New research in the emerging field of nanodermatology is setting the stage for the more efficient use of nitric oxide to treat infections. Nitric oxide (NO) is known for its antimicrobial activity, but it is difficult to channel this highly reactive gas into a convenient tool for clinical use.
Nanotechnology to the rescue! Nanotechnology allows researchers to create a vehicle for the controlled release of NO, study co-author Dr. Adam Friedman of Montefiore Medical Center in Bronx, NY, explained in an interview.
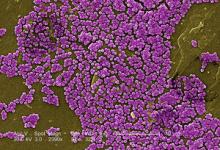
Tiny NO nanoparticles can penetrate the skin's surface and deliver the goods to deep tissue infections, overcoming the biological barriers that block the use of other therapeutic agents, he said.
"In this study [in rats], we demonstrated that both topical and intralesional injection of the nitric oxide nanoparticles were more effective in clearing MRSA muscle abscesses than vancomycin, a common first line systemic antibiotic for deep skin and soft tissue infections," said Dr. Friedman. "When the infected muscle tissue was examined under the microscope, samples from the nanoparticle-treated groups showed both decreased inflammation and destruction to normal tissue, likely owing to the swift and potent antibacterial impact of nitric oxide."
So, nanotechnology with NO is effective, but can it really be used in clinical practice? Dr. Friedman says yes.
"To date, most of the practical NO delivery systems have been based on NO donor molecules, which all suffer from various drawbacks ranging from tissue toxicity, instability (especially in the presence of light), and even carcinogenicity from related breakdown products," he said.
"The ease with which the nanoparticles can release NO, as well as that with which we can alter the rate of release by simply manipulating the production process, makes this technology a front runner for translation to the bedside," Dr. Friedman noted.
"That we were able to treat MRSA muscle infections by applying the nanoparticles to the skin, and that this approach was more effective then vancomycin, suggests that this technology may be a potent addition to our armament of treatments for skin and soft tissue infections," he said.
What's next? Filing an Investigation New Drug (IND) application with the FDA in hopes of beginning clinical trials, said Dr. Friedman.
"All in vitro and animal studies (including topical, subcutaneous injection, and intravenous) to date suggest that the nitric oxide-releasing nanoparticles are both safe (as in they do not cause damage to cells or tissues or negatively impact biological processes) and more importantly effective," he said. "We will continue to characterize the physical, chemical, and biological properties of this technology in the lab to help optimize its potential in the clinical setting."
Lead author Dr. David Shairer also of Montefiore Medical Center, Dr. Friedman, and their colleagues published their findings in the Jan./Feb. 2012 issue of Virulence ("Nitric oxide nanoparticles: Pre-clinical utility as a therapeutic for intramuscular abscesses").
Check out the website of the Nanodermatology Society for more about the intersection of these two fields.
–Heidi Splete (on twitter @hsplete)