User login
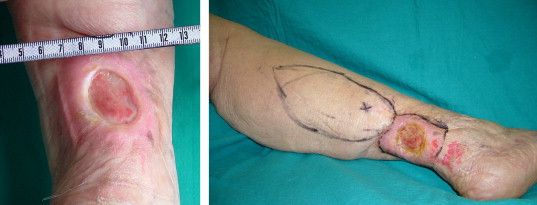
The use of topical timolol maleate as a treatment for chronic diabetic and chronic venous ulcers showed increased wound healing compared with controls, according to the results of a prospective observational study of 60 patients.
In the treatment group, 30 patients with chronic leg ulcer (15 diabetic ulcers; 15 venous) received topical application of 0.5% timolol maleate (a beta-blocker) plus conventional antibiotic and wound dressing therapy. In the control group, 30 patients (identical split between diabetic and venous ulcers) were treated with conventional therapy alone, according to a report published in the November issue of the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
The researchers found no significant difference in healing rates due to sex, between smokers and nonsmokers, or alcohol consumers vs. nonconsumers and they saw no major adverse effects due to timolol application (J Vasc Surg: Venous and Lym Dis 2017;5:844-50).
They reported that the limitations of their study included the lack of randomization and a formal power assessment.
“Topical application of timolol maleate is an effective therapeutic option for the treatment of chronic diabetic ulcer and chronic venous ulcer patients to improve ulcer healing by promoting keratinocyte migration,” the researchers concluded.
They reported having no relevant conflicts.
The use of topical timolol maleate as a treatment for chronic diabetic and chronic venous ulcers showed increased wound healing compared with controls, according to the results of a prospective observational study of 60 patients.
In the treatment group, 30 patients with chronic leg ulcer (15 diabetic ulcers; 15 venous) received topical application of 0.5% timolol maleate (a beta-blocker) plus conventional antibiotic and wound dressing therapy. In the control group, 30 patients (identical split between diabetic and venous ulcers) were treated with conventional therapy alone, according to a report published in the November issue of the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
The researchers found no significant difference in healing rates due to sex, between smokers and nonsmokers, or alcohol consumers vs. nonconsumers and they saw no major adverse effects due to timolol application (J Vasc Surg: Venous and Lym Dis 2017;5:844-50).
They reported that the limitations of their study included the lack of randomization and a formal power assessment.
“Topical application of timolol maleate is an effective therapeutic option for the treatment of chronic diabetic ulcer and chronic venous ulcer patients to improve ulcer healing by promoting keratinocyte migration,” the researchers concluded.
They reported having no relevant conflicts.
The use of topical timolol maleate as a treatment for chronic diabetic and chronic venous ulcers showed increased wound healing compared with controls, according to the results of a prospective observational study of 60 patients.
In the treatment group, 30 patients with chronic leg ulcer (15 diabetic ulcers; 15 venous) received topical application of 0.5% timolol maleate (a beta-blocker) plus conventional antibiotic and wound dressing therapy. In the control group, 30 patients (identical split between diabetic and venous ulcers) were treated with conventional therapy alone, according to a report published in the November issue of the Journal of Vascular Surgery: Venous and Lymphatic Disorders.
The researchers found no significant difference in healing rates due to sex, between smokers and nonsmokers, or alcohol consumers vs. nonconsumers and they saw no major adverse effects due to timolol application (J Vasc Surg: Venous and Lym Dis 2017;5:844-50).
They reported that the limitations of their study included the lack of randomization and a formal power assessment.
“Topical application of timolol maleate is an effective therapeutic option for the treatment of chronic diabetic ulcer and chronic venous ulcer patients to improve ulcer healing by promoting keratinocyte migration,” the researchers concluded.
They reported having no relevant conflicts.
FROM THE JOURNAL OF VASCULAR SURGERY: VENOUS AND LYMPHATIC DISORDERS