The Diagnosis: Lues Maligna
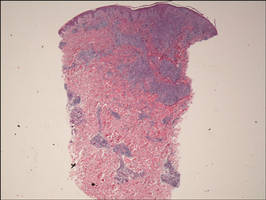
Biopsy revealed dense nodular aggregates of lymphocytes, histiocytes, and abundant plasma cells in both the superficial and deep dermis (Figure 1). There were perivascular and periadnexal aggregates of lymphocytes, histiocytes, and numerous plasma cells (Figure 2). Special stains for organisms, including Warthin-Starry silver, Giemsa, acid-fast bacilli, Gomori methenamine-silver, and Brown-Brenn stains were negative. Immunoperoxidase stain for Treponema pallidum also was negative. The patient’s rapid plasma reagin titer at the time of the fourth biopsy was 1:256, and appropriate treatment with penicillin resulted in complete clearance of the lesions in 3 to 4 weeks.
| Figure 1. Superficial and deep perivascular and periadnexal lymphohistiocytic infiltrate (H&E, original magnification ×2). |
| Figure 2. Perivascular and periadnexal aggregates of lymphocytes, histiocytes, and numerous plasma cells (H&E, original magnification ×20). |
Syphilis is caused by T pallidum. Three stages typically are identified in immunocompetent hosts: primary, secondary, and tertiary syphilis. Immunocompromised patients with human immunodeficiency virus (HIV) infection may have unusual presentations.
Lues maligna is used to describe a rare noduloulcerative form of secondary syphilis.1 It was first described in 18592 and has been associated with other disorders such as diabetes mellitus3 and chronic alcoholism.4 Patients usually are gravely ill and develop polymorphic ulcerating lesions. Facial and scalp involvement are common, but patients typically do not have palmoplantar involvement in conventional presentations of secondary syphilis.
A scanning view of a punch biopsy from our patient revealed irregular acanthosis of the epidermis with long and thin rete pegs, a bandlike infiltrate at the dermoepidermal junction, and a dense superficial and deep perivascular and periadnexal infiltrate. The histologic differential diagnosis includes pyoderma gangrenosum, vasculitis, lymphoma, leishmaniasis, leprosy, yaws, and mycobacterial or fungal infections.
The Centers for Disease Control and Prevention recommends screening of all HIV-positive indivi-duals for syphilis, and all sexually active individuals with syphilis should be screened for HIV.5 If clinical examination and findings suggest syphilis in the presence of negative serologic testing, then direct fluorescence assay for T pallidum staining of lesions, exudates or biopsy, or dark-field microscopic examination should be performed. In our case, dark-field microscopy was not performed and serologic tests were negative at presentation. Silver stains can detect T pallidum in tissue specimens, though detection may not be possible late in the course of disease.6
The morphology and rapid response to treatment confirmed the diagnosis in our patient. The incidence of syphilis in HIV-positive patients has risen substantially in the last 2 decades. This case illustrates an uncommon presentation that is increasing in prevalence.