The patient is probably presenting with a moderate asthma exacerbation. To confirm the diagnosis, spirometry assessments should be performed to establish the presence of baseline airway obstruction and determine its severity. Measurements should be obtained before and after inhalation of a short-acting bronchodilator. In addition, chest radiography can help to exclude other diagnoses, and pulse oximetry can exclude hypoxemia.
Asthma is a heterogeneous inflammatory disease and the most common chronic condition among children. Histologically, it is marked by vascular congestion, increased vascular permeability, increased tissue volume, and the presence of an exudate. Because the asthmatic lung undergoes a cycle of injury, repair, and regeneration, inflammation creates histologic changes and functional abnormalities in the airway mucosal epithelium. It is hypothesized that these changes play a major role in the pathophysiology of asthma.
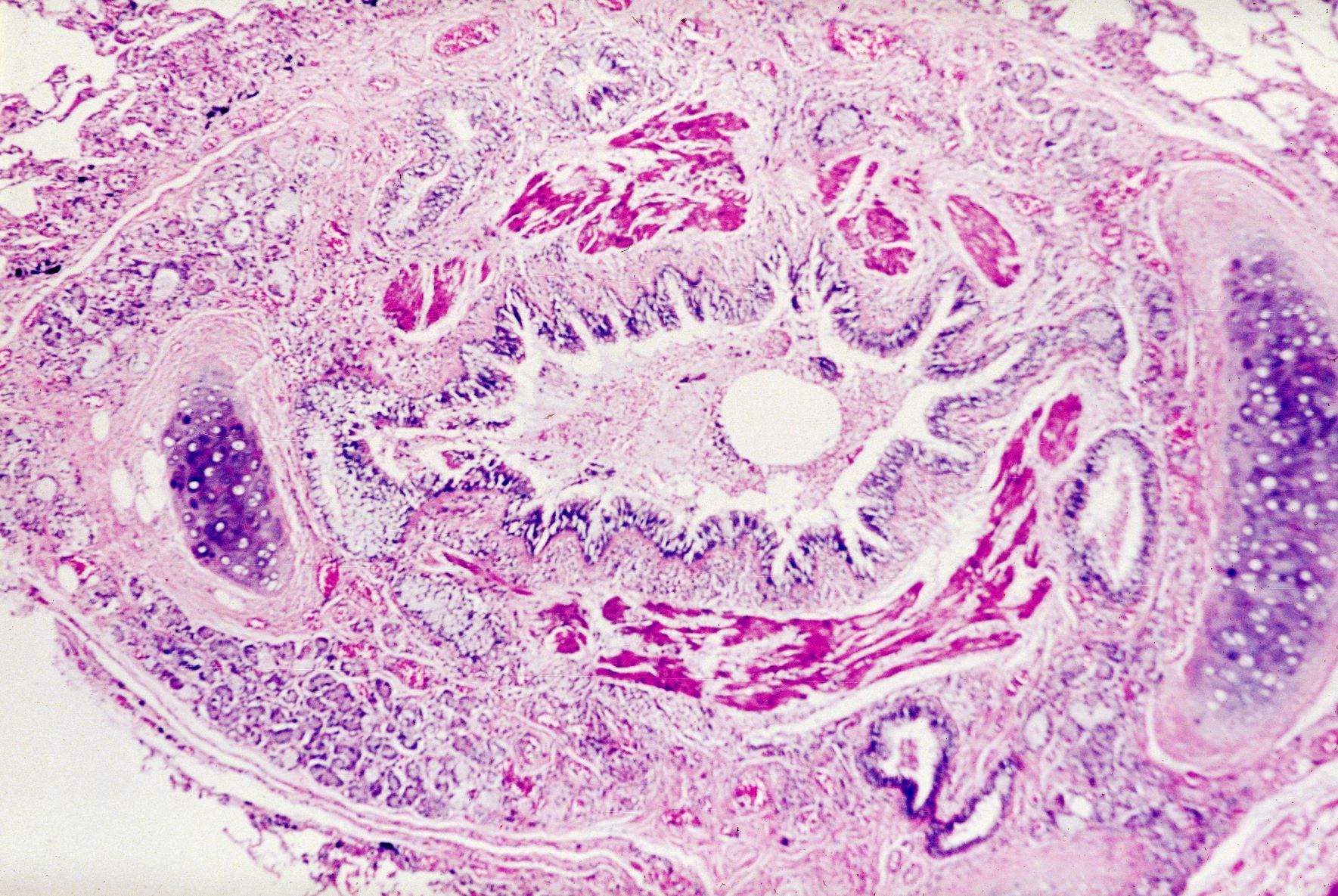
Eosinophilic infiltration is a hallmark of this inflammatory activity. Histologic evaluations of the large airways may also reveal narrowing of lumina, bronchial and bronchiolar epithelial denudation, and mucus plugs. Other relevant findings can include epithelial desquamation and hyperplasia, goblet cell metaplasia, subbasement membrane thickening, smooth muscle hypertrophy or hyperplasia, and submucosal gland hypertrophy. In patients with severe asthma, the basement membrane may be significantly thickened. In terms of the small airways, pathologic study from the lungs of living patients is rarely undertaken, and therefore the histopathologic findings of asthma at the level of the distal airways and alveolated lung parenchyma remains largely unknown.
Asthma is treated using a stepwise approach. As directed for pediatric patients younger than 5 years, the patient in this case may be provided with an as-needed inhaled short-acting beta2-agonist (SABA) and should be followed up every 2-6 weeks while gaining control of her symptoms.
Nathan L. Boyer, MD, Assistant Professor, Department of Medicine, Uniformed Services University, Bethesda, Maryland; Chief of Critical Care, Landstuhl Regional Medical Center, Landstuhl, Germany.
Nathan L. Boyer, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.

 Biophoto Associates/Science Source
Biophoto Associates/Science Source