Dermpath Diagnosis
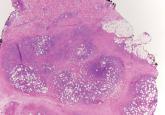
Subcutaneous Panniculitislike T-Cell Lymphoma
Subcutaneous panniculitislike T-cell lymphoma is a cutaneous lymphoma of α and β phenotype cytotoxic T cells in which the neoplastic cells are...
Sean W. Carlson, DO; Savina Aneja, MD; Kord Honda, MD; Kevin D. Cooper, MD
Dr. Carlson was from and Drs. Aneja, Honda, and Cooper are from the Department of Dermatology, University Hospitals Case Medical Center, Cleveland, Ohio. Dr. Carlson currently is from the Department of Radiology, Aultman Hospital,
Canton, Ohio. Drs. Honda and Cooper also are from the Multidisciplinary Cutaneous Oncology Program, Seidman Cancer Center, Cleveland, and the School of Medicine, Case Western Reserve University, Cleveland. Dr. Cooper also is from the Case Comprehensive Cancer Center, Cleveland.
The authors report no conflict of interest.
Correspondence: Sean W. Carlson, DO, 2600 Sixth St SW, Canton, OH 44710 (sean.carlson@aultman.org).

The natural history and therapeutic options differ greatly between subtypes of CBCL. For example, the prognosis of primary cutaneous follicle center lymphoma is generally favorable with a 5-year disease-specific survival rate of roughly 95%, and radiation therapy is recommended as a first-line therapy for localized disease.2,8 Conversely, primary cutaneous DLBCL (leg type) frequently spreads to extracutaneous sites8 and carries a much lower estimated 5-year disease-specific survival rate of 55%.2 Chemotherapy with R-CHOP is typically included in initial therapy for primary cutaneous DLBCL (leg type).8 The prognosis of systemic B-cell lymphomas also is highly variable and may depend on the type of B-cell lymphoma, the stage of disease at diagnosis, histologic and immunologic characteristics, and the therapy received. Wright et al9 reported that patients with systemic germinal center B cell–like DLBCL had a 5-year survival rate of 62%, whereas patients with activated B cell–like variants of DLBCL had a 5-year survival rate of 26%. Expression of CD40 may be a favorable prognostic factor following treatment with systemic chemotherapy in patients with DLBCL,10 whereas FOXP1 protein overexpression is correlated with poor disease-specific survival in certain DLBCL phenotypes.11
Although it is uncertain whether the cutaneous lesions preceded systemic disease in our patient, the cutaneous lesions could be arbitrarily classified as secondary because extracutaneous disease was discovered within 6 months of the initial diagnosis.1 However, classifying the CBCL as primary or secondary did not alter the course of treatment in our patient, as the presumed systemic disease necessitated treatment with systemic chemotherapy; both PCBCLs that develop systemic involvement and SCBCLs (primary extracutaneous disease) usually are treated with systemic chemotherapy. Our case highlights the importance of whole-body staging, as PET-CT scanning changed the course of care by detecting osseous involvement, necessitating systemic therapy as opposed to local radiation therapy alone. A multidisciplinary team with a focus on the diagnosis and management of cutaneous lymphomas helped streamline our patient’s laboratory testing and imaging studies, diagnostic and therapeutic decision making, and treatment implementation. Open channels and frequent opportunities for communication among dermatologists, dermatopathologists, medical oncologists, hematopathologists, radiologists, and radiation oncologists are needed to optimize and coordinate care for patients with cutaneous lymphoma who require transdisciplinary care.
Acknowledgement—The authors would like to thank Henry Koon, MD (hematology/oncology), for his input and expertise.
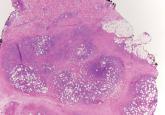
Subcutaneous panniculitislike T-cell lymphoma is a cutaneous lymphoma of α and β phenotype cytotoxic T cells in which the neoplastic cells are...

We report the case of a 61-year-old man with diffuse large B-cell lymphoma who presented with a tender skin lesion on the left side of the flank...

Primary extramedullary plasmacytoma is a rare plasma cell neoplasm that occurs as an isolated finding without detectable underlying multiple...
