Necrotizing fasciitis is a rare but lifethreatening soft-tissue infection. Its presentation is characterized by rapidly spreading inflammation and resultant death—both of the surrounding soft tissue and fascial planes. Prompt recognition and aggressive treatment are paramount to avoid fatality, and appropriate management in the ED is essential to a successful outcome. As the following case illustrates, a high index of suspicion and multidisciplinary approach, including applicable imaging studies, result in timely diagnosis and treatment.
Case
A 60-year-old woman with a medical history of childhood Lyme disease, asthma, high cholesterol, and seasonal allergies, presented to the ED with a 3-day history of left hip and thigh pain, general malaise, decreased appetite, nausea, myalgia, and increased lethargy. She reported difficulty with weight-bearing on her left leg but denied any recent leg trauma or falls. Patient also had a 3-year history of intermittent hip pain, which she treated with ibuprofen. Three weeks prior to presentation, she had undergone an invasive dental procedure in preparation for a root canal. She later developed a fever of 102° F and had taken ibuprofen two-and-a-half hours prior to arrival at our institution.
Initial vital signs on physical examination were: blood pressure (BP) 71/37 mm Hg; heart rate (HR), 98 beats/minute; respiratory rate, 18 breaths/minute; temperature, 98.5° F. Oxygen saturation was 100% on room air. Patient was awake and alert but extremely pale and sluggish. Her head, ears, nose, and throat; pulmonary; cardiac; and abdominal examinations were normal. On physical examination, the skin overlying her left hip and thigh was grossly unremarkable, and no previous incision sites or areas of trauma were observed throughout the left lower extremity. No obvious signs of infection or erythema were noted; however, an area of warmth was felt on the lateral aspect of the left thigh but did not extend beyond the knee. Patient was able to flex her left hip approximately 30° and only complained of pain to the lateral aspect of the upper leg with passive internal and external rotation. Heel strike was negative, and knee examination was negative for pathology. The right lower extremity was unremarkable.
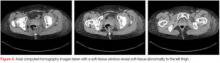
Laboratory evaluation revealed a white blood cell count of 6.6 x 109/L (reference range, 3.8-10.5 x 109/L); erythrocyte sedimentation rate of 21 mm/h, (reference range, 0-20 mm/h); C-reactive protein level of 31.40 mg/dL (reference range 0-0.40 mg/dL); and lactate level of 2.8 mmol/L (reference range, 0.7-2.1 mmol/L).A plain radiograph of the pelvis and left hip showed soft-tissue swelling but no bony pathology or fracture (Figure 1). There was no visual evidence of subcutaneous gas, and chest radiograph was negative for any active disease. Based on the clinical picture of septic shock due to possible septic arthritis, emergent magnetic resonance imaging (MRI) of the left hip and thigh was performed without contrast (Figures 2 and 3). Extensive edema was noted diffusely throughout patient’s left gluteus medius muscle and vastus latera lis muscle; no loculated fluid collection was noted. The edema was concentrated around the proximal left thigh but extended to the level of the knee. The left hip was free of any fluid collection, ruling-out septic arthritis. Based on these MRI findings, a computed tomography scan was ordered, which showed no fluid collection in the pelvis and abdomen (Figure 4).
During the course of evaluation, the patient continued to decline. Her vital signs were not responding appropriately, and she was started on a sepsis protocol, which included aggressive intravenous (IV) fluid resuscitation with normal saline and IV vancomycin. After 2 L of IV fluid, there was still no improvement in BP, although patient remained awake, alert, and oriented. She was then started on vasopressor support with continuous IV fluids, and a Foley catheter was placed to measure urinary output, which was minimal. After radiological review of all scans showed no infected joints, the patient was admitted to the intensive care unit (ICU) with a diagnosis of necrotizing fasciitis. She was promptly brought to the operating room (OR) where her vital signs continued to deteriorate to a BP of 68/50 mm Hg and HR of 126 beats/minute prior to anesthesia induction. After being positioned on the operating table, the lateral aspect of her left thigh was found to have a well-demarcated area of erythema, measuring approximately 4 x 3 cm, with palpable subcutaneous crepitus. Surgery was performed under general anesthesia while maintaining vasopressor support. Several lateral incisions were made, which revealed gray purulent fluid in the subcutaneous and fascial layers, and weakness and dullness of the vastus lateralis muscle. All necrotic fasciae were debrided. Fluid collections extended from the buttock to the posterolateral thigh region. Cultures were obtained and Penrose drains were placed, and the wounds were loosely approximated. After application of sterile dressings, patient was transferred to surgical ICU and remained intubated on vasopressor support. She returned to the OR the following day for further examination and debridement. All surgical wounds were again copiously irrigated and dressed sterilely.