Decreasing the burden of treating skin and soft tissue infections is critical to improving care and reducing the costs that SSTIs place on health care facilities, according to a study published in Hospital Practice.
“Despite expert panel recommendations and treatment guidelines, there is no widely accepted classification system for grading SSTIs to outcomes,” wrote the study’s lead author, Kristin E. Linder, PharmD, of Hartford (Conn.) Hospital. “This leads to a considerable variation in treatment approach on initial presentation when deciding which patients should be admitted to receive intravenous (IV) antibiotic therapy or treated as outpatients.”
Dr. Linder and her coinvestigators conducted a single-center retrospective cohort study with the primary objective of determining rates of admission and re-presentation, along with average length-of-stay (LOS) and cost of care for both inpatients and outpatients with SSTIs. Patients aged 18 years and older who received a primary diagnosis of an SSTI during May and June of 2015 at Hartford Hospital were screened; 446 were deemed eligible, with 357 ultimately selected for inclusion (Hosp Pract. 2017 Jan 5. doi: 10.1080/21548331.2017.1279519).
Of the 357 patients included for analysis, 106 (29.7%) were admitted as inpatients while the remaining 251 (70.3%) were treated as outpatients. However, there were no significant differences found in re-presentation rates, either overall – 22.6% for inpatients and 28.3% for outpatients (P greater than .05) – or for SSTI-related re-presentation: 10.4% for inpatients and 15.1% for outpatients (P greater than .05). For those patients who did get admitted, mean LOS was 7.3 days.
Patients who presented with a Charlson Comorbidity Index (CCI) score of zero were admitted at a rate of 14.1%, compared to 30.1% of those with a CCI score of one, and 60.9% of those with a CCI score of two or higher. The biggest disparity, however, was in terms of cost of care; while outpatient care cost an average of $413 per patient, inpatient care cost an average of $13,313 per patient.
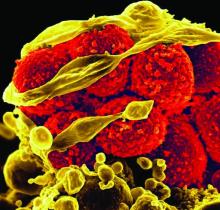
Wound and abscess cultures that were tested found methicillin-susceptible Staphylococcus aureus (MSSA) to be the most prevalent gram-positive organism (37.1%) found in inpatients, while for outpatients, methicillin-resistant S. aureus (MRSA) was the most common (66.7%). According to the investigators, Gram-negative bacteria were not isolated in every case, so “prevalent use of combination therapy in this setting may not be warranted.
“Understanding how and where patients with SSTI are treated and their re-presentation rate is important to understand to direct resources for this high frequency disease,” the authors concluded. “This study demonstrated that approximately 70% of patients presenting to the ED with SSTI were treated as outpatients [and] while 30-day re-presentation was similar for inpatient and outpatients, readmission was more likely in those previously admitted.”
This study was not funded, according to the authors. Dr. Linder did not report any relevant financial disclosures, but her coauthors disclosed receiving speakers’ and consultants’ fees from Astellas, Theravance. Bayer, Merck and Pfizer.