User login
LAS VEGAS – After participating in an 8-week neuromuscular exercise therapy program, patients with mild to moderate knee osteoarthritis showed significantly greater symptomatic improvement at 12 months of follow-up than if they had been instructed to treat with analgesics and anti-inflammatory agents in the randomized EXERPHARMA trial.
“Neuromuscular exercise could be the superior choice for long-term relief of symptoms such as swelling, stiffness, and catching, while avoiding the potential side effects of analgesics and anti-inflammatory drugs,” Anders Holsgaard-Larsen, MD, said in his presentation of the 1-year study results at the World Congress on Osteoarthritis.
Ninety-three patients with mild to moderate medial knee osteoarthritis – “a group we commonly see in primary care,” he noted – were randomized to the structured 8-week neuromuscular exercise therapy program or to 8 weeks of instruction in the appropriate use of NSAIDs and acetaminophen. The exercise program entailed two hour-long, physical therapist-supervised sessions per week, which included functional, proprioceptive, strength, and endurance exercises of three or four progressive degrees of difficulty.
The initial results obtained at the conclusion of the 8-week interventions – change in knee joint load while walking – have been published (Osteoarthritis Cartilage. 2017 Apr;25[4]:470-80). There was no significant difference between the two study groups. But outcomes at the prespecified 12-month follow-up designed to capture any late improvement were a different story, Dr. Holsgaard-Larsen said at the congress sponsored by the Osteoarthritis Research Society International.
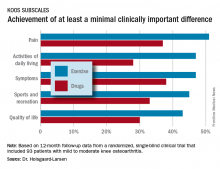
The neuromuscular exercise therapy group showed a significantly greater improvement on the Knee Injury and Osteoarthritis Scores (KOOS) symptom subscale at 12 months: a mean 10.9-point improvement from baseline, compared with a 3.3-point improvement with drug therapy.
That being said, the prespecified primary endpoint at 12 months was change on the activities of daily living subscale – and this between-group difference didn’t reach statistical significance. So technically EXERPHARMA was a negative study, according to the investigator.
That comment caused audience member Theodore P. Pincus, MD, to rise in protest.
“I might argue that perhaps we’ve gotten too focused on P-values rather than looking at the whole picture. In my opinion, your hypothesis is more validated than you seem to think,” said Dr. Pincus, professor of rheumatology at Rush University in Chicago.
The EXERPHARMA trial was funded by the Danish Rheumatism Association and other noncommercial research support. Dr. Holsgaard-Larsen reported having no financial conflicts of interest.
LAS VEGAS – After participating in an 8-week neuromuscular exercise therapy program, patients with mild to moderate knee osteoarthritis showed significantly greater symptomatic improvement at 12 months of follow-up than if they had been instructed to treat with analgesics and anti-inflammatory agents in the randomized EXERPHARMA trial.
“Neuromuscular exercise could be the superior choice for long-term relief of symptoms such as swelling, stiffness, and catching, while avoiding the potential side effects of analgesics and anti-inflammatory drugs,” Anders Holsgaard-Larsen, MD, said in his presentation of the 1-year study results at the World Congress on Osteoarthritis.
Ninety-three patients with mild to moderate medial knee osteoarthritis – “a group we commonly see in primary care,” he noted – were randomized to the structured 8-week neuromuscular exercise therapy program or to 8 weeks of instruction in the appropriate use of NSAIDs and acetaminophen. The exercise program entailed two hour-long, physical therapist-supervised sessions per week, which included functional, proprioceptive, strength, and endurance exercises of three or four progressive degrees of difficulty.
The initial results obtained at the conclusion of the 8-week interventions – change in knee joint load while walking – have been published (Osteoarthritis Cartilage. 2017 Apr;25[4]:470-80). There was no significant difference between the two study groups. But outcomes at the prespecified 12-month follow-up designed to capture any late improvement were a different story, Dr. Holsgaard-Larsen said at the congress sponsored by the Osteoarthritis Research Society International.
The neuromuscular exercise therapy group showed a significantly greater improvement on the Knee Injury and Osteoarthritis Scores (KOOS) symptom subscale at 12 months: a mean 10.9-point improvement from baseline, compared with a 3.3-point improvement with drug therapy.
That being said, the prespecified primary endpoint at 12 months was change on the activities of daily living subscale – and this between-group difference didn’t reach statistical significance. So technically EXERPHARMA was a negative study, according to the investigator.
That comment caused audience member Theodore P. Pincus, MD, to rise in protest.
“I might argue that perhaps we’ve gotten too focused on P-values rather than looking at the whole picture. In my opinion, your hypothesis is more validated than you seem to think,” said Dr. Pincus, professor of rheumatology at Rush University in Chicago.
The EXERPHARMA trial was funded by the Danish Rheumatism Association and other noncommercial research support. Dr. Holsgaard-Larsen reported having no financial conflicts of interest.
LAS VEGAS – After participating in an 8-week neuromuscular exercise therapy program, patients with mild to moderate knee osteoarthritis showed significantly greater symptomatic improvement at 12 months of follow-up than if they had been instructed to treat with analgesics and anti-inflammatory agents in the randomized EXERPHARMA trial.
“Neuromuscular exercise could be the superior choice for long-term relief of symptoms such as swelling, stiffness, and catching, while avoiding the potential side effects of analgesics and anti-inflammatory drugs,” Anders Holsgaard-Larsen, MD, said in his presentation of the 1-year study results at the World Congress on Osteoarthritis.
Ninety-three patients with mild to moderate medial knee osteoarthritis – “a group we commonly see in primary care,” he noted – were randomized to the structured 8-week neuromuscular exercise therapy program or to 8 weeks of instruction in the appropriate use of NSAIDs and acetaminophen. The exercise program entailed two hour-long, physical therapist-supervised sessions per week, which included functional, proprioceptive, strength, and endurance exercises of three or four progressive degrees of difficulty.
The initial results obtained at the conclusion of the 8-week interventions – change in knee joint load while walking – have been published (Osteoarthritis Cartilage. 2017 Apr;25[4]:470-80). There was no significant difference between the two study groups. But outcomes at the prespecified 12-month follow-up designed to capture any late improvement were a different story, Dr. Holsgaard-Larsen said at the congress sponsored by the Osteoarthritis Research Society International.
The neuromuscular exercise therapy group showed a significantly greater improvement on the Knee Injury and Osteoarthritis Scores (KOOS) symptom subscale at 12 months: a mean 10.9-point improvement from baseline, compared with a 3.3-point improvement with drug therapy.
That being said, the prespecified primary endpoint at 12 months was change on the activities of daily living subscale – and this between-group difference didn’t reach statistical significance. So technically EXERPHARMA was a negative study, according to the investigator.
That comment caused audience member Theodore P. Pincus, MD, to rise in protest.
“I might argue that perhaps we’ve gotten too focused on P-values rather than looking at the whole picture. In my opinion, your hypothesis is more validated than you seem to think,” said Dr. Pincus, professor of rheumatology at Rush University in Chicago.
The EXERPHARMA trial was funded by the Danish Rheumatism Association and other noncommercial research support. Dr. Holsgaard-Larsen reported having no financial conflicts of interest.
AT OARSI 2017
Key clinical point:
Major finding: At 12 months of follow-up, patients with knee osteoarthritis who had been assigned to an 8-week structured neuromuscular exercise therapy program had a mean 10.9-point improvement on the KOOS symptom subscale, significantly better than the 3.3-point improvement in patients assigned to primary therapy with NSAIDs and acetaminophen.
Data source: This randomized, single-blind clinical trial included 93 patients with mild to moderate knee osteoarthritis.
Disclosures: The EXERPHARMA trial was funded by the Danish Rheumatism Association and other noncommercial research support. The presenter reported having no financial conflicts of interest.