User login
AMSTERDAM – Patients with RA have a higher risk of developing sarcopenia if they are treated with glucocorticosteroids, study findings suggested.
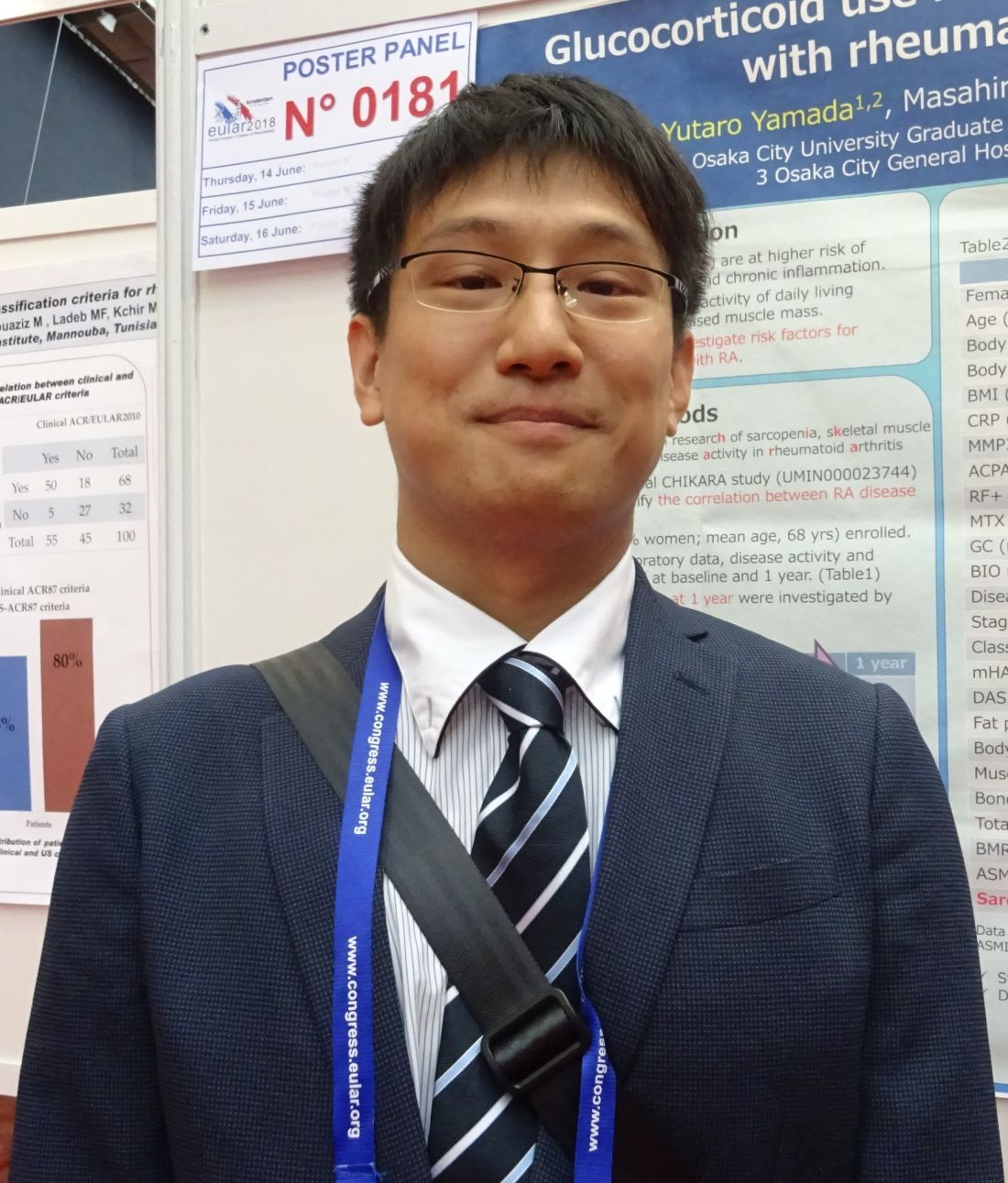
“The strength of our study is that it is a prospective, longitudinal study and this study is the first, to our knowledge, to look at risk factors for sarcopenia limited to RA patients,” Yutaro Yamada, MD, said in an interview at the European Congress of Rheumatology.
Dr. Yamada, of the department of orthopedic surgery at Osaka City University, Japan, said that there is a twofold rationale for looking at risk factors for sarcopenia in RA patients. First, RA causes chronic inflammation and this in turn is thought to lead to a metabolic state that then results in muscle loss. Furthermore, joint dysfunction and subsequent disuse likely contribute to weakening muscles. Second, glucocorticosteroids, which are commonly used to treat patients with RA, have themselves been associated with a low muscle area in prior research.
In 2016, the CHIKARA study was initiated “to clarify the correlation between RA disease activity and sarcopenia,” Dr. Yamada and his associates reported in a poster presentation. They recruited 100 patients, of whom 78% were women, and recorded body weight, muscle mass, fat mass, and predicted bone mass using a body composition analyzer at entry and 1 year later. Laboratory data and disease activity parameters were also assessed, along with radiologic findings and ability to perform activities of daily living. Patients’ treatment was also recorded.
At baseline, the mean age of study participants was 68 years with a mean disease duration of 5.5 years. The majority (86%) had been treated with methotrexate, with 26% also using glucocorticosteroids, and 30% using biologic agents.
Just over one-quarter (28%) were diagnosed with sarcopenia over the course of 1 year. Sarcopenia was defined by criteria agreed by the Asia Working Group on Sarcopenia (Am Med Dir Assoc. 2014;15[2]:95-101) that set thresholds for low muscle mass, low muscle strength, and low physical performance.
Comparing the 9 patients who did develop sarcopenia with the 86 who did not, the researchers found that sarcopenia patients tended to be younger (66.7 vs. 80.2 years), although the difference was not statistically significant. Interestingly, however, more than half (55.6%) of patients who developed sarcopenia were using glucocorticosteroids, compared with 22% of those who were not (P = .029). Of note, the average glucocorticosteroid dose was just 2 mg/day. Patients who developed sarcopenia were also observed to have a lower fat mass (11.7 vs. 15.8, P = .058).
A multiple logistic regression analysis found that using a glucocorticosteroid dose of 2 mg/day or more and lower body fat mass (odds ratio, 0.78; 95% CI 0.61-0.98; P = 0.037) were significant variables for the onset of sarcopenia.
Dr. Yamada noted that 2 mg/day is “a relatively low dose” and so avoiding glucocorticosteroid therapy in those at risk of sarcopenia, particularly those with a low fat mass, may be something to consider.
The study did not receive commercial funding, and Dr. Yamada had no conflicts of interest to disclose.
SOURCE: Yamada Y et al. Ann Rheum Dis. 2018;77(Suppl 2):308-9. Abstract THU0181.
AMSTERDAM – Patients with RA have a higher risk of developing sarcopenia if they are treated with glucocorticosteroids, study findings suggested.
“The strength of our study is that it is a prospective, longitudinal study and this study is the first, to our knowledge, to look at risk factors for sarcopenia limited to RA patients,” Yutaro Yamada, MD, said in an interview at the European Congress of Rheumatology.
Dr. Yamada, of the department of orthopedic surgery at Osaka City University, Japan, said that there is a twofold rationale for looking at risk factors for sarcopenia in RA patients. First, RA causes chronic inflammation and this in turn is thought to lead to a metabolic state that then results in muscle loss. Furthermore, joint dysfunction and subsequent disuse likely contribute to weakening muscles. Second, glucocorticosteroids, which are commonly used to treat patients with RA, have themselves been associated with a low muscle area in prior research.
In 2016, the CHIKARA study was initiated “to clarify the correlation between RA disease activity and sarcopenia,” Dr. Yamada and his associates reported in a poster presentation. They recruited 100 patients, of whom 78% were women, and recorded body weight, muscle mass, fat mass, and predicted bone mass using a body composition analyzer at entry and 1 year later. Laboratory data and disease activity parameters were also assessed, along with radiologic findings and ability to perform activities of daily living. Patients’ treatment was also recorded.
At baseline, the mean age of study participants was 68 years with a mean disease duration of 5.5 years. The majority (86%) had been treated with methotrexate, with 26% also using glucocorticosteroids, and 30% using biologic agents.
Just over one-quarter (28%) were diagnosed with sarcopenia over the course of 1 year. Sarcopenia was defined by criteria agreed by the Asia Working Group on Sarcopenia (Am Med Dir Assoc. 2014;15[2]:95-101) that set thresholds for low muscle mass, low muscle strength, and low physical performance.
Comparing the 9 patients who did develop sarcopenia with the 86 who did not, the researchers found that sarcopenia patients tended to be younger (66.7 vs. 80.2 years), although the difference was not statistically significant. Interestingly, however, more than half (55.6%) of patients who developed sarcopenia were using glucocorticosteroids, compared with 22% of those who were not (P = .029). Of note, the average glucocorticosteroid dose was just 2 mg/day. Patients who developed sarcopenia were also observed to have a lower fat mass (11.7 vs. 15.8, P = .058).
A multiple logistic regression analysis found that using a glucocorticosteroid dose of 2 mg/day or more and lower body fat mass (odds ratio, 0.78; 95% CI 0.61-0.98; P = 0.037) were significant variables for the onset of sarcopenia.
Dr. Yamada noted that 2 mg/day is “a relatively low dose” and so avoiding glucocorticosteroid therapy in those at risk of sarcopenia, particularly those with a low fat mass, may be something to consider.
The study did not receive commercial funding, and Dr. Yamada had no conflicts of interest to disclose.
SOURCE: Yamada Y et al. Ann Rheum Dis. 2018;77(Suppl 2):308-9. Abstract THU0181.
AMSTERDAM – Patients with RA have a higher risk of developing sarcopenia if they are treated with glucocorticosteroids, study findings suggested.
“The strength of our study is that it is a prospective, longitudinal study and this study is the first, to our knowledge, to look at risk factors for sarcopenia limited to RA patients,” Yutaro Yamada, MD, said in an interview at the European Congress of Rheumatology.
Dr. Yamada, of the department of orthopedic surgery at Osaka City University, Japan, said that there is a twofold rationale for looking at risk factors for sarcopenia in RA patients. First, RA causes chronic inflammation and this in turn is thought to lead to a metabolic state that then results in muscle loss. Furthermore, joint dysfunction and subsequent disuse likely contribute to weakening muscles. Second, glucocorticosteroids, which are commonly used to treat patients with RA, have themselves been associated with a low muscle area in prior research.
In 2016, the CHIKARA study was initiated “to clarify the correlation between RA disease activity and sarcopenia,” Dr. Yamada and his associates reported in a poster presentation. They recruited 100 patients, of whom 78% were women, and recorded body weight, muscle mass, fat mass, and predicted bone mass using a body composition analyzer at entry and 1 year later. Laboratory data and disease activity parameters were also assessed, along with radiologic findings and ability to perform activities of daily living. Patients’ treatment was also recorded.
At baseline, the mean age of study participants was 68 years with a mean disease duration of 5.5 years. The majority (86%) had been treated with methotrexate, with 26% also using glucocorticosteroids, and 30% using biologic agents.
Just over one-quarter (28%) were diagnosed with sarcopenia over the course of 1 year. Sarcopenia was defined by criteria agreed by the Asia Working Group on Sarcopenia (Am Med Dir Assoc. 2014;15[2]:95-101) that set thresholds for low muscle mass, low muscle strength, and low physical performance.
Comparing the 9 patients who did develop sarcopenia with the 86 who did not, the researchers found that sarcopenia patients tended to be younger (66.7 vs. 80.2 years), although the difference was not statistically significant. Interestingly, however, more than half (55.6%) of patients who developed sarcopenia were using glucocorticosteroids, compared with 22% of those who were not (P = .029). Of note, the average glucocorticosteroid dose was just 2 mg/day. Patients who developed sarcopenia were also observed to have a lower fat mass (11.7 vs. 15.8, P = .058).
A multiple logistic regression analysis found that using a glucocorticosteroid dose of 2 mg/day or more and lower body fat mass (odds ratio, 0.78; 95% CI 0.61-0.98; P = 0.037) were significant variables for the onset of sarcopenia.
Dr. Yamada noted that 2 mg/day is “a relatively low dose” and so avoiding glucocorticosteroid therapy in those at risk of sarcopenia, particularly those with a low fat mass, may be something to consider.
The study did not receive commercial funding, and Dr. Yamada had no conflicts of interest to disclose.
SOURCE: Yamada Y et al. Ann Rheum Dis. 2018;77(Suppl 2):308-9. Abstract THU0181.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Patients with RA and a lean body mass have a heightened risk of developing sarcopenia if they are treated with glucocorticosteroids.
Major finding: Using glucocorticosteroids at doses of 2 mg/day or more significantly increased the odds of developing sarcopenia (odds ratio, 8.0; 95% confidence interval, 1.17-54.8; P = .034).
Study details: The CHIKARA study – a prospective, observational study involving 100 patients with RA.
Disclosures: The study did not receive commercial funding, and Dr. Yamada had no conflicts of interest to disclose.
Source: Yamada Y et al. Ann Rheum Dis. 2018;77(Suppl 2):308-9. Abstract THU0181.