Monterey, Calif. - If there is a doppelganger in dermatology, malignant fibrous histiocytoma is it, according to Dr. Henry W. Randle at a meeting of the American Society for Mohs Surgery.
By immunohistochemistry, MFH is a dead ringer for atypical fibroxanthoma (AFX). Compared with rare mortality from AFX, however, approximately 38% of patients with MFH die within 3.5 years, said Dr. Randle.
Histologically, we can’t tell them apart. They look the same, but they behave very differently,” and require different treatment approaches, said Dr. Randle of the Mayo Clinic, Jacksonville, Fla.
The two main treatments for AFX are excision with a 1- to 2-cm margin that includes subcutaneous tissue or Mohs surgery.
For MFH, treatment involves tumor staging and wide excision to several centimeters, with consideration of node dissection, radiation, and chemotherapy. Mohs surgery is not the best option. “You’re brave if you do that” for MFH, he said. “This is a different animal.”
The problem lies in telling the two apart. Even the histologic diagnosis of AFX can be challenging, because no specific marker or test exists to identify AFX. Diagnosis requires excluding spindle cell squamous cell carcinomas, melanomas of the spindle cells, and other spindle cell malignancies.
The only identifiable characteristics that separate the relatively innocuous AFX from the more lethal MFH are the more superficial location of AFX and the fact that AFX typically appears on the head and neck, whereas MFH more typically occurs on the extremities and trunk, but not on the face.
A recent retrospective series of 89 patients with a histologic diagnosis of AFX claimed that no patients developed metastases, but that was because the authors decided not to include three cases with metastases because they acted differently from the other 86, Dr. Randle noted (Derm. Surg. 2009;35:765-772). Had the authors included those three cases, the metastases rate would be 3%.
“It is this small subset that is the problem,” he said.
Dr. Randle reserves the term AFX for small tumors that are less than 1.5 cm in diameter, that are based in the dermis and do not extend into the fat, and that occur in sun-damaged skin with no more than minimal involvement of the subcutis. Any diagnosis of AFX that did not analyze subcutaneous tissue with some fat has the potential for regional or distant spread, and may not be AFX, he said.
Consider the tumor to be MFH or another spindle cell tumor if it extends into the subcutis, shows vascular invasion, or has tumor necrosis, which does not occur with AFX. “I do not do Mohs if it has these features,” Dr. Randle said.
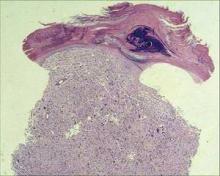
Visually, AFX usually looks like a rapidly growing red nodule, often ulcerated, on the sun-damaged head or neck skin of an elderly patient. It is twice as common in men as in women. Histologically, it’s a nonencapsulated cellular tumor, contiguous with the epidermis, with pleomorphic and atypical cells. It often has spindle-shaped cells with prominent, vesicular nuclei.
Reported recurrence rates range from 7% to 12% depending on the type of surgical treatment. Rare metastases in the regional node typically come from large, deep, recurrent tumors that are inadequately excised. In Dr. Randle’s personal experience with 56 AFX tumors in the past 20 years, 4 recurred (7%), one with metastasis. For MFH, the reported recurrence rate is 43%, he added.
Patients who have undergone organ transplants have higher prevalences of both AFX and MFH.
Disclosures: Dr. Randle reported having no relevant conflicts of interest.