In most high-income countries, including the US, HIV-1 infection continues to occur in high-risk groups, especially among men who have sex with men (MSM).2 In the absence of a vaccine, condom use has served as the primary method of preventing infection.
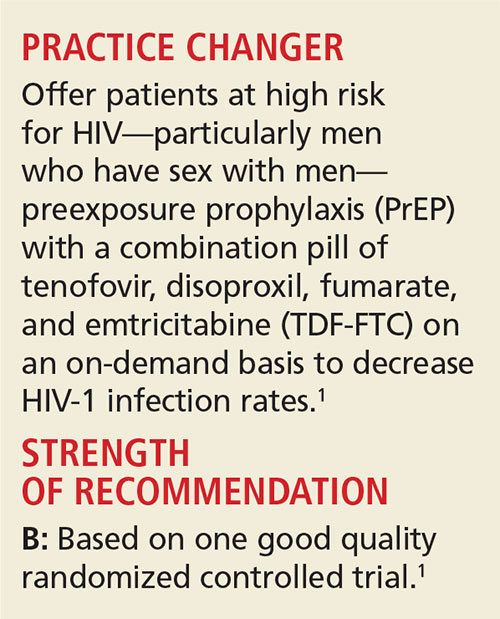
In 2014, the CDC began recommending daily use of tenofovir, disoproxil, fumarate, and emtricitabine (TDF-FTC) in high-risk individuals as a form of preexposure prophylaxis (PrEP).3-5 This recommendation is based primarily on the Preexposure Prophylaxis Initiative (iPrEx) trial, which showed a relative reduction of 44% (number needed to treat [NNT], 46 over 1.2 years) in the incidence of new HIV-1 infection among men and transgender women who have sex with men when TDF-FTC was used on a daily basis.6 However, the effectiveness of this strategy in the real world has not been as high as hoped, presumably due to the difficulty in getting patients to take the medication daily.7,8
While it would likely improve adherence rates, the use of prophylaxis in an on-demand manner is not currently recommended.5 This is because, until now, no studies had demonstrated the effectiveness of PrEP used episodically and taken only around the time of potential exposure.
STUDY SUMMARY
Fewer pills improves adherence, reduces HIV infection rates
The Intervention Preventive de l’Exposition aux Risques avec et pour les Gays study—a double-blind, multicenter study conducted in France and Canada—assessed the efficacy and safety of prophylaxis with TDF-FTC used in an on-demand fashion by MSM.1 The study hypothesis proposed that adherence would be higher if chemoprophylaxis was taken only around the time of intercourse, rather than daily, and that this would further reduce the risk for HIV infection.
The study randomized 414 participants who were considered to be at high risk for acquiring HIV-1 infection—defined as having a history of unprotected anal sex with at least two partners in the past six months. Other inclusion criteria included an age of at least 18 and male or transgender female sex. Exclusion criteria included current HIV infection, hepatitis B or C infection, creatinine clearance < 60 mL/min, alanine aminotransferase level more than 2.5 times the upper limit of normal, and significant glycosuria or proteinuria.
The pill and visit schedule. Those who withdrew consent, were lost to follow-up, or acquired HIV-1 infection were excluded, and the remaining study participants were randomized to take TDF-FTC (n = 199) or placebo (n = 201) before and after sexual activity. The dose of TDF-FTC was fixed at 300 mg of TDF and 200 mg of FTC per pill. Participants were instructed to take a loading dose of two pills of TDF-FTC or placebo with food two to 24 hours prior to intercourse, a third pill 24 hours later, and a fourth pill 24 hours after the third.
If there were multiple consecutive days of sexual intercourse, participants were to take one pill on each day of intercourse, followed by the two postexposure pills. If sexual activity resumed within a week of the prior episode, participants were instructed to take only one pill when resuming the PrEP; otherwise, they were to begin again with two pills two to 24 hours prior to intercourse and repeat the protocol.
Study coordinators followed participants four and eight weeks after enrollment, then every eight weeks subsequently. The investigators tested the participants for HIV-1 and HIV-2 at each visit and assessed adherence by pill count, drug levels in plasma, and with an at-home, computer-assisted interview completed by participants prior to each visit.
Participants received counseling from a peer community member and were offered preventive services and testing for other sexually transmitted infections. They were given free condoms and gel at each visit, as well as enough pills (TDF-FTC or placebo) to cover daily use until their next visit.
Forty-three percent took their assigned pills correctly. Participants were followed for a median of 9.3 months. Overall, 72% of participants took the study drugs (TDF-FTC or placebo), but 29% took a suboptimal dose. There was no change in the sexual behavior of the participants during the study. After 20 months, the study was unblinded and is now continuing as an open-label study because of the discontinuation of another PrEP study in the United Kingdom, which showed an NNT of 13 to prevent one new HIV infection per year.3
An independent data and safety monitoring board recommended the unblinding because the placebo group was considered to be at significantly increased risk for HIV without PrEP. The open-label part of the study (iPrex-OLE) completed enrollment and data gathering in November 2013. The data analysis and results are pending.9
Eighty-six percent experienced relative reduction in HIV. The primary end-point was the diagnosis of HIV-1 infection, and the results were based on an intention-to-treat analysis. HIV-1 infection was diagnosed in 19 study participants, with three of those new cases occurring between the time of randomization and enrollment. Fourteen of the cases were in the placebo group and two of the new cases were in the TDF-FTC group. This translated to an 86% relative reduction in the incidence of new HIV-1 seroconversion in the TDF-FTC group (NNT, 17 over 9.3 months).
The two cases in the TDF-FTC group occurred in participants found to be nonadherent to the prescribed prophylaxis, as they returned 58 and 60 of the 60 pills administered to them, and no study drugs were found in their plasma samples.
Adverse events included gastrointestinal symptoms of nausea, vomiting, diarrhea, and abdominal pain, which were seen more commonly in the treatment group than in the placebo group (14% vs 5%; number needed to harm, 11). There were also mild increases in serum creatinine level, but only two participants had a transient decrease in creatinine clearance to < 60 mL/min. None of the participants discontinued medications due to renal issues.