NEW YORK – .
The program was founded in 2013 by two Harvard Medical School dermatologists, Lilit Garibyan, MD, PhD, the program director, and her mentor R. Rox Anderson MD, director of the Wellman Center for Photomedicine at Massachusetts General Hospital (MGH), Boston. It was based on the idea that clinicians are in a unique position to identify gaps in patient care and should be active in developing medical solutions to address those gaps.
“I truly believe that if we do a better job educating, training, and empowering our clinicians to become innovators, this will benefit patients and hospitals and physicians,” Dr. Garibyan said at the 26th annual Mount Sinai Winter Symposium — Advances in Medical and Surgical Dermatology.
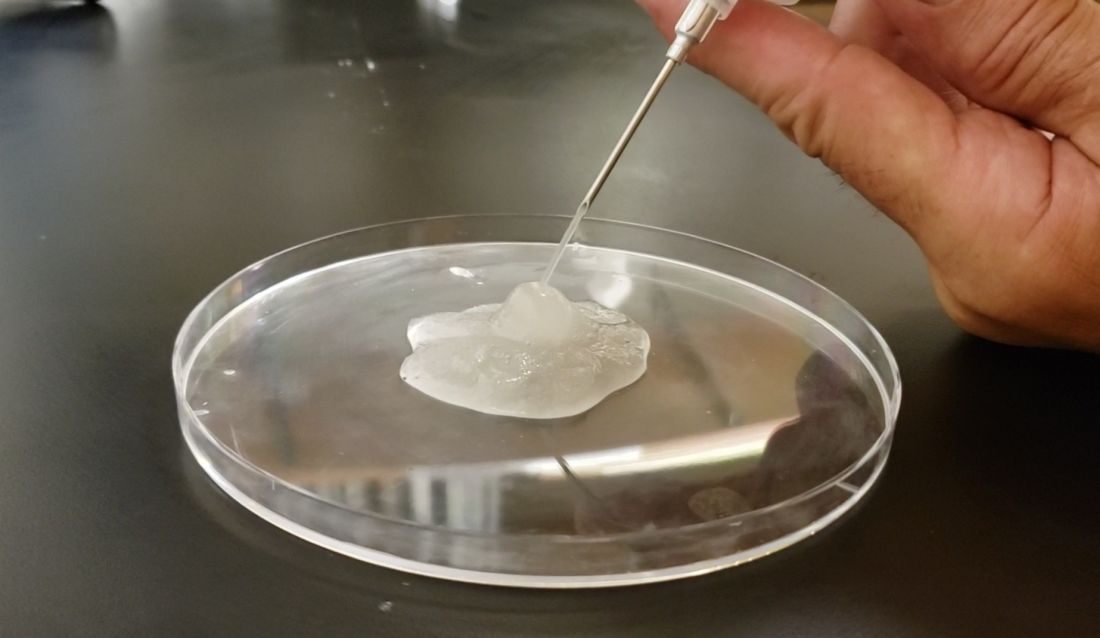
One of the seeds for the project was her own experience with cryolipolysis which involves topical cooling, a noninvasive method of removing subcutaneous fat for body contouring, which relies on conducting heat from subcutaneous fat across the skin and therefore, does not reach fat far from the dermis. With Dr. Anderson’s mentorship, she developed injectable cooling technology (ICT), a procedure where “ice slurry,” composed of normal saline and glycerol, is directly injected into adipose tissue, possibly leading to more efficient and effective cryolipolysis.
After nearly 10 years of animal studies at MGH, led by Dr. Garibyan as proof of concept trials, ice slurry (Coolio Therapy) recently received FDA breakthrough designation for long-term pain control and early-stage human trials of clinical applications are underway, she noted.
Magic Wand Program
In the Magic Wand program, participating physicians start by recording areas of unmet needs in their day-to-day practices, and in groups, engage in clinician-only brainstorming sessions to screen ideas, define problems, and generate lists of specifications and tools needed to address clinical problems. After working together to define challenges and possible solutions, they take their ideas to a development team, where scientists, engineers, regulatory experts, and industry professionals meet and help clinicians start pilot proof-of-concept projects, develop prototypes, and gain support for studies, followed by pilot feasibility studies.
Part of the project is the Virtual Magic Wand (VMW) Initiative, a 10-month online instructive and interactive course open to clinicians in the United States and Europe, designed to bring together dermatologists “interested in deeply understanding a dermatologic clinical problem worth solving,” according to Dr. Garibyan. Currently, there are more than 86 VMW scholars from 46 institutions, and military and private practice sites in the United States. The VMW was expanded to Europe in 2021 and there are plans to expand to Asia as well, she said.
The success of the program is not only attributed to its clinical methods but the fact that it provides a benefit to doctors at all stages of their careers, patients, and industry. “This is the only program that aims to engage in innovation from resident to full professor. We provide ideas that industry can then support and bring to market. Everyone including patients, doctors, and healthcare companies can benefit from active, engaged, and innovative physicians,” Dr. Garibyan said.
One of the success stories is that of Veradermics, a company founded by Kansas City dermatologist, Reid A. Waldman, MD, the company’s CEO, and Tim Durso, MD, the president, who met while participating in the VMW program in 2020, which eventually led them to start a company addressing an unmet need in dermatology, a kid-friendly treatment of warts.
In an interview with this news organization, Dr. Waldman explained how the program informed his company’s ethos. “Magic Wand Initiative is about identifying problems worth solving,” he said. At the company, “we find problems or unmet needs that are large enough to motivate prescribing changes, so we’ve really taken the philosophy I learned in the program into this company and building our portfolio.”
One of the first needs that Veradermics addressed was the fact that treatment for common warts, cryotherapy with liquid nitrogen, is painful and can frighten children, and, with a response rate of “at best, 50%,” Dr. Waldman said. Veradermics is in the process of creating a nearly painless, child-friendly wart treatment: an “immunostimulatory dissolvable microarray” patch that contains Candida antigen extract, which is currently being evaluated for treating warts in a phase 2 clinical trial started in 2023.
Although the Magic Wand Initiative was initially restricted to dermatologists at MGH, stories like that of Veradermics have made the program so popular that it has branched out to include anesthesiologists and otolaryngologists, as well as general and orthopedic surgeons at MGH, Dr. Garibyan said at the Mount Sinai meeting.
Dr. Garibyan disclosed that she is a cofounder of and has equity in Brixton Biosciences and EyeCool, and is a consultant for and/or investor in Brixton and Clarity Cosmetics. Royalties/inventorship are assigned to MGH.