Migraine is a form of recurrent headache that can present as migraine with aura or migraine without aura, with the latter being the most common form. As in this patient, migraine without aura is a chronic form of headache of moderate to severe intensity that usually lasts for several hours but rarely may persist for up to 3 days. Headache pain is unilateral and often aggravated by triggers such as routine physical activity. The American Headache Society diagnostic criteria for migraine without aura include having symptoms of nausea and/or hypersensitivity to light or sound. This patient also described symptoms typical of the prodromal phase of migraine, which include yawning, temperature control, excessive thirst, and mood swings.
Patients who have migraine with aura also have unilateral headache pain of several hours' duration but experience visual (eg, dots or flashes) or sensory (prickly sensation on skin) symptoms, or may have brief difficulty with speech or motor function. These aura symptoms generally last 5 to 60 minutes before abating.
The worldwide impact of migraine potentially reaches a billion individuals. Its prevalence is second only to tension-type headaches. Migraine occurs in patients of all ages and affects women at a rate two to three times higher than in men. Prevalence appears to peak in the third and fourth decades of life and tends to be lower among older adults. Migraine also has a negative effect on patients' work, school, or social lives, and is associated with increased rates of depression and anxiety in adults. For patients who are prone to migraines, potential triggers include some foods and beverages (including those that contain caffeine and alcohol), menstrual cycles in women, exposure to strobing or bright lights or loud sounds, stressful situations, extra physical activity, and too much or too little sleep.
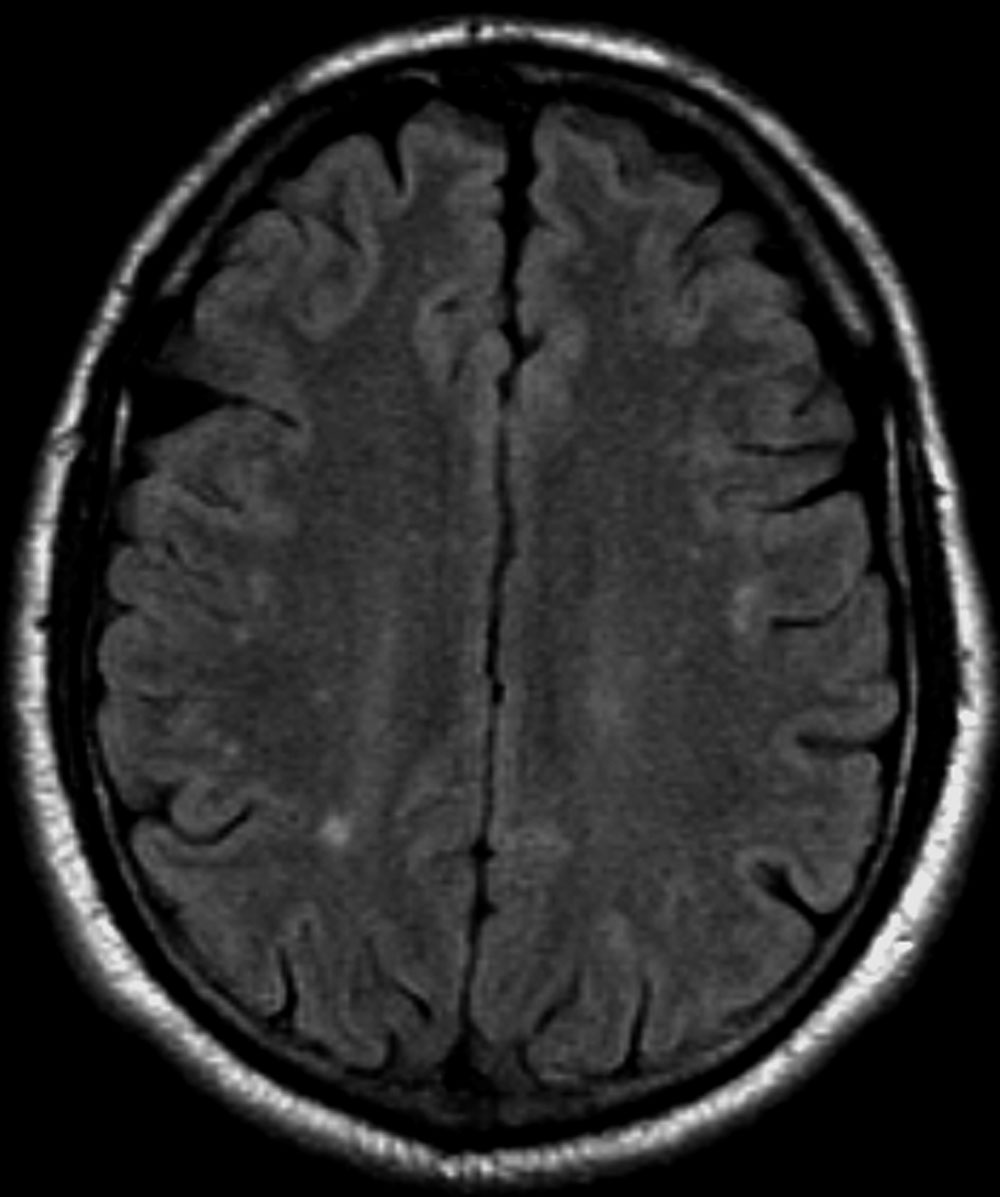
Migraine is a clinical diagnosis based on number of headaches (five or more episodes) plus two or more of the characteristic signs (unilateral, throbbing pain, pain intensity of ≥ 5 on a 10-point scale, and pain aggravated by routine physical motion, such as climbing stairs or bending over) plus nausea and/or photosensitivity or phonosensitivity. Prodrome symptoms are reported by about 70% of adult patients. Diagnosis rarely requires neuroimaging; however, before prescribing medication, a complete lab and metabolic workup should be done.
Management of migraine without aura includes acute and preventive interventions. Acute interventions cited by the American Headache Society include nonsteroidal anti-inflammatory drugs and acetaminophen for mild pain, and migraine-specific therapies such as the triptans, ergotamine derivatives, gepants (rimegepant, ubrogepant), and lasmiditan. Because response to any of these therapies will differ among patients with migraine, shared decision-making with patients about benefits and potential side effects is necessary and should include flexibility to change therapy if needed.
Preventive therapy should be offered to patients experiencing six or more migraines a month (regardless of impairment) and those, like this patient, with three or more migraines a month that significantly impair daily activities. Preventive therapy can be considered for those with fewer monthly episodes, depending on the degree of impairment. Oral preventive therapies with established efficacy include candesartan, certain beta-blockers, topiramate, and valproate. Parenteral monoclonal antibodies that inhibit calcitonin gene-related peptide activity (eptinezumab, erenumab, fremanezumab, and galcanezumab) and onabotulinumtoxinA may be considered if oral therapies provide inadequate prevention.
Tension-type headache is the most common form of primary headache. These headaches are bilateral and characterized by a pressing or dull sensation that is often mild in intensity. They are different from migraine in that they occur infrequently, lack sensory symptoms, and generally are of shorter duration (30 minutes to 24 hours). Fasting-related headache is characterized by diffuse, nonpulsating pain and is relieved with food.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.

 Steven Needell / Science Source
Steven Needell / Science Source