according to data from 50 patients at a single tertiary care center.
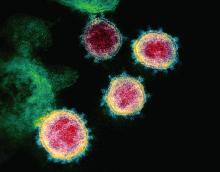
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.