User login
An 84‐year‐old female patient with hypertension, osteoarthritis, hypothyroidism, and remote breast cancer was admitted with complaints of generalized abdominal pain of 2 months' duration. Pain was described as noncolicky in nature and was associated with diarrhea. She reported 78 daily episodes of watery, non‐foul‐smelling diarrhea. She denied any nausea, vomiting, fever, joint pains, oral ulcers, eye redness, stool incontinence, melena, hematochezia, or weight loss. There was no history of recent travel, antibiotic use, or exposure to sick contacts. She had no risk factors for HIV infection or other sexually transmitted infections. Her social history was significant for dining out on a regular basis and living in an assisted living facility. However, she denied any relationship between her abdominal symptoms and any particular food intake or with bowel movements. She denied any anal pruritis but reported seeing white squiggly things on tissue paper after bowel movements. She denied use of over‐the‐counter laxatives or herbal supplements. None of her prescription medications had diarrhea as a major side effect. Her social history was unremarkable for smoking, alcohol use, or illicit drug use. There were no prior abdominal surgeries. The patient's physical exam showed normal vitals on presentation and was unremarkable except for vague, generalized abdominal tenderness with no involuntary guarding or rebound pain. Her initial laboratory evaluation showed normal complete blood counts with no eosinophilia and normal serum electrolytes and liver and thyroid panel. Acute‐phase reactants, erythrocyte sedimentation rate, and C‐reactive protein were not elevated. Stool evaluation was unremarkable for Clostridium difficile toxin, fat droplets, leukocytes, erythrocytes, ova, parasites, or any bacterial growth on cultures. Computed tomography scans of the abdomen and pelvis were nonrevealing. Her colonoscopic examination 1 year prior was significant only for diverticulosis.1, 2
The patient was treated with loperamide as an outpatient with no relief. She was then admitted to the hospital for further diagnostic workup. Hospital workup included a Scotch tape test, which showed adult pinworms. She was treated with a single dose of 400 mg of albendazole with complete resolution of her symptoms within 2 days. No further workup was done. Patient was discharged with advice to contact her primary care doctor for reevaluation if symptoms recurred. However, the patient remained symptom free 1 year after discharge.
DISCUSSION
Enterobius vermicularis is a parasite that infects 2040 million people annually in the United States and about 200 million people worldwide. Equal infection rates are seen in all races, socioeconomic classes, and cultures.1 It is more prevalent among those in crowded living conditions. Humans are the primary natural host for the parasite, although it has been documented in cockroaches and primates. Transmission occurs via the feco‐oral route or via airborne eggs that are dislodged from contaminated clothing or bed linen. Its life cycle begins with parasite eggs hatching in the duodenum, usually within 6 hours of ingestion. They mature into adults in as little as 2 weeks and have a life span of approximately 2 months. Enterobius vermicularis normally inhabits distal small bowel including the terminal ileum, cecum, and vermiform appendix, as well as the proximal ascending colon. After copulation, an adult female will migrate to the perineum, often at night, and lay an average of 10,00015,000 eggs. These eggs mature in about 6 hours and are then transmitted to a new host by the feco‐oral route. The worms live mainly in the intestinal lumen and do not invade tissue. Hence, pinworm infections, unlike many other parasitic infections, are rarely associated with serum eosinophilia or elevated serum IgE levels.
E. vermicularis is generally considered to be an innocuous parasite. Perianal pruritis, especially during the nighttime, is the most common symptom. Patients may develop secondary bacterial infection of the irritated anal skin. Rarely, E. vermicularis infection may result in a life‐threatening illness. A literature review showed pinworm infection to be an infrequent cause of eosinophilic enterocolitis, appendicitis, intestinal obstruction, intestinal perforation, hepatic infection, urinary tract infection, sialoadenitis, salpingitis, enterocolitis, eosinophilic ileocolitis, vulvovaginitis, pelvic inflammatory disease, conditions mimicking inflammatory bowel diseases, perianal abscesses, and perianal granulomas. In a retrospective review of 180 colonoscopies done on patients with rectal bleeding or suspected inflammatory bowel disease, E. vermicularis was identified macroscopically in 31 cases (17.2%). Data collected on 23 of these cases showed that symptoms were present for a mean of 17 months; the symptoms with the highest frequency were abdominal pain (73%), rectal bleeding (62%), chronic diarrhea (50%), and weight loss (42%). None of these patients experienced perianal pruritis or developed inflammatory bowel disease during the follow‐up period of up to 5 years, although 21 patients demonstrated histopathological evidence of nonspecific colitis.6
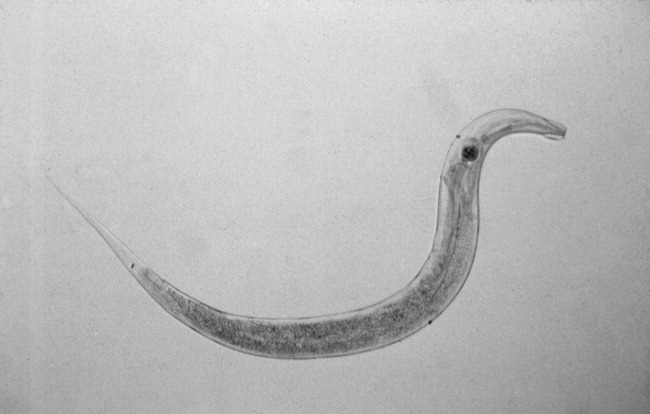
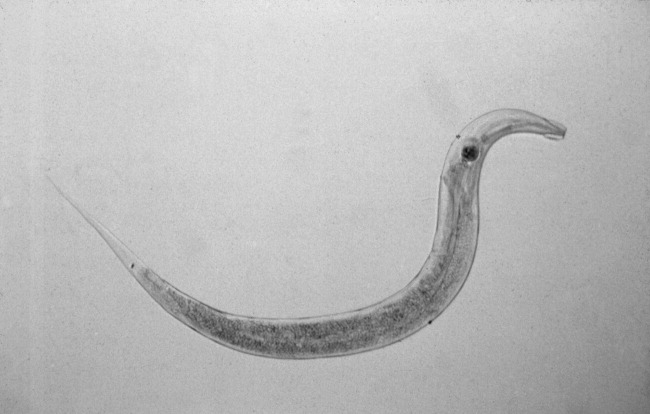
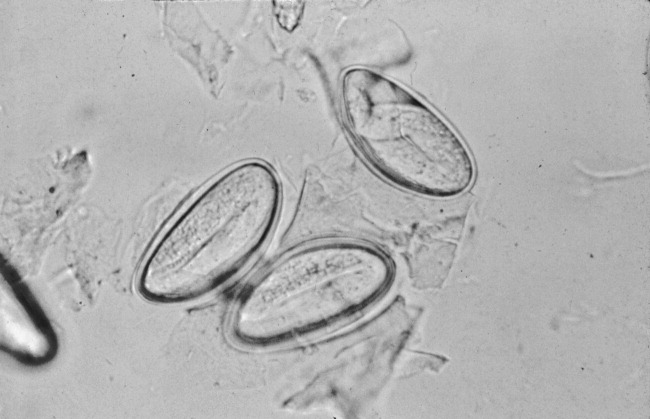
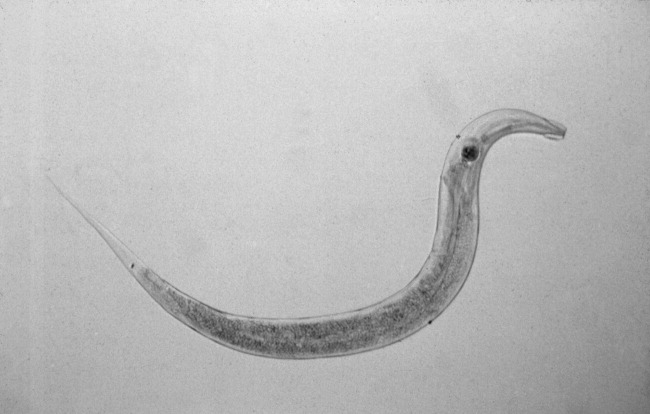
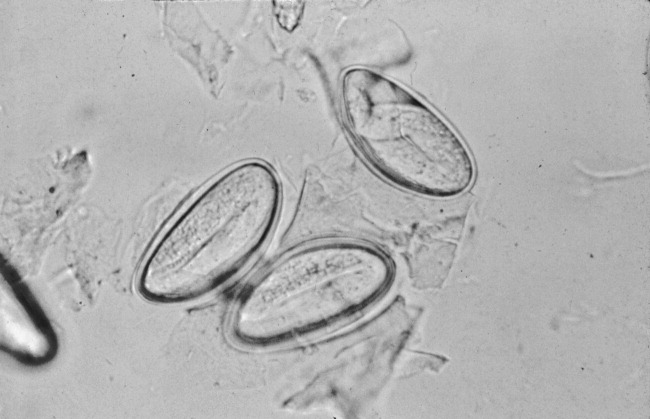
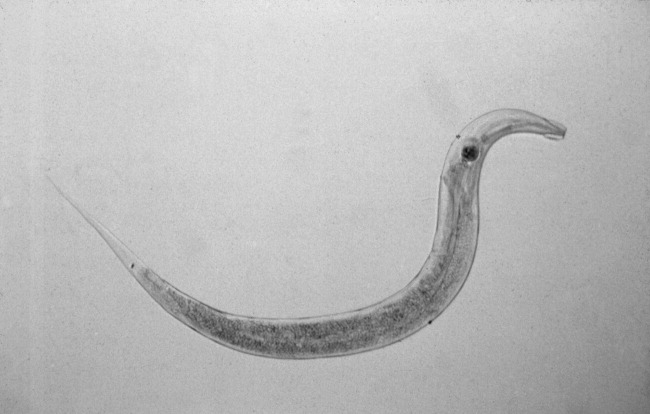
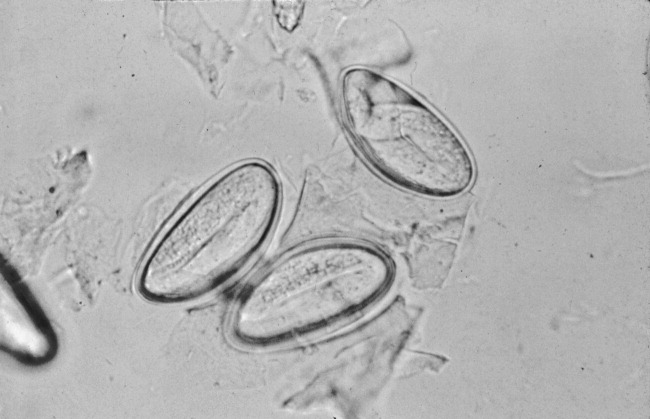
The gold standard for diagnosing E. vermicularis infection is by visualizing the worms directly or by examination of the parasitic eggs under a microscope. The Scotch tape test is a simple, inexpensive, and quick way for confirming the infection. It is performed by doubling clear cellophane Scotch tape onto a wooden stick so that the sticky side points outward and pressing it against the perianal skin. The kidney‐bean‐shaped eggs (50 25 m) will stick to the tape and can then be directly visualized under a microscope. Pinworms are most active during the night, and eggs are deposited around the perianal region and are best recovered before defecation, early in the morning. The sensitivity of this test is 90% if done on 3 consecutive mornings and goes up to 99% when performed on 5 consecutive mornings.2, 3 Female adult worms are pin‐shaped, about 813 mm long, and white in color. They may be seen by direct visualization in the perianal region or more invasively by an anoscopic or colonoscopic examination. However, endoscopic examination may sometimes give false‐negative results as the worms are small, (ie, only a few millimeters in length) and may be missed if the endoscopist is not actively looking for them.
A single oral dose of benzimidazoles (100 mg of mebendazole or 400 mg of albendazole) results in a cure of rate of 95% and 100%, respectively. Despite the high initial cure rates, reinfection remains common; hence, a second dose 12 weeks after the initial treatment is often given to prevent it.4, 5 Pyrantel pamoate and piperazine are alternate treatments. However, they have lower efficacy and are more toxic than benzimidazoles.
Close contacts such as household members are often concurrently infected, and treatment of the remaining household members or of the group institution is also indicated. All bedding and clothes should be laundered. Personal hygiene such as fingernail clipping, frequent hand washing, and bathing should also be encouraged.
Although the pinworm's entire life cycle is in the human intestinal tract, gastrointestinal symptoms have seldom been reported. However, this may be because of underreporting. Given the increasing number of patients living in institutionalized environments such as nursing homes and assisted living, it is important to consider the possibility of E. vermicularis infection early on in a diagnostic workup of patients presenting with symptoms of colitis, even when not accompanied by anal pruritis. In a patient presenting with symptoms of inflammatory bowel disease with histopathological evaluation of nonspecific colitis should prompt clinicians to consider E. vermicularis infection.6 On the other hand, in patients who fail to respond to antiparasitic therapy or those who present with weight loss, change in bowel habits, or melena, colonscopic examination is warranted. Considering pinworm infection early during evaluation of nonspecific abdominal complaints may avoid an unnecessary and expensive diagnostic workup.
KEY POINTS
-
Recognize early on that Enterobius vermicularis infection is an important differential diagnosis for patients presenting with symptoms of colitis, thus avoiding unnecessary, expensive, and potentially harmful invasive testing.
-
Recognize that a simple and inexpensive Scotch tape test and/or direct visualization is an easy and effective way of confirming diagnosis and that stool examination may be unhelpful.
-
Recognize that reinfection may be prevented using a second dose of the antiparasitic drug.
- .The pinworm, Enterobius vermicularis.Prim Care.1991;18:13–24.
- ,,,,.Prevalence of intestinal parasites in three socioeconomically‐different regions of Sivas, Turkey.J Health Popul Nutr.2005;23:184–191.
- ,,,.Pinworm infection.Gastrointest Endosc.2001;53:210.
- ,,.Mebendazole (R 17635) in enterobiasis. A clinical trial in mental retardates.Chemotherapy.1975;21:255–260.
- ,,, et al.Field trials on the efficacy of albendazole composite against intestinal nematodiasis.Chung Kuo Chi Sheng Chung Hsueh Yu Chi Sheng Chung Ping Tsa Chih.1998;16:1–5.
- ,,.Enterobius vermicularis and colitis in children.J Pediatr Gastroenterol Nutr.2006;43:610–612.
An 84‐year‐old female patient with hypertension, osteoarthritis, hypothyroidism, and remote breast cancer was admitted with complaints of generalized abdominal pain of 2 months' duration. Pain was described as noncolicky in nature and was associated with diarrhea. She reported 78 daily episodes of watery, non‐foul‐smelling diarrhea. She denied any nausea, vomiting, fever, joint pains, oral ulcers, eye redness, stool incontinence, melena, hematochezia, or weight loss. There was no history of recent travel, antibiotic use, or exposure to sick contacts. She had no risk factors for HIV infection or other sexually transmitted infections. Her social history was significant for dining out on a regular basis and living in an assisted living facility. However, she denied any relationship between her abdominal symptoms and any particular food intake or with bowel movements. She denied any anal pruritis but reported seeing white squiggly things on tissue paper after bowel movements. She denied use of over‐the‐counter laxatives or herbal supplements. None of her prescription medications had diarrhea as a major side effect. Her social history was unremarkable for smoking, alcohol use, or illicit drug use. There were no prior abdominal surgeries. The patient's physical exam showed normal vitals on presentation and was unremarkable except for vague, generalized abdominal tenderness with no involuntary guarding or rebound pain. Her initial laboratory evaluation showed normal complete blood counts with no eosinophilia and normal serum electrolytes and liver and thyroid panel. Acute‐phase reactants, erythrocyte sedimentation rate, and C‐reactive protein were not elevated. Stool evaluation was unremarkable for Clostridium difficile toxin, fat droplets, leukocytes, erythrocytes, ova, parasites, or any bacterial growth on cultures. Computed tomography scans of the abdomen and pelvis were nonrevealing. Her colonoscopic examination 1 year prior was significant only for diverticulosis.1, 2
The patient was treated with loperamide as an outpatient with no relief. She was then admitted to the hospital for further diagnostic workup. Hospital workup included a Scotch tape test, which showed adult pinworms. She was treated with a single dose of 400 mg of albendazole with complete resolution of her symptoms within 2 days. No further workup was done. Patient was discharged with advice to contact her primary care doctor for reevaluation if symptoms recurred. However, the patient remained symptom free 1 year after discharge.
DISCUSSION
Enterobius vermicularis is a parasite that infects 2040 million people annually in the United States and about 200 million people worldwide. Equal infection rates are seen in all races, socioeconomic classes, and cultures.1 It is more prevalent among those in crowded living conditions. Humans are the primary natural host for the parasite, although it has been documented in cockroaches and primates. Transmission occurs via the feco‐oral route or via airborne eggs that are dislodged from contaminated clothing or bed linen. Its life cycle begins with parasite eggs hatching in the duodenum, usually within 6 hours of ingestion. They mature into adults in as little as 2 weeks and have a life span of approximately 2 months. Enterobius vermicularis normally inhabits distal small bowel including the terminal ileum, cecum, and vermiform appendix, as well as the proximal ascending colon. After copulation, an adult female will migrate to the perineum, often at night, and lay an average of 10,00015,000 eggs. These eggs mature in about 6 hours and are then transmitted to a new host by the feco‐oral route. The worms live mainly in the intestinal lumen and do not invade tissue. Hence, pinworm infections, unlike many other parasitic infections, are rarely associated with serum eosinophilia or elevated serum IgE levels.
E. vermicularis is generally considered to be an innocuous parasite. Perianal pruritis, especially during the nighttime, is the most common symptom. Patients may develop secondary bacterial infection of the irritated anal skin. Rarely, E. vermicularis infection may result in a life‐threatening illness. A literature review showed pinworm infection to be an infrequent cause of eosinophilic enterocolitis, appendicitis, intestinal obstruction, intestinal perforation, hepatic infection, urinary tract infection, sialoadenitis, salpingitis, enterocolitis, eosinophilic ileocolitis, vulvovaginitis, pelvic inflammatory disease, conditions mimicking inflammatory bowel diseases, perianal abscesses, and perianal granulomas. In a retrospective review of 180 colonoscopies done on patients with rectal bleeding or suspected inflammatory bowel disease, E. vermicularis was identified macroscopically in 31 cases (17.2%). Data collected on 23 of these cases showed that symptoms were present for a mean of 17 months; the symptoms with the highest frequency were abdominal pain (73%), rectal bleeding (62%), chronic diarrhea (50%), and weight loss (42%). None of these patients experienced perianal pruritis or developed inflammatory bowel disease during the follow‐up period of up to 5 years, although 21 patients demonstrated histopathological evidence of nonspecific colitis.6
The gold standard for diagnosing E. vermicularis infection is by visualizing the worms directly or by examination of the parasitic eggs under a microscope. The Scotch tape test is a simple, inexpensive, and quick way for confirming the infection. It is performed by doubling clear cellophane Scotch tape onto a wooden stick so that the sticky side points outward and pressing it against the perianal skin. The kidney‐bean‐shaped eggs (50 25 m) will stick to the tape and can then be directly visualized under a microscope. Pinworms are most active during the night, and eggs are deposited around the perianal region and are best recovered before defecation, early in the morning. The sensitivity of this test is 90% if done on 3 consecutive mornings and goes up to 99% when performed on 5 consecutive mornings.2, 3 Female adult worms are pin‐shaped, about 813 mm long, and white in color. They may be seen by direct visualization in the perianal region or more invasively by an anoscopic or colonoscopic examination. However, endoscopic examination may sometimes give false‐negative results as the worms are small, (ie, only a few millimeters in length) and may be missed if the endoscopist is not actively looking for them.
A single oral dose of benzimidazoles (100 mg of mebendazole or 400 mg of albendazole) results in a cure of rate of 95% and 100%, respectively. Despite the high initial cure rates, reinfection remains common; hence, a second dose 12 weeks after the initial treatment is often given to prevent it.4, 5 Pyrantel pamoate and piperazine are alternate treatments. However, they have lower efficacy and are more toxic than benzimidazoles.
Close contacts such as household members are often concurrently infected, and treatment of the remaining household members or of the group institution is also indicated. All bedding and clothes should be laundered. Personal hygiene such as fingernail clipping, frequent hand washing, and bathing should also be encouraged.
Although the pinworm's entire life cycle is in the human intestinal tract, gastrointestinal symptoms have seldom been reported. However, this may be because of underreporting. Given the increasing number of patients living in institutionalized environments such as nursing homes and assisted living, it is important to consider the possibility of E. vermicularis infection early on in a diagnostic workup of patients presenting with symptoms of colitis, even when not accompanied by anal pruritis. In a patient presenting with symptoms of inflammatory bowel disease with histopathological evaluation of nonspecific colitis should prompt clinicians to consider E. vermicularis infection.6 On the other hand, in patients who fail to respond to antiparasitic therapy or those who present with weight loss, change in bowel habits, or melena, colonscopic examination is warranted. Considering pinworm infection early during evaluation of nonspecific abdominal complaints may avoid an unnecessary and expensive diagnostic workup.
KEY POINTS
-
Recognize early on that Enterobius vermicularis infection is an important differential diagnosis for patients presenting with symptoms of colitis, thus avoiding unnecessary, expensive, and potentially harmful invasive testing.
-
Recognize that a simple and inexpensive Scotch tape test and/or direct visualization is an easy and effective way of confirming diagnosis and that stool examination may be unhelpful.
-
Recognize that reinfection may be prevented using a second dose of the antiparasitic drug.
An 84‐year‐old female patient with hypertension, osteoarthritis, hypothyroidism, and remote breast cancer was admitted with complaints of generalized abdominal pain of 2 months' duration. Pain was described as noncolicky in nature and was associated with diarrhea. She reported 78 daily episodes of watery, non‐foul‐smelling diarrhea. She denied any nausea, vomiting, fever, joint pains, oral ulcers, eye redness, stool incontinence, melena, hematochezia, or weight loss. There was no history of recent travel, antibiotic use, or exposure to sick contacts. She had no risk factors for HIV infection or other sexually transmitted infections. Her social history was significant for dining out on a regular basis and living in an assisted living facility. However, she denied any relationship between her abdominal symptoms and any particular food intake or with bowel movements. She denied any anal pruritis but reported seeing white squiggly things on tissue paper after bowel movements. She denied use of over‐the‐counter laxatives or herbal supplements. None of her prescription medications had diarrhea as a major side effect. Her social history was unremarkable for smoking, alcohol use, or illicit drug use. There were no prior abdominal surgeries. The patient's physical exam showed normal vitals on presentation and was unremarkable except for vague, generalized abdominal tenderness with no involuntary guarding or rebound pain. Her initial laboratory evaluation showed normal complete blood counts with no eosinophilia and normal serum electrolytes and liver and thyroid panel. Acute‐phase reactants, erythrocyte sedimentation rate, and C‐reactive protein were not elevated. Stool evaluation was unremarkable for Clostridium difficile toxin, fat droplets, leukocytes, erythrocytes, ova, parasites, or any bacterial growth on cultures. Computed tomography scans of the abdomen and pelvis were nonrevealing. Her colonoscopic examination 1 year prior was significant only for diverticulosis.1, 2
The patient was treated with loperamide as an outpatient with no relief. She was then admitted to the hospital for further diagnostic workup. Hospital workup included a Scotch tape test, which showed adult pinworms. She was treated with a single dose of 400 mg of albendazole with complete resolution of her symptoms within 2 days. No further workup was done. Patient was discharged with advice to contact her primary care doctor for reevaluation if symptoms recurred. However, the patient remained symptom free 1 year after discharge.
DISCUSSION
Enterobius vermicularis is a parasite that infects 2040 million people annually in the United States and about 200 million people worldwide. Equal infection rates are seen in all races, socioeconomic classes, and cultures.1 It is more prevalent among those in crowded living conditions. Humans are the primary natural host for the parasite, although it has been documented in cockroaches and primates. Transmission occurs via the feco‐oral route or via airborne eggs that are dislodged from contaminated clothing or bed linen. Its life cycle begins with parasite eggs hatching in the duodenum, usually within 6 hours of ingestion. They mature into adults in as little as 2 weeks and have a life span of approximately 2 months. Enterobius vermicularis normally inhabits distal small bowel including the terminal ileum, cecum, and vermiform appendix, as well as the proximal ascending colon. After copulation, an adult female will migrate to the perineum, often at night, and lay an average of 10,00015,000 eggs. These eggs mature in about 6 hours and are then transmitted to a new host by the feco‐oral route. The worms live mainly in the intestinal lumen and do not invade tissue. Hence, pinworm infections, unlike many other parasitic infections, are rarely associated with serum eosinophilia or elevated serum IgE levels.
E. vermicularis is generally considered to be an innocuous parasite. Perianal pruritis, especially during the nighttime, is the most common symptom. Patients may develop secondary bacterial infection of the irritated anal skin. Rarely, E. vermicularis infection may result in a life‐threatening illness. A literature review showed pinworm infection to be an infrequent cause of eosinophilic enterocolitis, appendicitis, intestinal obstruction, intestinal perforation, hepatic infection, urinary tract infection, sialoadenitis, salpingitis, enterocolitis, eosinophilic ileocolitis, vulvovaginitis, pelvic inflammatory disease, conditions mimicking inflammatory bowel diseases, perianal abscesses, and perianal granulomas. In a retrospective review of 180 colonoscopies done on patients with rectal bleeding or suspected inflammatory bowel disease, E. vermicularis was identified macroscopically in 31 cases (17.2%). Data collected on 23 of these cases showed that symptoms were present for a mean of 17 months; the symptoms with the highest frequency were abdominal pain (73%), rectal bleeding (62%), chronic diarrhea (50%), and weight loss (42%). None of these patients experienced perianal pruritis or developed inflammatory bowel disease during the follow‐up period of up to 5 years, although 21 patients demonstrated histopathological evidence of nonspecific colitis.6
The gold standard for diagnosing E. vermicularis infection is by visualizing the worms directly or by examination of the parasitic eggs under a microscope. The Scotch tape test is a simple, inexpensive, and quick way for confirming the infection. It is performed by doubling clear cellophane Scotch tape onto a wooden stick so that the sticky side points outward and pressing it against the perianal skin. The kidney‐bean‐shaped eggs (50 25 m) will stick to the tape and can then be directly visualized under a microscope. Pinworms are most active during the night, and eggs are deposited around the perianal region and are best recovered before defecation, early in the morning. The sensitivity of this test is 90% if done on 3 consecutive mornings and goes up to 99% when performed on 5 consecutive mornings.2, 3 Female adult worms are pin‐shaped, about 813 mm long, and white in color. They may be seen by direct visualization in the perianal region or more invasively by an anoscopic or colonoscopic examination. However, endoscopic examination may sometimes give false‐negative results as the worms are small, (ie, only a few millimeters in length) and may be missed if the endoscopist is not actively looking for them.
A single oral dose of benzimidazoles (100 mg of mebendazole or 400 mg of albendazole) results in a cure of rate of 95% and 100%, respectively. Despite the high initial cure rates, reinfection remains common; hence, a second dose 12 weeks after the initial treatment is often given to prevent it.4, 5 Pyrantel pamoate and piperazine are alternate treatments. However, they have lower efficacy and are more toxic than benzimidazoles.
Close contacts such as household members are often concurrently infected, and treatment of the remaining household members or of the group institution is also indicated. All bedding and clothes should be laundered. Personal hygiene such as fingernail clipping, frequent hand washing, and bathing should also be encouraged.
Although the pinworm's entire life cycle is in the human intestinal tract, gastrointestinal symptoms have seldom been reported. However, this may be because of underreporting. Given the increasing number of patients living in institutionalized environments such as nursing homes and assisted living, it is important to consider the possibility of E. vermicularis infection early on in a diagnostic workup of patients presenting with symptoms of colitis, even when not accompanied by anal pruritis. In a patient presenting with symptoms of inflammatory bowel disease with histopathological evaluation of nonspecific colitis should prompt clinicians to consider E. vermicularis infection.6 On the other hand, in patients who fail to respond to antiparasitic therapy or those who present with weight loss, change in bowel habits, or melena, colonscopic examination is warranted. Considering pinworm infection early during evaluation of nonspecific abdominal complaints may avoid an unnecessary and expensive diagnostic workup.
KEY POINTS
-
Recognize early on that Enterobius vermicularis infection is an important differential diagnosis for patients presenting with symptoms of colitis, thus avoiding unnecessary, expensive, and potentially harmful invasive testing.
-
Recognize that a simple and inexpensive Scotch tape test and/or direct visualization is an easy and effective way of confirming diagnosis and that stool examination may be unhelpful.
-
Recognize that reinfection may be prevented using a second dose of the antiparasitic drug.
- .The pinworm, Enterobius vermicularis.Prim Care.1991;18:13–24.
- ,,,,.Prevalence of intestinal parasites in three socioeconomically‐different regions of Sivas, Turkey.J Health Popul Nutr.2005;23:184–191.
- ,,,.Pinworm infection.Gastrointest Endosc.2001;53:210.
- ,,.Mebendazole (R 17635) in enterobiasis. A clinical trial in mental retardates.Chemotherapy.1975;21:255–260.
- ,,, et al.Field trials on the efficacy of albendazole composite against intestinal nematodiasis.Chung Kuo Chi Sheng Chung Hsueh Yu Chi Sheng Chung Ping Tsa Chih.1998;16:1–5.
- ,,.Enterobius vermicularis and colitis in children.J Pediatr Gastroenterol Nutr.2006;43:610–612.
- .The pinworm, Enterobius vermicularis.Prim Care.1991;18:13–24.
- ,,,,.Prevalence of intestinal parasites in three socioeconomically‐different regions of Sivas, Turkey.J Health Popul Nutr.2005;23:184–191.
- ,,,.Pinworm infection.Gastrointest Endosc.2001;53:210.
- ,,.Mebendazole (R 17635) in enterobiasis. A clinical trial in mental retardates.Chemotherapy.1975;21:255–260.
- ,,, et al.Field trials on the efficacy of albendazole composite against intestinal nematodiasis.Chung Kuo Chi Sheng Chung Hsueh Yu Chi Sheng Chung Ping Tsa Chih.1998;16:1–5.
- ,,.Enterobius vermicularis and colitis in children.J Pediatr Gastroenterol Nutr.2006;43:610–612.