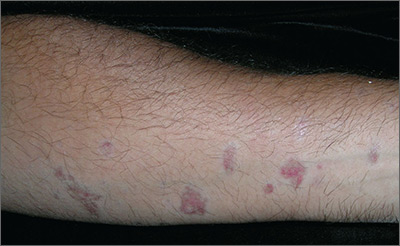
Biopsy results revealed that this was a case of atrophic lichen planus, one of the rarer types of lichen planus that is defined by nonpalpable lesions. The FP examined areas of the patient where lichen planus is commonly found (including the wrist, ankles, and back) and discovered a few similar lesions around the patient’s ankles.
The FP explained the diagnosis to the patient and offered a mid-potency topical corticosteroid—0.1% triamcinolone cream. She advised the patient that if the lesions became more atrophic, they could try to get a topical vitamin D medication approved as an alternative. There is evidence that topical vitamin D may be beneficial, with no risk of skin atrophy. However, these are high-cost medications—despite the fact that some are now generic. A prior authorization for one of these vitamin D medications is more likely to be approved if there has been a failure, or adverse effects, from a first-line topical steroid.
Other treatment options for atrophic lichen planus include oral metronidazole and oral prednisone. The mechanism for the effectiveness of oral metronidazole is unknown, but it is a relatively safe option if topical treatments fail. Oral prednisone taken for 20 to 30 days is more likely to be effective, but is also more likely to cause adverse effects.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com