The recent spike in Zika virus cases in Central and South America brings with it the alarming risk – and even the expectation – of outbreaks occurring in the United States. How should U.S.-based clinicians prepare for the inevitable?
“The current outbreaks of Zika virus are the first of their kind in the Americas, so there isn’t a previous history of Zika virus spreading into the [United States],” explained Dr. Joy St. John, director of surveillance, disease prevention and control at the Caribbean Public Health Agency in Trinidad.
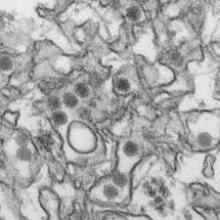
But now that the virus has hit the United States, with a confirmed case in Texas last week and more emerging since then, Dr. St. John said the most important thing is for U.S. health care providers to recognize the signs and symptoms of Zika virus infection. The virus is carried and transmitted by the Aedes aegypti species of mosquito, the same vector that transmits the dengue and chikungunya viruses. Zika virus symptoms are relatively mild, consisting predominantly of maculopapular rash, fever, arthralgia, myalgia, and conjunctivitis. Only one in five individuals with a Zika virus infection develop symptoms, but patients who present as such and who have traveled to Central or South America in the week prior to the onset of symptoms should be considered likely infected.
"At present, there is no rapid test available for diagnosis of Zika,” said Dr. St. John. “Diagnosis is primarily based on detection of viral RNA from clinical serum specimens in acutely ill patients.”
To that end, polymerase chain reaction (PCR) testing can be conducted on serum samples collected within 3-5 days of symptom onset. Beyond that, elevated levels of IgM antibodies can be confirmed by serology, based on the neutralization, seroconversion, or four-fold increase of Zika-specific antibodies in paired samples. However, Dr. St. John warned that “Due to the possibility of cross reactivity with other viruses, for example, dengue, it is strongly recommended samples be collected early enough for PCR testing.”
Zika and pregnancy
Zika virus has now been identified in more than 20 countries and territories worldwide, most of them in the Americas, although outbreaks have occurred in areas of Africa, Southeast Asia, and the Pacific Islands. While most infected patients experience relatively mild symptoms, Zika may be particularly dangerous when it infects a pregnant woman. There have been multiple cases of microcephaly in children whose mothers were infected with Zika virus during pregnancy, although the association of microcephaly with Zika virus infection during pregnancy has not been definitively confirmed. The Centers for Disease Control and Prevention recently issued a warning to Americans – particularly pregnant women – about traveling to high-risk areas.
“Scientifically, we’re not 100% sure if Zika virus is causing microcephaly, [but] what we’re seeing is in certain Brazilian districts, there’s been a 20-fold increase in rates of microcephaly at the same time that there’s been a lot more Zika virus in pregnant women,” explained Dr. Sanjaya Senanayake of Australian National University in Canberra.
According to data from the CDC, 1,248 suspected cases of microcephaly had been reported in Brazil as of Nov. 28, 2015, compared with the annual rate of just 150-200 such cases during 2010-2014. “Examination of the fetus [and] amniotic fluid, in some cases, has shown Zika virus, so there seems to be an association,” Dr. Senanayake clarified, adding that “the [ANVISA – Brazilian Health Surveillance Agency] has told women in certain districts where there’s been a lot of microcephaly not to get pregnant.”
Brazil is set to host millions of guests from around the world as the 2016 Olympics get underway in only a few months’ time. Women who are pregnant or anticipate becoming pregnant should consider the risks if they are planning to travel to Rio de Janeiro. The risk of microcephaly does not apply to infected women who are not pregnant, however, as the CDC states that “Zika virus usually remains in the blood of an infected person for only a few days to a week,” and therefore, “does not pose a risk of birth defects for future pregnancies.”
Dr. St. John also stated that “public health personnel are still cautioning pregnant women to take special care to avoid mosquito bites during their pregnancies,” adding that the “[Pan-American Health Organization] is working on their guidelines for surveillance of congenital abnormalities.”
Clinical insights
With treatment options so sparse – there is no vaccine or drug available specifically meant to combat a Zika virus infection – what can health care providers do for their patients? The CDC advises health care providers to “treat the symptoms,” which means telling patients to stay in bed, stay hydrated, and, most importantly, stay away from aspirin and NSAIDs “until dengue can be ruled out to reduce the risk of hemorrhage.” Acetaminophen is safe to use, in order to mitigate fever symptoms.