often, the patient will report that symptoms are aggravated by repetitive movements that require strenuous use of the hand, wrist, and/or forearm.10 Examples may include using a screwdriver, grasping a lever, or lifting a heavy load. Occupations associated with risk for lateral epicondylitis include those in the construction industry (eg, plumbers, carpenters) and in manufacturing.
Because a positive association has been established between lateral epicondylitis and ipsilateral rotator cuff tears, carpal tunnel syndrome, and De Quervain’s syndrome, it is important to inquire about any prior history of musculoskeletal injury and coexisting musculoskeletal symptoms. Previous use of oral corticosteroids and a history of smoking are also considered risk factors for lateral epicondylitis.5
Physical Examination
Physical exam findings include reproducible pain at the lateral elbow with resisted supination or wrist dorsiflexion when the forearm is fully extended.9 The examiner may also elicit pain by palpating just distal to the lateral epicondyle over the extensor tendon mass (see Figure 1). Range of motion in the wrist may be diminished due to pain, as when the patient is asked to extend the wrist against resistance. As the condition progresses, the patient may also experience pain and weakness of the forearm with resisted finger motion.
TREATMENT
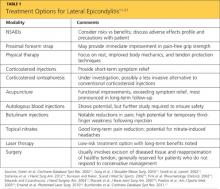
A number of researchers have investigated the most efficacious therapies for lateral epicondylitis (see Table 111-21); as in the case of other musculoskeletal injuries, rest is a cornerstone of treatment. NSAIDs, too, are often indicated, but the clinician must thoroughly evaluate risk versus benefit before initiating NSAID use.11 Additionally, the patient should be educated regarding NSAIDs’ potential side effects and recommended safety precautions.
Two bracing interventions commonly used to treat lateral epicondylitis are the wrist extension splint and the counterforce forearm strap (see Figure 2). In one small prospective, randomized trial (n = 44) in which these devices were compared, no significant between-group differences were found in terms of Mayo Elbow Performance scores, but according to scores derived from American Shoulder and Elbow Society assessments, pain relief was significantly better in patients who wore the wrist extension splint.12 In another study of orthotic management of lateral epicondylosis, immediate improvement in pain-free grip strength was reported in subjects wearing either an elbow strap or an elbow sleeve, but wearers of a wrist splint experienced no immediate change, making it inadvisable as a first-choice orthotic modality.22