Expert Commentary

Webcast: Factors that contribute to overall contraceptive efficacy and risks
In this webcast Dr. Burkman compares perfect and typical use failure rates of the 2 most popular forms of contraception, OCs and condoms, with...
Dr. Creinin is Professor and Director of Family Planning, Department of Obstetrics and Gynecology, University of California, Davis, Sacramento.
Dr. Schimmoeller is a Fellow, Family Planning, Department of Obstetrics and Gynecology, University of California, Davis, Sacramento.
Dr. Creinin reports receiving grant or research support (all of which goes to the Department of Obstetrics and Gynecology, University of California, Davis) from ContraMed, Medicines360, Merck & Co., and the National Institutes of Health/Eunice Kennedy Schriver National Institute of Child Health and Human Development. He reports being a consultant to Allergan, Danco, Estetra, Femasys, HRA Pharma, Lemonaid Health, Medicines360, and Merck & Co. and is a speaker for Allergan and Merck & Co.
Dr. Schimmoeller reports no financial relationships relevant to this article.

In this article
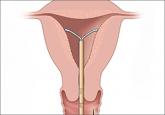
Contraception is an important tool that allows patients to carry out their reproductive-life plans. In the United States, the average woman desires 2 children.1 To achieve this goal, she will spend more than 30 years of her reproductive life avoiding pregnancy.1 The most effective reversible contraceptive methods, the intrauterine device (IUD) and the contraceptive implant, offer an efficient way to cover this significant period. Currently, American women more commonly choose an IUD than an implant by a factor 8 to 1.2 Between 2002 and 2012, the percentage of US contraceptive users aged 15 to 44 using the IUD rose from 2% to 10%.2
Significant barriers to contraceptive access still exist, however. Although widespread reports have lauded the decrease in unintended pregnancies in the United States, improvement only has been marginal for women who live below the poverty level. In fact, for unintended pregnancy the gap between women above and below the poverty level has increased from a 2.6-fold difference in 1994 to a 5.6-fold difference in 2011 (FIGURE).3−5 Since the decrease in the unintended pregnancy rate is most likely related to an increase in contraceptive use, particularly the IUD, we are not providing equal contraceptive access to all women.5
Both the copper IUD and the 3 available levonorgestrel (LNG)-releasing intrauterine system (IUS) products provide safe and effective contraception. As IUD research expands, it is imperative for providers to stay up to date so patients can have full access to these devices.
In this article, we present important updates regarding IUD use that will help break down some continuing barriers to contraceptive access, including:

One in 10 women now use 1 of the 4 available intrauterine devices for contraception. Despite a decrease in the US unintended pregnancy rate over the past 20 years, the gap between rates for women above and below the poverty line has doubled in that same time span to a 5.6-fold difference. New data on IUDs reinforce their use among all women.
Currently, the 2 LNG 52-mg IUS products (Liletta, Mirena) approved by the US Food and Drug Administration (FDA) are available for use for 3 and 5 years, respectively. The pivotal approval trial for Liletta is still ongoing and is planned to continue for up to 7 years.6 The TCu380A (ParaGard) copper IUD is FDA approved for up to 10 years of use; however, this product initially was approved for only 4 years. The duration of use was expanded to 10 years based on continued clinical trials.
Based on current data, we will not need to wait for the Liletta pivotal trial to have clinical evidence of a longer duration of efficacy for the LNG 52-mg IUS. A collaborative group as part of the UNDP/UNFPA/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction performed a multicenter, open-label randomized controlled trial to evaluate outcomes through 7 years of use of the LNG 52-mg IUS and the TCu380A IUD.
A total of 3,836 women were enrolled at 20 centers in Europe, Asia, South America, and China and were randomly assigned to one of the 2 products. Eligible women were aged 16 to 40 years, parous, and without known leiomyoma or recent pelvic infection. After excluding 15 failed IUD insertions, 1,910 women received an LNG 52-mg IUS and 1,911 received a TCu380A. Ultimately, 398 women in the LNG 52-mg IUS group and 682 in the TCu380A group completed 7-year follow-up with the IUD in place. Women were surveyed regarding pregnancy and method discontinuation.
The cumulative 7-year pregnancy rate among LNG 52-mg IUS users was significantly lower than among TCu380A users (0.53 per 100 women vs 2.45 per 100 women, respectively). All pregnancies in the LNG 52-mg IUS group occurred in the first 5 years of study follow-up--with no pregnancies in years 6 through 7 (TABLE). The cumulative pregnancy rate in the TCu380A group in this study is consistent with that in a previous long-term trial of this IUD.7

In this webcast Dr. Burkman compares perfect and typical use failure rates of the 2 most popular forms of contraception, OCs and condoms, with...
Although use of long-acting reversible contraception is increasing slowly in the United States, there is plenty of room for improvement,...

Yes. In 2008, the rate of unintended pregnancy was 54 per 1,000 among women and girls aged 15 to 44 years. In 2011, this rate dropped by 18%, to...

The US unintended pregnancy rate has reached an all-time high. Two experts explore the roots of the problem (cost most paramount) and offer...
