User login
The Case
A 62-year-old obese woman with prior history of type 2 diabetes, hypertension, and a pack-a-day smoking habit presented to the emergency department (ED) for acute onset of right-side weakness and sensory loss noted on awakening from sleep.
She reports taking a baby aspirin daily to “prevent heart attacks” prior to her stroke. Her electrocardiogram demonstrates a left bundle branch block and frequent premature atrial contractions. She recovers with mild hemiparesis and is ready for discharge. What is the best medical therapy for secondary prevention of stroke?
Overview
Cerebrovascular accident (CVA) represents an important diagnosis for the hospitalist, with 700,000 people suffering a stroke in the U.S. each year.1 This translates to a stroke every 45 seconds. About 200,000 of these strokes are recurrent events.
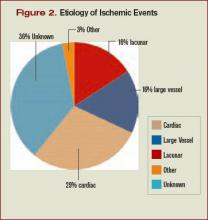
Cardioembolism is the largest cause of ischemic strokes, representing 29% of all infarcts.2 Stasis from impaired contractile function, atrial fibrillation, or mechanical valves are significant risk factors. More rarely, a paradoxical embolus arising in the venous system may pass through a patent foramen ovale.
Large-artery atherosclerosis and lacunar infarcts each account for 16% of strokes. Risk factors for these forms of strokes are the same as those for atherosclerosis and include hypertension and diabetes. Rarer causes such as vasculitis, dissection, hypercoagulability, or hematological disorders account for 3% of strokes. Work-up for these should be driven by historical and atypical features such as young age, family history, or unusual distribution of ischemic zones. Despite appropriate work-up, the mechanism remains uncertain in 36% of strokes.
Regardless of the manifestation and residua of the index event, the hospitalist must initiate appropriate therapy to prevent a disabling CVA. While antithrombotic drugs are the mainstay of secondary prevention, it is a mistake to miss other opportunities for risk modification. Optimal management requires a tailored evaluation for etiology, identification of modifiable risk factors, and initiation of antiplatelet or anticoagulant therapy.
Cardioembolic Stroke
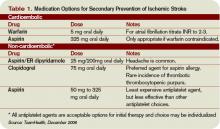
Treatment of stroke depends on the etiology of the original infarct. Evidence is strong that the optimal therapy for cardioembolic stroke is anticoagulation with warfarin.
The European Atrial Fibrillation Trial found that warfarin reduces the risk for second strokes in patients with atrial fibrillation by two-thirds and is superior to antiplatelet agents for preventing cardioembolic strokes.3 Warfarin increases the risk of extracranial bleeding, but not severely enough to negate the benefit of reducing stroke death and disability. The target international normalized ratio (INR) for non-valvular atrial fibrillation is generally two to three, although this may be higher for certain prosthetic valves.
Noncardioembolic Stroke
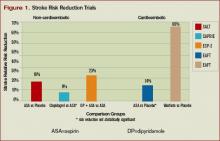
For large-vessel atherosclerotic and lacunar cerebral ischemia, the oldest—and still effective—treatment for recurrent stroke is aspirin. The use of low-dose aspirin after transient ischemic attack (TIA) or stroke reduces second strokes or death by approximately 15%-18%.4-5 Larger doses do not appear to be more effective, although the rate of gastrointestinal complaints is greater with increased dosage. The use of either 325 mg or 1,200 mg of aspirin produced the same 15% reduction in second ischemic events. Similar efficacy has been seen in comparisons between 30 mg and 283 mg dosing.6
While a subset of patients may experience aspirin resistance, reliable assays in clinical practice are not commonly available to guide management. Current recommendations suggest that use of between 50 mg and 325 mg of aspirin is appropriate for secondary prevention.7
Clopidogrel is another antiplatelet agent that can be given daily at 75 mg as alternate therapy for secondary prevention of non-cardioembolic stroke. The Clopidogrel versus Aspirin in Patients at Risk of Ischemic Events trial comparing clopidogrel with aspirin in patients at risk of ischemic events demonstrated significant reduction in the annual rate of combined endpoint of stroke, myocardial infarction, and vascular death—from 5.83% with aspirin to 5.32% with clopidogrel.8 This study’s applicability to secondary prevention of stroke is limited by the fact that only 19% of the patients in this trial were included because of prior stroke, and the results were not significant for reduction of stroke as a lone endpoint. Clopidogrel is recommended as an acceptable agent for CVA secondary prevention and is preferred for patients with stroke and an aspirin allergy or with recent coronary stent.
The combination of a low-dose aspirin and extended-release dipyridamole has proved superior to aspirin monotherapy in multiple trials. Over two years, the European Stroke Prevention 2 trial found an 18% reduction with aspirin alone compared with 37% reduction with the combination therapy, and the European/Australasian Stroke Prevention in Reversible Ischaemia trial confirmed that the combination reduced the absolute rate of second ischemic events by 1% annually.9-10 Headache is a common side effect of dipyridamole and may limit use. Dypridamole/aspirin is recommended as another acceptable option for secondary prevention of non-cardioembolic stroke.
Evidence suggests that aspirin/dipyridamole and clopidogrel—although significantly more expensive—are more effective than aspirin monotherapy for preventing second cerebral ischemic events. Direct comparison between aspirin/dipyridamole and clopidogrel is ongoing in the Prevention Regimen for Effectively Avoiding Second Stroke trial, with results anticipated in 2008.
Things That Don’t Work
The Warfarin-Aspirin Recurrent Stroke Study trial demonstrated that warfarin was not better than aspirin for prevention of non-cardioembolic stroke, and the Warfarin–Aspirin Symptomatic Intracranial Disease trial found the same result for patients with intracranial stenosis.11-12 There is little evidence that warfarin should have a role in the treatment of most non-cardioembolic strokes. The MATCH trial failed to show benefit to adding aspirin to clopidogrel over clopidogrel monotherapy for secondary preventions of non-cardioembolic cerebral ischemia.13 Despite efficacy following coronary stenting, the combination of clopidogrel and aspirin can not be recommended for stroke prevention.
What To Do
Aggressive risk factor modification is key in the prevention of second ischemic events. One of the most promising therapies is the use of statins following a CVA. Maintaining low-density lipoprotein (LDL) at less than 100 mg/dL (or less than 70 mg/dL in the highest-risk patients) is recommended despite a relatively weak association between stroke and hyperlipidemia.
This stands in contrast to the strong relationship between elevated LDL and coronary disease. However, the Stroke Prevention by Aggressive Reduction in Cholesterol Levels trial utilized high-dose atorvastatin after acute CVA and was able to create an absolute risk reduction for second stroke of 2.2% over the next five years.14 It is possible that the findings of this trial may reflect actions of statin therapy on the endothelium independent of the lipid lowering effect.
Blood pressure commonly has a transient elevation following cerebral ischemia. This is managed permissively to preserve perfusion to the ischemic penumbra. Once the hyperacute period is over, reduction of blood pressure to less than 140/90 mm/Hg (130/80 mm/Hg for diabetics) is recommended.
Interventions to treat chronic hypertension have been demonstrated to reduce the rate of strokes by approximately 30% to 40% over four to five years.15-16 An optimal agent has not been determined, but therapy with angiotensin converting enzyme inhibitor (ACE-I) or angiotensin II receptor blocker (ARB), possibly in combination with a diuretic, have been effective. Close follow-up for titration to goal in the outpatient setting should be arranged. Diabetics should have optimization of glycemic control, and lifestyle counseling should occur regarding recognized risk factors for stroke such as smoking, inactivity, and alcohol abuse.
While antithrombotic therapy is the mainstay of what we think of in secondary prevention of stroke, treatment of these other modifiable risk factors have been shown to affect mortality and second strokes of a similar magnitude and should not be neglected.
How to Treat This Case
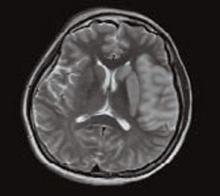
The patient described should undergo an MRI with diffusion (to define the area of ischemia) and targeted evaluation for etiology with cardiac monitoring, echocardiogram, and carotid ultrasound.
Assuming atrial fibrillation or intracardiac thrombus is ruled out, this likely represents atherosclerotic disease. MRI will help distinguish between large-vessel atherosclerotic etiology and lacunar infarct. If carotid stenosis of greater than 70% is found in the setting of large vessel atherosclerotic stroke, then she should be referred for carotid endarterectomy. At 50% to 69% stenosis, carotid endarterectomy would still be a consideration. Antithrombotic agent of choice for non-cardioembolic CVA is an anti-platelet agent. With a stroke occurring on a reasonable dose of aspirin, I would not recommend increasing the dose as there is little evidence that 325 mg is more effective than 81mg. The most appropriate step would be to change to an alternate anti-platelet agent such as combination dipyridamole/aspirin or clopidogrel.
In the absence of a direct comparison trial, either choice is acceptable. The evidence supporting dipyridamole/aspirin is stronger for secondary stroke prevention. Atorvastatin 80 mg daily is an evidence-based therapy after acute stroke and can be started immediately. Her hypertension should be managed permissively for the first few days after the acute event, but then an ACE-I or ARB—possibly in combination with a diuretic—would be appropriate. This patient’s goal blood pressure as a diabetic would be at least less than 130/80 mm/Hg.
Finally we would be remiss if we did not stress the importance of smoking cessation, exercise, and weight loss. TH
Dr. Cumbler is an assistant professor in the Section of Hospital Medicine at the University of Colorado, where he is a member of the Acute Stroke Service and serves on the Stroke Council.
References
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics-2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007 Feb 6;115(5):e69-e171.
- Petty GW, Brown RD, Whisnant JP, et al. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke. 1999;30:2513-2516.
- European Atrial Fibrillation Trial Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet. 1993;342:1255-1262.
- Swedish Aspirin Low-Dose Trial Collaborative Group. Swedish aspirin low-dose aspirin trial (SALT) of 775 mg aspirin as secondary prophylaxis after cerebrovascular ischaemic events. Lancet. 1991;338(8779):1345-1349.
- Farrell B, Godwin J, Richards S, et al. The United Kingdom Transient Ischaemic Attack (UK-TIA) aspirin trial: final results (abstract). J Neurol Neurosurg. Psychiatry 1991;54:1044-1054.
- Dutch TIA Trial Study Group. A comparison of two doses of aspirin (30 mg versus 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med. 1991 Oct 31;325(18):1261-1266.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack. Stroke. 2006 Feb;37(2):577-617.
- CAPRIE Steering Committee. A randomized, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events. Lancet 1996 Jan;348:1329-1339.
- Diener H, Cunha L, Forbes C, et al. European stroke prevention study 2: dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996;143:1-13.
- ESPRIT Study Group. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet. 2006;367:1665-1673.
- Mohr JP, Thompson JLP, Lazar RM, et al. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001 Nov 15; 345(20):1444-1451.
- Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005 Mar 31;352(13):1305-1316.
- Diener HC, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo controlled trial. Lancet. 2004 Jul 24-30;36499431):331-337.
- Stroke Prevention by Aggressive Reduction in Cholesterol Levels Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355(6):549-559.
- The PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 2001;358(9287):1033-1041.
- The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000 Jan 20;342:145-153.
The Case
A 62-year-old obese woman with prior history of type 2 diabetes, hypertension, and a pack-a-day smoking habit presented to the emergency department (ED) for acute onset of right-side weakness and sensory loss noted on awakening from sleep.
She reports taking a baby aspirin daily to “prevent heart attacks” prior to her stroke. Her electrocardiogram demonstrates a left bundle branch block and frequent premature atrial contractions. She recovers with mild hemiparesis and is ready for discharge. What is the best medical therapy for secondary prevention of stroke?
Overview
Cerebrovascular accident (CVA) represents an important diagnosis for the hospitalist, with 700,000 people suffering a stroke in the U.S. each year.1 This translates to a stroke every 45 seconds. About 200,000 of these strokes are recurrent events.
Cardioembolism is the largest cause of ischemic strokes, representing 29% of all infarcts.2 Stasis from impaired contractile function, atrial fibrillation, or mechanical valves are significant risk factors. More rarely, a paradoxical embolus arising in the venous system may pass through a patent foramen ovale.
Large-artery atherosclerosis and lacunar infarcts each account for 16% of strokes. Risk factors for these forms of strokes are the same as those for atherosclerosis and include hypertension and diabetes. Rarer causes such as vasculitis, dissection, hypercoagulability, or hematological disorders account for 3% of strokes. Work-up for these should be driven by historical and atypical features such as young age, family history, or unusual distribution of ischemic zones. Despite appropriate work-up, the mechanism remains uncertain in 36% of strokes.
Regardless of the manifestation and residua of the index event, the hospitalist must initiate appropriate therapy to prevent a disabling CVA. While antithrombotic drugs are the mainstay of secondary prevention, it is a mistake to miss other opportunities for risk modification. Optimal management requires a tailored evaluation for etiology, identification of modifiable risk factors, and initiation of antiplatelet or anticoagulant therapy.
Cardioembolic Stroke
Treatment of stroke depends on the etiology of the original infarct. Evidence is strong that the optimal therapy for cardioembolic stroke is anticoagulation with warfarin.
The European Atrial Fibrillation Trial found that warfarin reduces the risk for second strokes in patients with atrial fibrillation by two-thirds and is superior to antiplatelet agents for preventing cardioembolic strokes.3 Warfarin increases the risk of extracranial bleeding, but not severely enough to negate the benefit of reducing stroke death and disability. The target international normalized ratio (INR) for non-valvular atrial fibrillation is generally two to three, although this may be higher for certain prosthetic valves.
Noncardioembolic Stroke
For large-vessel atherosclerotic and lacunar cerebral ischemia, the oldest—and still effective—treatment for recurrent stroke is aspirin. The use of low-dose aspirin after transient ischemic attack (TIA) or stroke reduces second strokes or death by approximately 15%-18%.4-5 Larger doses do not appear to be more effective, although the rate of gastrointestinal complaints is greater with increased dosage. The use of either 325 mg or 1,200 mg of aspirin produced the same 15% reduction in second ischemic events. Similar efficacy has been seen in comparisons between 30 mg and 283 mg dosing.6
While a subset of patients may experience aspirin resistance, reliable assays in clinical practice are not commonly available to guide management. Current recommendations suggest that use of between 50 mg and 325 mg of aspirin is appropriate for secondary prevention.7
Clopidogrel is another antiplatelet agent that can be given daily at 75 mg as alternate therapy for secondary prevention of non-cardioembolic stroke. The Clopidogrel versus Aspirin in Patients at Risk of Ischemic Events trial comparing clopidogrel with aspirin in patients at risk of ischemic events demonstrated significant reduction in the annual rate of combined endpoint of stroke, myocardial infarction, and vascular death—from 5.83% with aspirin to 5.32% with clopidogrel.8 This study’s applicability to secondary prevention of stroke is limited by the fact that only 19% of the patients in this trial were included because of prior stroke, and the results were not significant for reduction of stroke as a lone endpoint. Clopidogrel is recommended as an acceptable agent for CVA secondary prevention and is preferred for patients with stroke and an aspirin allergy or with recent coronary stent.
The combination of a low-dose aspirin and extended-release dipyridamole has proved superior to aspirin monotherapy in multiple trials. Over two years, the European Stroke Prevention 2 trial found an 18% reduction with aspirin alone compared with 37% reduction with the combination therapy, and the European/Australasian Stroke Prevention in Reversible Ischaemia trial confirmed that the combination reduced the absolute rate of second ischemic events by 1% annually.9-10 Headache is a common side effect of dipyridamole and may limit use. Dypridamole/aspirin is recommended as another acceptable option for secondary prevention of non-cardioembolic stroke.
Evidence suggests that aspirin/dipyridamole and clopidogrel—although significantly more expensive—are more effective than aspirin monotherapy for preventing second cerebral ischemic events. Direct comparison between aspirin/dipyridamole and clopidogrel is ongoing in the Prevention Regimen for Effectively Avoiding Second Stroke trial, with results anticipated in 2008.
Things That Don’t Work
The Warfarin-Aspirin Recurrent Stroke Study trial demonstrated that warfarin was not better than aspirin for prevention of non-cardioembolic stroke, and the Warfarin–Aspirin Symptomatic Intracranial Disease trial found the same result for patients with intracranial stenosis.11-12 There is little evidence that warfarin should have a role in the treatment of most non-cardioembolic strokes. The MATCH trial failed to show benefit to adding aspirin to clopidogrel over clopidogrel monotherapy for secondary preventions of non-cardioembolic cerebral ischemia.13 Despite efficacy following coronary stenting, the combination of clopidogrel and aspirin can not be recommended for stroke prevention.
What To Do
Aggressive risk factor modification is key in the prevention of second ischemic events. One of the most promising therapies is the use of statins following a CVA. Maintaining low-density lipoprotein (LDL) at less than 100 mg/dL (or less than 70 mg/dL in the highest-risk patients) is recommended despite a relatively weak association between stroke and hyperlipidemia.
This stands in contrast to the strong relationship between elevated LDL and coronary disease. However, the Stroke Prevention by Aggressive Reduction in Cholesterol Levels trial utilized high-dose atorvastatin after acute CVA and was able to create an absolute risk reduction for second stroke of 2.2% over the next five years.14 It is possible that the findings of this trial may reflect actions of statin therapy on the endothelium independent of the lipid lowering effect.
Blood pressure commonly has a transient elevation following cerebral ischemia. This is managed permissively to preserve perfusion to the ischemic penumbra. Once the hyperacute period is over, reduction of blood pressure to less than 140/90 mm/Hg (130/80 mm/Hg for diabetics) is recommended.
Interventions to treat chronic hypertension have been demonstrated to reduce the rate of strokes by approximately 30% to 40% over four to five years.15-16 An optimal agent has not been determined, but therapy with angiotensin converting enzyme inhibitor (ACE-I) or angiotensin II receptor blocker (ARB), possibly in combination with a diuretic, have been effective. Close follow-up for titration to goal in the outpatient setting should be arranged. Diabetics should have optimization of glycemic control, and lifestyle counseling should occur regarding recognized risk factors for stroke such as smoking, inactivity, and alcohol abuse.
While antithrombotic therapy is the mainstay of what we think of in secondary prevention of stroke, treatment of these other modifiable risk factors have been shown to affect mortality and second strokes of a similar magnitude and should not be neglected.
How to Treat This Case
The patient described should undergo an MRI with diffusion (to define the area of ischemia) and targeted evaluation for etiology with cardiac monitoring, echocardiogram, and carotid ultrasound.
Assuming atrial fibrillation or intracardiac thrombus is ruled out, this likely represents atherosclerotic disease. MRI will help distinguish between large-vessel atherosclerotic etiology and lacunar infarct. If carotid stenosis of greater than 70% is found in the setting of large vessel atherosclerotic stroke, then she should be referred for carotid endarterectomy. At 50% to 69% stenosis, carotid endarterectomy would still be a consideration. Antithrombotic agent of choice for non-cardioembolic CVA is an anti-platelet agent. With a stroke occurring on a reasonable dose of aspirin, I would not recommend increasing the dose as there is little evidence that 325 mg is more effective than 81mg. The most appropriate step would be to change to an alternate anti-platelet agent such as combination dipyridamole/aspirin or clopidogrel.
In the absence of a direct comparison trial, either choice is acceptable. The evidence supporting dipyridamole/aspirin is stronger for secondary stroke prevention. Atorvastatin 80 mg daily is an evidence-based therapy after acute stroke and can be started immediately. Her hypertension should be managed permissively for the first few days after the acute event, but then an ACE-I or ARB—possibly in combination with a diuretic—would be appropriate. This patient’s goal blood pressure as a diabetic would be at least less than 130/80 mm/Hg.
Finally we would be remiss if we did not stress the importance of smoking cessation, exercise, and weight loss. TH
Dr. Cumbler is an assistant professor in the Section of Hospital Medicine at the University of Colorado, where he is a member of the Acute Stroke Service and serves on the Stroke Council.
References
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics-2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007 Feb 6;115(5):e69-e171.
- Petty GW, Brown RD, Whisnant JP, et al. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke. 1999;30:2513-2516.
- European Atrial Fibrillation Trial Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet. 1993;342:1255-1262.
- Swedish Aspirin Low-Dose Trial Collaborative Group. Swedish aspirin low-dose aspirin trial (SALT) of 775 mg aspirin as secondary prophylaxis after cerebrovascular ischaemic events. Lancet. 1991;338(8779):1345-1349.
- Farrell B, Godwin J, Richards S, et al. The United Kingdom Transient Ischaemic Attack (UK-TIA) aspirin trial: final results (abstract). J Neurol Neurosurg. Psychiatry 1991;54:1044-1054.
- Dutch TIA Trial Study Group. A comparison of two doses of aspirin (30 mg versus 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med. 1991 Oct 31;325(18):1261-1266.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack. Stroke. 2006 Feb;37(2):577-617.
- CAPRIE Steering Committee. A randomized, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events. Lancet 1996 Jan;348:1329-1339.
- Diener H, Cunha L, Forbes C, et al. European stroke prevention study 2: dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996;143:1-13.
- ESPRIT Study Group. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet. 2006;367:1665-1673.
- Mohr JP, Thompson JLP, Lazar RM, et al. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001 Nov 15; 345(20):1444-1451.
- Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005 Mar 31;352(13):1305-1316.
- Diener HC, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo controlled trial. Lancet. 2004 Jul 24-30;36499431):331-337.
- Stroke Prevention by Aggressive Reduction in Cholesterol Levels Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355(6):549-559.
- The PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 2001;358(9287):1033-1041.
- The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000 Jan 20;342:145-153.
The Case
A 62-year-old obese woman with prior history of type 2 diabetes, hypertension, and a pack-a-day smoking habit presented to the emergency department (ED) for acute onset of right-side weakness and sensory loss noted on awakening from sleep.
She reports taking a baby aspirin daily to “prevent heart attacks” prior to her stroke. Her electrocardiogram demonstrates a left bundle branch block and frequent premature atrial contractions. She recovers with mild hemiparesis and is ready for discharge. What is the best medical therapy for secondary prevention of stroke?
Overview
Cerebrovascular accident (CVA) represents an important diagnosis for the hospitalist, with 700,000 people suffering a stroke in the U.S. each year.1 This translates to a stroke every 45 seconds. About 200,000 of these strokes are recurrent events.
Cardioembolism is the largest cause of ischemic strokes, representing 29% of all infarcts.2 Stasis from impaired contractile function, atrial fibrillation, or mechanical valves are significant risk factors. More rarely, a paradoxical embolus arising in the venous system may pass through a patent foramen ovale.
Large-artery atherosclerosis and lacunar infarcts each account for 16% of strokes. Risk factors for these forms of strokes are the same as those for atherosclerosis and include hypertension and diabetes. Rarer causes such as vasculitis, dissection, hypercoagulability, or hematological disorders account for 3% of strokes. Work-up for these should be driven by historical and atypical features such as young age, family history, or unusual distribution of ischemic zones. Despite appropriate work-up, the mechanism remains uncertain in 36% of strokes.
Regardless of the manifestation and residua of the index event, the hospitalist must initiate appropriate therapy to prevent a disabling CVA. While antithrombotic drugs are the mainstay of secondary prevention, it is a mistake to miss other opportunities for risk modification. Optimal management requires a tailored evaluation for etiology, identification of modifiable risk factors, and initiation of antiplatelet or anticoagulant therapy.
Cardioembolic Stroke
Treatment of stroke depends on the etiology of the original infarct. Evidence is strong that the optimal therapy for cardioembolic stroke is anticoagulation with warfarin.
The European Atrial Fibrillation Trial found that warfarin reduces the risk for second strokes in patients with atrial fibrillation by two-thirds and is superior to antiplatelet agents for preventing cardioembolic strokes.3 Warfarin increases the risk of extracranial bleeding, but not severely enough to negate the benefit of reducing stroke death and disability. The target international normalized ratio (INR) for non-valvular atrial fibrillation is generally two to three, although this may be higher for certain prosthetic valves.
Noncardioembolic Stroke
For large-vessel atherosclerotic and lacunar cerebral ischemia, the oldest—and still effective—treatment for recurrent stroke is aspirin. The use of low-dose aspirin after transient ischemic attack (TIA) or stroke reduces second strokes or death by approximately 15%-18%.4-5 Larger doses do not appear to be more effective, although the rate of gastrointestinal complaints is greater with increased dosage. The use of either 325 mg or 1,200 mg of aspirin produced the same 15% reduction in second ischemic events. Similar efficacy has been seen in comparisons between 30 mg and 283 mg dosing.6
While a subset of patients may experience aspirin resistance, reliable assays in clinical practice are not commonly available to guide management. Current recommendations suggest that use of between 50 mg and 325 mg of aspirin is appropriate for secondary prevention.7
Clopidogrel is another antiplatelet agent that can be given daily at 75 mg as alternate therapy for secondary prevention of non-cardioembolic stroke. The Clopidogrel versus Aspirin in Patients at Risk of Ischemic Events trial comparing clopidogrel with aspirin in patients at risk of ischemic events demonstrated significant reduction in the annual rate of combined endpoint of stroke, myocardial infarction, and vascular death—from 5.83% with aspirin to 5.32% with clopidogrel.8 This study’s applicability to secondary prevention of stroke is limited by the fact that only 19% of the patients in this trial were included because of prior stroke, and the results were not significant for reduction of stroke as a lone endpoint. Clopidogrel is recommended as an acceptable agent for CVA secondary prevention and is preferred for patients with stroke and an aspirin allergy or with recent coronary stent.
The combination of a low-dose aspirin and extended-release dipyridamole has proved superior to aspirin monotherapy in multiple trials. Over two years, the European Stroke Prevention 2 trial found an 18% reduction with aspirin alone compared with 37% reduction with the combination therapy, and the European/Australasian Stroke Prevention in Reversible Ischaemia trial confirmed that the combination reduced the absolute rate of second ischemic events by 1% annually.9-10 Headache is a common side effect of dipyridamole and may limit use. Dypridamole/aspirin is recommended as another acceptable option for secondary prevention of non-cardioembolic stroke.
Evidence suggests that aspirin/dipyridamole and clopidogrel—although significantly more expensive—are more effective than aspirin monotherapy for preventing second cerebral ischemic events. Direct comparison between aspirin/dipyridamole and clopidogrel is ongoing in the Prevention Regimen for Effectively Avoiding Second Stroke trial, with results anticipated in 2008.
Things That Don’t Work
The Warfarin-Aspirin Recurrent Stroke Study trial demonstrated that warfarin was not better than aspirin for prevention of non-cardioembolic stroke, and the Warfarin–Aspirin Symptomatic Intracranial Disease trial found the same result for patients with intracranial stenosis.11-12 There is little evidence that warfarin should have a role in the treatment of most non-cardioembolic strokes. The MATCH trial failed to show benefit to adding aspirin to clopidogrel over clopidogrel monotherapy for secondary preventions of non-cardioembolic cerebral ischemia.13 Despite efficacy following coronary stenting, the combination of clopidogrel and aspirin can not be recommended for stroke prevention.
What To Do
Aggressive risk factor modification is key in the prevention of second ischemic events. One of the most promising therapies is the use of statins following a CVA. Maintaining low-density lipoprotein (LDL) at less than 100 mg/dL (or less than 70 mg/dL in the highest-risk patients) is recommended despite a relatively weak association between stroke and hyperlipidemia.
This stands in contrast to the strong relationship between elevated LDL and coronary disease. However, the Stroke Prevention by Aggressive Reduction in Cholesterol Levels trial utilized high-dose atorvastatin after acute CVA and was able to create an absolute risk reduction for second stroke of 2.2% over the next five years.14 It is possible that the findings of this trial may reflect actions of statin therapy on the endothelium independent of the lipid lowering effect.
Blood pressure commonly has a transient elevation following cerebral ischemia. This is managed permissively to preserve perfusion to the ischemic penumbra. Once the hyperacute period is over, reduction of blood pressure to less than 140/90 mm/Hg (130/80 mm/Hg for diabetics) is recommended.
Interventions to treat chronic hypertension have been demonstrated to reduce the rate of strokes by approximately 30% to 40% over four to five years.15-16 An optimal agent has not been determined, but therapy with angiotensin converting enzyme inhibitor (ACE-I) or angiotensin II receptor blocker (ARB), possibly in combination with a diuretic, have been effective. Close follow-up for titration to goal in the outpatient setting should be arranged. Diabetics should have optimization of glycemic control, and lifestyle counseling should occur regarding recognized risk factors for stroke such as smoking, inactivity, and alcohol abuse.
While antithrombotic therapy is the mainstay of what we think of in secondary prevention of stroke, treatment of these other modifiable risk factors have been shown to affect mortality and second strokes of a similar magnitude and should not be neglected.
How to Treat This Case
The patient described should undergo an MRI with diffusion (to define the area of ischemia) and targeted evaluation for etiology with cardiac monitoring, echocardiogram, and carotid ultrasound.
Assuming atrial fibrillation or intracardiac thrombus is ruled out, this likely represents atherosclerotic disease. MRI will help distinguish between large-vessel atherosclerotic etiology and lacunar infarct. If carotid stenosis of greater than 70% is found in the setting of large vessel atherosclerotic stroke, then she should be referred for carotid endarterectomy. At 50% to 69% stenosis, carotid endarterectomy would still be a consideration. Antithrombotic agent of choice for non-cardioembolic CVA is an anti-platelet agent. With a stroke occurring on a reasonable dose of aspirin, I would not recommend increasing the dose as there is little evidence that 325 mg is more effective than 81mg. The most appropriate step would be to change to an alternate anti-platelet agent such as combination dipyridamole/aspirin or clopidogrel.
In the absence of a direct comparison trial, either choice is acceptable. The evidence supporting dipyridamole/aspirin is stronger for secondary stroke prevention. Atorvastatin 80 mg daily is an evidence-based therapy after acute stroke and can be started immediately. Her hypertension should be managed permissively for the first few days after the acute event, but then an ACE-I or ARB—possibly in combination with a diuretic—would be appropriate. This patient’s goal blood pressure as a diabetic would be at least less than 130/80 mm/Hg.
Finally we would be remiss if we did not stress the importance of smoking cessation, exercise, and weight loss. TH
Dr. Cumbler is an assistant professor in the Section of Hospital Medicine at the University of Colorado, where he is a member of the Acute Stroke Service and serves on the Stroke Council.
References
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics-2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007 Feb 6;115(5):e69-e171.
- Petty GW, Brown RD, Whisnant JP, et al. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke. 1999;30:2513-2516.
- European Atrial Fibrillation Trial Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet. 1993;342:1255-1262.
- Swedish Aspirin Low-Dose Trial Collaborative Group. Swedish aspirin low-dose aspirin trial (SALT) of 775 mg aspirin as secondary prophylaxis after cerebrovascular ischaemic events. Lancet. 1991;338(8779):1345-1349.
- Farrell B, Godwin J, Richards S, et al. The United Kingdom Transient Ischaemic Attack (UK-TIA) aspirin trial: final results (abstract). J Neurol Neurosurg. Psychiatry 1991;54:1044-1054.
- Dutch TIA Trial Study Group. A comparison of two doses of aspirin (30 mg versus 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med. 1991 Oct 31;325(18):1261-1266.
- Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack. Stroke. 2006 Feb;37(2):577-617.
- CAPRIE Steering Committee. A randomized, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events. Lancet 1996 Jan;348:1329-1339.
- Diener H, Cunha L, Forbes C, et al. European stroke prevention study 2: dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996;143:1-13.
- ESPRIT Study Group. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet. 2006;367:1665-1673.
- Mohr JP, Thompson JLP, Lazar RM, et al. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001 Nov 15; 345(20):1444-1451.
- Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005 Mar 31;352(13):1305-1316.
- Diener HC, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo controlled trial. Lancet. 2004 Jul 24-30;36499431):331-337.
- Stroke Prevention by Aggressive Reduction in Cholesterol Levels Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355(6):549-559.
- The PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 2001;358(9287):1033-1041.
- The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000 Jan 20;342:145-153.