Prostate cancers that are missed on multiparametric (mp) MRI are small and “not life-threatening,” according to an analysis of data from the Prostate MR Imaging Study (PROMIS).
“Our work suggests that MRI scans of the prostate appear to deliver crucial information about a man’s risk of dying from prostate cancer, even before he has a biopsy,” said Joseph Norris, BM BS, from University College London.
“This may mean that we can finally move prostate cancer to a position in which we can use imaging as the primary tool to direct further investigations, treatment, and prediction of risk,” he told Medscape Medical News.
This is “a position that all other solid organ cancers have reached,” said Norris, who will present the findings at the upcoming virtual European Association of Urology 2020 Congress.
All 576 PROMIS participants underwent an mpMRI scan, a transrectal ultrasonography (TRUS)–guided biopsy, and a template prostate mapping (TPM) biopsy taken at 5-mm intervals across the entire prostate.
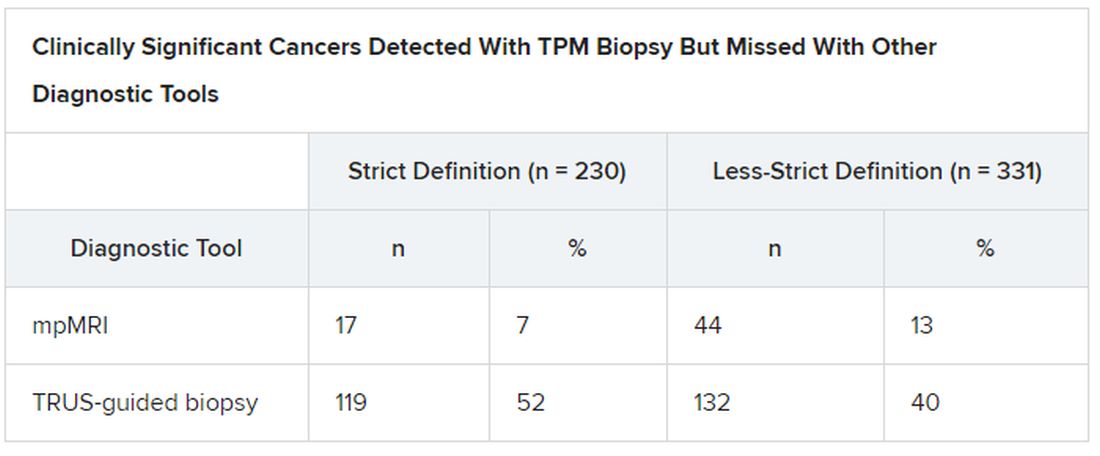
PROMIS researchers previously showed that mpMRI had a 93% sensitivity for clinically significant cancer, whereas TRUS biopsy had only a 48% sensitivity, as reported by Medscape Medical News. And they concluded that the use of mpMRI as a first-line diagnostic tool could prevent 27% of all biopsies, which can have serious adverse effects, such as pain, urinary problems, infection, bleeding, and erectile dysfunction.
However, in their study looking at the accuracy of mpMRI and TRUS biopsy, the researchers did not investigate the severity of the 7% of cancers that mpMRI missed. “What if those missed cancers are, in fact, aggressive? That’s what we set out to examine,” Norris explained.
So he and his colleagues conducted a post ad hoc analysis of the PROMIS participants in whom clinically significant cancer had been detected with TPM biopsy to see which of those cancers had been detected with mpMRI. The findings were published online in European Urology.
Cancers met the strict definition of clinically significant if they had a Gleason score of at least 4+3 for a tumor of any length, or a maximum cancer core length (MCCL) greater than 6 mm for a cancer of any grade. They met the less-strict definition if they had a Gleason score of at least 3+4 for a tumor of any length, or a MCCL greater than 4 mm for a cancer of any grade.
In PROMIS, TPM biopsy detected 230 cancers that met the strict definition of clinically significant and 331 that met the less-strict definition.
Overall Gleason scores were significantly lower for the 17 strict-definition cancers not detected with 1.5 T mpMRI than for those detected with mpMRI (P = .0007), as were maximum Gleason scores (P < .0001).
Median MCCL was 3 mm shorter for all 17 tumors missed with mpMRI than for those detected with mpMRI (5 vs 8 mm; P < .0001).
mpMRI detected all tumors identified on TPM biopsy that had an overall Gleason score greater than 3+4 (Gleason grades 3 to 5) or a maximum Gleason score greater than 4+3 (Gleason grades 4 and 5).
“This finding is important, given that in PROMIS, no men with an overall Gleason score of 4+3 had cancer missed by MRI, indicating that actually MRI may be able to identify all truly significant cancers,” said Norris.
Adding PSA Density Threshold
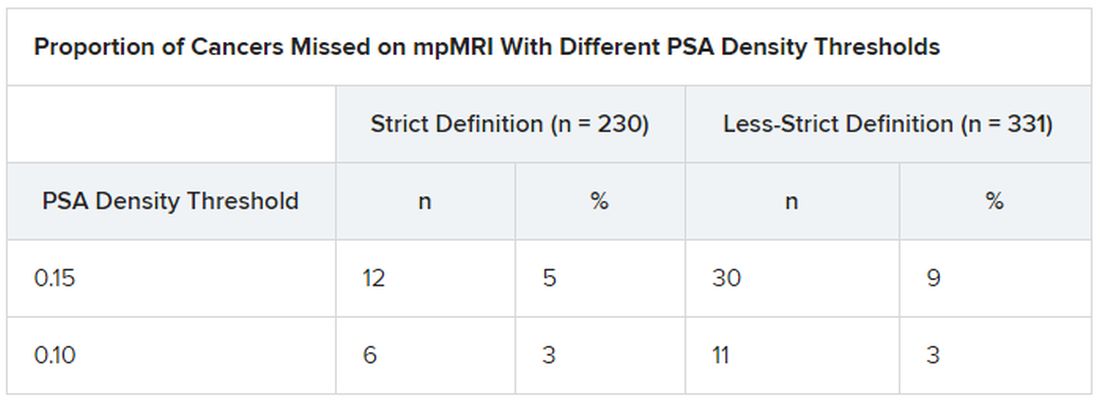
To further assess cancers missed on mpMRI, the researchers looked at prostate-specific antigen (PSA) density, calculated as total PSA level (ng/mL) divided by prostate volume (mL).
“We found that if we applied a threshold PSA density to men with normal-looking MRI scans, we could reduce the proportion of missed significant cancer to just 5%. This is exciting; it means we can make MRI an even more effective test for prostate cancer in a very simple way,” Norris reported.
“These data show that no highly aggressive prostate cancers were missed by MRI, either at the level of the whole prostate or at the individual needle level,” said Norris. This should lead to positive outcomes in the long term.
And since the PROMIS data were gathered, MRI technology has improved, he said. The “MRI scanners in PROMIS were 1.5 Tesla,” whereas today’s machines are 3.0 T, which could increase the detection of significant prostate cancer.
In fact, “our analysis here potentially overestimates the amount of undetected disease,” he noted.
Prostate cancer that is not clinically significant is often monitored with active surveillance, so “invisible” cancers missed on mpMRI could actually be looked at in a positive light, he explained.