CHICAGO – Frequent flyers, patients with a history of at least five visits per year to the emergency department, might benefit from high-risk care plans, based on research from the University of Maryland health care system.
The plans are designed to improve patient safety by reducing exposure to ionizing radiation and have the additional benefit of reducing the costs of care, Dr. Leen Alblaihed, a resident physician at the university, reported at the annual meeting of the American College of Emergency Physicians.
After high-risk care plans were put into the emergency physician work flow for 41 patients with a history of high emergency department utilization, unneeded tests declined. Other important outcomes were statistically significant reductions in hospitalizations and quantities of prescribed opioids.
he patients considered for the study had to have at least five ED visits and three admissions per year. Based on the electronic medical record data of the university’s two suburban medical centers, a total of 845 patients met that definition.
The high-risk care plans for the management of the 41 patients were developed by a multi-disciplinary team of case managers, emergency physicians, and hospitalists. The plans were then integrated into the physician electronic documentation and work flow.
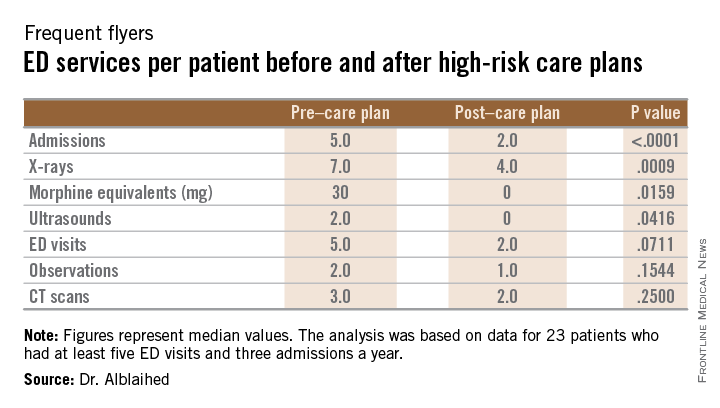
The data analysis was based on 23 of the patients, 10 men and 13 women with a median age of 48 years, who had 6 months of data before and 6 months of data after the care plan was instituted. The primary outcome measures were a reduction in ionizing radiation. Secondary outcome measures were reductions in ED visits, hospital admissions, observation stays, and opioid prescriptions based on morphine equivalent totals.
Compared to the data before the care plan was instituted, the 23 patients had nearly half as many x-rays and CT scans and a nearly sixfold reduction in prescribing of morphine equivalents. While ED visits decreased modestly from 116 to 82, the admission rates dropped from 99 to 37 and observation stays declined from 43 to 28.
The study group had decreases in all measures after high-risk care plans. X-ray studies decreased from 202 to 106, CT scans declined from 107 to 50, and opiate prescribing decreased from 3824 mg to 675 mg in morphine equivalents.
Because the outcomes were not normally distributed, medians and interquartile ranges were analyzed using the Wilcoxon signed-rank test to compare the pre/post median values (see table).