Diagnosis: Pemphigoid gestationis
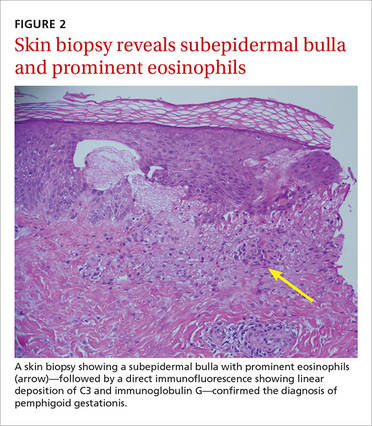
Based on the appearance of the lesions and the lab findings, we diagnosed our patient with pemphigoid gestationis (PG). The pathology demonstrated a subepidermal blister with prominent eosinophils, which supported the diagnosis (FIGURE 2). Direct immunofluorescence further supported the diagnosis, as it showed a thick, dense, and linear C3 deposition and weak immunoglobulin G deposition along the epidermal basement membrane zone.
PG, previously referred to as herpes gestationis, is a rare autoimmune dermatosis of pregnancy that usually presents with intense, pruritic, erythematous papules and blisters that surround the umbilicus. PG lesions spread rapidly throughout the body, but tend to spare the face and oral mucosa. The incidence is approximately 1 in 50,000 pregnancies.1
Although the exact pathogenesis of PG is unknown, it is hypothesized that major histocompatibility complex class II antigens within the placenta may play a role through cross-reaction with maternal skin.2
PG usually develops weeks to months before delivery
The onset of PG is usually during the second or third trimester; it typically manifests earlier and with greater severity in subsequent pregnancies.2 That said, postpartum cases and cases where PG “skipped” pregnancies have been reported.2 PG can impact the fetus—about 5% to 10% of infants born to affected mothers have a diffuse bullous eruption similar to that of PG.3 One study found a fetal mortality rate of up to 30% and high rates of prematurity.1
This case represents an interesting variation because the patient hadn’t developed any dermatologic conditions during her previous 2 pregnancies, and it was only after she delivered her third child that she developed PG. While there is a wide range of possible presentations of PG, all mothers who have it should be monitored by an obstetrician and should follow up with a dermatologist during their prenatal periods due to the small but significant risks of prematurity and fetal growth restriction.4
Reactivation of symptoms. Although PG symptoms typically resolve several weeks before delivery, 75% of patients experience reactivation of their symptoms at delivery.4 Progestin has immunosuppressive properties, and variations in progestin levels near delivery are thought to be responsible for the relapsing-remitting course of PG symptoms.4
Rule out other diagnoses with patch testing, skin biopsy
Pruritic and erythematous bullae and vesicles, particularly around the umbilicus, should raise clinical suspicion for PG in a pregnant patient. A skin biopsy showing a subepidermal bulla with prominent eosinophils, as well as direct immunofluorescence showing linear deposition of C3 and IgG at the dermo-epidermal junction, indicates a diagnosis of PG.
The differential diagnosis of PG includes urticarial/bullous drug eruptions, viral exanthems, allergic contact dermatitis, and pruritic urticarial papules and plaques of pregnancy (PUPPP). Clinical correlation and a careful review of the patient’s medications, symptoms, and exposure to viruses can aid in ruling out a drug eruption or viral exanthema. Patch testing can be performed to rule out allergic contact dermatitis, and serum testing or indirect immunofluorescence or enzyme-linked immunosorbent assay is recommended to rule out PUPPP.