When I became a family physician (FP), it never crossed my mind that I would one day be asking school-aged children about bullying. Not so much because bullying didn’t exist, but because I wasn’t aware of the pervasiveness and seriousness of the problem and because there were no professional recommendations to do so.
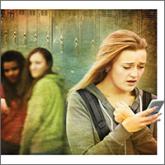
That said, my family had some first-hand experience with the issue: One of my children was bullied in grade school. When my wife found out, she promptly visited the 2 boys’ homes and told them and their parents that the behavior would stop or else! (She may have used more colorful language.) And it did stop. But times have changed, and so has the nature of bullying, which can now extend beyond the hallway to an entire school body in seconds with a few taps on a cell phone. And the adverse consequences can be significant, as described by McClowry and colleagues.
The prevalence of bullying is discouragingly high, estimated to be about 20% in national surveys.1 Because bullying occurs so frequently, public health, community-based, and school-based approaches, rather than one-on-one office-based interventions, are likely to have the greatest overall impact on decreasing bullying. Randomized trials bear this out, showing that prevention programs in schools can effectively reduce the behavior.2,3
What is our responsibility as FPs? Screening is a reasonable first step, even in the absence of randomized trials demonstrating benefit. Because there have been no physician office-based trials of screening or interventions for bullying, we must rely on “expert opinion” at this time, with no assurance that what we do will actually help children. Absence of proof of benefit, however, does not mean absence of benefit, and doing nothing will definitely not help anyone. The authors recommend a single screening question: "Are you being bullied?"—especially for children who are at higher risk, such as those with disabilities/special health needs, LGBTQ+ status, and who are under- or overweight.
Clearly we need research to know which interventions truly help these children/adolescents and their parents. In the meantime, however, identifying the problem and offering emotional support are unlikely to harm—and may help. Opening the lines of communication, connecting children and their parents with available community resources, and supporting anti-bullying programs in your schools are additional ways we can make a difference today.