A previously healthy 12-year-old boy with normal development presented to his primary care physician (PCP) with a 1-week history of moderate ear pain. He was given a diagnosis of acute otitis media (AOM) and prescribed a 7-day course of amoxicillin. Although the child’s history was otherwise unremarkable, the mother reported that she’d had a deep venous thrombosis and pulmonary embolism a year earlier.
The boy continued to experience intermittent left ear pain 2 weeks after completing his antibiotic treatment, leading the PCP to refer him to an otolaryngologist. An examination by the otolaryngologist revealed a cloudy, bulging tympanic membrane. The patient was prescribed amoxicillin/clavulanate and ofloxacin ear drops.
Two days later, he was admitted to the emergency department (ED) due to worsening left ear pain and a new-onset left-sided headache. His left tympanic membrane was normal, with no tenderness or erythema of the mastoid. His vital signs were normal. He was afebrile and discharged home.
A week later, he returned to the ED with worsening ear pain and severe persistent headache, which was localized in the left occipital, left frontal, and retro-orbital regions. He denied light or sound sensitivity, nausea, vomiting, or increased lacrimation. He was tearful on examination due to the pain. He had no meningismus and normal fundi. A neurologic examination was nonlateralizing. Laboratory tests showed a normal complete blood count but increased C-reactive protein at 113 mg/dL (normal, < 0.3 mg/dL) and an erythrocyte sedimentation rate of 88 mm/hr (normal, 0-20 mm/hr).
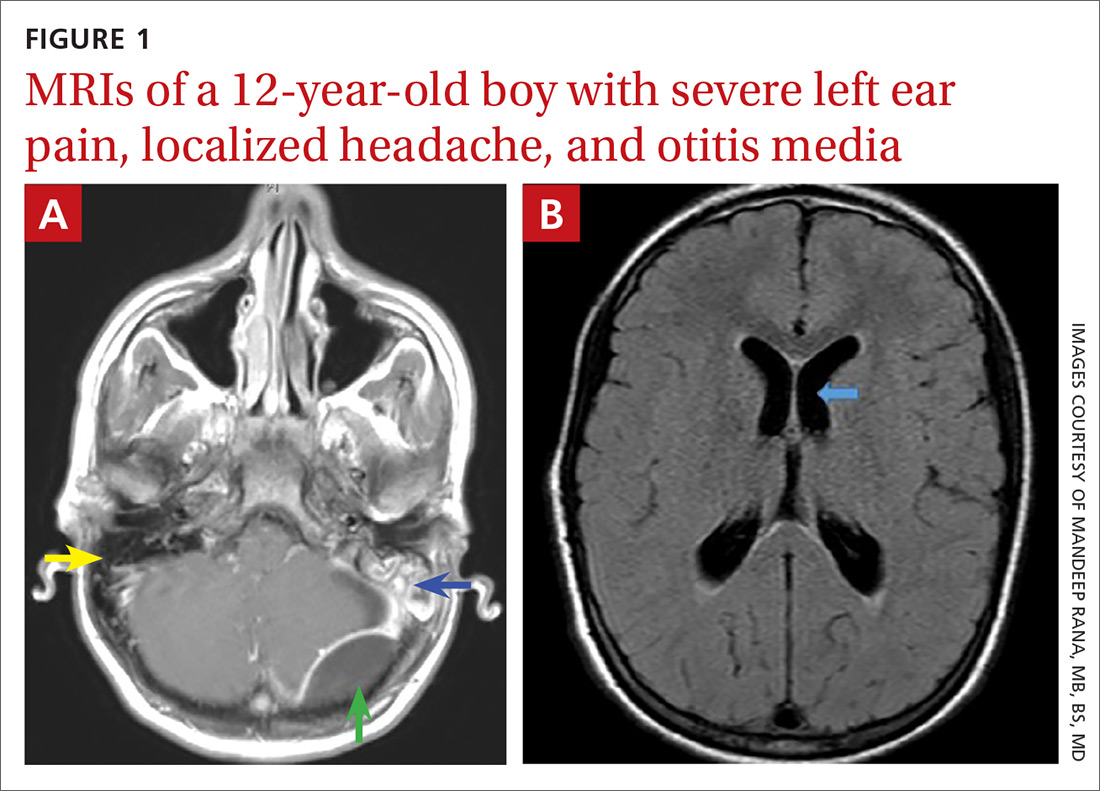
Magnetic resonance imaging was ordered (FIGURES 1A and 1B), and Neurosurgery and Otolaryngology were consulted.