WASHINGTON – Recommendations for universal lipid screening between 9 and 11 years and again between ages 17 and 21 – and selective screening of children with risk factors starting at age 2 years – may best be heeded by measuring nonfasting total cholesterol and high-density lipoprotein, pediatric cardiologist Dr. Sarah de Ferranti told a packed room at the annual meeting of the American Academy of Pediatrics.
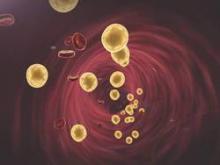
The difference of the two values is the non-HDL cholesterol level (total cholesterol minus HDL) and represents the atherogenic portion of the lipid profile. It is a “valid” initial result, she assured pediatricians.
Non-HDL values of 145 mg/dL and over should then be further explored through a complete fasting lipid profile, said Dr. de Ferranti, who directs the preventive cardiology program at Boston Children’s Hospital.
While the nonfasting, non-HDL approach has been deemed acceptable for universal screening, national guidelines endorsed by the AAP recommend that selective testing of high-risk children be done with a fasting profile. “But I think people find that onerous,” Dr. de Ferranti said. “Doing a nonfasting test initially [in any pediatric case] is quite reasonable. It’s more convenient, and it may help us to better implement the guidelines and not lose families.”
In 2011, the National Heart, Lung, and Blood Institute (NHLBI) called on physicians not only to selectively screen children with risk factors for cardiovascular disease, but to screen their healthy 9- to 11- and 17- to 21-year-old patients, and to provide lifestyle therapy for patients who have high LDL cholesterol readings on follow-up testing, and then statin treatment for those who don’t respond.
Surveys have shown that fewer than half of pediatricians do routine screening, however, and that many are frustrated with the limitations of lifestyle interventions and at least somewhat uncomfortable with the concept of statin treatment.
The AAP’s own recommendations for lipid screening, issued in 2008, were confined to selective screening of children with risk factors such as obesity, diabetes, or hypertension, or a family history of heart attack, stroke, and high cholesterol. But in 2011, the academy endorsed the NHLBI’s Integrated Guidelines for Cardiovascular Risk Reduction in Childhood and Adolescence, embracing its additional call for screening healthy children during two windows of time.
Both guidelines – the AAP’s and the NHLBI’s – recommend statin treatment for patients whose LDL remains at 190 mg/dL or above after 6 months of lifestyle therapy, and for patients whose LDL is 160 mg/dL or above after lifestyle therapy when additional risk factors are present.
Dr. de Ferranti acknowledged gaps in research on the benefits of early treatment and said that, personally, she is “not sure that [universal screening] will definitely be the right approach for the future.”
She implored pediatricians, however, to remember when making practice decisions that universal screening “has attempted to address the fact that getting a family history [of cardiovascular disease] isn’t always helpful or reliable” for identifying children at high risk of cardiovascular disease, even those with familial hypercholesterolemia.
Familiar hypercholesterolemia is a disorder of LDL cholesterol processing estimated to affect 1 in 250 individuals. It’s usually “asymptomatic until individuals present in their young adulthood with a much higher risk of heart disease … or until they come to the ER as young adults,” said de Ferranti, assistant professor of medicine at Harvard Medical School, Boston.
Studies have shown that individuals aged 20-39 years who have the disorder are almost 90 times as likely to die from coronary heart disease as is the general population in that age group, she noted.
Available data on the impact of treating familiar hypercholesterolemia in childhood is “relatively scant” but “convincing,” she said. One randomized controlled study of statin treatment in children with the disorder used vascular thickness as a proxy for cardiovascular events. Children who took pravastatin for 2 years had a lower mean carotid intima media thickness, and lower LDL levels, compared with children assigned to placebo (JAMA 2004 Jul 21;292[3]:331-7).
Further follow-up of these children has suggested delayed atherosclerotic disease and prevention of cardiac events in the statin group, Dr. de Ferranti noted. And separate observational research shows a significant reduction in cardiovascular disease events in affected adults taking statins.
Not all pediatricians are convinced that screening is justified. A 2013 electronic survey of pediatric providers in Minnesota showed that while 77% supported the concept of lipid screening, 33% performed no screening, 50% screened selectively, and only 16% performed universal screening. (J. Pediatr. 2014 Mar;164[3]:572-6).
In a recent national survey of randomly selected, practicing AAP members, at least two-thirds indicated that they screen based on family history, high-risk conditions, and obesity. Fewer than half said they perform universal age-based screening.