Copeptin levels of less than 2.5 pmol/L reliably identified diabetes insipidus after pituitary surgery, while levels of more than 30 pmol/L ruled out the condition, investigators reported online in the Journal of Clinical Endocrinology and Metabolism.
“Copeptin represents a new, early, and reliable single marker for postoperative diabetes insipidus in the post–pituitary surgery setting, where no such marker currently is known,” said Dr. Bettina Winzeler at University Hospital of Basel (Switzerland) and her associates. Postoperative measures of copeptin levels might help clinicians to differentiate patients who need closer postsurgical inpatient observation from those who can safely be discharged.
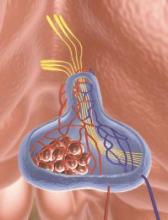
About 16%-34% of patients who undergo surgery in the sellar region develop central diabetes insipidus, which, without prompt rehydration, can cause severe hypernatremia, Dr. Winzeler and her associates noted. Risk factors for postoperative diabetes insipidus are not useful markers; however, copeptin, a surrogate of arginine vasopressin, is stable and can be measured quickly and reliably.
The researchers hypothesized that patients with postoperative diabetes insipidus would not have the markedly elevated copeptin levels that surgical stress normally triggers when posterior pituitary function is adequate. To test that theory, they measured daily postoperative copeptin levels for 205 consecutive patients who underwent surgeries for sellar lesions or tumors near the hypothalamus or pituitary gland (J. Clin. Endocrinol. Metab. 2015 Apr. 29 [doi:10.1210/jc.2014-4527]).
One day after surgery, 22 (81.5%) of the 27 patients whose copeptin levels were less than 2.5 pmol/L had diabetes insipidus (positive predictive value, 81%; specificity, 97%), said the researchers. In contrast, one of 40 (2.5%) patients with copeptin levels greater than 30 pmol/L had diabetes insipidus (negative predictive value 95%; sensitivity, 94%). Patients with diabetes insipidus also had significantly lower median and interquartile (25th-75th percentile) copeptin levels, compared with other patients (median for patients with diabetes insipidus, 2.9 pmol/L; interquartile range, 1.9-7.9 pmol/L; median for other patients, 10.8 pmol/L; IQR, 5.2-30.4 pmol/L; P less than .001). In the multivariate analysis, low postoperative copeptin levels remained associated with diabetes insipidus after adjusting for age, gender, body-mass index, tumor size and type of surgery, history of surgery or radiotherapy, cerebrospinal fluid leakage, and serum sodium concentration, the investigators reported (odds ratio, 1.62; 95% confidence interval, 1.25-2.10; P less than .001).
The study did not use standardized diagnostic criteria for diabetes insipidus, and postoperative blood samples were obtained as part of daily care and not at fixed time points, Dr. Winzeler and her associates noted. “Absence of standardized sampling for copeptin measurement at a defined early time point presumably decreased copeptin accuracy in this study, rendering our findings conservative,” they cautioned.
The Swiss National Foundation partially funded the research. Three coauthors reported having received speaker honoraria from Thermo Scientific Biomarkers, which develops and makes the copeptin assay.