ROME - Adults with rheumatoid arthritis have a 65% higher rate of incident myocardial infarctions than does the general population, according to Danish data that strengthen the already significant evidence supporting a link between rheumatoid arthritis and elevated cardiovascular disease.
In addition, the new findings again showed that the heightened MI risk of RA patients matched the MI risk of patients with diabetes, Dr. Jesper Lindhardsen said at the annual European Congress of Rheumatology.
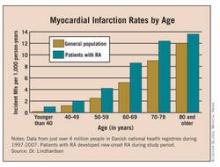
The new results also showed that the MI risk for RA patients at any age throughout adult life roughly matched the risk of a person without RA or diabetes who is 10 years older.
“An increased focus on the increased cardiovascular risk in patients with RA is warranted,” said Dr. Lindhardsen, a physician in the department of cardiology at Gentofte Hospital, Hellerup, Denmark. The attention paid to cardiovascular risk in RA patients should at least match the attention paid in diabetes patients, he added.
At last year’s European Congress of Rheumatology, a report from a task force convened by the European League Against Rheumatism declared that “rheumatoid arthritis should be regarded as a condition that is associated with higher risk for cardiovascular disease.” The report also spelled out 10 recommendations for cardiovascular disease risk management in RA patients. The report appeared in published form earlier this year (Ann. Rheum. Dis. 2010;69:325-1400).
The new findings by Dr. Lindhardsen and his associates took the prior evidence a step further by including RA patients with no prior diagnosis of cardiovascular disease, he said. The new study also provided a direct comparison of the risks conferred by RA and diabetes within the same background population, the entire Danish adult population during 1997-2007.
Dr. Lindhardsen and his associates used Danish national registry data during that period, a group of slightly more than 4 million people. During the decade studied, 10,547 adult Danes had newly diagnosed RA, and 132,868 had newly diagnosed diabetes, including both type 1 and type 2. The average age of those who developed RA was 56 years, and of those who developed diabetes it was 57 years, compared with an average age for everyone else of 46. Women constituted 71% of the incident RA cases, 46% of the incident diabetes cases, and 52% of the remaining population.
The researchers then tracked the rate of incident MIs in all three groups, with an average follow-up of 9 years in the general population, and 4 years following both the RA and diabetes diagnoses.
Compared with the rate of new-onset MI in the general population, RA patients had a 65% higher rate and patients with diabetes had a 73% higher rate, both statistically significant increases over the comparator group. This analysis adjusted for age, gender, cardiovascular pharmacotherapy, comorbidities, and socioeconomic status. About 400 people developed both RA and diabetes during the study period, and while their MI incidence was not additive, it significantly surpassed the rate among patients who had only RA or only diabetes, Dr. Lindhardsen said.
The analyses also provided insights into the interaction of age and gender with MI risk among RA patients. In general, the results showed that RA boosted MI risk regardless of age and gender. Among women younger than 50 years, RA and diabetes each boosted the MI risk sixfold, compared with similarly aged women without RA or diabetes. The impact on MI risk from either RA or diabetes fell substantially in women aged 50-65 years, and in women older than 65 years, although both RA and diabetes elevated the risk in both of these age groups. In men younger than 50 years, RA did not significantly raise MI risk but diabetes did. The biggest impact of RA on MI risk occurred in men aged 50-65, who had a twofold increased MI risk, compared with men who did not have RA or diabetes.
In another analysis that stratified all people studied by age, RA consistently boosted the MI rate across all age ranges, starting in people younger than 40 through those older than 80 (see chart above). This analysis showed that the presence of RA produced a MI rate roughly comparable to people who were 10 years older.