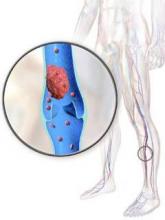
In cancer patients with acute, symptomatic venous thromboembolisms, daily tinzaparin does not significantly reduce recurrent venous thromboembolisms, overall mortality, or major bleeding compared with warfarin, but does reduce clinically-relevant nonmajor bleeding, according to a 900-patient randomized trial published in JAMA.
Tinzaparin (Innohep) is a low-molecular-weight heparin (LMWH) marketed outside the United States. LMWHs are generally recommended over warfarin to treat acute venous thromboembolism (VTE) in cancer patients, but the recommendation is based mostly on a single trial over a decade old; that might explain why, worldwide, vitamin K antagonists are still heavily used in patients with cancer-associated thrombosis, said the authors, led by Dr. Agnes Lee, of the University of British Columbia (Vancouver).
To revisit the issue in the modern treatment era, Dr. Lee and her colleagues randomized 449 adults with active cancer and documented deep vein thrombosis or pulmonary embolism to tinzaparin (175 IU/kg) once daily for 6 months, and 451 others to 6 months of conventional therapy with tinzaparin (175 IU/kg) once daily for 5-10 days followed by warfarin dose adjusted to maintain therapeutic range (JAMA. 2015;314[7]:677-86).
The subjects were recruited from 164 centers in Asia, Africa, Europe, Canada, and Central and South America; all had a life expectancy greater than 6 months. The mean age in the study was 59 years, and 60% of the subjects were women. Gynecologic and colorectal cancers were the most common in the study.
Recurrent VTE occurred in 31 patients in the tinzaparin group and 45 in the warfarin group, giving a 6-month cumulative incidence of 7.2% for tinzaparin versus 10.5% for warfarin (hazard ratio [HR] 0.65; 95% CI 0.41-1.03; P = .07).
There was major bleeding in 12 (2.7%) tinzaparin patients and 11 (2.4%) warfarin patients, an insignificant difference (HR 0.89; 95% CI 0.40-1.99; P = .77); 150 tinzaparin patients (33.4%) and 138 warfarin patients (30.6%) died in the trial, also an insignificant difference (HR, 1.08; 95% CI 0.85-1.36; P = .54).
There were 49 (10.9%) clinically relevant but nonmajor bleeds in the tinzaparin group versus 69 (15.3%) among warfarin patients, a difference that was significant (HR 0.58; 95% CI 0.40-0.84; P = .004). Clinically relevant nonmajor bleeding meant nonfatal bleeding outside of a critical area or organ that still required intervention but did not cause a fall in hemoglobin greater than 2 g/dL.
There were fewer than anticipated thrombotic events in the warfarin group. “We had expected a recurrence rate of 12.6% with warfarin; the observed rate was only 10.5%. This potentially affected the power of the trial to detect a benefit associated with tinzaparin.” Also, “a significant reduction in recurrent [VTEs] might be observed with tinzaparin” among patients at higher risk for them than were in the study, the investigators said.
Even so, the trial did demonstrate “that tinzaparin, even when given at a full therapeutic dose for up to 6 months, is safe in a broad oncology population,” they said.
LEO Pharma, makers of tinzaparin, funded the study. The company was involved throughout the trial, including data analysis and approval of the manuscript. Dr. Lee reported honoraria, consulting fees, and research funding from the company. Other authors reported payments from LEO for those or other reasons.