User login
WASHINGTON – Vitamin D deficiency was not only twice as common in women undergoing breast cancer surgery, but it also was associated with poor-prognosis tumors in a case-control study that compared cancer patients with cancer-free women who had been tested for vitamin D.
The breast cancer patients had significantly lower mean vitamin D levels than did controls (33 ng/mL vs. 37 ng/mL), Dr. Kristin A. Skinner reported at the annual meeting of the American Association of Breast Surgeons. Patients were also more than twice as likely to have deficient levels (odds ratio, 2.4; P less than .01), she said.
Analyses presented by Dr. Skinner showed that mean vitamin D levels were significantly lower in the following subgroups of breast cancer patients:
• Those with estrogen receptornegative cancers vs. those with ER-positive cancers (28 ng/mL vs. 33 ng/mL; P = .04).
• Those with triple-negative cancers vs. those with cancers that were not triple negative (26 ng/mL vs.33 ng/mL; P -= .02).
• Those of the basal-like phenotype vs. those of the luminal A phenotype (24 ng/mL vs. 33 ng/mL; P = .04).
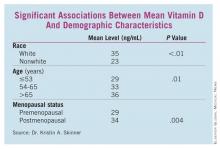
Some patient characteristics also carried significant associations with decreased vitamin D. White women, women aged 65 years and older, and those who were postmenopausal had significantly higher vitamin D levels than did nonwhite, younger, and premenopausal women, respectively. (See box.)
Although vitamin D levels were lower in patients with high Oncotype DX recurrence scores, progesterone receptornegative tumors, and invasive tumors, these differences were not statistically significant. Nor were family history or HER2, tumor, or nodal status significantly related to vitamin D levels, according to Dr. Skinner, a surgical oncologist and breast specialist at the cancer center of the University of Rochester (N.Y.).
In the case-control study, Dr. Skinner and her colleagues selected 194 women who were treated for breast cancer (stage 0-III) at the center and had total 25-hydroxy vitamin D levels drawn in the 3 months before or after their cancer surgery; the mean time of the blood draw was 30 days before surgery.
The patients were matched 1:1 with cancer-free controls who were drawn from a pool of more than 37,000 women who also underwent vitamin D testing in the university’s clinical labs in 2009-2010, the same time the cases were treated. The women were matched for age and the season of testing, since vitamin D levels can change as sun exposure varies.
The researchers divided vitamin D levels into tertiles: Optimal level was considered at least 32 ng/mL, suboptimal was 20-31 ng/mL, and deficient was less than 20 ng/mL.
The findings may argue for vitamin D testing and supplementation either in a primary care setting or in one devoted to breast health, Dr. Skinner said during a press briefing.
"At our institution, we routinely check vitamin D levels and replace them until they are well into the normal range," which is greater than 32 ng/mL, she said. "We really aim for a level of about 50 ng/mL, and titrate their replacement to those levels. In terms of taking supplements, we usually recommend starting at 1,000-2,000 IU daily, but the most effective way is to check levels, and replace accordingly."
Extant epidemiologic data have consistently found a link between more aggressive breast cancers and low vitamin D levels, she said, describing the relationship as biologically plausible. "The vitamin D receptor appears to modulate cell cycles, including the proliferation and differentiation of cells and the activation of apoptosis. Some studies have shown that vitamin D supplementation reduces the risk of breast cancer and improves survival outcomes, but very little is known about vitamin D levels and standard prognostic factors in breast cancer," she said.
"These findings may explain the associations seen in the epidemiologic studies, and may help explain why the black and other nonwhite populations tend to get more-aggressive breast cancer, and get breast cancer at a younger age," Dr. Skinner said.
She had no financial declarations with regard to the work.
WASHINGTON – Vitamin D deficiency was not only twice as common in women undergoing breast cancer surgery, but it also was associated with poor-prognosis tumors in a case-control study that compared cancer patients with cancer-free women who had been tested for vitamin D.
The breast cancer patients had significantly lower mean vitamin D levels than did controls (33 ng/mL vs. 37 ng/mL), Dr. Kristin A. Skinner reported at the annual meeting of the American Association of Breast Surgeons. Patients were also more than twice as likely to have deficient levels (odds ratio, 2.4; P less than .01), she said.
Analyses presented by Dr. Skinner showed that mean vitamin D levels were significantly lower in the following subgroups of breast cancer patients:
• Those with estrogen receptornegative cancers vs. those with ER-positive cancers (28 ng/mL vs. 33 ng/mL; P = .04).
• Those with triple-negative cancers vs. those with cancers that were not triple negative (26 ng/mL vs.33 ng/mL; P -= .02).
• Those of the basal-like phenotype vs. those of the luminal A phenotype (24 ng/mL vs. 33 ng/mL; P = .04).
Some patient characteristics also carried significant associations with decreased vitamin D. White women, women aged 65 years and older, and those who were postmenopausal had significantly higher vitamin D levels than did nonwhite, younger, and premenopausal women, respectively. (See box.)
Although vitamin D levels were lower in patients with high Oncotype DX recurrence scores, progesterone receptornegative tumors, and invasive tumors, these differences were not statistically significant. Nor were family history or HER2, tumor, or nodal status significantly related to vitamin D levels, according to Dr. Skinner, a surgical oncologist and breast specialist at the cancer center of the University of Rochester (N.Y.).
In the case-control study, Dr. Skinner and her colleagues selected 194 women who were treated for breast cancer (stage 0-III) at the center and had total 25-hydroxy vitamin D levels drawn in the 3 months before or after their cancer surgery; the mean time of the blood draw was 30 days before surgery.
The patients were matched 1:1 with cancer-free controls who were drawn from a pool of more than 37,000 women who also underwent vitamin D testing in the university’s clinical labs in 2009-2010, the same time the cases were treated. The women were matched for age and the season of testing, since vitamin D levels can change as sun exposure varies.
The researchers divided vitamin D levels into tertiles: Optimal level was considered at least 32 ng/mL, suboptimal was 20-31 ng/mL, and deficient was less than 20 ng/mL.
The findings may argue for vitamin D testing and supplementation either in a primary care setting or in one devoted to breast health, Dr. Skinner said during a press briefing.
"At our institution, we routinely check vitamin D levels and replace them until they are well into the normal range," which is greater than 32 ng/mL, she said. "We really aim for a level of about 50 ng/mL, and titrate their replacement to those levels. In terms of taking supplements, we usually recommend starting at 1,000-2,000 IU daily, but the most effective way is to check levels, and replace accordingly."
Extant epidemiologic data have consistently found a link between more aggressive breast cancers and low vitamin D levels, she said, describing the relationship as biologically plausible. "The vitamin D receptor appears to modulate cell cycles, including the proliferation and differentiation of cells and the activation of apoptosis. Some studies have shown that vitamin D supplementation reduces the risk of breast cancer and improves survival outcomes, but very little is known about vitamin D levels and standard prognostic factors in breast cancer," she said.
"These findings may explain the associations seen in the epidemiologic studies, and may help explain why the black and other nonwhite populations tend to get more-aggressive breast cancer, and get breast cancer at a younger age," Dr. Skinner said.
She had no financial declarations with regard to the work.
WASHINGTON – Vitamin D deficiency was not only twice as common in women undergoing breast cancer surgery, but it also was associated with poor-prognosis tumors in a case-control study that compared cancer patients with cancer-free women who had been tested for vitamin D.
The breast cancer patients had significantly lower mean vitamin D levels than did controls (33 ng/mL vs. 37 ng/mL), Dr. Kristin A. Skinner reported at the annual meeting of the American Association of Breast Surgeons. Patients were also more than twice as likely to have deficient levels (odds ratio, 2.4; P less than .01), she said.
Analyses presented by Dr. Skinner showed that mean vitamin D levels were significantly lower in the following subgroups of breast cancer patients:
• Those with estrogen receptornegative cancers vs. those with ER-positive cancers (28 ng/mL vs. 33 ng/mL; P = .04).
• Those with triple-negative cancers vs. those with cancers that were not triple negative (26 ng/mL vs.33 ng/mL; P -= .02).
• Those of the basal-like phenotype vs. those of the luminal A phenotype (24 ng/mL vs. 33 ng/mL; P = .04).
Some patient characteristics also carried significant associations with decreased vitamin D. White women, women aged 65 years and older, and those who were postmenopausal had significantly higher vitamin D levels than did nonwhite, younger, and premenopausal women, respectively. (See box.)
Although vitamin D levels were lower in patients with high Oncotype DX recurrence scores, progesterone receptornegative tumors, and invasive tumors, these differences were not statistically significant. Nor were family history or HER2, tumor, or nodal status significantly related to vitamin D levels, according to Dr. Skinner, a surgical oncologist and breast specialist at the cancer center of the University of Rochester (N.Y.).
In the case-control study, Dr. Skinner and her colleagues selected 194 women who were treated for breast cancer (stage 0-III) at the center and had total 25-hydroxy vitamin D levels drawn in the 3 months before or after their cancer surgery; the mean time of the blood draw was 30 days before surgery.
The patients were matched 1:1 with cancer-free controls who were drawn from a pool of more than 37,000 women who also underwent vitamin D testing in the university’s clinical labs in 2009-2010, the same time the cases were treated. The women were matched for age and the season of testing, since vitamin D levels can change as sun exposure varies.
The researchers divided vitamin D levels into tertiles: Optimal level was considered at least 32 ng/mL, suboptimal was 20-31 ng/mL, and deficient was less than 20 ng/mL.
The findings may argue for vitamin D testing and supplementation either in a primary care setting or in one devoted to breast health, Dr. Skinner said during a press briefing.
"At our institution, we routinely check vitamin D levels and replace them until they are well into the normal range," which is greater than 32 ng/mL, she said. "We really aim for a level of about 50 ng/mL, and titrate their replacement to those levels. In terms of taking supplements, we usually recommend starting at 1,000-2,000 IU daily, but the most effective way is to check levels, and replace accordingly."
Extant epidemiologic data have consistently found a link between more aggressive breast cancers and low vitamin D levels, she said, describing the relationship as biologically plausible. "The vitamin D receptor appears to modulate cell cycles, including the proliferation and differentiation of cells and the activation of apoptosis. Some studies have shown that vitamin D supplementation reduces the risk of breast cancer and improves survival outcomes, but very little is known about vitamin D levels and standard prognostic factors in breast cancer," she said.
"These findings may explain the associations seen in the epidemiologic studies, and may help explain why the black and other nonwhite populations tend to get more-aggressive breast cancer, and get breast cancer at a younger age," Dr. Skinner said.
She had no financial declarations with regard to the work.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF BREAST SURGEONS
Finding: Vitamin D deficiency was more than twice as common as normal levels in women undergoing surgery for breast cancer (OR, 2.4).
Data Source: A case-control study of vitamin D levels in 194 women with breast cancer matched 1:1 to a control population.
Disclosures: Dr. Skinner said she had no relevant disclosures.