User login
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
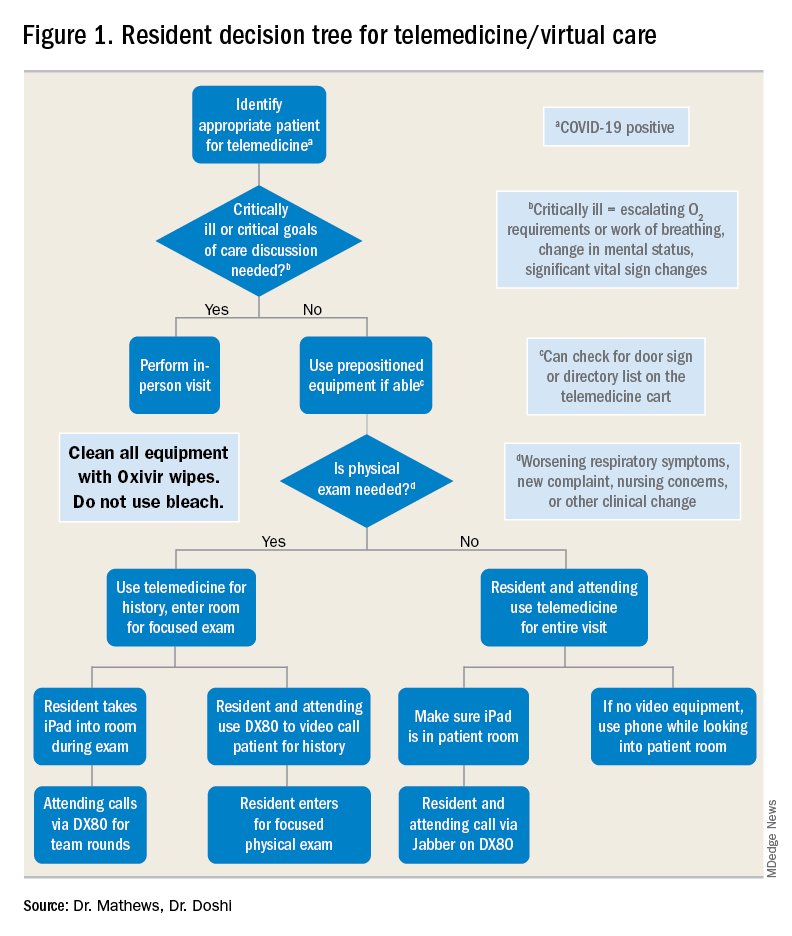
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
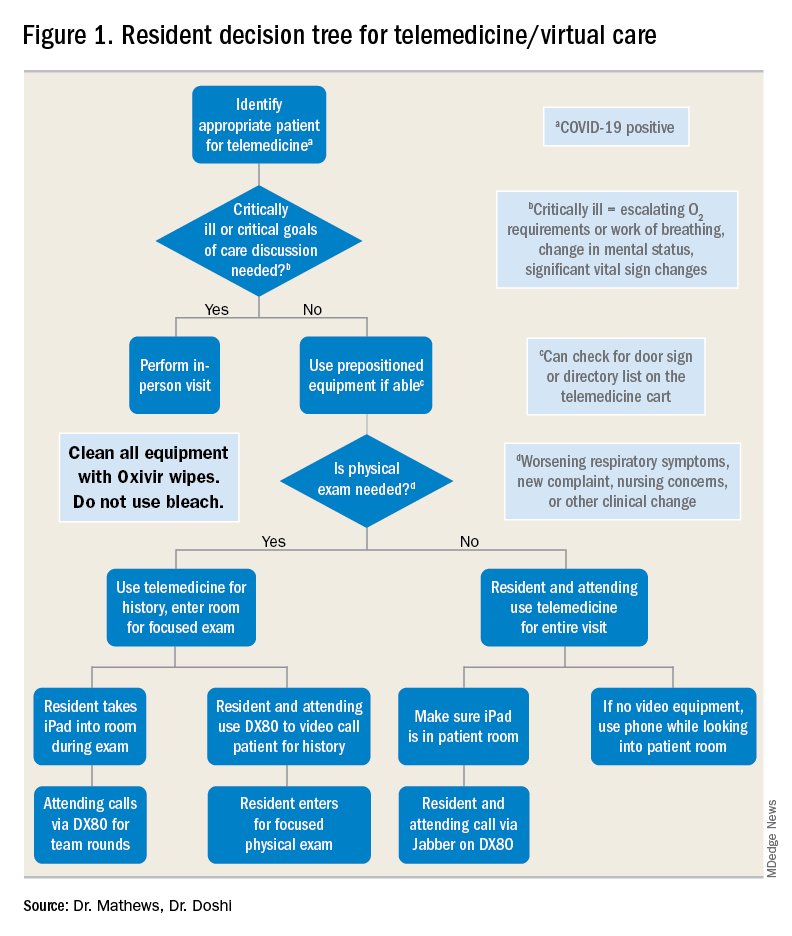
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.
At the start of each shift on his clinical service with rotating internal medicine residents, Benji Mathews, MD, SFHM, now adds a few components to his usual preparation. First, visiting the Minnesota Department of Health and various organizational websites to review the latest COVID-19 updates and guidelines. Next comes checking to see where he needs to pick up the surgical mask and eye protection that he will need to wear through the day. Last, he evaluates which of his patients are in telemedicine-equipped rooms; this last change has fast become a crucial part of working with his resident learners during a pandemic.
During the COVID-19 pandemic, residents and residency programs find themselves in a unique situation. Balancing the educational needs of a training program with the safety of trainees is a challenging task, specifically when taking care of patients who are COVID-19 positive or patients under investigation (PUI). One increasingly available tool that can help protect trainees while continuing to prioritize patient care and medical education is the use of telemedicine for virtual rounding. For our internal medicine residents through the University of Minnesota Internal Medicine Residency program rotating at Regions Hospital in Saint Paul, Minn., we have used video visits to continue our mandate as both health care and education professionals.
Virtual care decision tree
Virtual care can mitigate exposure risk, minimize use of personal protective equipment (PPE), and improve communications with patients and their families. To guide our teaching teams on the optimal situations for telemedicine, we needed to select those patients who would be most appropriate for a virtual visit.
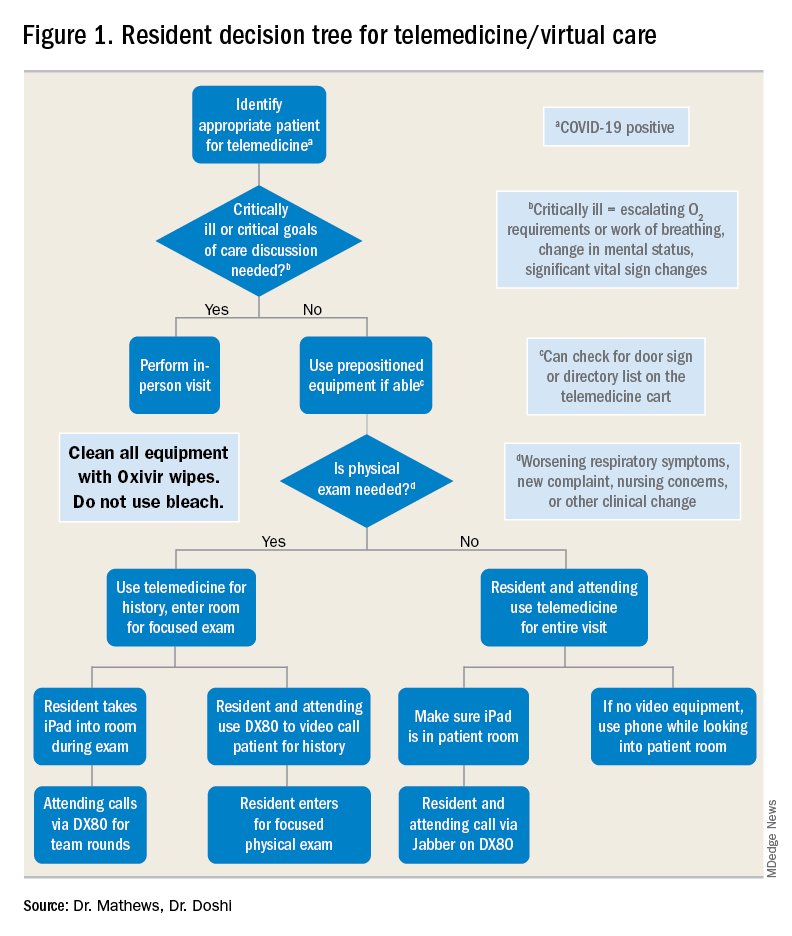
For example, patients with advanced dementia, or intubated in the intensive care unit, would have less utility from a real-time video encounter. Further, we implemented a simple decision tree (Figure 1). First, the team needs to decide whether the patient needs an immediate in-person assessment; for instance, for critically ill patients or those who need end-of-life care discussions, telemedicine would not be an appropriate modality. Next, the decision is made on whether a patient requires an in-person exam at that time. The idea of forgoing the in-person physical exam may run counterintuitive to the core training medical providers undergo, but in certain circumstances telemedicine can still provide the appropriate level of care a patient requires.
Virtual rounding with residents: Pros and cons
Through the course of this pandemic, there have many questions raised regarding how to handle inpatient teaching services: Should resident teams be assigned COVID-19 positives or PUIs? How do you optimize assessing and learning from patients’ conditions that require human touch? Should all members of the teaching team be donning PPE and entering the patient room?
Internal medicine residents in our hospital have been assigned COVID-19 positive and PUI patients. With proper PPE, and donning and doffing practices, residents may continue to learn from this important training opportunity while also optimizing care for patients supplemented by telemedicine. This pandemic has flattened the hierarchy; often residents are teaching their attendings much of the latest literature and best practices around COVID-19. Residents also benefit by joining the organization’s daily virtual interprofessional COVID-19 huddle where they partner with infectious disease, critical care, pharmacy, and other experts to collaborate in the care of these patients.
There have been counterarguments made for residents joining the front lines with COVID-19 patients. Some have conditions that limit them from seeing this subgroup of patients, such as their immune status or other issues. For these residents, we do not assign COVID-19–positive patients. However, they may continue to support in virtually updating COVID-19 patients and their families. A second argument has been the use of PPE. We have implemented telemedicine to limit the total number of exposures and have a protocol for the fewest number of providers possible to see any at-risk or confirmed COVID-19 patient. For example, a resident who sees a COVID-19 patient in person may also be simultaneously virtually supervised by the attending.
Webside manner
The physical exam is only one of several operational considerations when delivering virtual care, whether with a teaching or nonteaching service. One important aspect is the “webside manner” of the provider, the virtual analogue to bedside manner.
Inherent parts of in-person encounters, such as eye contact and allowing for patients to finish their sentences, have added nuances with virtual care. For instance, providers must adjust to looking into the web camera to make eye contact, even though the patient’s face may be on the screen below. Additionally, for patients who are hard of hearing or unfamiliar with video calling, providers must be cognizant of projecting well over an Internet connection and timing responses to avoid overlapping conversation.
Similarly, there are nuances to the virtual physical exam, some specific to care in the COVID-19 era. In our previous virtual care practice, a bedside facilitator assisted in using tools such a digital stethoscope. In contrast, our current practice aims to refine the observational skills of our learners in conjunction with chart review, vital signs, and actively incorporating the patient in the physical exam. This does not mean asking them to auscultate themselves, but is more toward allowing patients to participate in focused evaluations, such as assessing abdominal tenderness or working through range of motion. Remote guidance for virtual exams also extends itself to teaching teams; for example, in our practice, we have been able to conduct bedside ultrasound teaching with in-person team members and a virtual facilitator.
Maskless connections: ‘Face-to-face’ visits with patients
As many hospitalists have witnessed, COVID-19 is so isolating for patients and their families. Patients have limited visitors, and their care team members are aiming to minimize exposures. Those who are entering the rooms wear masks and face shields that limit connecting with patients in a truly “face-to-face” manner. Telemedicine provides a face-to-face encounter that arguably improves upon portions of the traditional in-person encounter during this pandemic, with providers wearing PPE. For medical learners, gaining the interpersonal skills essential for health care professionals has been skewed with pandemic-related limitations; telemedicine can provide a tool to adapt to this unique era and augment this important educational piece.
Limitations, equity, and technological considerations
Realistically, the virtual exam during COVID-19 does have its limitations. An important part of virtual care and teaching services is instilling the appropriate times for use of telemedicine. If a patient has a clinical change (such as increase in FiO2 requirements) or other clinical need, there should be no hesitation for learners to conduct in-person assessments with appropriate PPE.
Nonexam indications are just as important – for example, if a patient requires extensive goals of care counseling, we recommend this not be done virtually. Other indications may vary between organizations; in our practice, we suggest at least one in-person assessment on the initial and discharge hospital days. Regardless of the specific indications, a successful virtual inpatient teaching service must be predicated on outlining the appropriate uses of telemedicine.
In the United States, there are already health care disparities for people of color and non–English speakers. If there is not a careful consideration for these marginalized groups, their health disparities could be further exacerbated – not just around COVID-19, but also for other inpatient conditions where telemedicine is being used. Groups whose equity must be thoughtfully managed include those who do not speak English and those who do not have access to smartphones or the Internet. Our HealthPartners organization has implemented the integration of interpreters for virtual three-way connections with patients and their clinicians to help mitigate this for non–English speakers. Additionally, utilizing easy-to-use tablets and telemedicine-capable carts has helped patients overcome technology barriers.
Last, the members of the teaching team must know the essential technical aspects of the technology they are using. Robust information technology (IT) support is also needed, but no matter how simple the equipment may be, staff and trainees must know how to both operate it and handle basic troubleshooting (such as audio or video disconnections). This also dovetails with the important element of on-boarding other members of the care team. In our practice, nursing staff, chaplains, interpreters, and dietitians also use virtual care as part of their workflow. However, even if it is used only by the teaching team, orienting other care team members will limit technical problems such as equipment being turned off or moved out of position.
Prior to the COVID-19 pandemic, telemedicine adoption was limited because of lack of awareness, barriers in training, understanding, and narrow beliefs regarding the innovation. The COVID-19 pandemic has resulted in a remarkable increase in the provision of telemedicine services in the inpatient hospital medicine services. Importantly, it is, and should be, a developing part of the education and training for health care learners. This pandemic has underscored the need for providing telemedicine services that will likely long outlast this crisis, and to support our health care learners in being effective “iResidents” on our care teams.
Takeaways
- The future of graduate medical education involves virtual care.
The COVID-19 pandemic response has demonstrated that virtual care plays an instrumental part in patient care, and its effects will not dissipate when the pandemic is done. The curriculum for health care trainees should incorporate telemedicine competencies so that they may more effectively leverage this technology for improving care delivery.
- Selection of telemedicine patients must be stratified.
In order to obtain the highest utility for medical learners on telemedicine, there needs to be a clear decision process for which patients can be seen virtually. This involves both clinical criteria, such as avoiding virtual care for end-of-life discussions, and patient criteria, such as those who are hard of hearing.
- Virtual communication requires new communication skills.
Seeing patients via telemedicine mandates a different skill set than in-person communication. Learners must improve their “webside manner” in order to build the patient-provider relationship. Instilling these tools can pay dividends in settings where telemedicine has high yield, such as maskless communication during a pandemic.
- Health disparities could be further exacerbated by telemedicine and should not be overlooked.
Equity in access to health care applies to telemedicine as it does to many other elements. There are multiple groups that can suffer from disparities, such as patients who need interpreters, or those who have lower technological literacy and access to digital devices. Creating awareness of these pitfalls in virtual care can help medical learners recognize and support in creative solutions for these factors.
Dr. Mathews is chief, hospital medicine, at Regions Hospital, HealthPartners, St. Paul, Minn. Dr. Doshi is telemedicine director, hospital medicine, HealthPartners.

