Case
A 76-year-old woman presented to the ED with right rib pain after tripping on a rug and sustaining a fall down the stairs in her home. The patient’s chart review showed a history of multiple falls over the past year, with injuries including left rib fracture, right distal radius fracture, ankle sprain, forehead contusion, and left hip contusion. Regarding her social history, the patient denied any alcohol or drug use. She was not on any prescription medications and had no known medication or food allergies.
The physical examination was notable for a thin, white female in no apparent distress. The patient’s vital signs at presentation were: temperature, 97.2°F; blood pressure, 110/78 mm Hg; heart rate, 110 beats/minute; respiratory rate, 24 breaths/minute. She was somnolent but arousable and oriented to person, place, and time. The right chest wall was tender, and her lungs were clear to auscultation. The cardiac and neurological examinations were within normal limits. The patient had multiple contusions of various stages of healing over all extremities.Introduction
Geriatric patients aged 65 years and older represent a large, growing segment of the US population and, according to US Census Bureau data, represent an estimated 14% of the population.1 Moreover, this population accounts for 36% of all ambulance transports, 25% of hospitalizations, and 25% of total trauma costs.2 Although geriatric patients are less likely to be involved in trauma compared with other age groups, they are more likely to have fatal outcomes when injured. Approximately 28% of deaths due to accidental causes involve persons aged 65 and older. The highest mortality rates from trauma are noted in patients in the 8th decade and older.3
Mechanism of Injury and Preexisting Conditions
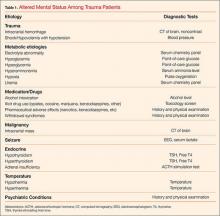
Falls are the most common mechanism of injury in patients over age 65 years,4 and mortality as a result of falls increases with advanced age.5 In addition to the increased risk of trauma, comorbid diseases are also common in this population and include diabetes mellitus, coronary artery disease, arthritis, renal disease, and pulmonary disease.6The presence of preexisting conditions, which affect a patient’s physiological age, is associated with increased mortality rates.7,8 As with other age groups, outcomes for geriatric trauma patients can also be predicted using the Injury Severity Score.9 Conditions associated with altered mental status in the geriatric trauma population and are listed in Table 1.
Review Data
Geriatric trauma patients frequently present with altered mental status. An understanding of potential etiologies of altered mental status is important to the ED diagnosis and management.The issue of traumatic injury in the aging population was studied at the authors’ institution through a retrospective chart review at the ED of Miami Valley Hospital, Dayton, Ohio, an urban hospital with an annual patient census of 95,000 visits.10 This study was approved by the Wright State University Institutional Review Board (IRB) and the Miami Valley Hospital Human Investigation and Research Committee (HIRC).
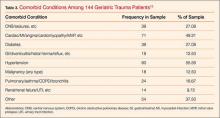
The study included 1,077 geriatric trauma patients, 144 of whom had a Glasgow Coma Score (GCS) of 14 or lower (13.4%). Fifty-four percent of the patients were male. Most (88.19%) of the patients were white, 9.72 % were black, 0.69% were Hispanic, and 1.39% were of other ethnicities. The median patient age was 78.5±7.81 (SD). Forty-two percent of patients were transferred to Miami Valley Hospital from another institution. The mode of arrival and mechanism of injury are outlined in Table 2. The most common mode of arrival was ambulance (n = 101), followed by helicopter (n = 38), and walk-in (n = 5). Fall (n = 106) and motor vehicle collision (n = 26) were the most common mechanisms of injury. The most common comorbid medical conditions were hypertension (56%) and heart disease (49%; Table 3).Laboratory Findings
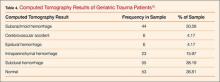
Hyperglycemia (n = 121) was the most common laboratory abnormality seen in patients, followed by anemia (n = 71), sodium abnormalities (n = 13), and hypoglycemia (n = 4). The most common finding on brain computed tomography (CT) was subdural hemorrhage (n = 55; Table 4). The results of both alcohol and urine toxicology screens are outlined in Table 5. In this study, 82 patients were not tested for alcohol intoxication, and 109 patients did not have a urine toxicology screen. Of the patients tested for alcohol intoxication, 20% had an alcohol level greater than 80 mg/mL (legal limit for operating a motor vehicle in the state of Ohio). There was no significant association between alcohol level and age, gender (Fisher’s exact test, P=.49), or ethnicity (Fisher’s exact test, P=.08). Opiates were the most commonly found substance in patients tested via a urine toxicology screen.