User login
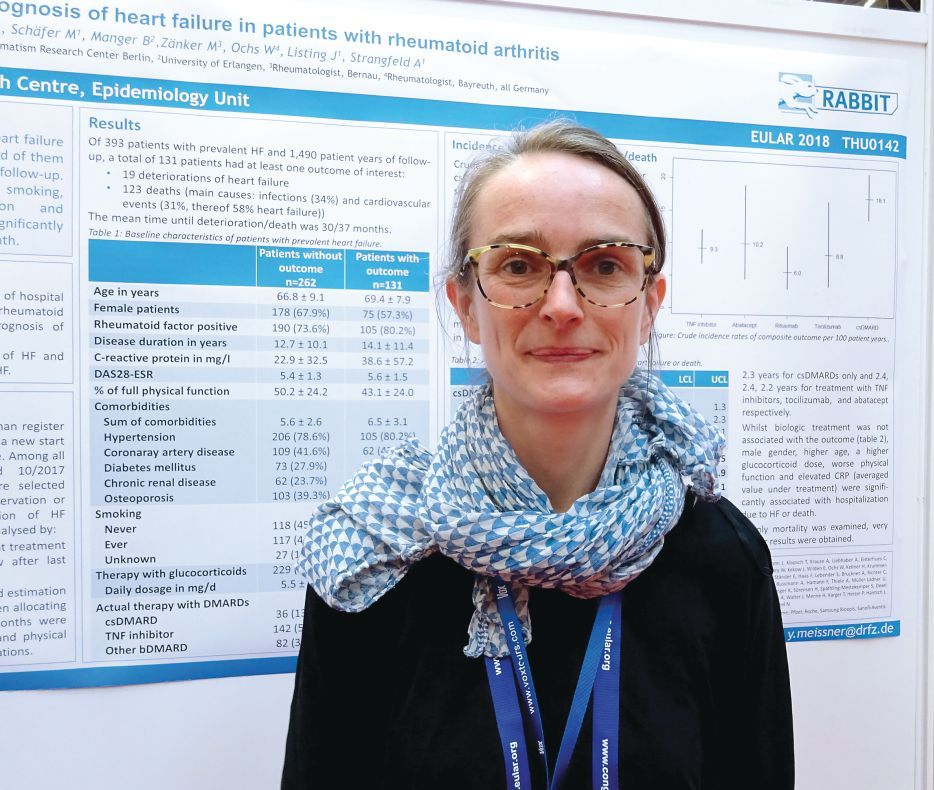
AMSTERDAM – The combination of heart failure and rheumatoid arthritis carries a poor prognosis, according to data from the German biologics register.
Of 393 patients enrolled in RABBIT (Rheumatoide Arthritis: Beobachtung der Biologika-Therapie) who had heart failure in addition to their rheumatoid arthritis, 131 (33%) needed hospital treatment or died over a 10-year period. The mean time to hospitalization or death was 2.5-3.0 years.
“We include patients at the start of their DMARD [disease modifying antirheumatic drug] treatment and follow them up for at least 5 years,” said Dr. Meissner, explaining how the German biologics register works. “For this analysis, we selected all the patients with prevalent heart failure and followed them up until either the database was closed, they dropped out, or had an event.” In this case, an event was defined as a composite of deterioration in heart failure that required hospitalization or death from any cause.
Dr. Meissner, of the German Rheumatism Research Center in Berlin, noted that 19 (14.5%) patients experienced a deterioration in their heart failure and 123 deaths were recorded during the study period that started in May 2001 and ended in October 2017. Around one-third of deaths were attributable to infections (34%), and one-third were attributable to cardiovascular causes (31%). Of the CV deaths, more than half (58%) were attributed to patients’ heart failure.
“What impressed us the most is the number of comorbidities at baseline,” Dr. Meissner said. Not including heart failure or rheumatoid arthritis, patients who experienced an event had an average of 6.5 comorbidities versus 5.6 for those who did not have an event. These additional comorbidities included hypertension, coronary artery disease, diabetes mellitus, chronic renal disease, and osteoporosis.
Crude incidence rates (IRs) for heart failure deterioration or death were calculated according to the rheumatoid arthritis treatment being used and found to be highest in those treated with conventional DMARDs, at 18.1/100 patient-years. IRs with biologic treatments were lower, at 10.2/100 patient-years for abatacept, 9.3 for TNF inhibitors, 8.8 for tocilizumab, and 6.0 for rituximab. What this suggests it that better control of inflammation results in a lower risk for hospitalization and death, Dr. Meissner and her associates reported in their poster presentation.
“If patients are not effectively treated for rheumatoid arthritis, there might be other consequences like the deterioration of heart failure or death,” Dr. Meissner said.
She noted that investigators also looked at identifying risk factors for hospitalization or death and found that there was a greater adjusted relative risk if patients were male (RR = 2.4), older (RR = 1.3 per 5-year increase in age), or if they smoked (RR = 1.7). Using higher doses of glucocorticoids also was a risk factor, with a RR of 1.4 for every 5 mg/day increase in dose.
Better physical function was associated with a lower risk of an event (RR = 0.9) and, along with smoking and adjustment of the steroid dose, is a risk factor that could potentially be influenced, Dr. Meissner proposed.
No data on how the heart failure was being managed are available for this cohort and more research is needed.
“There is still not enough known about this topic, and we need the research to determine how to best manage these patients,” Dr. Meissner said. “The time to an event was only 3 years from the time of inclusion in the register, so we need better management of those patients with heart failure as a comorbidity.”
RABBIT is supported by a joint, unconditional grant from AbbVie, Bristol-Myers Squibb, Celltrion, Hexal AG, Lilly, MSD Sharp & Dohme, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Meissner disclosed being on a speakers bureau for Pfizer.
SOURCE: Meissner Y et al. EULAR 2018 Congress. Abstract THU0142 .
AMSTERDAM – The combination of heart failure and rheumatoid arthritis carries a poor prognosis, according to data from the German biologics register.
Of 393 patients enrolled in RABBIT (Rheumatoide Arthritis: Beobachtung der Biologika-Therapie) who had heart failure in addition to their rheumatoid arthritis, 131 (33%) needed hospital treatment or died over a 10-year period. The mean time to hospitalization or death was 2.5-3.0 years.
“We include patients at the start of their DMARD [disease modifying antirheumatic drug] treatment and follow them up for at least 5 years,” said Dr. Meissner, explaining how the German biologics register works. “For this analysis, we selected all the patients with prevalent heart failure and followed them up until either the database was closed, they dropped out, or had an event.” In this case, an event was defined as a composite of deterioration in heart failure that required hospitalization or death from any cause.
Dr. Meissner, of the German Rheumatism Research Center in Berlin, noted that 19 (14.5%) patients experienced a deterioration in their heart failure and 123 deaths were recorded during the study period that started in May 2001 and ended in October 2017. Around one-third of deaths were attributable to infections (34%), and one-third were attributable to cardiovascular causes (31%). Of the CV deaths, more than half (58%) were attributed to patients’ heart failure.
“What impressed us the most is the number of comorbidities at baseline,” Dr. Meissner said. Not including heart failure or rheumatoid arthritis, patients who experienced an event had an average of 6.5 comorbidities versus 5.6 for those who did not have an event. These additional comorbidities included hypertension, coronary artery disease, diabetes mellitus, chronic renal disease, and osteoporosis.
Crude incidence rates (IRs) for heart failure deterioration or death were calculated according to the rheumatoid arthritis treatment being used and found to be highest in those treated with conventional DMARDs, at 18.1/100 patient-years. IRs with biologic treatments were lower, at 10.2/100 patient-years for abatacept, 9.3 for TNF inhibitors, 8.8 for tocilizumab, and 6.0 for rituximab. What this suggests it that better control of inflammation results in a lower risk for hospitalization and death, Dr. Meissner and her associates reported in their poster presentation.
“If patients are not effectively treated for rheumatoid arthritis, there might be other consequences like the deterioration of heart failure or death,” Dr. Meissner said.
She noted that investigators also looked at identifying risk factors for hospitalization or death and found that there was a greater adjusted relative risk if patients were male (RR = 2.4), older (RR = 1.3 per 5-year increase in age), or if they smoked (RR = 1.7). Using higher doses of glucocorticoids also was a risk factor, with a RR of 1.4 for every 5 mg/day increase in dose.
Better physical function was associated with a lower risk of an event (RR = 0.9) and, along with smoking and adjustment of the steroid dose, is a risk factor that could potentially be influenced, Dr. Meissner proposed.
No data on how the heart failure was being managed are available for this cohort and more research is needed.
“There is still not enough known about this topic, and we need the research to determine how to best manage these patients,” Dr. Meissner said. “The time to an event was only 3 years from the time of inclusion in the register, so we need better management of those patients with heart failure as a comorbidity.”
RABBIT is supported by a joint, unconditional grant from AbbVie, Bristol-Myers Squibb, Celltrion, Hexal AG, Lilly, MSD Sharp & Dohme, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Meissner disclosed being on a speakers bureau for Pfizer.
SOURCE: Meissner Y et al. EULAR 2018 Congress. Abstract THU0142 .
AMSTERDAM – The combination of heart failure and rheumatoid arthritis carries a poor prognosis, according to data from the German biologics register.
Of 393 patients enrolled in RABBIT (Rheumatoide Arthritis: Beobachtung der Biologika-Therapie) who had heart failure in addition to their rheumatoid arthritis, 131 (33%) needed hospital treatment or died over a 10-year period. The mean time to hospitalization or death was 2.5-3.0 years.
“We include patients at the start of their DMARD [disease modifying antirheumatic drug] treatment and follow them up for at least 5 years,” said Dr. Meissner, explaining how the German biologics register works. “For this analysis, we selected all the patients with prevalent heart failure and followed them up until either the database was closed, they dropped out, or had an event.” In this case, an event was defined as a composite of deterioration in heart failure that required hospitalization or death from any cause.
Dr. Meissner, of the German Rheumatism Research Center in Berlin, noted that 19 (14.5%) patients experienced a deterioration in their heart failure and 123 deaths were recorded during the study period that started in May 2001 and ended in October 2017. Around one-third of deaths were attributable to infections (34%), and one-third were attributable to cardiovascular causes (31%). Of the CV deaths, more than half (58%) were attributed to patients’ heart failure.
“What impressed us the most is the number of comorbidities at baseline,” Dr. Meissner said. Not including heart failure or rheumatoid arthritis, patients who experienced an event had an average of 6.5 comorbidities versus 5.6 for those who did not have an event. These additional comorbidities included hypertension, coronary artery disease, diabetes mellitus, chronic renal disease, and osteoporosis.
Crude incidence rates (IRs) for heart failure deterioration or death were calculated according to the rheumatoid arthritis treatment being used and found to be highest in those treated with conventional DMARDs, at 18.1/100 patient-years. IRs with biologic treatments were lower, at 10.2/100 patient-years for abatacept, 9.3 for TNF inhibitors, 8.8 for tocilizumab, and 6.0 for rituximab. What this suggests it that better control of inflammation results in a lower risk for hospitalization and death, Dr. Meissner and her associates reported in their poster presentation.
“If patients are not effectively treated for rheumatoid arthritis, there might be other consequences like the deterioration of heart failure or death,” Dr. Meissner said.
She noted that investigators also looked at identifying risk factors for hospitalization or death and found that there was a greater adjusted relative risk if patients were male (RR = 2.4), older (RR = 1.3 per 5-year increase in age), or if they smoked (RR = 1.7). Using higher doses of glucocorticoids also was a risk factor, with a RR of 1.4 for every 5 mg/day increase in dose.
Better physical function was associated with a lower risk of an event (RR = 0.9) and, along with smoking and adjustment of the steroid dose, is a risk factor that could potentially be influenced, Dr. Meissner proposed.
No data on how the heart failure was being managed are available for this cohort and more research is needed.
“There is still not enough known about this topic, and we need the research to determine how to best manage these patients,” Dr. Meissner said. “The time to an event was only 3 years from the time of inclusion in the register, so we need better management of those patients with heart failure as a comorbidity.”
RABBIT is supported by a joint, unconditional grant from AbbVie, Bristol-Myers Squibb, Celltrion, Hexal AG, Lilly, MSD Sharp & Dohme, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Meissner disclosed being on a speakers bureau for Pfizer.
SOURCE: Meissner Y et al. EULAR 2018 Congress. Abstract THU0142 .
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Comorbid heart failure and rheumatoid arthritis carry an unfavorable prognosis, but risk factors have been identified.
Major finding: One-third of patients were hospitalized or died, with a mean time to deterioration or death of 2.5-3 years.
Study details: 393 patients with both heart failure and rheumatoid arthritis enrolled in the German biologics register RABBIT.
Disclosures: RABBIT is supported by a joint, unconditional grant from AbbVie, Bristol-Myers Squibb, Celltrion, Hexal AG, Lilly, MSD Sharp & Dohme, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Meissner disclosed being part of a speakers bureau for Pfizer.
Source: Meissner Y et al. EULAR 2018 Congress, Abstract THU0142.