User login
The rigid dichotomy between combat deployment and postdeployment environments necessitates a multitude of cognitive, behavioral, and emotional adjustments for National Guard members and reservists to resume postdeployment civilian lifestyles successfully. Reacclimating to the postdeployment world is not a quick process for these veterans because of the time required to adjust from a deeply ingrained military combat mentality to civilian life. The process of this reintegration into the civilian world is known as postdeployment transition.
More than half of post-9/11 combat veterans report at least some difficulty with postdeployment transition.1,2 Frequently encountered symptoms of this period include impaired sleep, low frustration tolerance, decreased attention, poor concentration, short-term memory deficits, and difficulty with emotional regulation.1,3,4 Veterans will have difficulty reintegrating into the family unit and society without successful coping strategies to address these symptoms. If transition symptoms are prolonged, veterans are at risk for developing chronic adjustment difficulty or mental health issues.
Although there is significant attention paid to postdeployment adjustment by military family advocacy groups, there is little information in the medical literature on what constitutes common, nonpathologic postdeployment reactions among combat veterans. Frequently, when postdeployment transition symptoms are discussed, the medical literature tends to explain these in the context of a mental health disorder, such posttraumatic stress disorder (PTSD) or a cognitive injury, such as traumatic brain injury.5-8 Without a balanced understanding of normal postdeployment transitions, a health care provider (HCP) inappropriately may equate transition symptoms with the presence of mental health disorders or cognitive injury and medicalize the coping strategies needed to promote healthy adjustment.
The purpose of this article is to promote HCP awareness of common, nonpathologic postdeployment transition symptoms in combat veterans who are National Guard members or reservists. Such knowledge will enable HCPs to evaluate transition symptoms among these combat veterans reentering the civilian world, normalize common transition reactions, and recognize when further intervention is needed. This article reflects the author’s experience as a medical director working in a VA postdeployment clinic combined with data available in the medical literature and lay press.
Postdeployment Transition Symptoms
Dysregulation of emotional expression in returning combat veterans potentially can be present throughout the postdeployment period of adjustment. Although individual experiences vary widely in intensity and frequency, during postdeployment transition veterans often note difficulty in adjusting emotional expression to match that of nonmilitary counterparts.1,9-11 These difficulties usually fall into 2 broad categories: (1) relative emotional neutrality to major life events that cause nonmilitary civilians great joy or sadness; and (2) overreaction to trivial events, causing significant irritation, anger, or sadness that normally would not produce such emotional reactions in nonmilitary civilians. The former is largely overlooked in medical literature to date except in relation to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) categories, and the latter is often described in limited terms as increased irritability, restlessness, and low frustration tolerance. This emotional dysregulation creates confusing paradoxes for veterans. For example, a veteran might feel no strong emotion when notified of the death of a close relative and yet cry uncontrollably while watching a sad scene in a fictional movie.
Sleep difficulties are intrinsic to the postdeployment period.9-12 Sleep-wake cycles often are altered, reflecting residual effects of the rigid schedules required by military duties and poor sleep hygiene in the combat theater. Inadequate, nonrestful sleep is frequently reported on return to the civilian world. Difficulty falling asleep or difficulty staying asleep also commonly occurs. Nightmares may be present.
Transient difficulty with concentration and attention is often prominent within the postdeployment transition period.9-11,13 Manifestations are variable, but problems with focusing on minor tasks are commonly reported. A more intense effort to master new concepts may be required. Learning styles developed during predeployment phases may be altered so that more conscious effort is required to comprehend and retain new information.
Short-term memory frequently may be affected during postdeployment transition.9-11,13 Veterans often report postdeployment difficulty in recalling appointments or tasks that must be completed even if they had a keen sense of memory during predeployment or deployment. Veterans also may have difficulty recalling the details of specific routines that were done without hesitation during deployment. Compared with predeployment time frames, veterans may exert greater effort to recall newly learned material.
Automatic behaviors necessary for survival in a combat theater still may be prominent in the postdeployment period.10,11,14 Aggressive driving required to avoid deployment ambush may be problematic during the postdeployment transition. Steering clear of any roadside trash may be a residual instinctive drive postdeployment because of the risk of improvised explosive devices concealed by debris in the combat theater. Veterans may avoid sitting with their back to the exit as the result of military safety training. Carrying weapons to ensure safety may be a compelling urge, because being armed and ready at all times was necessary for survival during deployment. Avoiding large crowds may be another strong tendency, because throngs of people were associated with potential danger in the combat theater.
Decision making may be challenging to resume in the postdeployment phase.9-11,15 In the deployment theater, time is relativel structured with rules in place, whereas at home veterans face a myriad of choices and decisions that must be made in order to complete the responsibilities of everyday living. As a result, making decisions about what item to buy, which clothes to wear, or what activities to prioritize, though relatively minor, can be a source of significant frustration. It may be difficult to independently navigate a realm of options available for new employment, schooling, or benefits, especially when there is little or no prior experience with these issues.
Relationship of Symptoms to Mental Health Diagnoses
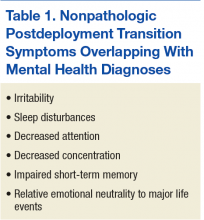
Postdeployment transition symptoms do not automatically indicate the presence of an underlying mental health diagnosis. However, persistent and/or severe symptoms of postdeployment transition can overlap with or contribute to the development of mental health concerns (Table 1).14 The effects of the emotional disconnect also can exacerbate underlying mental health diagnoses.
While postdeployment emotional numbness to major life events, irritability, sleep disturbances, and impaired concentration can be associated with acute stress disorder (ASD) or PTSD, there is a constellation of other symptoms that must be present to diagnose these psychiatric conditions.16 Diagnostic criteria include persistent intrusive symptoms associated with the trauma, persistent avoidance of triggers/reminders associated with the trauma, significant changes in physiologic and cognitive arousal states, and negative changes in mood or cognition related to the trauma.16 The symptoms must cause significant impairment in some aspect of functioning on an individual, social, or occupational level. Acute stress disorder occurs when the symptoms last 30 days or less, whereas PTSD is diagnosed if the symptoms persist longer than a month.
Impaired emotional regulation, sleep disturbances, and decreased concentration also can be associated with depression or anxiety but are insufficient in themselves to make the diagnosis of those disorders.16 At least a 2-week history of depressed mood or inability to experience interest or pleasure in activities must be present as one of the criteria for depression as well as 4 or more other symptoms affecting sleep, appetite, energy, movement, self-esteem, or suicidal thoughts. Anxiety disorders have varying specific diagnostic criteria, but recurrent excessive worrying is a hallmark. Just like ASD or PTSD, the diagnostic symptoms of either depression or anxiety disorders must be causing significant impairment in functioning on an individual, social, or occupational level.
Irritability, sleep disturbances, agitation, memory impairment, and difficulty with concentration and attention can mimic the symptoms associated with mild-to-moderate traumatic brain injury (TBI).17,18 However, symptom onset must have a temporal relationship with a TBI. The presence of other TBI symptoms not associated with normal postdeployment transition usually can be used to differentiate between the diagnoses. Those TBI symptoms include recurrent headaches, poor balance, dizziness, tinnitus, and/or light sensitivity. In the majority of mild TBI cases, the symptoms resolve spontaneously within 3 months of TBI symptom manifestation.16,19 For those with persistent postconcussive syndrome, symptoms usually stabilize or improve over time.18,19 If symptoms worsen, there is often a confounding diagnosis such as PTSD or depression.17,20,21
Some returning combat veterans mistakenly believe postdeployment emotional transition symptoms are always a sign of a mental health disorder. Because there is a significant stigma associated with mental health disorders as well as potential repercussions on their service record if they use mental health resources, many reservists and National Guard members avoid accessing health care services if they are experiencing postdeployment adjustment issues, especially if those symptoms are related to emotional transitions.22-24 Unfortunately, such avoidance carries the risk that stress-inducing symptoms will persist and potentiate adjustment problems.
Course of Symptoms
The range for the postdeployment adjustment period generally falls within 3 to 12 months but can extend longer, depending on individual factors.10,11,25 Factors include presence of significant physical injury or illness, co-occurrence of mental health issues, underlying communication styles, and efficacy of coping strategies chosen. Although there is no clear-cut time frame for transition, ideally transition is complete when the returning veteran successfully enters his or her civilian lifestyle roles and feels a sense of purpose and belonging in society.
Postdeployment transition symptoms occur on a continuum in terms of duration and intensity for reservists and National Guard members. It is difficult to predict how specific transition symptoms will affect a particular veteran. The degree to which those symptoms will complicate reintegration depends on the individual veteran’s ability to adapt within the psychosocial context in which the symptoms occur. For example, minor irritation may be short-lived if a veteran can employ techniques to diffuse that feeling. Alternatively, minor irritation also suddenly may explode into a powerful wave of anger if the veteran has significant underlying emotional tension. Similarly, impaired short-term memory may be limited to forgetting a few appointments or may be so common that the veteran is at risk of losing track of his or her day. The level of memory impairment depends on emotional functioning, co-occurring stressors, and use of adaptive strategies.
In general, as these veterans successfully take on civilian routines, postdeployment transition symptoms will improve. Although such symptom improvement may be a passive process for some veterans, others will need to actively employ strategies to help change the military combat mind-set. The goal is to initiate useful interventions early in transition before symptoms become problematic.14
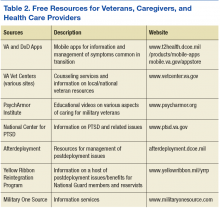
There are numerous self-help techniques and mobile apps that can be applied to a wide number of symptoms. Viable strategies include exercise, yoga, meditation, mindfulness training, and cognitive reframing. Reaching out for early assistance from various military assistance organizations that are well versed in dealing with postdeployment transition challenges often is helpful for reducing stress and navigating postdeployment obstacles (Table 2).
Symptom Strain and Exacerbation
Whenever stumbling blocks are encountered during the postdeployment period, any transition symptom can persist and/or worsen.10,11,14 Emotional disconnect and other transition symptoms can be exacerbated by physical, psychological, and social stressors common in the postdeployment period. Insomnia, poor quality sleep, or other sleep impairments that frequently occur as part of postdeployment transition can negatively impact the veteran’s ability to psychologically cope with daytime stressors. Poor concentration and short-term memory impairment noted by many reservists and National Guard members in the postdeployment phase can cause increased difficulty in attention to the moment and complicate completion of routine tasks. These difficulties can compound frustration and irritation to minor events and make it hard to emotionally connect with more serious issues.
Concentration and attention to mundane activities may be further reduced if the veteran feels no connection to the civilian world and/or experiences the surreal sensation that he or she should be attending to more serious life and death matters, such as those experienced in the combat theater. Ongoing psychological adjustment to physical injuries sustained during deployment can limit emotional flexibility when adapting to either minor or major stressors. Insufficient financial resources, work issues, or school problems can potentiate irritation, anger, and sadness and create an overwhelming emotional overload, leading to helplessness and hopelessness.
Perceived irregularities in emotional connection to the civilian world can significantly strain interpersonal relationships and be powerful impediments to successful reintegration.9,11,14 Failure to express emotions to major life events in the civilian world can result in combat veterans being viewed as not empathetic to others’ feelings. Overreaction to trivial events during postdeployment can lead to the veteran being labeled as unreasonable, controlling, and/or unpredictable. Persistent emotional disconnect with civilians engenders a growing sense of emotional isolation from family and friends when there is either incorrect interpretation of emotional transitions or failure to adapt healthy coping strategies. This isolation further enlarges the emotional chasm and may greatly diminish the veteran’s ability to seek assistance and appropriately address stressors in the civilian world.
Transition and the Family
Emotional disconnection may be more acutely felt within the immediate family unit.26 Redistribution of family unit responsibilities during deployment may mean that roles the veteran played during predeployment now may be handled by a partner. On the veteran’s return to the civilian world, such circumstances require active renegotiation of duties. Interactions with loved ones, especially children, may be colored by the family members’ individual perspectives on deployment as well as by the veteran’s transition symptoms. When there is disagreement about role responsibilities and/or underlying family resentment about deployment, conditions are ripe for significant discord between the veteran and family members, vital loss of partner intimacy, and notable loss of psychological safety to express feelings within the family unit. If there are concerns about infidelity by the veteran or significant other during the period of deployment, postdeployment tensions can further escalate. If unaddressed in the presence of emotional disconnect, any of these situations can raise the risk of domestic violence and destruction of relationships.
Without adequate knowledge of common postdeployment transitions and coping strategies, the postdeployment transition period is often bewildering to returning veterans and their families. They are taken aback by postdeployment behaviors that do not conform to the veteran’s predeployment personality or mannerisms. Families may feel they have “lost” the veteran and view the emotionally distant postdeployment veteran as a stranger. Veterans mistakenly may view the postdeployment emotional disconnect as evidence that they were permanently altered by deployment and no longer can assimilate into the civilian world. Unless veterans and families develop an awareness of the postdeployment transition symptoms and healthy coping strategies, these perspectives can contribute to a veteran’s persistent feelings of alienation, significant sense of personal failure, and loss of vital social supports.
When transition symptoms are or have the potential to become significant stressors, veterans would benefit from mental health counseling either individually or with family members. Overcoming the stigma of seeking mental health services can prove challenging. Explaining that these postdeployment symptoms occur commonly, stem from military combat training, can be reversed, and when reversed will empower the individual to control his or her life may help veterans overcome the stigma and seek mental health services.
The fear of future career impairment with the military reserve or National Guard is another real concern among this cohort who might consider accessing behavioral health care, especially since VA mental health medical records can be accessed by DoD officials through links with the VHA. Fortunately, this concern can be alleviated through the use of Vet Centers, free-standing counseling centers nationwide that offer no-cost individual and family counseling to veterans with combat exposure. Vet Center counseling records are completely confidential, never shared, and are not linked to the VHA electronic health record, the DoD, or any other entity. Although Vet Center providers don’t prescribe medications, the counselors can actively address many issues for veterans and their families. For individuals who do not live near a Vet Center or for those who require psychiatric medications, a frank discussion on the benefits of treatment vs the risk of treatment avoidance must be held.
Assessing Symptoms and Coping Mechanisms
Postdeployment transition symptoms vary, depending on the nature and context of the symptom. Not only must the returning reservist and National Guard member be screened for symptoms, but HCPs also should assess the impact of those symptoms on the veteran and his or her interpersonal relationships. Some veterans will feel that the symptoms have relatively minor impact in their lives, because the veteran can easily compensate for the transient effects. Others may feel that the symptoms are somewhat burdensome because the issues are complicating the smooth transition to civilian roles. Still others will judge the symptoms to be devastating because of the negative effects on personal control, selfesteem, and emotional connection with family and friends.
In addition to screening for symptoms, HCPs should assess these veterans’ current coping adaptations to various transition symptoms. Whereas some activities may be functional and promote reintegration, other short-term coping solutions may cripple the veteran’s ability to successfully resume civilian life. Global avoidance of communication with others and/or retreating from all social situations is a destructive coping pattern that can further alienate veterans from their families and the civilian world. Reacting with anger to all stressful issues is another maladaptive pattern of coping with life’s frustrations. Because of the potential to self-medicate when dealing with social difficulties, depression, anxiety, or other mental health diagnoses, veterans may develop an inappropriate reliance on drugs or alcohol to handle postdeployment stressors.27 Therefore, HCP screening for substance use disorders (SUD) is important so that interventions can be initiated early.
Because of the overlap of postdeployment transition symptoms with mental health disorders and the relative frequency of those mental health disorders among combat veterans, HCPs should have a heightened awareness of the potential for co-occurring mental health difficulties in the postdeployment reservist and National Guard cohort. Health care providers should screen for depression, anxiety, and PTSD. Even if initial screening is done early within the transition period, repeat screening would be of benefit 6 months into the postdeployment period because of the tendency of mental health issues to develop during that time.28,29
By evaluating the impact of the transition symptom and coping strategies on these veterans’ lives, HCPs can better determine which strategies might adequately compensate for symptom effects. In general, informal counseling, even if just to help veterans normalize postdeployment transition symptoms and develop a plan to address such symptoms, can significantly minimize the negative impact of transition symptoms.14,26 Specific symptoms should be targeted by interventions that match the degree of symptom impact.
Symptoms to be aggressively addressed are those that significantly interfere with successful reintegration into the civilian world. For example, persistent sleep difficulties should be dealt with because they can worsen all other transition symptoms. However, the majority of strategies to address sleep do not require medication unless there are confounding factors such as severe nightmares. Minor memory issues attributed to the transition phase can be mitigated by several strategies to improve recall, including use of task lists, digital calendars, or other memory-prodding techniques. However, severe memory issues related to depression or anxiety likely would require pharmaceutical assistance and formal counseling in addition to other nonpharmacologic approaches.
Intermittent irritation or restlessness may be amenable to selfhelp strategies, but significant anger outbursts or aggression will require additional support, such as formal behavioral interventions to help identify the triggers and develop strategic plans to reduce emotional tension. A mild sense of not belonging may resolve without intervention, but a stronger sense of alienation will require further evaluation.
Conclusion
Civilian reintegration after combat deployment is a gradual process rather than a discrete event for reservists and National Guard members. There are common, nonpathologic postdeployment transition symptoms that, if misunderstood or inappropriately addressed, can complicate civilian reintegration. Health care providers are in the unique position to promote a healthy postdeployment transition by assisting veterans to recognize nonpathologic transition symptoms, select appropriate coping strategies, and seek further assistance for more complex problems.
1. Pew Research Center. War and sacrifice in the post 9/11 era: executive summary. http://www
.pewsocialtrends.org/2011/10/05/war-and-sacrifice-in-the-post-911-era. Published October 5, 2011. Accessed June 12, 2017.
2. Interian A, Kline A, Callahan L, Losonczy M. Readjustment stressors and early mental health treatment seeking by returning National Guard soldiers with PTSD. Psychiatr Serv. 2012;63(9):855-861.
3. Spelman JF, Hunt SC, Seal KH, Burgo-Black AL. Post deployment care for returning combat veterans. J Gen Intern Med. 2012;27(9):1200-1209.
4. Vasterling JJ, Daily ES, Friedman MJ. Posttraumatic stress reactions over time: the battlefield, homecoming, and long-term course. In: Ruzek JI, Schnurr PP, Vasterling JJ, Friedman MJ, eds. Caring for Veterans With Deployment-Related Stress Disorders: Iraq, Afghanistan, and Beyond. Washington,DC: American Psychological Association;2011:chap 2.
5. Wilcox SL, Oh H, Redmon SA, Chicas J, Hassan AM, Lee PJ, Ell K. A scope of the problem: Postdeployment reintegration challenges in a National Guard Unit. Work. 2015;50(1):73-83.
6. Griffith J. Homecoming of citizen soldiers: Postdeployment problems and service use among Army National Guard soldiers. Community Ment Health J. 2017. doi:10.1007/s10597-017-0132-9. (Epub ahead of print)
7. Schultz M, Glickman ME, Eisen SV. Predictors of decline in overall mental health, PTSD and alcohol use in OEF/OIF veterans. Comprehensive Psychiatry. 2014;55(7):1654-1664.
8. Polusny MA, Kehle SM, Nelson NW, Erbes CR, Arbisi PA, Thuras P. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in National Guard soldiers deployed to Iraq. Arch Gen Psychiatry. 2011:68(1):79-89.
9. U.S. Department of Veterans Affairs, National Center for PTSD. Returning from the war zone: a guide for military personnel. http://www.ptsd.va.gov/public/reintegration/guide-pdf/SMGuide.pdf. Updated January 2014. Accessed June 12, 2017.
10. Slone LB, Friedman MJ. After the War Zone: A Practical Guide for Returning Troops and their Families. Philadelphia, PA: Da Capo Press; 2008.
11. Ainspan ND, Penk WE, eds. When the Warrior Returns: Making the Transition at Home. Annapolis, MD: Naval Institute Press; 2012.
12. Yosick T, Bates M, Moore M, Crowe C, Phillips J, Davison J. A review of post-deployment reintegration: evidence, challenges, and strategies for program development. http://www.dcoe.mil/files/Review_of_Post-Deployment_Reintegration.pdf. Published February 10, 2012. Accessed June 12, 2017.
13. Vasterling JJ, Proctor SP, Amoroso P, Kane R, Heeren T, White RF. Neuropsychological outcomes of army personnel following deployment to the Iraq war. JAMA. 2006;296(5):519-529.
14. Castro CA, Kintzle S, Hassan AM. The combat veteran paradox: paradoxes and dilemmas encountered with reintegrating combat veterans and the agencies that support them. Traumatology. 2015;21(4):299-310.
15. Rivers FM, Gordon S, Speraw S, Reese S. U.S. Army nurses’ reintegration and homecoming experiences after Iraq and Afghanistan. Mil Med. 2013;178(2):166-173.
16. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington,VA: American Psychiatric Association;2013.
17. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: Rand Corporation, 2008.
18. Orff HJ, Hays CC, Heldreth AA, Stein MB, Twamley EW. Clinical considerations in the evaluation and management of patients following traumatic brain injury. Focus. 2013;11(3):328-340.
19. Morissette SB, Woodward M, Kimbrel NA, et al. Deployment-related TBI, persistent postconcussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabil Psychol. 2011;56(4):340-350.
20. Polusny MA, Kehle SM, Nelson NW, Erbes CR, Arbisi PA, Thuras P. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in national guard soldiers deployed to Iraq. Arch Gen Psychiatry. 2011;68(1):79-89.
21. Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosom Med. 2012;74(3):249-257.
22. Hoge CW, Grossman SH, Auchterlonie JL, Riviere LA, Milliken CS, Wilk JE. PTSD treatment for soldiers after combat deployment: low utilization of mental health care and reasons for dropout. Psychiatr Serv. 2014;65(8):997-1004.
23. Hines LA, Goodwin L, Jones M, et al. Factors affecting help seeking for mental health problems after deployment to Iraq and Afghanistan. Psychiatr Serv. 2014;65(1):98-105.
24. Gorman LA, Blow AJ, Ames BD, Read PL. National Guard families after combat: mental health, use of mental health services, and perceived treatment barriers. Psychiatr Serv. 2011;62(1):28-34.
25. Marek LI, Hollingsworth WG, D’Aniello C, et al. Returning home: what we know about the reintegration of deployed service members into their families and communities. https://www.ncfr.org/ncfr-report/focus/military-families/returninghome. Published March 1, 2012. Accessed June 13, 2017.
26. Bowling UB, Sherman MD. Welcoming them home: supporting service members and their families in navigating the tasks of reintegration. Prof Psychol Res Pr. 2008;39(4):451-458.
27. Jacobson IG, Ryan MA, Hooper TI, et al. Alcohol use and alcohol-related problems before
and after military combat deployment. JAMA. 2008;300(6):663-675.
28. Seal KH, Metzler TH, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans Department of Veterans Affairs health care, 2002-2008. Am J Public Health. 2009;99(9):1651-1658.
29. Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298(18):2141-2148.
The rigid dichotomy between combat deployment and postdeployment environments necessitates a multitude of cognitive, behavioral, and emotional adjustments for National Guard members and reservists to resume postdeployment civilian lifestyles successfully. Reacclimating to the postdeployment world is not a quick process for these veterans because of the time required to adjust from a deeply ingrained military combat mentality to civilian life. The process of this reintegration into the civilian world is known as postdeployment transition.
More than half of post-9/11 combat veterans report at least some difficulty with postdeployment transition.1,2 Frequently encountered symptoms of this period include impaired sleep, low frustration tolerance, decreased attention, poor concentration, short-term memory deficits, and difficulty with emotional regulation.1,3,4 Veterans will have difficulty reintegrating into the family unit and society without successful coping strategies to address these symptoms. If transition symptoms are prolonged, veterans are at risk for developing chronic adjustment difficulty or mental health issues.
Although there is significant attention paid to postdeployment adjustment by military family advocacy groups, there is little information in the medical literature on what constitutes common, nonpathologic postdeployment reactions among combat veterans. Frequently, when postdeployment transition symptoms are discussed, the medical literature tends to explain these in the context of a mental health disorder, such posttraumatic stress disorder (PTSD) or a cognitive injury, such as traumatic brain injury.5-8 Without a balanced understanding of normal postdeployment transitions, a health care provider (HCP) inappropriately may equate transition symptoms with the presence of mental health disorders or cognitive injury and medicalize the coping strategies needed to promote healthy adjustment.
The purpose of this article is to promote HCP awareness of common, nonpathologic postdeployment transition symptoms in combat veterans who are National Guard members or reservists. Such knowledge will enable HCPs to evaluate transition symptoms among these combat veterans reentering the civilian world, normalize common transition reactions, and recognize when further intervention is needed. This article reflects the author’s experience as a medical director working in a VA postdeployment clinic combined with data available in the medical literature and lay press.
Postdeployment Transition Symptoms
Dysregulation of emotional expression in returning combat veterans potentially can be present throughout the postdeployment period of adjustment. Although individual experiences vary widely in intensity and frequency, during postdeployment transition veterans often note difficulty in adjusting emotional expression to match that of nonmilitary counterparts.1,9-11 These difficulties usually fall into 2 broad categories: (1) relative emotional neutrality to major life events that cause nonmilitary civilians great joy or sadness; and (2) overreaction to trivial events, causing significant irritation, anger, or sadness that normally would not produce such emotional reactions in nonmilitary civilians. The former is largely overlooked in medical literature to date except in relation to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) categories, and the latter is often described in limited terms as increased irritability, restlessness, and low frustration tolerance. This emotional dysregulation creates confusing paradoxes for veterans. For example, a veteran might feel no strong emotion when notified of the death of a close relative and yet cry uncontrollably while watching a sad scene in a fictional movie.
Sleep difficulties are intrinsic to the postdeployment period.9-12 Sleep-wake cycles often are altered, reflecting residual effects of the rigid schedules required by military duties and poor sleep hygiene in the combat theater. Inadequate, nonrestful sleep is frequently reported on return to the civilian world. Difficulty falling asleep or difficulty staying asleep also commonly occurs. Nightmares may be present.
Transient difficulty with concentration and attention is often prominent within the postdeployment transition period.9-11,13 Manifestations are variable, but problems with focusing on minor tasks are commonly reported. A more intense effort to master new concepts may be required. Learning styles developed during predeployment phases may be altered so that more conscious effort is required to comprehend and retain new information.
Short-term memory frequently may be affected during postdeployment transition.9-11,13 Veterans often report postdeployment difficulty in recalling appointments or tasks that must be completed even if they had a keen sense of memory during predeployment or deployment. Veterans also may have difficulty recalling the details of specific routines that were done without hesitation during deployment. Compared with predeployment time frames, veterans may exert greater effort to recall newly learned material.
Automatic behaviors necessary for survival in a combat theater still may be prominent in the postdeployment period.10,11,14 Aggressive driving required to avoid deployment ambush may be problematic during the postdeployment transition. Steering clear of any roadside trash may be a residual instinctive drive postdeployment because of the risk of improvised explosive devices concealed by debris in the combat theater. Veterans may avoid sitting with their back to the exit as the result of military safety training. Carrying weapons to ensure safety may be a compelling urge, because being armed and ready at all times was necessary for survival during deployment. Avoiding large crowds may be another strong tendency, because throngs of people were associated with potential danger in the combat theater.
Decision making may be challenging to resume in the postdeployment phase.9-11,15 In the deployment theater, time is relativel structured with rules in place, whereas at home veterans face a myriad of choices and decisions that must be made in order to complete the responsibilities of everyday living. As a result, making decisions about what item to buy, which clothes to wear, or what activities to prioritize, though relatively minor, can be a source of significant frustration. It may be difficult to independently navigate a realm of options available for new employment, schooling, or benefits, especially when there is little or no prior experience with these issues.
Relationship of Symptoms to Mental Health Diagnoses
Postdeployment transition symptoms do not automatically indicate the presence of an underlying mental health diagnosis. However, persistent and/or severe symptoms of postdeployment transition can overlap with or contribute to the development of mental health concerns (Table 1).14 The effects of the emotional disconnect also can exacerbate underlying mental health diagnoses.
While postdeployment emotional numbness to major life events, irritability, sleep disturbances, and impaired concentration can be associated with acute stress disorder (ASD) or PTSD, there is a constellation of other symptoms that must be present to diagnose these psychiatric conditions.16 Diagnostic criteria include persistent intrusive symptoms associated with the trauma, persistent avoidance of triggers/reminders associated with the trauma, significant changes in physiologic and cognitive arousal states, and negative changes in mood or cognition related to the trauma.16 The symptoms must cause significant impairment in some aspect of functioning on an individual, social, or occupational level. Acute stress disorder occurs when the symptoms last 30 days or less, whereas PTSD is diagnosed if the symptoms persist longer than a month.
Impaired emotional regulation, sleep disturbances, and decreased concentration also can be associated with depression or anxiety but are insufficient in themselves to make the diagnosis of those disorders.16 At least a 2-week history of depressed mood or inability to experience interest or pleasure in activities must be present as one of the criteria for depression as well as 4 or more other symptoms affecting sleep, appetite, energy, movement, self-esteem, or suicidal thoughts. Anxiety disorders have varying specific diagnostic criteria, but recurrent excessive worrying is a hallmark. Just like ASD or PTSD, the diagnostic symptoms of either depression or anxiety disorders must be causing significant impairment in functioning on an individual, social, or occupational level.
Irritability, sleep disturbances, agitation, memory impairment, and difficulty with concentration and attention can mimic the symptoms associated with mild-to-moderate traumatic brain injury (TBI).17,18 However, symptom onset must have a temporal relationship with a TBI. The presence of other TBI symptoms not associated with normal postdeployment transition usually can be used to differentiate between the diagnoses. Those TBI symptoms include recurrent headaches, poor balance, dizziness, tinnitus, and/or light sensitivity. In the majority of mild TBI cases, the symptoms resolve spontaneously within 3 months of TBI symptom manifestation.16,19 For those with persistent postconcussive syndrome, symptoms usually stabilize or improve over time.18,19 If symptoms worsen, there is often a confounding diagnosis such as PTSD or depression.17,20,21
Some returning combat veterans mistakenly believe postdeployment emotional transition symptoms are always a sign of a mental health disorder. Because there is a significant stigma associated with mental health disorders as well as potential repercussions on their service record if they use mental health resources, many reservists and National Guard members avoid accessing health care services if they are experiencing postdeployment adjustment issues, especially if those symptoms are related to emotional transitions.22-24 Unfortunately, such avoidance carries the risk that stress-inducing symptoms will persist and potentiate adjustment problems.
Course of Symptoms
The range for the postdeployment adjustment period generally falls within 3 to 12 months but can extend longer, depending on individual factors.10,11,25 Factors include presence of significant physical injury or illness, co-occurrence of mental health issues, underlying communication styles, and efficacy of coping strategies chosen. Although there is no clear-cut time frame for transition, ideally transition is complete when the returning veteran successfully enters his or her civilian lifestyle roles and feels a sense of purpose and belonging in society.
Postdeployment transition symptoms occur on a continuum in terms of duration and intensity for reservists and National Guard members. It is difficult to predict how specific transition symptoms will affect a particular veteran. The degree to which those symptoms will complicate reintegration depends on the individual veteran’s ability to adapt within the psychosocial context in which the symptoms occur. For example, minor irritation may be short-lived if a veteran can employ techniques to diffuse that feeling. Alternatively, minor irritation also suddenly may explode into a powerful wave of anger if the veteran has significant underlying emotional tension. Similarly, impaired short-term memory may be limited to forgetting a few appointments or may be so common that the veteran is at risk of losing track of his or her day. The level of memory impairment depends on emotional functioning, co-occurring stressors, and use of adaptive strategies.
In general, as these veterans successfully take on civilian routines, postdeployment transition symptoms will improve. Although such symptom improvement may be a passive process for some veterans, others will need to actively employ strategies to help change the military combat mind-set. The goal is to initiate useful interventions early in transition before symptoms become problematic.14
There are numerous self-help techniques and mobile apps that can be applied to a wide number of symptoms. Viable strategies include exercise, yoga, meditation, mindfulness training, and cognitive reframing. Reaching out for early assistance from various military assistance organizations that are well versed in dealing with postdeployment transition challenges often is helpful for reducing stress and navigating postdeployment obstacles (Table 2).
Symptom Strain and Exacerbation
Whenever stumbling blocks are encountered during the postdeployment period, any transition symptom can persist and/or worsen.10,11,14 Emotional disconnect and other transition symptoms can be exacerbated by physical, psychological, and social stressors common in the postdeployment period. Insomnia, poor quality sleep, or other sleep impairments that frequently occur as part of postdeployment transition can negatively impact the veteran’s ability to psychologically cope with daytime stressors. Poor concentration and short-term memory impairment noted by many reservists and National Guard members in the postdeployment phase can cause increased difficulty in attention to the moment and complicate completion of routine tasks. These difficulties can compound frustration and irritation to minor events and make it hard to emotionally connect with more serious issues.
Concentration and attention to mundane activities may be further reduced if the veteran feels no connection to the civilian world and/or experiences the surreal sensation that he or she should be attending to more serious life and death matters, such as those experienced in the combat theater. Ongoing psychological adjustment to physical injuries sustained during deployment can limit emotional flexibility when adapting to either minor or major stressors. Insufficient financial resources, work issues, or school problems can potentiate irritation, anger, and sadness and create an overwhelming emotional overload, leading to helplessness and hopelessness.
Perceived irregularities in emotional connection to the civilian world can significantly strain interpersonal relationships and be powerful impediments to successful reintegration.9,11,14 Failure to express emotions to major life events in the civilian world can result in combat veterans being viewed as not empathetic to others’ feelings. Overreaction to trivial events during postdeployment can lead to the veteran being labeled as unreasonable, controlling, and/or unpredictable. Persistent emotional disconnect with civilians engenders a growing sense of emotional isolation from family and friends when there is either incorrect interpretation of emotional transitions or failure to adapt healthy coping strategies. This isolation further enlarges the emotional chasm and may greatly diminish the veteran’s ability to seek assistance and appropriately address stressors in the civilian world.
Transition and the Family
Emotional disconnection may be more acutely felt within the immediate family unit.26 Redistribution of family unit responsibilities during deployment may mean that roles the veteran played during predeployment now may be handled by a partner. On the veteran’s return to the civilian world, such circumstances require active renegotiation of duties. Interactions with loved ones, especially children, may be colored by the family members’ individual perspectives on deployment as well as by the veteran’s transition symptoms. When there is disagreement about role responsibilities and/or underlying family resentment about deployment, conditions are ripe for significant discord between the veteran and family members, vital loss of partner intimacy, and notable loss of psychological safety to express feelings within the family unit. If there are concerns about infidelity by the veteran or significant other during the period of deployment, postdeployment tensions can further escalate. If unaddressed in the presence of emotional disconnect, any of these situations can raise the risk of domestic violence and destruction of relationships.
Without adequate knowledge of common postdeployment transitions and coping strategies, the postdeployment transition period is often bewildering to returning veterans and their families. They are taken aback by postdeployment behaviors that do not conform to the veteran’s predeployment personality or mannerisms. Families may feel they have “lost” the veteran and view the emotionally distant postdeployment veteran as a stranger. Veterans mistakenly may view the postdeployment emotional disconnect as evidence that they were permanently altered by deployment and no longer can assimilate into the civilian world. Unless veterans and families develop an awareness of the postdeployment transition symptoms and healthy coping strategies, these perspectives can contribute to a veteran’s persistent feelings of alienation, significant sense of personal failure, and loss of vital social supports.
When transition symptoms are or have the potential to become significant stressors, veterans would benefit from mental health counseling either individually or with family members. Overcoming the stigma of seeking mental health services can prove challenging. Explaining that these postdeployment symptoms occur commonly, stem from military combat training, can be reversed, and when reversed will empower the individual to control his or her life may help veterans overcome the stigma and seek mental health services.
The fear of future career impairment with the military reserve or National Guard is another real concern among this cohort who might consider accessing behavioral health care, especially since VA mental health medical records can be accessed by DoD officials through links with the VHA. Fortunately, this concern can be alleviated through the use of Vet Centers, free-standing counseling centers nationwide that offer no-cost individual and family counseling to veterans with combat exposure. Vet Center counseling records are completely confidential, never shared, and are not linked to the VHA electronic health record, the DoD, or any other entity. Although Vet Center providers don’t prescribe medications, the counselors can actively address many issues for veterans and their families. For individuals who do not live near a Vet Center or for those who require psychiatric medications, a frank discussion on the benefits of treatment vs the risk of treatment avoidance must be held.
Assessing Symptoms and Coping Mechanisms
Postdeployment transition symptoms vary, depending on the nature and context of the symptom. Not only must the returning reservist and National Guard member be screened for symptoms, but HCPs also should assess the impact of those symptoms on the veteran and his or her interpersonal relationships. Some veterans will feel that the symptoms have relatively minor impact in their lives, because the veteran can easily compensate for the transient effects. Others may feel that the symptoms are somewhat burdensome because the issues are complicating the smooth transition to civilian roles. Still others will judge the symptoms to be devastating because of the negative effects on personal control, selfesteem, and emotional connection with family and friends.
In addition to screening for symptoms, HCPs should assess these veterans’ current coping adaptations to various transition symptoms. Whereas some activities may be functional and promote reintegration, other short-term coping solutions may cripple the veteran’s ability to successfully resume civilian life. Global avoidance of communication with others and/or retreating from all social situations is a destructive coping pattern that can further alienate veterans from their families and the civilian world. Reacting with anger to all stressful issues is another maladaptive pattern of coping with life’s frustrations. Because of the potential to self-medicate when dealing with social difficulties, depression, anxiety, or other mental health diagnoses, veterans may develop an inappropriate reliance on drugs or alcohol to handle postdeployment stressors.27 Therefore, HCP screening for substance use disorders (SUD) is important so that interventions can be initiated early.
Because of the overlap of postdeployment transition symptoms with mental health disorders and the relative frequency of those mental health disorders among combat veterans, HCPs should have a heightened awareness of the potential for co-occurring mental health difficulties in the postdeployment reservist and National Guard cohort. Health care providers should screen for depression, anxiety, and PTSD. Even if initial screening is done early within the transition period, repeat screening would be of benefit 6 months into the postdeployment period because of the tendency of mental health issues to develop during that time.28,29
By evaluating the impact of the transition symptom and coping strategies on these veterans’ lives, HCPs can better determine which strategies might adequately compensate for symptom effects. In general, informal counseling, even if just to help veterans normalize postdeployment transition symptoms and develop a plan to address such symptoms, can significantly minimize the negative impact of transition symptoms.14,26 Specific symptoms should be targeted by interventions that match the degree of symptom impact.
Symptoms to be aggressively addressed are those that significantly interfere with successful reintegration into the civilian world. For example, persistent sleep difficulties should be dealt with because they can worsen all other transition symptoms. However, the majority of strategies to address sleep do not require medication unless there are confounding factors such as severe nightmares. Minor memory issues attributed to the transition phase can be mitigated by several strategies to improve recall, including use of task lists, digital calendars, or other memory-prodding techniques. However, severe memory issues related to depression or anxiety likely would require pharmaceutical assistance and formal counseling in addition to other nonpharmacologic approaches.
Intermittent irritation or restlessness may be amenable to selfhelp strategies, but significant anger outbursts or aggression will require additional support, such as formal behavioral interventions to help identify the triggers and develop strategic plans to reduce emotional tension. A mild sense of not belonging may resolve without intervention, but a stronger sense of alienation will require further evaluation.
Conclusion
Civilian reintegration after combat deployment is a gradual process rather than a discrete event for reservists and National Guard members. There are common, nonpathologic postdeployment transition symptoms that, if misunderstood or inappropriately addressed, can complicate civilian reintegration. Health care providers are in the unique position to promote a healthy postdeployment transition by assisting veterans to recognize nonpathologic transition symptoms, select appropriate coping strategies, and seek further assistance for more complex problems.
The rigid dichotomy between combat deployment and postdeployment environments necessitates a multitude of cognitive, behavioral, and emotional adjustments for National Guard members and reservists to resume postdeployment civilian lifestyles successfully. Reacclimating to the postdeployment world is not a quick process for these veterans because of the time required to adjust from a deeply ingrained military combat mentality to civilian life. The process of this reintegration into the civilian world is known as postdeployment transition.
More than half of post-9/11 combat veterans report at least some difficulty with postdeployment transition.1,2 Frequently encountered symptoms of this period include impaired sleep, low frustration tolerance, decreased attention, poor concentration, short-term memory deficits, and difficulty with emotional regulation.1,3,4 Veterans will have difficulty reintegrating into the family unit and society without successful coping strategies to address these symptoms. If transition symptoms are prolonged, veterans are at risk for developing chronic adjustment difficulty or mental health issues.
Although there is significant attention paid to postdeployment adjustment by military family advocacy groups, there is little information in the medical literature on what constitutes common, nonpathologic postdeployment reactions among combat veterans. Frequently, when postdeployment transition symptoms are discussed, the medical literature tends to explain these in the context of a mental health disorder, such posttraumatic stress disorder (PTSD) or a cognitive injury, such as traumatic brain injury.5-8 Without a balanced understanding of normal postdeployment transitions, a health care provider (HCP) inappropriately may equate transition symptoms with the presence of mental health disorders or cognitive injury and medicalize the coping strategies needed to promote healthy adjustment.
The purpose of this article is to promote HCP awareness of common, nonpathologic postdeployment transition symptoms in combat veterans who are National Guard members or reservists. Such knowledge will enable HCPs to evaluate transition symptoms among these combat veterans reentering the civilian world, normalize common transition reactions, and recognize when further intervention is needed. This article reflects the author’s experience as a medical director working in a VA postdeployment clinic combined with data available in the medical literature and lay press.
Postdeployment Transition Symptoms
Dysregulation of emotional expression in returning combat veterans potentially can be present throughout the postdeployment period of adjustment. Although individual experiences vary widely in intensity and frequency, during postdeployment transition veterans often note difficulty in adjusting emotional expression to match that of nonmilitary counterparts.1,9-11 These difficulties usually fall into 2 broad categories: (1) relative emotional neutrality to major life events that cause nonmilitary civilians great joy or sadness; and (2) overreaction to trivial events, causing significant irritation, anger, or sadness that normally would not produce such emotional reactions in nonmilitary civilians. The former is largely overlooked in medical literature to date except in relation to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) categories, and the latter is often described in limited terms as increased irritability, restlessness, and low frustration tolerance. This emotional dysregulation creates confusing paradoxes for veterans. For example, a veteran might feel no strong emotion when notified of the death of a close relative and yet cry uncontrollably while watching a sad scene in a fictional movie.
Sleep difficulties are intrinsic to the postdeployment period.9-12 Sleep-wake cycles often are altered, reflecting residual effects of the rigid schedules required by military duties and poor sleep hygiene in the combat theater. Inadequate, nonrestful sleep is frequently reported on return to the civilian world. Difficulty falling asleep or difficulty staying asleep also commonly occurs. Nightmares may be present.
Transient difficulty with concentration and attention is often prominent within the postdeployment transition period.9-11,13 Manifestations are variable, but problems with focusing on minor tasks are commonly reported. A more intense effort to master new concepts may be required. Learning styles developed during predeployment phases may be altered so that more conscious effort is required to comprehend and retain new information.
Short-term memory frequently may be affected during postdeployment transition.9-11,13 Veterans often report postdeployment difficulty in recalling appointments or tasks that must be completed even if they had a keen sense of memory during predeployment or deployment. Veterans also may have difficulty recalling the details of specific routines that were done without hesitation during deployment. Compared with predeployment time frames, veterans may exert greater effort to recall newly learned material.
Automatic behaviors necessary for survival in a combat theater still may be prominent in the postdeployment period.10,11,14 Aggressive driving required to avoid deployment ambush may be problematic during the postdeployment transition. Steering clear of any roadside trash may be a residual instinctive drive postdeployment because of the risk of improvised explosive devices concealed by debris in the combat theater. Veterans may avoid sitting with their back to the exit as the result of military safety training. Carrying weapons to ensure safety may be a compelling urge, because being armed and ready at all times was necessary for survival during deployment. Avoiding large crowds may be another strong tendency, because throngs of people were associated with potential danger in the combat theater.
Decision making may be challenging to resume in the postdeployment phase.9-11,15 In the deployment theater, time is relativel structured with rules in place, whereas at home veterans face a myriad of choices and decisions that must be made in order to complete the responsibilities of everyday living. As a result, making decisions about what item to buy, which clothes to wear, or what activities to prioritize, though relatively minor, can be a source of significant frustration. It may be difficult to independently navigate a realm of options available for new employment, schooling, or benefits, especially when there is little or no prior experience with these issues.
Relationship of Symptoms to Mental Health Diagnoses
Postdeployment transition symptoms do not automatically indicate the presence of an underlying mental health diagnosis. However, persistent and/or severe symptoms of postdeployment transition can overlap with or contribute to the development of mental health concerns (Table 1).14 The effects of the emotional disconnect also can exacerbate underlying mental health diagnoses.
While postdeployment emotional numbness to major life events, irritability, sleep disturbances, and impaired concentration can be associated with acute stress disorder (ASD) or PTSD, there is a constellation of other symptoms that must be present to diagnose these psychiatric conditions.16 Diagnostic criteria include persistent intrusive symptoms associated with the trauma, persistent avoidance of triggers/reminders associated with the trauma, significant changes in physiologic and cognitive arousal states, and negative changes in mood or cognition related to the trauma.16 The symptoms must cause significant impairment in some aspect of functioning on an individual, social, or occupational level. Acute stress disorder occurs when the symptoms last 30 days or less, whereas PTSD is diagnosed if the symptoms persist longer than a month.
Impaired emotional regulation, sleep disturbances, and decreased concentration also can be associated with depression or anxiety but are insufficient in themselves to make the diagnosis of those disorders.16 At least a 2-week history of depressed mood or inability to experience interest or pleasure in activities must be present as one of the criteria for depression as well as 4 or more other symptoms affecting sleep, appetite, energy, movement, self-esteem, or suicidal thoughts. Anxiety disorders have varying specific diagnostic criteria, but recurrent excessive worrying is a hallmark. Just like ASD or PTSD, the diagnostic symptoms of either depression or anxiety disorders must be causing significant impairment in functioning on an individual, social, or occupational level.
Irritability, sleep disturbances, agitation, memory impairment, and difficulty with concentration and attention can mimic the symptoms associated with mild-to-moderate traumatic brain injury (TBI).17,18 However, symptom onset must have a temporal relationship with a TBI. The presence of other TBI symptoms not associated with normal postdeployment transition usually can be used to differentiate between the diagnoses. Those TBI symptoms include recurrent headaches, poor balance, dizziness, tinnitus, and/or light sensitivity. In the majority of mild TBI cases, the symptoms resolve spontaneously within 3 months of TBI symptom manifestation.16,19 For those with persistent postconcussive syndrome, symptoms usually stabilize or improve over time.18,19 If symptoms worsen, there is often a confounding diagnosis such as PTSD or depression.17,20,21
Some returning combat veterans mistakenly believe postdeployment emotional transition symptoms are always a sign of a mental health disorder. Because there is a significant stigma associated with mental health disorders as well as potential repercussions on their service record if they use mental health resources, many reservists and National Guard members avoid accessing health care services if they are experiencing postdeployment adjustment issues, especially if those symptoms are related to emotional transitions.22-24 Unfortunately, such avoidance carries the risk that stress-inducing symptoms will persist and potentiate adjustment problems.
Course of Symptoms
The range for the postdeployment adjustment period generally falls within 3 to 12 months but can extend longer, depending on individual factors.10,11,25 Factors include presence of significant physical injury or illness, co-occurrence of mental health issues, underlying communication styles, and efficacy of coping strategies chosen. Although there is no clear-cut time frame for transition, ideally transition is complete when the returning veteran successfully enters his or her civilian lifestyle roles and feels a sense of purpose and belonging in society.
Postdeployment transition symptoms occur on a continuum in terms of duration and intensity for reservists and National Guard members. It is difficult to predict how specific transition symptoms will affect a particular veteran. The degree to which those symptoms will complicate reintegration depends on the individual veteran’s ability to adapt within the psychosocial context in which the symptoms occur. For example, minor irritation may be short-lived if a veteran can employ techniques to diffuse that feeling. Alternatively, minor irritation also suddenly may explode into a powerful wave of anger if the veteran has significant underlying emotional tension. Similarly, impaired short-term memory may be limited to forgetting a few appointments or may be so common that the veteran is at risk of losing track of his or her day. The level of memory impairment depends on emotional functioning, co-occurring stressors, and use of adaptive strategies.
In general, as these veterans successfully take on civilian routines, postdeployment transition symptoms will improve. Although such symptom improvement may be a passive process for some veterans, others will need to actively employ strategies to help change the military combat mind-set. The goal is to initiate useful interventions early in transition before symptoms become problematic.14
There are numerous self-help techniques and mobile apps that can be applied to a wide number of symptoms. Viable strategies include exercise, yoga, meditation, mindfulness training, and cognitive reframing. Reaching out for early assistance from various military assistance organizations that are well versed in dealing with postdeployment transition challenges often is helpful for reducing stress and navigating postdeployment obstacles (Table 2).
Symptom Strain and Exacerbation
Whenever stumbling blocks are encountered during the postdeployment period, any transition symptom can persist and/or worsen.10,11,14 Emotional disconnect and other transition symptoms can be exacerbated by physical, psychological, and social stressors common in the postdeployment period. Insomnia, poor quality sleep, or other sleep impairments that frequently occur as part of postdeployment transition can negatively impact the veteran’s ability to psychologically cope with daytime stressors. Poor concentration and short-term memory impairment noted by many reservists and National Guard members in the postdeployment phase can cause increased difficulty in attention to the moment and complicate completion of routine tasks. These difficulties can compound frustration and irritation to minor events and make it hard to emotionally connect with more serious issues.
Concentration and attention to mundane activities may be further reduced if the veteran feels no connection to the civilian world and/or experiences the surreal sensation that he or she should be attending to more serious life and death matters, such as those experienced in the combat theater. Ongoing psychological adjustment to physical injuries sustained during deployment can limit emotional flexibility when adapting to either minor or major stressors. Insufficient financial resources, work issues, or school problems can potentiate irritation, anger, and sadness and create an overwhelming emotional overload, leading to helplessness and hopelessness.
Perceived irregularities in emotional connection to the civilian world can significantly strain interpersonal relationships and be powerful impediments to successful reintegration.9,11,14 Failure to express emotions to major life events in the civilian world can result in combat veterans being viewed as not empathetic to others’ feelings. Overreaction to trivial events during postdeployment can lead to the veteran being labeled as unreasonable, controlling, and/or unpredictable. Persistent emotional disconnect with civilians engenders a growing sense of emotional isolation from family and friends when there is either incorrect interpretation of emotional transitions or failure to adapt healthy coping strategies. This isolation further enlarges the emotional chasm and may greatly diminish the veteran’s ability to seek assistance and appropriately address stressors in the civilian world.
Transition and the Family
Emotional disconnection may be more acutely felt within the immediate family unit.26 Redistribution of family unit responsibilities during deployment may mean that roles the veteran played during predeployment now may be handled by a partner. On the veteran’s return to the civilian world, such circumstances require active renegotiation of duties. Interactions with loved ones, especially children, may be colored by the family members’ individual perspectives on deployment as well as by the veteran’s transition symptoms. When there is disagreement about role responsibilities and/or underlying family resentment about deployment, conditions are ripe for significant discord between the veteran and family members, vital loss of partner intimacy, and notable loss of psychological safety to express feelings within the family unit. If there are concerns about infidelity by the veteran or significant other during the period of deployment, postdeployment tensions can further escalate. If unaddressed in the presence of emotional disconnect, any of these situations can raise the risk of domestic violence and destruction of relationships.
Without adequate knowledge of common postdeployment transitions and coping strategies, the postdeployment transition period is often bewildering to returning veterans and their families. They are taken aback by postdeployment behaviors that do not conform to the veteran’s predeployment personality or mannerisms. Families may feel they have “lost” the veteran and view the emotionally distant postdeployment veteran as a stranger. Veterans mistakenly may view the postdeployment emotional disconnect as evidence that they were permanently altered by deployment and no longer can assimilate into the civilian world. Unless veterans and families develop an awareness of the postdeployment transition symptoms and healthy coping strategies, these perspectives can contribute to a veteran’s persistent feelings of alienation, significant sense of personal failure, and loss of vital social supports.
When transition symptoms are or have the potential to become significant stressors, veterans would benefit from mental health counseling either individually or with family members. Overcoming the stigma of seeking mental health services can prove challenging. Explaining that these postdeployment symptoms occur commonly, stem from military combat training, can be reversed, and when reversed will empower the individual to control his or her life may help veterans overcome the stigma and seek mental health services.
The fear of future career impairment with the military reserve or National Guard is another real concern among this cohort who might consider accessing behavioral health care, especially since VA mental health medical records can be accessed by DoD officials through links with the VHA. Fortunately, this concern can be alleviated through the use of Vet Centers, free-standing counseling centers nationwide that offer no-cost individual and family counseling to veterans with combat exposure. Vet Center counseling records are completely confidential, never shared, and are not linked to the VHA electronic health record, the DoD, or any other entity. Although Vet Center providers don’t prescribe medications, the counselors can actively address many issues for veterans and their families. For individuals who do not live near a Vet Center or for those who require psychiatric medications, a frank discussion on the benefits of treatment vs the risk of treatment avoidance must be held.
Assessing Symptoms and Coping Mechanisms
Postdeployment transition symptoms vary, depending on the nature and context of the symptom. Not only must the returning reservist and National Guard member be screened for symptoms, but HCPs also should assess the impact of those symptoms on the veteran and his or her interpersonal relationships. Some veterans will feel that the symptoms have relatively minor impact in their lives, because the veteran can easily compensate for the transient effects. Others may feel that the symptoms are somewhat burdensome because the issues are complicating the smooth transition to civilian roles. Still others will judge the symptoms to be devastating because of the negative effects on personal control, selfesteem, and emotional connection with family and friends.
In addition to screening for symptoms, HCPs should assess these veterans’ current coping adaptations to various transition symptoms. Whereas some activities may be functional and promote reintegration, other short-term coping solutions may cripple the veteran’s ability to successfully resume civilian life. Global avoidance of communication with others and/or retreating from all social situations is a destructive coping pattern that can further alienate veterans from their families and the civilian world. Reacting with anger to all stressful issues is another maladaptive pattern of coping with life’s frustrations. Because of the potential to self-medicate when dealing with social difficulties, depression, anxiety, or other mental health diagnoses, veterans may develop an inappropriate reliance on drugs or alcohol to handle postdeployment stressors.27 Therefore, HCP screening for substance use disorders (SUD) is important so that interventions can be initiated early.
Because of the overlap of postdeployment transition symptoms with mental health disorders and the relative frequency of those mental health disorders among combat veterans, HCPs should have a heightened awareness of the potential for co-occurring mental health difficulties in the postdeployment reservist and National Guard cohort. Health care providers should screen for depression, anxiety, and PTSD. Even if initial screening is done early within the transition period, repeat screening would be of benefit 6 months into the postdeployment period because of the tendency of mental health issues to develop during that time.28,29
By evaluating the impact of the transition symptom and coping strategies on these veterans’ lives, HCPs can better determine which strategies might adequately compensate for symptom effects. In general, informal counseling, even if just to help veterans normalize postdeployment transition symptoms and develop a plan to address such symptoms, can significantly minimize the negative impact of transition symptoms.14,26 Specific symptoms should be targeted by interventions that match the degree of symptom impact.
Symptoms to be aggressively addressed are those that significantly interfere with successful reintegration into the civilian world. For example, persistent sleep difficulties should be dealt with because they can worsen all other transition symptoms. However, the majority of strategies to address sleep do not require medication unless there are confounding factors such as severe nightmares. Minor memory issues attributed to the transition phase can be mitigated by several strategies to improve recall, including use of task lists, digital calendars, or other memory-prodding techniques. However, severe memory issues related to depression or anxiety likely would require pharmaceutical assistance and formal counseling in addition to other nonpharmacologic approaches.
Intermittent irritation or restlessness may be amenable to selfhelp strategies, but significant anger outbursts or aggression will require additional support, such as formal behavioral interventions to help identify the triggers and develop strategic plans to reduce emotional tension. A mild sense of not belonging may resolve without intervention, but a stronger sense of alienation will require further evaluation.
Conclusion
Civilian reintegration after combat deployment is a gradual process rather than a discrete event for reservists and National Guard members. There are common, nonpathologic postdeployment transition symptoms that, if misunderstood or inappropriately addressed, can complicate civilian reintegration. Health care providers are in the unique position to promote a healthy postdeployment transition by assisting veterans to recognize nonpathologic transition symptoms, select appropriate coping strategies, and seek further assistance for more complex problems.
1. Pew Research Center. War and sacrifice in the post 9/11 era: executive summary. http://www
.pewsocialtrends.org/2011/10/05/war-and-sacrifice-in-the-post-911-era. Published October 5, 2011. Accessed June 12, 2017.
2. Interian A, Kline A, Callahan L, Losonczy M. Readjustment stressors and early mental health treatment seeking by returning National Guard soldiers with PTSD. Psychiatr Serv. 2012;63(9):855-861.
3. Spelman JF, Hunt SC, Seal KH, Burgo-Black AL. Post deployment care for returning combat veterans. J Gen Intern Med. 2012;27(9):1200-1209.
4. Vasterling JJ, Daily ES, Friedman MJ. Posttraumatic stress reactions over time: the battlefield, homecoming, and long-term course. In: Ruzek JI, Schnurr PP, Vasterling JJ, Friedman MJ, eds. Caring for Veterans With Deployment-Related Stress Disorders: Iraq, Afghanistan, and Beyond. Washington,DC: American Psychological Association;2011:chap 2.
5. Wilcox SL, Oh H, Redmon SA, Chicas J, Hassan AM, Lee PJ, Ell K. A scope of the problem: Postdeployment reintegration challenges in a National Guard Unit. Work. 2015;50(1):73-83.
6. Griffith J. Homecoming of citizen soldiers: Postdeployment problems and service use among Army National Guard soldiers. Community Ment Health J. 2017. doi:10.1007/s10597-017-0132-9. (Epub ahead of print)
7. Schultz M, Glickman ME, Eisen SV. Predictors of decline in overall mental health, PTSD and alcohol use in OEF/OIF veterans. Comprehensive Psychiatry. 2014;55(7):1654-1664.
8. Polusny MA, Kehle SM, Nelson NW, Erbes CR, Arbisi PA, Thuras P. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in National Guard soldiers deployed to Iraq. Arch Gen Psychiatry. 2011:68(1):79-89.
9. U.S. Department of Veterans Affairs, National Center for PTSD. Returning from the war zone: a guide for military personnel. http://www.ptsd.va.gov/public/reintegration/guide-pdf/SMGuide.pdf. Updated January 2014. Accessed June 12, 2017.
10. Slone LB, Friedman MJ. After the War Zone: A Practical Guide for Returning Troops and their Families. Philadelphia, PA: Da Capo Press; 2008.
11. Ainspan ND, Penk WE, eds. When the Warrior Returns: Making the Transition at Home. Annapolis, MD: Naval Institute Press; 2012.
12. Yosick T, Bates M, Moore M, Crowe C, Phillips J, Davison J. A review of post-deployment reintegration: evidence, challenges, and strategies for program development. http://www.dcoe.mil/files/Review_of_Post-Deployment_Reintegration.pdf. Published February 10, 2012. Accessed June 12, 2017.
13. Vasterling JJ, Proctor SP, Amoroso P, Kane R, Heeren T, White RF. Neuropsychological outcomes of army personnel following deployment to the Iraq war. JAMA. 2006;296(5):519-529.
14. Castro CA, Kintzle S, Hassan AM. The combat veteran paradox: paradoxes and dilemmas encountered with reintegrating combat veterans and the agencies that support them. Traumatology. 2015;21(4):299-310.
15. Rivers FM, Gordon S, Speraw S, Reese S. U.S. Army nurses’ reintegration and homecoming experiences after Iraq and Afghanistan. Mil Med. 2013;178(2):166-173.
16. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington,VA: American Psychiatric Association;2013.
17. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: Rand Corporation, 2008.
18. Orff HJ, Hays CC, Heldreth AA, Stein MB, Twamley EW. Clinical considerations in the evaluation and management of patients following traumatic brain injury. Focus. 2013;11(3):328-340.
19. Morissette SB, Woodward M, Kimbrel NA, et al. Deployment-related TBI, persistent postconcussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabil Psychol. 2011;56(4):340-350.
20. Polusny MA, Kehle SM, Nelson NW, Erbes CR, Arbisi PA, Thuras P. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in national guard soldiers deployed to Iraq. Arch Gen Psychiatry. 2011;68(1):79-89.
21. Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosom Med. 2012;74(3):249-257.
22. Hoge CW, Grossman SH, Auchterlonie JL, Riviere LA, Milliken CS, Wilk JE. PTSD treatment for soldiers after combat deployment: low utilization of mental health care and reasons for dropout. Psychiatr Serv. 2014;65(8):997-1004.
23. Hines LA, Goodwin L, Jones M, et al. Factors affecting help seeking for mental health problems after deployment to Iraq and Afghanistan. Psychiatr Serv. 2014;65(1):98-105.
24. Gorman LA, Blow AJ, Ames BD, Read PL. National Guard families after combat: mental health, use of mental health services, and perceived treatment barriers. Psychiatr Serv. 2011;62(1):28-34.
25. Marek LI, Hollingsworth WG, D’Aniello C, et al. Returning home: what we know about the reintegration of deployed service members into their families and communities. https://www.ncfr.org/ncfr-report/focus/military-families/returninghome. Published March 1, 2012. Accessed June 13, 2017.
26. Bowling UB, Sherman MD. Welcoming them home: supporting service members and their families in navigating the tasks of reintegration. Prof Psychol Res Pr. 2008;39(4):451-458.
27. Jacobson IG, Ryan MA, Hooper TI, et al. Alcohol use and alcohol-related problems before
and after military combat deployment. JAMA. 2008;300(6):663-675.
28. Seal KH, Metzler TH, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans Department of Veterans Affairs health care, 2002-2008. Am J Public Health. 2009;99(9):1651-1658.
29. Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298(18):2141-2148.
1. Pew Research Center. War and sacrifice in the post 9/11 era: executive summary. http://www
.pewsocialtrends.org/2011/10/05/war-and-sacrifice-in-the-post-911-era. Published October 5, 2011. Accessed June 12, 2017.
2. Interian A, Kline A, Callahan L, Losonczy M. Readjustment stressors and early mental health treatment seeking by returning National Guard soldiers with PTSD. Psychiatr Serv. 2012;63(9):855-861.
3. Spelman JF, Hunt SC, Seal KH, Burgo-Black AL. Post deployment care for returning combat veterans. J Gen Intern Med. 2012;27(9):1200-1209.
4. Vasterling JJ, Daily ES, Friedman MJ. Posttraumatic stress reactions over time: the battlefield, homecoming, and long-term course. In: Ruzek JI, Schnurr PP, Vasterling JJ, Friedman MJ, eds. Caring for Veterans With Deployment-Related Stress Disorders: Iraq, Afghanistan, and Beyond. Washington,DC: American Psychological Association;2011:chap 2.
5. Wilcox SL, Oh H, Redmon SA, Chicas J, Hassan AM, Lee PJ, Ell K. A scope of the problem: Postdeployment reintegration challenges in a National Guard Unit. Work. 2015;50(1):73-83.
6. Griffith J. Homecoming of citizen soldiers: Postdeployment problems and service use among Army National Guard soldiers. Community Ment Health J. 2017. doi:10.1007/s10597-017-0132-9. (Epub ahead of print)
7. Schultz M, Glickman ME, Eisen SV. Predictors of decline in overall mental health, PTSD and alcohol use in OEF/OIF veterans. Comprehensive Psychiatry. 2014;55(7):1654-1664.
8. Polusny MA, Kehle SM, Nelson NW, Erbes CR, Arbisi PA, Thuras P. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in National Guard soldiers deployed to Iraq. Arch Gen Psychiatry. 2011:68(1):79-89.
9. U.S. Department of Veterans Affairs, National Center for PTSD. Returning from the war zone: a guide for military personnel. http://www.ptsd.va.gov/public/reintegration/guide-pdf/SMGuide.pdf. Updated January 2014. Accessed June 12, 2017.
10. Slone LB, Friedman MJ. After the War Zone: A Practical Guide for Returning Troops and their Families. Philadelphia, PA: Da Capo Press; 2008.
11. Ainspan ND, Penk WE, eds. When the Warrior Returns: Making the Transition at Home. Annapolis, MD: Naval Institute Press; 2012.
12. Yosick T, Bates M, Moore M, Crowe C, Phillips J, Davison J. A review of post-deployment reintegration: evidence, challenges, and strategies for program development. http://www.dcoe.mil/files/Review_of_Post-Deployment_Reintegration.pdf. Published February 10, 2012. Accessed June 12, 2017.
13. Vasterling JJ, Proctor SP, Amoroso P, Kane R, Heeren T, White RF. Neuropsychological outcomes of army personnel following deployment to the Iraq war. JAMA. 2006;296(5):519-529.
14. Castro CA, Kintzle S, Hassan AM. The combat veteran paradox: paradoxes and dilemmas encountered with reintegrating combat veterans and the agencies that support them. Traumatology. 2015;21(4):299-310.
15. Rivers FM, Gordon S, Speraw S, Reese S. U.S. Army nurses’ reintegration and homecoming experiences after Iraq and Afghanistan. Mil Med. 2013;178(2):166-173.
16. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington,VA: American Psychiatric Association;2013.
17. Tanielian T, Jaycox LH, eds. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: Rand Corporation, 2008.
18. Orff HJ, Hays CC, Heldreth AA, Stein MB, Twamley EW. Clinical considerations in the evaluation and management of patients following traumatic brain injury. Focus. 2013;11(3):328-340.
19. Morissette SB, Woodward M, Kimbrel NA, et al. Deployment-related TBI, persistent postconcussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabil Psychol. 2011;56(4):340-350.
20. Polusny MA, Kehle SM, Nelson NW, Erbes CR, Arbisi PA, Thuras P. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in national guard soldiers deployed to Iraq. Arch Gen Psychiatry. 2011;68(1):79-89.
21. Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: association with postdeployment symptoms. Psychosom Med. 2012;74(3):249-257.
22. Hoge CW, Grossman SH, Auchterlonie JL, Riviere LA, Milliken CS, Wilk JE. PTSD treatment for soldiers after combat deployment: low utilization of mental health care and reasons for dropout. Psychiatr Serv. 2014;65(8):997-1004.
23. Hines LA, Goodwin L, Jones M, et al. Factors affecting help seeking for mental health problems after deployment to Iraq and Afghanistan. Psychiatr Serv. 2014;65(1):98-105.
24. Gorman LA, Blow AJ, Ames BD, Read PL. National Guard families after combat: mental health, use of mental health services, and perceived treatment barriers. Psychiatr Serv. 2011;62(1):28-34.
25. Marek LI, Hollingsworth WG, D’Aniello C, et al. Returning home: what we know about the reintegration of deployed service members into their families and communities. https://www.ncfr.org/ncfr-report/focus/military-families/returninghome. Published March 1, 2012. Accessed June 13, 2017.
26. Bowling UB, Sherman MD. Welcoming them home: supporting service members and their families in navigating the tasks of reintegration. Prof Psychol Res Pr. 2008;39(4):451-458.
27. Jacobson IG, Ryan MA, Hooper TI, et al. Alcohol use and alcohol-related problems before
and after military combat deployment. JAMA. 2008;300(6):663-675.
28. Seal KH, Metzler TH, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans Department of Veterans Affairs health care, 2002-2008. Am J Public Health. 2009;99(9):1651-1658.
29. Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298(18):2141-2148.