User login
Case
A 58-year-old male with a past medical history significant for hypertension and hypercholesterolemia presents four hours after acute onset of substernal chest pain that rates eight on a scale of 10. There is no radiation of the pain or associated dyspnea. He describes diaphoresis and nausea. Cardiac enzymes are negative on admission, and the electrocardiogram (ECG) is unchanged. Can computed tomography (CT) coronary angiography effectively rule out coronary disease in this patient admitted with chest pain?
Overview
Approximately 5 million patients presented to U.S. hospitals in 2002 for evaluation of chest pain.1 Less than a third of these patients were ultimately diagnosed with acute coronary syndrome.2 Current strategies to differentiate acute coronary syndrome from non-cardiac causes of chest pain have included electrocardiography, cardiac enzymes, exercise treadmill, echocardiography, and nuclear perfusion.
Unfortunately, each of these modalities has false positive and negative rates that result in a significant number of patients undergoing further evaluation for coronary artery stenosis. Although coronary angiography is the current gold standard to evaluate coronary luminal obstruction, it has many drawbacks. It is costly and inconvenient for patients, invasive, and demonstrates only the later stages of atherosclerosis—not which plaques are prone to rupture. All these limitations necessitate a search for a non-invasive evaluation of the coronary vasculature.
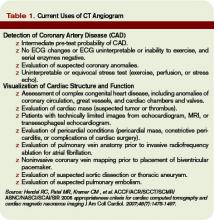
Because 64-slice CT scanners allow for visualization of the cardiac anatomy and coronary vasculature without catheters, there has been increasing interest in this modality to evaluate for coronary artery stenosis in low- to intermediate-risk patients presenting with chest pain. Comparative studies have found it allows for faster, safer evaluation of chest pain with sensitivity and specificity comparable to traditional angiography and a negative predictive value superior to nuclear imaging.3,4
Additional advantages include easy access to CT scanners over cardiac catheterization facilities; 88% of community hospitals with six or more beds had CT scanners in 2004. Further, turnaround is faster (15 to 20 minutes for the CT angiography versus six to eight hours of observation after cardiac catheterization). Also, physicians can simultaneously exclude other life-threatening causes of chest pain including aortic dissection and pulmonary embolus.5 Finally, CT angiography is less expensive (about $800 to $1,000) than invasive coronary angiography (approximately $3,000 to $4,000).6
Review of the Data
Patients undergoing CT angiography require a target heart rate of less than 70 beats per minute. Oral or intravenous beta-blockers are typically given prior to the procedure.
Nitroglycerin 0.4-0.8 mg is also administered sublingually to enhance visualization of the coronary vasculature.
Pulse, ECG, and blood pressure are monitored throughout the imaging process. Initially, a non-contrast scan is performed for coronary artery calcium (CAC) scoring. This is followed by angiography using a bolus of iodinated contrast. At this time, multislice cardiac scanning is synchronized with an ECG (i.e., gating the scan) and images are obtained during diastole.
Two types of CT are capable of obtaining the necessary high-speed images. Electron-beam CT (EBCT) and helical or spiral CT scanning. Multidetector helical CT (MDCT) or multislice CT (MSCT) is an evolution of helical CT. MDCT is available in four-, eight-, 16-, 32-, or 64-slice. Interpretation of the imaging uses the American College of Cardiology nomenclature: no stenosis, insignificant stenosis (less than 50% of coronary luminal diameter), significant stenosis (more than 50%), and total occlusion.
The presence of CAC has been shown in numerous studies to have prognostic significance for cardiac events and death. An elevated CAC score more accurately predicts coronary heart disease (CHD) risk in adults with an initial Framingham risk score between 10% and 19%. In addition, compared with a CAC score of zero, a score of more than 300 was predictive of CHD risk.7
Some studies suggest negative CAC scores alone are enough to risk-stratify patients presenting with chest pain, reporting sensitivities between 96% and 100% for the detection of significant cardiac events.8
Clinical studies of CT angiography typically consist of patients already selected to receive traditional invasive coronary angiography. Initial reports by Leschka, et al., showed sensitivity and specificity of 94% and 97%, respectively, with positive predictive values and negative predictive values of 87% and 99%.9
Additionally, a meta-analysis revealed multislice computed tomography (MSCT) for the diagnosis of CHD was highly sensitive (95% to 100%) for the detection of significant CHD. Specificity was 100% with the 64-slice MSCT and only slightly lower with the four- and 16-slice scanners (87%). A positive predictive value of 66% and negative predictive value of 98% for the presence of significant coronary stenosis have also been reported.10
Gallagher, et al., and previous studies comparing CT angiography with traditional invasive coronary angiography suggest further testing, such as stress nuclear imaging for any patient with stenosis more than 25% or CCS of greater than 100 and further recommends cardiac catheterization of any patient with greater than 70% stenosis by MSCT.
The utility of CT coronary angiography in the evaluation of patients presenting to the ED with chest pain was studied by Goldstein and peers.11 A randomized trial was conducted with patients admitted with chest pain or anginal equivalent, considered to be at low risk for CAD. Patients with negative cardiac enzymes and non-diagnostic ECG were assigned to either MSCCT or myocardial perfusion scan. CT angiography was adequate to diagnose or exclude CAD as the cause of chest pain in 75% of patients. The remaining 25% of patients had additional nuclear stress imaging. Average cost of the MDCT cohort was $1,586 compared with $1,872 for standard diagnostic evaluation. The time required for diagnosis was significantly shorter in the CT cohort: 3.4 hours, compared with 15 hours in the standard group.
An ongoing study at Beaumont Hospital in Royal Oak, Mich., is evaluating the length of stay and cost of care in patients presenting to the ED with chest pain. Patients are randomized to standard evaluation with serial enzymes, ECG, and nuclear perfusion testing or 64-slice CT angiography, plus coronary calcium score. Preliminary results presented at the 2006 American College of Cardiology Annual Scientific Session regarding the initial 200 patients showed a shorter length of stay and lower cost of care with similar patient outcomes in the group that underwent CT angiography.12
A large randomized controlled trial, Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT), is planned to definitively study the use of coronary CT angiography in low-risk patients with chest pain. The large-scale study will involve 750 patients in 15 U.S. hospitals.
CT angiography remains limited despite many recent advances. A stable rhythm is a prerequisite, precluding use in patients with atrial fibrillation or frequent extra-systoles. Also, the required dose of 80 cc to 100 cc of iodinated contrast puts patients at risk for contrast-induced nephropathy, especially those with renal insufficiency.
Finally, radiation exposure is higher than that required for cardiac catheterization.13 Coronary calcification interferes with the images obtained by CT. Therefore, patients with heavy coronary calcium burden (CAC more than 400) may have reduced specificity and negative predictive value. Because this calcification increases with age, the diagnostic accuracy of CT angiography may decrease with age.
Morbidly obese patients may also have decreased image quality. Raff. et al., found significant stenosis in patients with normal body-mass index (BMI) (less than 25 kg/m2). Sensitivity, specificity, and positive and negative predictive values were all 100% and remained accurate in overweight patients. When BMI was more than 30, sensitivity and specificity were reduced to 90% and 86%, respectively.
Visualization of the coronary artery within a stent may be less accurate with CT angiography due to beam artifact, but evaluation of native coronary arteries and bypass grafts maintain similar sensitivity and specificity in these patients.14 A final concern is that CT angiography is only diagnostic. Although only 25% to 30% of diagnostic cardiac catheterizations reveal disease that meets criteria for stent placement, the study is redundant in these high-risk patients, who likely will be referred for traditional coronary angiography with stenting.
Back to the Case
The patient underwent nuclear stress testing the morning following admission. He had minimal attenuation in the infero-lateral distribution. A 64-slice CT angiogram was obtained, and images of the coronary anatomy demonstrated no plaque. The patient was reassured, and no further cardiac imaging was pursued. TH
Dr. Jenkins is an associate clinical professor and associate chief of hospital medicine in the Department of Family Medicine and Community Health at the University of Massachusetts medical school, Worcester.
References
- Statistics CNCH, ed. National Hospital Ambulatory Medical Care Survey: 2002 Emergency Department Summary, 2004. Available at www.cdc.gov/nchs/pressroom/04facts/emergencydept.htm. Last accessed Nov. 8, 2007.
- Kohn MA, Kwan E, Gupta M, et al. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med. 2005;29(4):383-390.
- Stein PD, Beemath A, Kayali F, et al. Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am J Med. 2006;119(3):203-216.
- Gallagher MJ, Ross MA, Raff G, et al. The diagnostic accuracy of 64-slice computed tomography coronary angiography compared with stress nuclear imaging in emergency department low-risk chest pain patients. Ann of Emerg Med. 200;49(2):125-136.
- AHA Hospital Statistics, 2006 Edition. Chicago: American Hospital Association; 2006:158, 161.
- Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet. Available at www.ahrq.gov/data/hcup. Last accessed Nov. 8, 2007.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210-215.
- Kondos GT, Hoff JA, Sevrkov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5,635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107(20):2571-2676.
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;177:1482-1487.
- Raff GL, Gallagher MJ, O’Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552-557.
- Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863-871.
- Raff GL, Gallagher MJ, O’Neill WW. Immediate coronary artery computed tomographic angiography rapidly and definitively excludes coronary artery disease in low-risk acute chest pain. Abstract 807-8. 55th Annual Scientific Session of the American College of Cardiology, March 11-14, 2006.
- de Feyter PJ, Nieman K. Noninvasive multi-slice computed tomography coronary angiography: an emerging clinical modality. J Am Coll Cardiol. 2004;44(6):1238-1240.
- Garcia MJ. Noninvasive coronary angiography: hype or new paradigm? J Am Med Assoc. 2005; 293:2531-2533.
Case
A 58-year-old male with a past medical history significant for hypertension and hypercholesterolemia presents four hours after acute onset of substernal chest pain that rates eight on a scale of 10. There is no radiation of the pain or associated dyspnea. He describes diaphoresis and nausea. Cardiac enzymes are negative on admission, and the electrocardiogram (ECG) is unchanged. Can computed tomography (CT) coronary angiography effectively rule out coronary disease in this patient admitted with chest pain?
Overview
Approximately 5 million patients presented to U.S. hospitals in 2002 for evaluation of chest pain.1 Less than a third of these patients were ultimately diagnosed with acute coronary syndrome.2 Current strategies to differentiate acute coronary syndrome from non-cardiac causes of chest pain have included electrocardiography, cardiac enzymes, exercise treadmill, echocardiography, and nuclear perfusion.
Unfortunately, each of these modalities has false positive and negative rates that result in a significant number of patients undergoing further evaluation for coronary artery stenosis. Although coronary angiography is the current gold standard to evaluate coronary luminal obstruction, it has many drawbacks. It is costly and inconvenient for patients, invasive, and demonstrates only the later stages of atherosclerosis—not which plaques are prone to rupture. All these limitations necessitate a search for a non-invasive evaluation of the coronary vasculature.
Because 64-slice CT scanners allow for visualization of the cardiac anatomy and coronary vasculature without catheters, there has been increasing interest in this modality to evaluate for coronary artery stenosis in low- to intermediate-risk patients presenting with chest pain. Comparative studies have found it allows for faster, safer evaluation of chest pain with sensitivity and specificity comparable to traditional angiography and a negative predictive value superior to nuclear imaging.3,4
Additional advantages include easy access to CT scanners over cardiac catheterization facilities; 88% of community hospitals with six or more beds had CT scanners in 2004. Further, turnaround is faster (15 to 20 minutes for the CT angiography versus six to eight hours of observation after cardiac catheterization). Also, physicians can simultaneously exclude other life-threatening causes of chest pain including aortic dissection and pulmonary embolus.5 Finally, CT angiography is less expensive (about $800 to $1,000) than invasive coronary angiography (approximately $3,000 to $4,000).6
Review of the Data
Patients undergoing CT angiography require a target heart rate of less than 70 beats per minute. Oral or intravenous beta-blockers are typically given prior to the procedure.
Nitroglycerin 0.4-0.8 mg is also administered sublingually to enhance visualization of the coronary vasculature.
Pulse, ECG, and blood pressure are monitored throughout the imaging process. Initially, a non-contrast scan is performed for coronary artery calcium (CAC) scoring. This is followed by angiography using a bolus of iodinated contrast. At this time, multislice cardiac scanning is synchronized with an ECG (i.e., gating the scan) and images are obtained during diastole.
Two types of CT are capable of obtaining the necessary high-speed images. Electron-beam CT (EBCT) and helical or spiral CT scanning. Multidetector helical CT (MDCT) or multislice CT (MSCT) is an evolution of helical CT. MDCT is available in four-, eight-, 16-, 32-, or 64-slice. Interpretation of the imaging uses the American College of Cardiology nomenclature: no stenosis, insignificant stenosis (less than 50% of coronary luminal diameter), significant stenosis (more than 50%), and total occlusion.
The presence of CAC has been shown in numerous studies to have prognostic significance for cardiac events and death. An elevated CAC score more accurately predicts coronary heart disease (CHD) risk in adults with an initial Framingham risk score between 10% and 19%. In addition, compared with a CAC score of zero, a score of more than 300 was predictive of CHD risk.7
Some studies suggest negative CAC scores alone are enough to risk-stratify patients presenting with chest pain, reporting sensitivities between 96% and 100% for the detection of significant cardiac events.8
Clinical studies of CT angiography typically consist of patients already selected to receive traditional invasive coronary angiography. Initial reports by Leschka, et al., showed sensitivity and specificity of 94% and 97%, respectively, with positive predictive values and negative predictive values of 87% and 99%.9
Additionally, a meta-analysis revealed multislice computed tomography (MSCT) for the diagnosis of CHD was highly sensitive (95% to 100%) for the detection of significant CHD. Specificity was 100% with the 64-slice MSCT and only slightly lower with the four- and 16-slice scanners (87%). A positive predictive value of 66% and negative predictive value of 98% for the presence of significant coronary stenosis have also been reported.10
Gallagher, et al., and previous studies comparing CT angiography with traditional invasive coronary angiography suggest further testing, such as stress nuclear imaging for any patient with stenosis more than 25% or CCS of greater than 100 and further recommends cardiac catheterization of any patient with greater than 70% stenosis by MSCT.
The utility of CT coronary angiography in the evaluation of patients presenting to the ED with chest pain was studied by Goldstein and peers.11 A randomized trial was conducted with patients admitted with chest pain or anginal equivalent, considered to be at low risk for CAD. Patients with negative cardiac enzymes and non-diagnostic ECG were assigned to either MSCCT or myocardial perfusion scan. CT angiography was adequate to diagnose or exclude CAD as the cause of chest pain in 75% of patients. The remaining 25% of patients had additional nuclear stress imaging. Average cost of the MDCT cohort was $1,586 compared with $1,872 for standard diagnostic evaluation. The time required for diagnosis was significantly shorter in the CT cohort: 3.4 hours, compared with 15 hours in the standard group.
An ongoing study at Beaumont Hospital in Royal Oak, Mich., is evaluating the length of stay and cost of care in patients presenting to the ED with chest pain. Patients are randomized to standard evaluation with serial enzymes, ECG, and nuclear perfusion testing or 64-slice CT angiography, plus coronary calcium score. Preliminary results presented at the 2006 American College of Cardiology Annual Scientific Session regarding the initial 200 patients showed a shorter length of stay and lower cost of care with similar patient outcomes in the group that underwent CT angiography.12
A large randomized controlled trial, Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT), is planned to definitively study the use of coronary CT angiography in low-risk patients with chest pain. The large-scale study will involve 750 patients in 15 U.S. hospitals.
CT angiography remains limited despite many recent advances. A stable rhythm is a prerequisite, precluding use in patients with atrial fibrillation or frequent extra-systoles. Also, the required dose of 80 cc to 100 cc of iodinated contrast puts patients at risk for contrast-induced nephropathy, especially those with renal insufficiency.
Finally, radiation exposure is higher than that required for cardiac catheterization.13 Coronary calcification interferes with the images obtained by CT. Therefore, patients with heavy coronary calcium burden (CAC more than 400) may have reduced specificity and negative predictive value. Because this calcification increases with age, the diagnostic accuracy of CT angiography may decrease with age.
Morbidly obese patients may also have decreased image quality. Raff. et al., found significant stenosis in patients with normal body-mass index (BMI) (less than 25 kg/m2). Sensitivity, specificity, and positive and negative predictive values were all 100% and remained accurate in overweight patients. When BMI was more than 30, sensitivity and specificity were reduced to 90% and 86%, respectively.
Visualization of the coronary artery within a stent may be less accurate with CT angiography due to beam artifact, but evaluation of native coronary arteries and bypass grafts maintain similar sensitivity and specificity in these patients.14 A final concern is that CT angiography is only diagnostic. Although only 25% to 30% of diagnostic cardiac catheterizations reveal disease that meets criteria for stent placement, the study is redundant in these high-risk patients, who likely will be referred for traditional coronary angiography with stenting.
Back to the Case
The patient underwent nuclear stress testing the morning following admission. He had minimal attenuation in the infero-lateral distribution. A 64-slice CT angiogram was obtained, and images of the coronary anatomy demonstrated no plaque. The patient was reassured, and no further cardiac imaging was pursued. TH
Dr. Jenkins is an associate clinical professor and associate chief of hospital medicine in the Department of Family Medicine and Community Health at the University of Massachusetts medical school, Worcester.
References
- Statistics CNCH, ed. National Hospital Ambulatory Medical Care Survey: 2002 Emergency Department Summary, 2004. Available at www.cdc.gov/nchs/pressroom/04facts/emergencydept.htm. Last accessed Nov. 8, 2007.
- Kohn MA, Kwan E, Gupta M, et al. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med. 2005;29(4):383-390.
- Stein PD, Beemath A, Kayali F, et al. Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am J Med. 2006;119(3):203-216.
- Gallagher MJ, Ross MA, Raff G, et al. The diagnostic accuracy of 64-slice computed tomography coronary angiography compared with stress nuclear imaging in emergency department low-risk chest pain patients. Ann of Emerg Med. 200;49(2):125-136.
- AHA Hospital Statistics, 2006 Edition. Chicago: American Hospital Association; 2006:158, 161.
- Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet. Available at www.ahrq.gov/data/hcup. Last accessed Nov. 8, 2007.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210-215.
- Kondos GT, Hoff JA, Sevrkov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5,635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107(20):2571-2676.
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;177:1482-1487.
- Raff GL, Gallagher MJ, O’Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552-557.
- Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863-871.
- Raff GL, Gallagher MJ, O’Neill WW. Immediate coronary artery computed tomographic angiography rapidly and definitively excludes coronary artery disease in low-risk acute chest pain. Abstract 807-8. 55th Annual Scientific Session of the American College of Cardiology, March 11-14, 2006.
- de Feyter PJ, Nieman K. Noninvasive multi-slice computed tomography coronary angiography: an emerging clinical modality. J Am Coll Cardiol. 2004;44(6):1238-1240.
- Garcia MJ. Noninvasive coronary angiography: hype or new paradigm? J Am Med Assoc. 2005; 293:2531-2533.
Case
A 58-year-old male with a past medical history significant for hypertension and hypercholesterolemia presents four hours after acute onset of substernal chest pain that rates eight on a scale of 10. There is no radiation of the pain or associated dyspnea. He describes diaphoresis and nausea. Cardiac enzymes are negative on admission, and the electrocardiogram (ECG) is unchanged. Can computed tomography (CT) coronary angiography effectively rule out coronary disease in this patient admitted with chest pain?
Overview
Approximately 5 million patients presented to U.S. hospitals in 2002 for evaluation of chest pain.1 Less than a third of these patients were ultimately diagnosed with acute coronary syndrome.2 Current strategies to differentiate acute coronary syndrome from non-cardiac causes of chest pain have included electrocardiography, cardiac enzymes, exercise treadmill, echocardiography, and nuclear perfusion.
Unfortunately, each of these modalities has false positive and negative rates that result in a significant number of patients undergoing further evaluation for coronary artery stenosis. Although coronary angiography is the current gold standard to evaluate coronary luminal obstruction, it has many drawbacks. It is costly and inconvenient for patients, invasive, and demonstrates only the later stages of atherosclerosis—not which plaques are prone to rupture. All these limitations necessitate a search for a non-invasive evaluation of the coronary vasculature.
Because 64-slice CT scanners allow for visualization of the cardiac anatomy and coronary vasculature without catheters, there has been increasing interest in this modality to evaluate for coronary artery stenosis in low- to intermediate-risk patients presenting with chest pain. Comparative studies have found it allows for faster, safer evaluation of chest pain with sensitivity and specificity comparable to traditional angiography and a negative predictive value superior to nuclear imaging.3,4
Additional advantages include easy access to CT scanners over cardiac catheterization facilities; 88% of community hospitals with six or more beds had CT scanners in 2004. Further, turnaround is faster (15 to 20 minutes for the CT angiography versus six to eight hours of observation after cardiac catheterization). Also, physicians can simultaneously exclude other life-threatening causes of chest pain including aortic dissection and pulmonary embolus.5 Finally, CT angiography is less expensive (about $800 to $1,000) than invasive coronary angiography (approximately $3,000 to $4,000).6
Review of the Data
Patients undergoing CT angiography require a target heart rate of less than 70 beats per minute. Oral or intravenous beta-blockers are typically given prior to the procedure.
Nitroglycerin 0.4-0.8 mg is also administered sublingually to enhance visualization of the coronary vasculature.
Pulse, ECG, and blood pressure are monitored throughout the imaging process. Initially, a non-contrast scan is performed for coronary artery calcium (CAC) scoring. This is followed by angiography using a bolus of iodinated contrast. At this time, multislice cardiac scanning is synchronized with an ECG (i.e., gating the scan) and images are obtained during diastole.
Two types of CT are capable of obtaining the necessary high-speed images. Electron-beam CT (EBCT) and helical or spiral CT scanning. Multidetector helical CT (MDCT) or multislice CT (MSCT) is an evolution of helical CT. MDCT is available in four-, eight-, 16-, 32-, or 64-slice. Interpretation of the imaging uses the American College of Cardiology nomenclature: no stenosis, insignificant stenosis (less than 50% of coronary luminal diameter), significant stenosis (more than 50%), and total occlusion.
The presence of CAC has been shown in numerous studies to have prognostic significance for cardiac events and death. An elevated CAC score more accurately predicts coronary heart disease (CHD) risk in adults with an initial Framingham risk score between 10% and 19%. In addition, compared with a CAC score of zero, a score of more than 300 was predictive of CHD risk.7
Some studies suggest negative CAC scores alone are enough to risk-stratify patients presenting with chest pain, reporting sensitivities between 96% and 100% for the detection of significant cardiac events.8
Clinical studies of CT angiography typically consist of patients already selected to receive traditional invasive coronary angiography. Initial reports by Leschka, et al., showed sensitivity and specificity of 94% and 97%, respectively, with positive predictive values and negative predictive values of 87% and 99%.9
Additionally, a meta-analysis revealed multislice computed tomography (MSCT) for the diagnosis of CHD was highly sensitive (95% to 100%) for the detection of significant CHD. Specificity was 100% with the 64-slice MSCT and only slightly lower with the four- and 16-slice scanners (87%). A positive predictive value of 66% and negative predictive value of 98% for the presence of significant coronary stenosis have also been reported.10
Gallagher, et al., and previous studies comparing CT angiography with traditional invasive coronary angiography suggest further testing, such as stress nuclear imaging for any patient with stenosis more than 25% or CCS of greater than 100 and further recommends cardiac catheterization of any patient with greater than 70% stenosis by MSCT.
The utility of CT coronary angiography in the evaluation of patients presenting to the ED with chest pain was studied by Goldstein and peers.11 A randomized trial was conducted with patients admitted with chest pain or anginal equivalent, considered to be at low risk for CAD. Patients with negative cardiac enzymes and non-diagnostic ECG were assigned to either MSCCT or myocardial perfusion scan. CT angiography was adequate to diagnose or exclude CAD as the cause of chest pain in 75% of patients. The remaining 25% of patients had additional nuclear stress imaging. Average cost of the MDCT cohort was $1,586 compared with $1,872 for standard diagnostic evaluation. The time required for diagnosis was significantly shorter in the CT cohort: 3.4 hours, compared with 15 hours in the standard group.
An ongoing study at Beaumont Hospital in Royal Oak, Mich., is evaluating the length of stay and cost of care in patients presenting to the ED with chest pain. Patients are randomized to standard evaluation with serial enzymes, ECG, and nuclear perfusion testing or 64-slice CT angiography, plus coronary calcium score. Preliminary results presented at the 2006 American College of Cardiology Annual Scientific Session regarding the initial 200 patients showed a shorter length of stay and lower cost of care with similar patient outcomes in the group that underwent CT angiography.12
A large randomized controlled trial, Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT), is planned to definitively study the use of coronary CT angiography in low-risk patients with chest pain. The large-scale study will involve 750 patients in 15 U.S. hospitals.
CT angiography remains limited despite many recent advances. A stable rhythm is a prerequisite, precluding use in patients with atrial fibrillation or frequent extra-systoles. Also, the required dose of 80 cc to 100 cc of iodinated contrast puts patients at risk for contrast-induced nephropathy, especially those with renal insufficiency.
Finally, radiation exposure is higher than that required for cardiac catheterization.13 Coronary calcification interferes with the images obtained by CT. Therefore, patients with heavy coronary calcium burden (CAC more than 400) may have reduced specificity and negative predictive value. Because this calcification increases with age, the diagnostic accuracy of CT angiography may decrease with age.
Morbidly obese patients may also have decreased image quality. Raff. et al., found significant stenosis in patients with normal body-mass index (BMI) (less than 25 kg/m2). Sensitivity, specificity, and positive and negative predictive values were all 100% and remained accurate in overweight patients. When BMI was more than 30, sensitivity and specificity were reduced to 90% and 86%, respectively.
Visualization of the coronary artery within a stent may be less accurate with CT angiography due to beam artifact, but evaluation of native coronary arteries and bypass grafts maintain similar sensitivity and specificity in these patients.14 A final concern is that CT angiography is only diagnostic. Although only 25% to 30% of diagnostic cardiac catheterizations reveal disease that meets criteria for stent placement, the study is redundant in these high-risk patients, who likely will be referred for traditional coronary angiography with stenting.
Back to the Case
The patient underwent nuclear stress testing the morning following admission. He had minimal attenuation in the infero-lateral distribution. A 64-slice CT angiogram was obtained, and images of the coronary anatomy demonstrated no plaque. The patient was reassured, and no further cardiac imaging was pursued. TH
Dr. Jenkins is an associate clinical professor and associate chief of hospital medicine in the Department of Family Medicine and Community Health at the University of Massachusetts medical school, Worcester.
References
- Statistics CNCH, ed. National Hospital Ambulatory Medical Care Survey: 2002 Emergency Department Summary, 2004. Available at www.cdc.gov/nchs/pressroom/04facts/emergencydept.htm. Last accessed Nov. 8, 2007.
- Kohn MA, Kwan E, Gupta M, et al. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med. 2005;29(4):383-390.
- Stein PD, Beemath A, Kayali F, et al. Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am J Med. 2006;119(3):203-216.
- Gallagher MJ, Ross MA, Raff G, et al. The diagnostic accuracy of 64-slice computed tomography coronary angiography compared with stress nuclear imaging in emergency department low-risk chest pain patients. Ann of Emerg Med. 200;49(2):125-136.
- AHA Hospital Statistics, 2006 Edition. Chicago: American Hospital Association; 2006:158, 161.
- Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, HCUPnet. Available at www.ahrq.gov/data/hcup. Last accessed Nov. 8, 2007.
- Greenland P, LaBree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291(2):210-215.
- Kondos GT, Hoff JA, Sevrkov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5,635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107(20):2571-2676.
- Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J. 2005;177:1482-1487.
- Raff GL, Gallagher MJ, O’Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552-557.
- Goldstein JA, Gallagher MJ, O’Neill WW, et al. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49(8):863-871.
- Raff GL, Gallagher MJ, O’Neill WW. Immediate coronary artery computed tomographic angiography rapidly and definitively excludes coronary artery disease in low-risk acute chest pain. Abstract 807-8. 55th Annual Scientific Session of the American College of Cardiology, March 11-14, 2006.
- de Feyter PJ, Nieman K. Noninvasive multi-slice computed tomography coronary angiography: an emerging clinical modality. J Am Coll Cardiol. 2004;44(6):1238-1240.
- Garcia MJ. Noninvasive coronary angiography: hype or new paradigm? J Am Med Assoc. 2005; 293:2531-2533.